ZumBeat: Evaluation of a Zumba Dance Intervention in Postmenopausal Overweight Women
Abstract
:1. Introduction
2. Materials and Methods
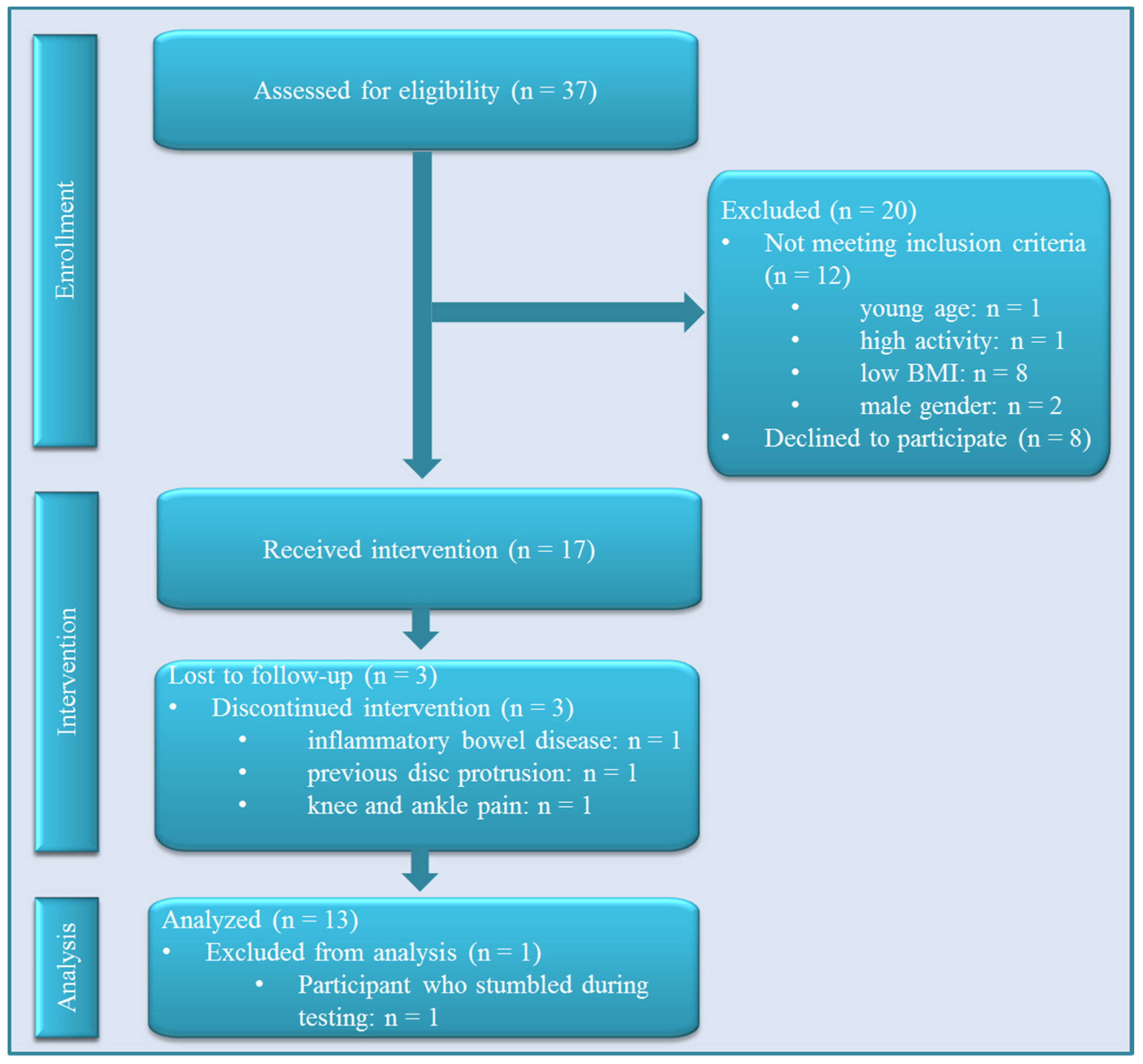
2.1. Study Design
2.2. Participants
2.3. Measurements
2.4. Exercise Testing
2.5. Dance Intervention
2.6. Statistical Analyses
2.7. Power Calculation
3. Results
3.1. Participant Characteristics
| Characteristic | All Participants (n = 17) |
|---|---|
| Female sex, n | 17 |
| Age, years | 55 (6) |
| Height, cm | 167 (9) |
| Weight, kg | 85 (79, 94) |
| BMI, kg/m2 | 30 (29, 33) |
| Waist circumference, cm | 103 (102, 114) |
| Percent body fat, % | 39 (8) |
| Visceral fat mass 1, cm2 | 130 (118, 156) |
| Systolic blood pressure 2, mmHg | 126 (12) |
| Diastolic blood pressure 2, mmHg | 80 (10) |
| Smoking, n | – |
| Non-smoker | 13 |
| Ex-smoker | 3 |
| Current smoker | 1 |
3.2. Training Completion and Intensity

3.3. Effect of the Intervention on Cardiorespiratory Fitness

| Parameter | N 1 | Intervention (n = 17) | Change from Baseline (95% CI) | p-Value | Cohen’s d | |
|---|---|---|---|---|---|---|
| Baseline (Mean (SD)) | Follow-up (Mean (SD)) | |||||
| VO2peak, mL/kg/min | 13 | 24.3 (2.9) | 23.9 (3.2) | −0.5 (−1.0, 0.1) | 0.114 | –0.47 |
| HRmax, bpm | 12 | 161.8 (15.5) | 164.5 (17.0) | 2.7 (−2.8, 8.1) | 0.305 | 0.31 |
| Anthropometry | ||||||
| Weight, kg | 14 | 91.0 (13.1) | 90.4 (11.6) | −0.6 (−2.4, 1.3) | 0.509 | –0.18 |
| BMI, kg/m2 | 14 | 32.7 (4.9) | 32.5 (4.2) | −0.2 (−0.9, 0.4) | 0.444 | –0.21 |
| Waist circumference, cm | 14 | 108.8 (9.2) | 107.2 (8.5) | −1.6 (−3.3, 0.2) | 0.072 | –0.52 |
| Percent body fat, % | 14 | 39.5 (8.2) | 38.1 (7.4) | −1.3 (−3.6, 0.9) | 0.210 | –0.35 |
| Fat mass, kg | 14 | 36.1 (10.2) | 34.7 (9.0) | −1.4 (−3.7, 0.9) | 0.200 | –0.36 |
| Visceral fat mass, cm2 | 13 | 140.7 (25.6) | 138.4 (27.1) | −2.2 (−9.6, 5.1) | 0.523 | –0.18 |
| Muscle mass, kg | 14 | 30.3 (5.3) | 31.0 (5.0) | 0.7 (−0.3, 1.7) | 0.162 | 0.40 |
| Cardiovascular parameters | ||||||
| SBP, mmHg | 12 | 126.6 (14.2) | 131.0 (12.3) | 4.4 (−1.4, 10.2) | 0.124 | 0.48 |
| DBP, mmHg | 12 | 80.4 (9.9) | 83.3 (9.8) | 2.9 (−1.2, 6.9) | 0.146 | 0.45 |
| Resting heart rate, bpm | 13 | 63.5 (7.5) | 62.3 (6.5) | −1.2 (−5.5, 3.2) | 0.578 | –0.16 |
3.4. Effect of the Intervention on Anthropometric Parameters
3.5. Effect of the Intervention on Psychometric Parameters
3.5.1. Quality of Life
| Questionnaire | N 1 | Intervention (n = 17) | Change from Baseline (95% CI) | p-Value | Cohen’s d | +/− 2 | Norm 3 | |
|---|---|---|---|---|---|---|---|---|
| Baseline (Mean (SD)) | Follow-up (Mean (SD)) | |||||||
| IWQOL (0–100) | 14 | − | − | − | − | − | − | − |
| Total score | − | 79.4 (17.2) | 88.7 (8.8) | 9.2 (1.6, 16.8) | 0.022 | 0.70 | + | 91.8 |
