The Effect of Resistance Exercise Intensity on Acute Hyperglycemia in Young Adult Males
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Protocol
2.3. Biochemistry
2.4. Statistics
3. Results
3.1. Induction of Pre-RE Hyperglycemia
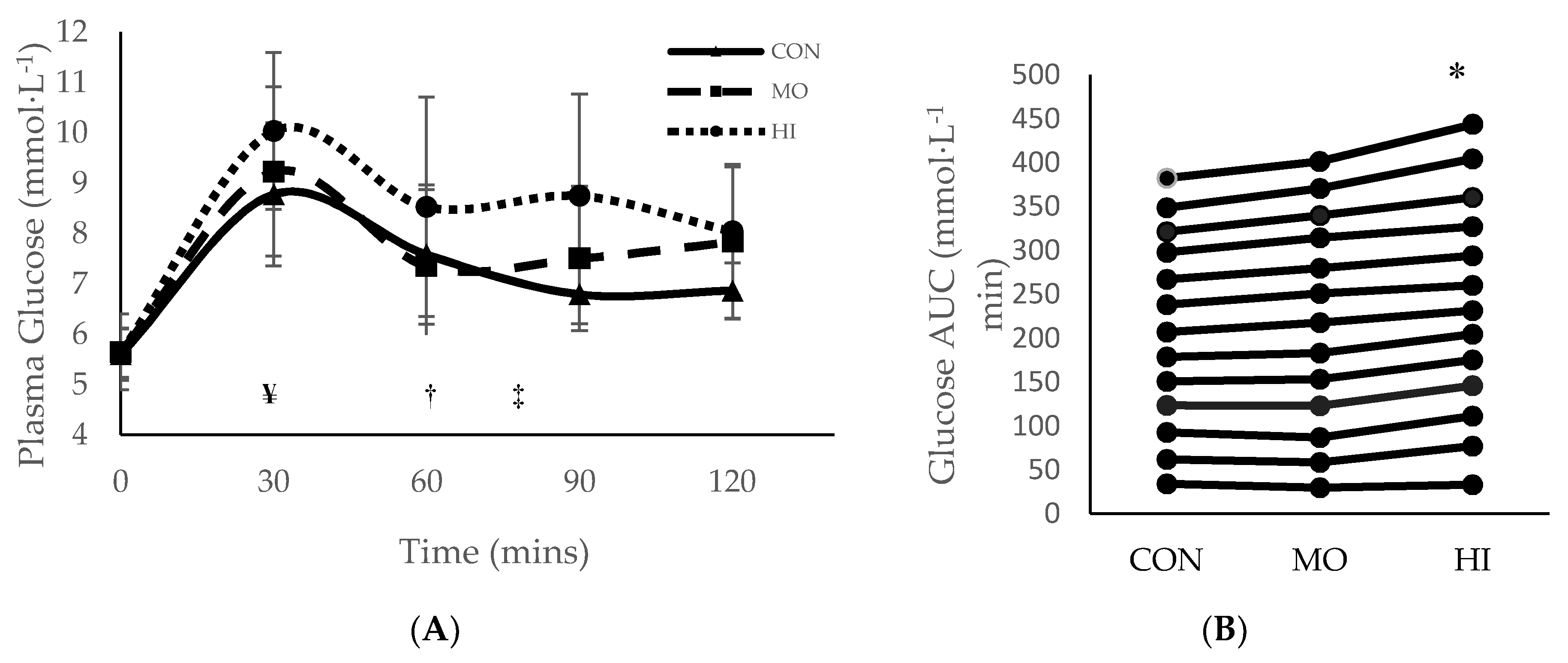
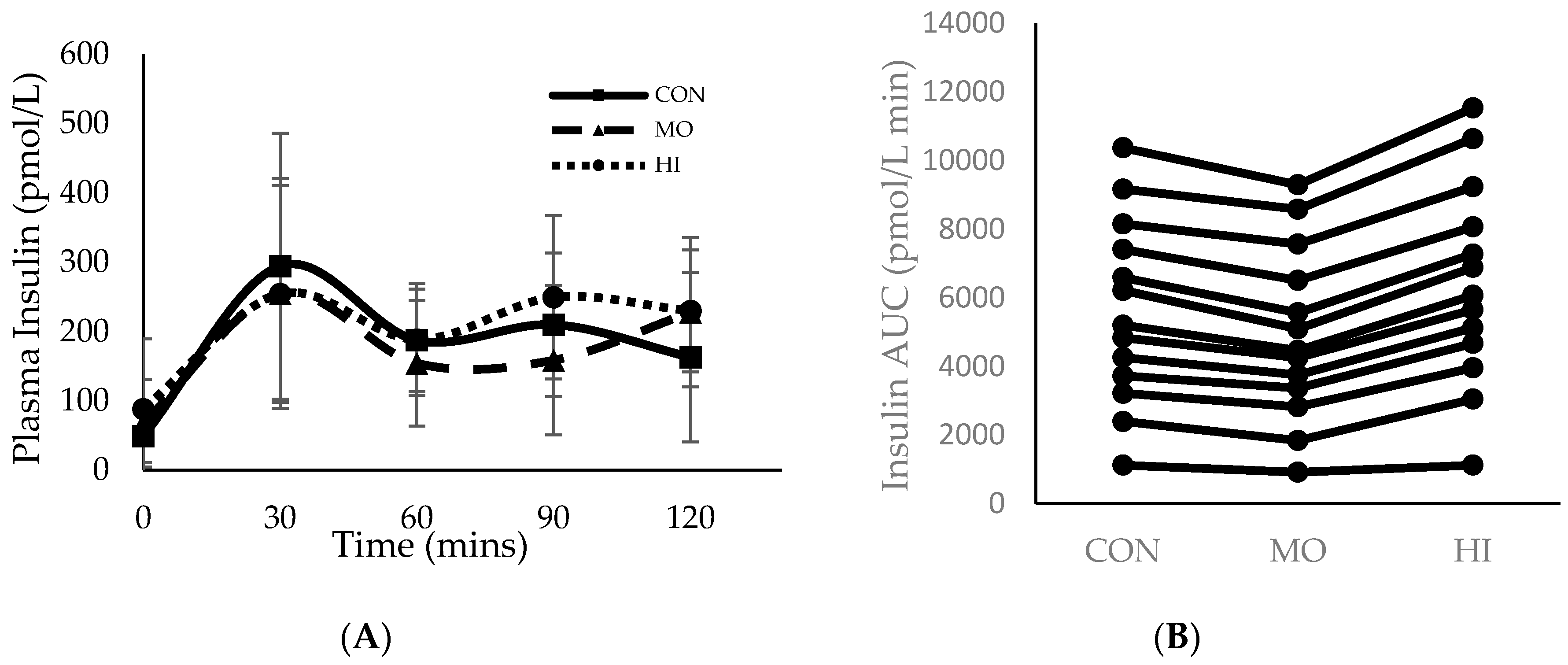
3.2. Glycemic Response during RE
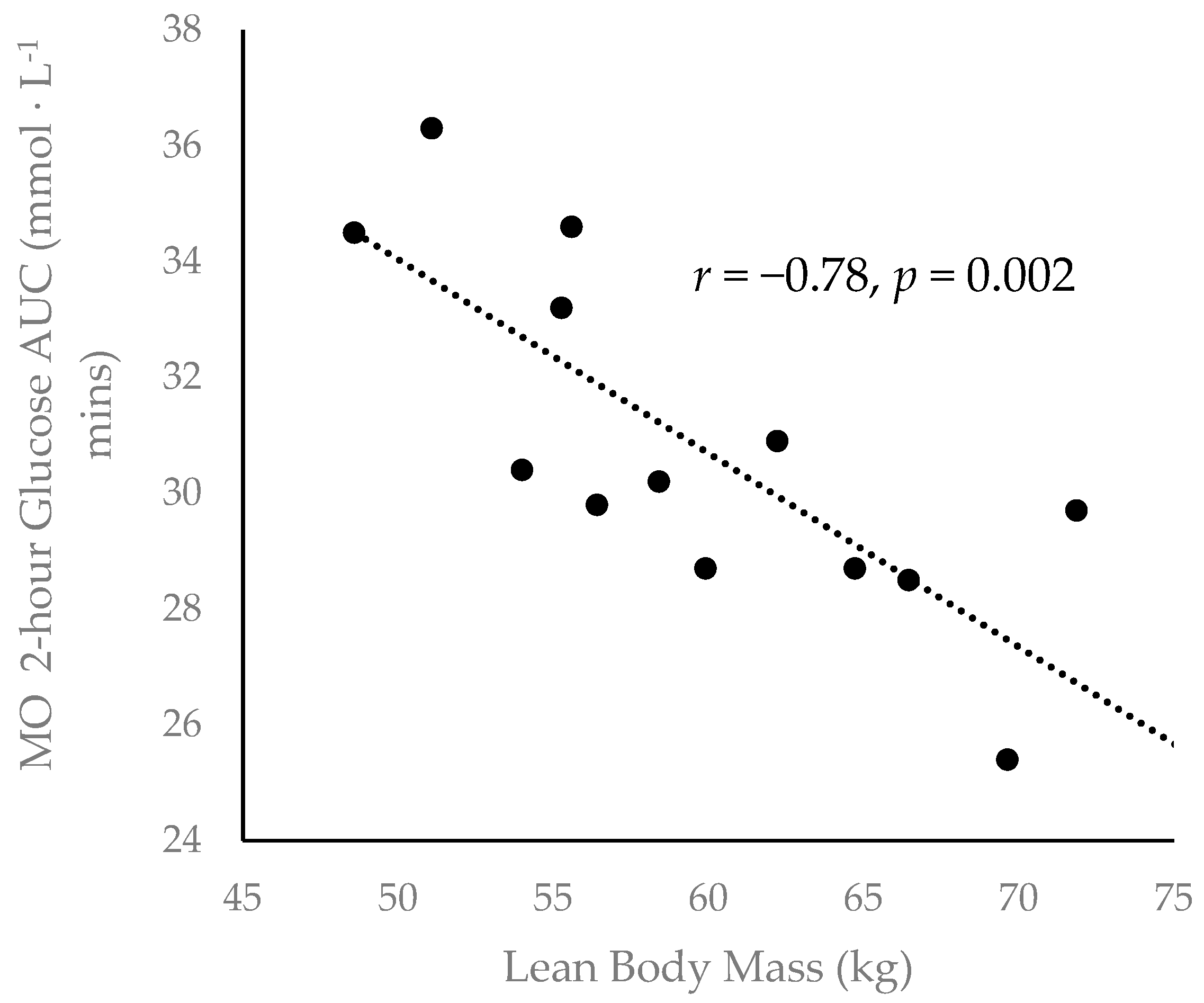
3.3. Body Composition and Glycemic Response
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Danaei, G.; Finucane, M.M.; Lu, Y.; Singh, G.M.; Cowan, M.J.; Paciorek, C.J.; Lin, J.K.; Farzadfar, F.; Khang, Y.-O.; Stevens, G.A.; et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011, 378, 31–40. [Google Scholar] [CrossRef]
- NCD-RisC. Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4·4 million participants. Lancet 2016, 387, 1513–1530. [Google Scholar] [CrossRef]
- Kaiser, A.B.; Zhang, N.; van der Pluijm, W. Global Prevalence of Type 2 Diabetes over the Next Ten Years (2018–2028). Diabetes 2018, 67, 202. [Google Scholar] [CrossRef]
- Yang, C.; Ding, Z.; Zhou, H.; Chen, D.; Huang, Z.H.; Yang, C.F.; Liu, S.G.; Li, Q.; You, Y.B.; Zhong, X.; et al. Prevalence of prediabetes by the fasting plasma glucose and HbA1c screening criteria among the children and adolescents of Shenzhen, China. J. Diabetes 2018. [Google Scholar] [CrossRef] [PubMed]
- Umapathi, K.K.; Thavamani, A.; Al-Kindi, S. Prediabetes in children and adolescents in the United States: Prevalence estimates and comorbidities—A population analysis. J. Pediatr. Endocrinol. Metab. 2019, 32, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Spurr, S.; Bally, J.; Hill, P.; Gray, K.; Newman, P.; Hutton, A. Exploring the Prevalence of Undiagnosed Prediabetes, Type 2 Diabetes Mellitus, and Risk Factors in Adolescents: A Systematic Review. J. Pediatr. Nurs. 2020, 50, 94–104. [Google Scholar] [CrossRef]