| Physical function | − | 75.5 (17.9) | 83.6 (13.3) | 8.1 (−1.2, 17.4) | 0.082 | 0.50 | + | 90.0 |
| Self-esteem | − | 68.1 (29.0) | 83.7 (19.5) | 15.6 (2.8, 28.4) | 0.021 | 0.70 | + | 87.5 |
| Sexual life | − | 86.2 (25.4) | 92.9 (18.2) | 6.7 (−2.0, 15.3) | 0.119 | 0.45 | + | 95.1 |
| Public distress | − | 91.9 (14.7) | 96.1 (5.3) | 4.2 (−2.3, 10.7) | 0.189 | 0.37 | + | 96.5 |
| Work | − | 87.5 (18.0) | 97.8 (5.2) | 10.3 (0.1, 20.4) | 0.048 | 0.58 | + | 95.4 |
| SBB (0 to 4) | 14 | 2.5 (0.5) | 2.1 (0.6) | −0.4 (−0.7, −0.2) | 0.001 | −1.09 | + | 2.2 |
| MRS(0 to 44) | 14 | 11.9 (7.6) | 9.5 (7.1) | −2.4 (−4.6, −0.2) | 0.036 | −0.62 | + | 8.8 |
| BDI (0 to 63) | 14 | 7.2 (7.8) | 4.8 (5.3) | −2.4 (−5.6, 0.7) | 0.118 | −0.45 | + | 7.7 |
| ISR (0 to 4) | 14 | 0.5 (0.5) | 0.4 (0.4) | −0.1 (−0.2, 0.0) | 0.216 | −0.35 | + | 0.4 |
| I-8 (0 to 4) | 14 | − | − | − | − | − | − | − |
| Urgency | − | 2.3 (0.6) | 2.2 (0.8) | −0.1 (−0.4, 0.1) | 0.314 | −0.28 | + | 2.5 |
| Intention | − | 3.6 (1.0) | 4.0 (0.6) | 0.4 (−0.1, 0.9) | 0.094 | 0.48 | + | 3.8 |
| Endurance | − | 4.1 (0.6) | 3.9 (0.9) | −0.2 (−0.6, 0.2) | 0.254 | −0.32 | − | 4.3 |
| Risk | − | 3.6 (0.8) | 3.2 (0.8) | −0.4 (−0.9, 0.2) | 0.156 | −0.40 | + | 2.8 |
| FEV | 14 | − | − | − | − | − | − | − |
| Dietary restraint (0 to 21) | − | 9.1 (3.8) | 9.8 (4.4) | 0.7 (−2.0, 3.4) | 0.582 | 0.15 | + | 8.2 |
| Disinhibition (0 to 16) | − | 8.2 (3.6) | 7.1 (3.2) | −1.1 (−2.5, 0.4) | 0.132 | −0.43 | + | 7.1 |
| Hunger (0 to 14) | − | 7.2 (3.8) | 5.0 (3.7) | −2.2 (−4.2, −0.3) | 0.028 | −0.66 | + | 5.7 |
3.5.2. Menopausal Symptoms
3.5.3. Sports-Related Barriers
3.5.4. Psychiatric Symptoms
3.5.5. Impulsivity and Eating Behavior
3.6. Sensitivity Analyses
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lentz, G.M.; Lobo, R.A.; Gershenson, D.M.; Katz, V.L. Comprehensive Gynecology: Expert Consult Online and Print, 6th ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2012; pp. 273–299. [Google Scholar]
- Lobo, R.A.; Davis, S.R.; de Villiers, T.J.; Gompel, A.; Henderson, V.W.; Hodis, H.N.; Lumsden, M.A.; Mack, W.J.; Shapiro, S.; Baber, R.J. Prevention of diseases after menopause. Climacteric 2014, 17, 540–556. [Google Scholar] [CrossRef] [PubMed]
- Al-Safi, Z.A.; Polotsky, A.J. Obesity and menopause. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 29, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Lovejoy, J.C. Weight gain in women at midlife: The influence of menopause. Obes. Manag. 2009, 5, 52–56. [Google Scholar] [CrossRef]
- Duval, K.; Prud’homme, D.; Rabasa-Lhoret, R.; Strychar, I.; Brochu, M.; Lavoie, J.M.; Doucet, E. Effects of the menopausal transition on energy expenditure: A monet group study. Eur. J. Clin. Nutr. 2013, 67, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Lovejoy, J.C.; Champagne, C.M.; de Jonge, L.; Xie, H.; Smith, S.R. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int. J. Obes. Lond. 2008, 32, 949–958. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Norman, I.J.; While, A.E. Physical activity in older people: A systematic review. BMC Public Health 2013, 13, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Sui, X.; Zhang, J.; Lee, D.C.; Church, T.S.; Lu, W.; Liu, J.; Blair, S.N. Physical activity/fitness peaks during perimenopause and bmi change patterns are not associated with baseline activity/fitness in women: A longitudinal study with a median 7-year follow-up. Br. J. Sports Med. 2013, 47, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Chomistek, A.K.; Manson, J.E.; Stefanick, M.L.; Lu, B.; Sands-Lincoln, M.; Going, S.B.; Garcia, L.; Allison, M.A.; Sims, S.T.; LaMonte, M.J.; et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: Results from the women’s health initiative. J. Am. Coll. Cardiol. 2013, 61, 2346–2354. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- McArthur, D.; Dumas, A.; Woodend, K.; Beach, S.; Stacey, D. Factors influencing adherence to regular exercise in middle-aged women: A qualitative study to inform clinical practice. BMC Womens Health 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Bruner, B.; Chad, K. Physical activity attitudes, beliefs, and practices among women in a woodland cree community. J. Phys. Act. Health 2013, 10, 1119–1127. [Google Scholar] [PubMed]
- Im, E.O.; Lee, B.; Chee, W.; Stuifbergen, A. eMAPA Research Team. Attitudes toward physical activity of white midlife women. J. Obstet. Gynecol. Neonatal Nurs. 2011, 40, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.X.; Kowaleski-Jones, L.; Wen, M. Walking or dancing: Patterns of physical activity by cross-sectional age among u.S. Women. J. Aging Health 2013, 25, 1182–1203. [Google Scholar] [CrossRef] [PubMed]
- Kattenstroth, J.C.; Kalisch, T.; Holt, S.; Tegenthoff, M.; Dinse, H.R. Six months of dance intervention enhances postural, sensorimotor, and cognitive performance in elderly without affecting cardio-respiratory functions. Front. Aging Neurosci. 2013, 5. [Google Scholar] [CrossRef] [PubMed]
- Belardinelli, R. Exercise training in chronic heart failure: How to harmonize oxidative stress, sympathetic outflow, and angiotensin II. Circulation 2007, 115, 3042–3044. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, M.; Ahn, Y.B.; Lim, H.K.; Kang, S.G.; Cho, J.H.; Park, S.J.; Song, S.W. Effect of dance exercise on cognitive function in elderly patients with metabolic syndrome: A pilot study. J. Sports Sci. Med. 2011, 10, 671–678. [Google Scholar] [PubMed]