- Spurr, S.; Bally, J.; Bullin, C.; Allan, D.; McNair, E. The prevalence of undiagnosed Prediabetes/type 2 diabetes, prehypertension/hypertension and obesity among ethnic groups of adolescents in Western Canada. BMC Pediatr. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Chahkandi, T.; Taheri, F.; Bijari, B.; Kazemi, T.; Namakin, K.; Zardast, M. Prevalence of high normal FBS and prediabetes among adolescents in Birjand, East of Iran, 2012. J. Educ. Health Promot. 2015, 4, 68. [Google Scholar]
- Andes, L.J.; Cheng, Y.J.; Rolka, D.B.; Gregg, E.W.; Imperatore, G. Prevalence of Prediabetes Among Adolescents and Young Adults in the United States, 2005–2016. JAMA Pediatr. 2020, 174, e194498. [Google Scholar] [CrossRef]
- Al Amiri, E.; Abdullatif, M.; Abdulle, A.; Al Bitar, N.; Afandi, E.Z.; Parish, M.; Darwiche, G. The prevalence, risk factors, and screening measure for prediabetes and diabetes among Emirati overweight/obese children and adolescents. BMC Public Health 2015, 15, 1298. [Google Scholar] [CrossRef]
- Steffes, G.D.; Megura, A.E.; Adams, J.; Claytor, R.P.; Ward, R.M.; Horn, T.S.; Potteiger, J.A. Prevalence of metabolic syndrome risk factors in high school and NCAA division I football players. J. Strength Cond. Res. 2013, 27, 1749–1757. [Google Scholar] [CrossRef] [PubMed]
- Buell, J.L.; Calland, D.; Hanks, F.; Johnston, B.; Pester, B.; Sweeney, R.; Thorne, R. Presence of metabolic syndrome in football linemen. J. Athl. Train. 2008, 43, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Cook, S.; Weitzman, M.; Auinger, P.; Nguyen, M.; Dietz, W.H. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch. Pediatr. Adolesc. Med. 2003, 157, 821–827. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Gunnarsson, R.; Bjorkman, O.; Olsson, M.; Wahren, J. Effects of insulin on peripheral and splanchnic glucose metabolism in noninsulin-dependent (type II) diabetes mellitus. J. Clin. Investig. 1985, 76, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, M.; DeFronzo, R.A. Insulin sensitivity indices obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care 1999, 22, 1462–1470. [Google Scholar] [CrossRef] [PubMed]
- Richter, E.A.; Hargreaves, M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol. Rev. 2013, 93, 993–1017. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.J.; Richter, E.A. Skeletal muscle glucose uptake during exercise: How is it regulated? Physiology (Bethesda) 2005, 20, 260–270. [Google Scholar] [CrossRef]
- Richter, E.A.; Kiens, B.; Saltin, B.; Christensen, N.J.; Savard, G. Skeletal muscle glucose uptake during dynamic exercise in humans: Role of muscle mass. Am. J. Physiol. 1988, 254, E555–E561. [Google Scholar] [CrossRef]
- Moore, M.C.; Coate, K.C.; Winnick, J.J.; An, Z.; Cherrington, A.D. Regulation of hepatic glucose uptake and storage in vivo. Adv. Nutr. 2012, 3, 286–294. [Google Scholar] [CrossRef]
- Craig, B.W.; Everhart, J.; Brown, R. The influence of high-resistance training on glucose tolerance in young and elderly subjects. Mech. Ageing Dev. 1989, 49, 147–157. [Google Scholar] [CrossRef]
- Reed, M.E.; Ben-Ezra, V.; Biggerstaff, K.D.; Nichols, D.L. The effects of two bouts of high- and low-volume resistance exercise on glucose tolerance in normoglycemic women. J. Strength Cond. Res. 2012, 26, 251–260. [Google Scholar] [CrossRef]
- Hetrick, M.M.; Naquin, M.; Gillan, W.W.; Williams, B.M.; Kraemer, R.R. A Hydrothermally Processed Maize Starch and its Effects on Blood Glucose Levels During High Intensity Interval Exercise. J. Strength Cond. Res. 2018, 32, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Barillas, S.R.; Watkins, C.M.; Wong, M.A.; Dobbs, I.J.; Archer, D.C.; Munger, C.N.; Galpin, A.J.; Coburn, J.W.; Brown, L.E. Repeated Plyometric Exercise Attenuates Blood Glucose in Healthy Adults. Int. J. Exerc. Sci. 2017, 10, 1076–1084. [Google Scholar]
- Marliss, E.B.; Vranic, M. Intense exercise has unique effects on both insulin release and its roles in glucoregulation: Implications for diabetes. Diabetes 2002, 51 (Suppl. S1), S271–S283. [Google Scholar] [CrossRef] [PubMed]