- Shimamoto, H.; Adachi, Y.; Takahashi, M.; Tanaka, K. Low impact aerobic dance as a useful exercise mode for reducing body mass in mildly obese middle-aged women. Appl. Hum. Sci. 1998, 17, 109–114. [Google Scholar] [CrossRef]
- Murrock, C.J.; Graor, C.H. The effects of dance on depression, physical function, and disability in underserved adults. J Aging Phys Act 2014, 22, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Coubard, O.A.; Duretz, S.; Lefebvre, V.; Lapalus, P.; Ferrufino, L. Practice of contemporary dance improves cognitive flexibility in aging. Front. Aging Neurosci. 2011, 3. [Google Scholar] [CrossRef] [PubMed]
- Duberg, A.; Hagberg, L.; Sunvisson, H.; Moller, M. Influencing self-rated health among adolescent girls with dance intervention: A randomized controlled trial. JAMA Pediatr. 2013, 167, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Gillett, P.A.; Eisenman, P.A. The effect of intensity controlled aerobic dance exercise on aerobic capacity of middle-aged, overweight women. Res. Nurs. Health 1987, 10, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Murrock, C.J.; Gary, F.A. Culturally specific dance to reduce obesity in african american women. Health Promot. Pract. 2010, 11, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Gullu, E.; Gullu, A.; Cicek, G.; Yamaner, F.; Imamoglu, O.; Gumusdag, H. The effects of aerobic exercises on cardiovascular risk factors of sedentary women. Int. J. Acad. Res. 2013, 5, 160–167. [Google Scholar] [CrossRef]
- Okura, T.; Nakata, Y.; Ohkawara, K.; Numao, S.; Katayama, Y.; Matsuo, T.; Tanaka, K. Effects of aerobic exercise on metabolic syndrome improvement in response to weight reduction. Obesity 2007, 15, 2478–2484. [Google Scholar] [CrossRef] [PubMed]
- Mosher, P.E.; Ferguson, M.A.; Arnold, R.O. Lipid and lipoprotein changes in premenstrual women following step aerobic dance training. Int. J. Sports Med. 2005, 26, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Williford, H.N.; Blessing, D.L.; Barksdale, J.M.; Smith, F.H. The effects of aerobic dance training on serum lipids, lipoproteins and cardiopulmonary function. J. Sports Med. Phys. Fit. 1988, 28, 151–157. [Google Scholar]
- Thomson, W.R. Worldwide survey of fitness trends for 2013. ACSMs Health Fit. J. 2012, 16, 8–17. [Google Scholar]
- Luettgen, M.; Foster, C.; Doberstein, S.; Mikat, R.; Porcari, J. Zumba(®): Is the “fitness-party” a good workout? J. Sports Sci. Med. 2012, 11, 357–358. [Google Scholar] [PubMed]
- Otto, R.M.; Maniguet, E.; Peters, A.; Boutagy, N.; Gabbard, A.; Wygand, J.W.; Yoke, M. The Energy Cost of Zumba Exercise. Med. Sci. Sports Exerc. 2011, 43. [Google Scholar] [CrossRef]