- Hari, A.; Fealy, C.; Solomon, T.P.J.; Haus, J.M.; Kelly, K.R.; Barkoukis, H.; Kirwan, J.P. Exercise-induced improvements in glucose effectiveness are blunted by a high glycemic diet in adults with prediabetes. Acta Diabetol. 2019, 56, 211–217. [Google Scholar] [CrossRef]
- Coker, R.H.; Kjaer, M. Glucoregulation during exercise: The role of the neuroendocrine system. Sports Med. 2005, 35, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Winding, K.M.; Munch, G.W.; Iepsen, U.W.; Van Hall, G.; Pedersen, B.K.; Mortensen, S.P. The effect on glycaemic control of low-volume high-intensity interval training versus endurance training in individuals with type 2 diabetes. Diabetes Obes. Metab. 2018, 20, 1131–1139. [Google Scholar] [CrossRef]
- Barclay, A.W.; Petocz, P.; McMillan-Price, J.; Flood, V.M.; Prvan, T.; Mitchell, P.; Brand-Miller, J.C. Glycemic index, glycemic load, and chronic disease risk--a meta-analysis of observational studies. Am. J Clin. Nutr. 2008, 87, 627–637. [Google Scholar] [CrossRef]
- Heung-Sang Wong, S.; Sun, F.H.; Chen, Y.J.; Li, C.; Zhang, Y.J.; Ya-Jun Huang, W. Effect of pre-exercise carbohydrate diets with high vs low glycemic index on exercise performance: A meta-analysis. Nutr. Rev. 2017, 75, 327–338. [Google Scholar] [CrossRef]
- Forbes, S.C.; Candow, D.G.; Little, J.P.; Magnus, C.; Chilibeck, P.D. Effect of Red Bull energy drink on repeated Wingate cycle performance and bench-press muscle endurance. Int. J. Sport. Nutr. Exerc. Metab. 2007, 17, 433–444. [Google Scholar] [CrossRef]
- Astorino, T.A.; Matera, A.J.; Basinger, J.; Evans, M.; Schurman, T.; Marquez, R. Effects of red bull energy drink on repeated sprint performance in women athletes. Amino Acids 2012, 42, 1803–1808. [Google Scholar] [CrossRef]
- Duchan, E.; Patel, N.D.; Feucht, C. Energy drinks: A review of use and safety for athletes. Phys. Sportsmed. 2010, 38, 171–179. [Google Scholar] [CrossRef]