- Bennett, P.; Corradini, A.; Ockerby, C.; Cossich, T. Exercise during hemodialysis the intradialytic Zumba Gold. Nephrol. News Issues 2012, 26, 31–32. [Google Scholar] [PubMed]
- Sanders, M.E.; Prouty, J. Zumba® fitness is gold for all ages. Acsms Health Fit. J. 2012, 16, 25–28. [Google Scholar]
- Inouye, J.; Nichols, A.; Maskarinec, G.; Tseng, C.W. A survey of musculoskeletal injuries associated with zumba. Hawaii J. Med. Public Health 2013, 72, 433–436. [Google Scholar] [PubMed]
- Schrimpf, C.; Haastert-Talini, K.; von Falck, C.; Rustum, S.; Wilhelmi, M.; Teebken, O.E. High sport sneakers may lead to peripheral artery occlusion in Zumba® dancers. Vasa 2014, 43, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Donath, L.; Roth, R.; Hohn, Y.; Zahner, L.; Faude, O. The effects of zumba training on cardiovascular and neuromuscular function in female college students. Eur. J. Sport Sci. 2014, 14, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Barene, S.; Krustrup, P.; Brekke, O.L.; Holtermann, A. Soccer and Zumba as health-promoting activities among female hospital employees: A 40-weeks cluster randomised intervention study. J. Sports Sci. 2014, 32, 1539–1549. [Google Scholar] [CrossRef] [PubMed]
- Barene, S.; Krustrup, P.; Holtermann, A. Effects of the workplace health promotion activities soccer and Zumba on muscle pain, work ability and perceived physical exertion among female hospital employees. PLoS ONE 2014, 9, e115059. [Google Scholar] [CrossRef] [PubMed]
- Barene, S.; Krustrup, P.; Jackman, S.R.; Brekke, O.L.; Holtermann, A. Do soccer and Zumba exercise improve fitness and indicators of health among female hospital employees? A 12-week rct. Scand. J. Med. Sci. Sports 2014, 24, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Araneta, M.R.; Tanori, D. Benefits of zumba fitness among sedentary adults with components of the metabolic syndrome: A pilot study. J. Sports Med. Phys. Fit. 2015, 55, 1227–1233. [Google Scholar]
- Krishnan, S.; Tokar, T.N.; Boylan, M.M.; Griffin, K.; Feng, D.; McMurry, L.; Esperat, C.; Cooper, J.A. Zumba® dance improves health in overweight/obese or type 2 diabetic women. Am. J. Health Behav. 2015, 39, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Delextrat, A.A.; Warner, S.; Graham, S.; Neupert, E. An 8-week exercise intervention based on Zumba® improves aerobic fitness and psychological well-being in healthy women. J. Phys. Act. Health 2015. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.J.; Pieper, C.F.; Morey, M.C. Accuracy of VO2(max) prediction equations in older adults. Med. Sci. Sports Exerc. 2003, 35, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Borg, G. Perceived exertion as an indicator of somatic stress. Scand. J. Rehabil. Med. 1970, 2, 92–98. [Google Scholar] [PubMed]