- Clauson, K.A.; Shields, K.M.; McQueen, C.E.; Persad, N. Safety issues associated with commercially available energy drinks. J. Am. Pharm. Assoc. 2008, 48, e55–e67. [Google Scholar] [CrossRef]
- Lime-Ma, F.; Cotter, J.A.; Schick, E.E. The Effect of Acute Hyperglycemia on Muscular Strength, Power and Endurance. Int. J. Exerc. Sci. 2017, 10, 390–396. [Google Scholar] [PubMed]
- American Diabetes Association. Standards of Medical Care in Diabetes-2016: Summary of Revisions. Diabetes Care 2016, 39 (Suppl. S1), S4–S5. [Google Scholar] [CrossRef] [PubMed]
- Haff, G.; Triplett, N.T. Essentials of Strength Training and Conditioning, 4th ed.; Human Kinetics: Champaign, IL, USA, 2016. [Google Scholar]
- American Diabetes Association. Erratum. Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes-2016. Diabetes Care 2016, 39 (Suppl. S1), S13–S22. [Google Scholar]
- Wilk, M.; Gepfert, M.; Krzysztofik, M.; Mostowik, A.; Filip, A.; Hajduk, G.; Zajac, A. Impact of Duration of Eccentric Movement in the One-Repetition Maximum Test Result in the Bench Press among Women. J. Sports Sci. Med. 2020, 19, 317–322. [Google Scholar]
- Bentley, J.R.; Amonette, W.E.; De Witt, J.K.; Hagan, R.D. Effects of different lifting cadences on ground reaction forces during the squat exercise. J. Strength Cond. Res. 2010, 24, 1414–1420. [Google Scholar] [CrossRef]
- Mukaka, M.M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Gordon, B.A.; Bird, S.R.; Macisaac, R.J.; Benson, A.C. Glycemic response varies between resistance and aerobic exercise in inactive males with long-term type 2 diabetes. Appl. Physiol. Nutr. Metab. 2013, 38, 900–904. [Google Scholar] [CrossRef]
- Chansky, M.E.; Corbett, J.G.; Cohen, E. Hyperglycemic emergencies in athletes. Clin. Sports Med. 2009, 28, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Manders, R.J.; van Dijk, J.W.; van Loon, L.J. Low-intensity exercise reduces the prevalence of hyperglycemia in type 2 diabetes. Med. Sci. Sports Exerc. 2010, 42, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.D.; Ruby, B.C.; Laskin, J.J.; Gaskill, S.E. Effects of high intensity/low volume and low intensity/high volume isokinetic resistance exercise on postexercise glucose tolerance. J. Strength Cond. Res. 2007, 21, 330–335. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jelleyman, C.; Yates, T.; O’Donovan, G.; Gray, L.J.; King, J.A.; Khunti, K.; Davies, M.J. The effects of high-intensity interval training on glucose regulation and insulin resistance: A meta-analysis. Obes. Rev. 2015, 16, 942–961. [Google Scholar] [CrossRef] [PubMed]
- Gillen, J.B.; Little, J.P.; Punthakee, Z.; Tarnopolsky, M.A.; Riddell, M.C.; Gibala, M.J. Acute high-intensity interval exercise reduces the postprandial glucose response and prevalence of hyperglycaemia in patients with type 2 diabetes. Diabetes Obes. Metab. 2012, 14, 575–577. [Google Scholar] [CrossRef]
- Praet, S.F.; Manders, R.J.; Lieverse, A.G.; Kuipers, H.; Stehouwer, C.D.; Keizer, H.A.; van Loon, L.J. Influence of acute exercise on hyperglycemia in insulin-treated type 2 diabetes. Med. Sci. Sports Exerc. 2006, 38, 2037–2044. [Google Scholar] [CrossRef]
- Way, K.L.; Hackett, D.A.; Baker, M.K.; Johnson, N.A. The Effect of Regular Exercise on Insulin Sensitivity in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Diabetes Metab. J. 2016, 40, 253–271. [Google Scholar] [CrossRef]
- Thomas, D.E.; Brotherhood, J.R.; Brand, J.C. Carbohydrate feeding before exercise: Effect of glycemic index. Int. J. Sports Med. 1991, 12, 180–186. [Google Scholar] [CrossRef]
- Wu, C.L.; Williams, C. A low glycemic index meal before exercise improves endurance running capacity in men. Int. J. Sport Nutr. Exerc. Metab. 2006, 16, 510–527. [Google Scholar] [CrossRef]
- Little, J.P.; Gillen, J.B.; Percival, M.E.; Safdar, A.; Tarnopolsky, M.A.; Punthakee, Z.; Jung, M.E.; Gibala, M.J. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J. Appl. Physiol. 2011, 111, 1554–1560. [Google Scholar] [CrossRef]
| Descriptive | Mean ± Std. Deviation |
|---|---|
| Age (yrs.) | 23.43 ± 2.18 |
| Height (cm) | 175.16 ± 10.44 |
| Weight (kg) | 77.02 ± 8.91 |
| 1-RM BHSQ (kg) | 116.23 ± 26.25 |
| 1-RM BP (kg) | 99.17 ± 17.63 |
| Lean Mass Total (kg) | 59.55 ± 7.09 |
| Body Fat (%) | 20 ± 0.03 |
| HbA1c | 5.15 ± 0.17 |
| Fasting Insulin (pmol∙L−1) | 68.51 ± 19.41 |
| Condition | Oral Glucose Dosage | RE Performed 30-min Following Oral Glucose Ingestion |
|---|---|---|
| CON | 2 g/kg BW | None |
| MO | 2 g/kg BW | 3 sets, 14 reps @ 65% 1-RM |
| HI | 2 g/kg BW | 5 sets, 4 reps @ 90% 1-RM |
| Plasma Glucose | Mean ± Std Deviation (mmol∙L−1) |
|---|---|
| Fasting | 5.6 ± 0.42 |
| CON 2-hr | 7.1 ± 1.3 * |
| MO 2-hr | 7.5 ± 0.6 * |
| HI 2-hr | 8.2 ± 1.9 *,† |
| Condition | Volume Load Mean ± Std. Deviation |
|---|---|
| HI BHSQ | 2111.89 ± 452.12 |
| HI BP | 1776.22 ± 264.38 |
| MO BHSQ | 2251.75 ± 462.40 |
| MO BP | 1894.41 ± 470.98 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schick, E.E.; Segura, L.E.; Emamjomeh, S.; Cotter, J.A. The Effect of Resistance Exercise Intensity on Acute Hyperglycemia in Young Adult Males. Sports 2020, 8, 121. https://doi.org/10.3390/sports8090121
Schick EE, Segura LE, Emamjomeh S, Cotter JA. The Effect of Resistance Exercise Intensity on Acute Hyperglycemia in Young Adult Males. Sports. 2020; 8(9):121. https://doi.org/10.3390/sports8090121
Chicago/Turabian StyleSchick, Evan E., Luis E. Segura, Shayán Emamjomeh, and Joshua A. Cotter. 2020. "The Effect of Resistance Exercise Intensity on Acute Hyperglycemia in Young Adult Males" Sports 8, no. 9: 121. https://doi.org/10.3390/sports8090121
APA StyleSchick, E. E., Segura, L. E., Emamjomeh, S., & Cotter, J. A. (2020). The Effect of Resistance Exercise Intensity on Acute Hyperglycemia in Young Adult Males. Sports, 8(9), 121. https://doi.org/10.3390/sports8090121