- Dalle Grave, R.; Calugi, S.; Centis, E.; El Ghoch, M.; Marchesini, G. Cognitive-behavioral strategies to increase the adherence to exercise in the management of obesity. J. Obes. 2011, 2011, 348293. [Google Scholar] [CrossRef] [PubMed]
- Woodard, C.M.; Berry, M.J. Enhancing adherence to prescribed exercise: Structured behavioral interventions in clinical exercise programs. J. Cardiopulm. Rehabil. 2001, 21, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Carels, R.A.; Darby, L.A.; Rydin, S.; Douglass, O.M.; Cacciapaglia, H.M.; O’Brien, W.H. The relationship between self-monitoring, outcome expectancies, difficulties with eating and exercise, and physical activity and weight loss treatment outcomes. Ann. Behav. Med. 2005, 30, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, D. Lattice: Multivariate Data Visualization with R; Springer: New York, NY, USA, 2008; p. 265. [Google Scholar]
- Garber, C.E.; McKinney, J.S.; Carleton, R.A. Is aerobic dance an effective alternative to walk-jog exercise training? J. Sports Med. Phys. Fit. 1992, 32, 136–141. [Google Scholar]
- Leelarungrayub, D.; Saidee, K.; Pothongsunun, P.; Pratanaphon, S.; YanKai, A.; Bloomer, R.J. Six weeks of aerobic dance exercise improves blood oxidative stress status and increases interleukin-2 in previously sedentary women. J. Bodyw. Mov. Ther. 2011, 15, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.C.; Sui, X.; Artero, E.G.; Lee, I.M.; Church, T.S.; McAuley, P.A.; Stanford, F.C.; Kohl, H.W., 3rd; Blair, S.N. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: The aerobics center longitudinal study. Circulation 2011, 124, 2483–2490. [Google Scholar] [CrossRef] [PubMed]
- Kolotkin, R.L.; Crosby, R.D. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (iwqol-lite) in a community sample. Qual. Life Res. 2002, 11, 157–171. [Google Scholar] [CrossRef] [PubMed]
- Potthoff, P.; Heinemann, L.A.; Schneider, H.P.; Rosemeier, H.P.; Hauser, G.A. [The menopause rating scale (MRS II): Methodological standardization in the German population]. Zentralbl. Gynakol. 2000, 122, 280–286. [Google Scholar] [PubMed]
- Krämer, L.; Fuchs, R. Barrieren und Barrierenmanagement im Prozess der Sportteilnahme. Zwei neue Messinstrumente. Z. Gesundheitspsychol. 2010, 18, 170–182. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Ball, R.; Ranieri, W. Comparison of beck depression inventories -ia and -ii in psychiatric outpatients. J. Pers. Assess. 1996, 67, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Tritt, K.; von Heymann, F.; Zaudig, M.; Zacharias, I.; Sollner, W.; Loew, T. [Development of the “Icd-10-Symptom-Rating”(ISR) questionnaire]. Z. Psychosom. Med. Psychother. 2008, 54, 409–418. [Google Scholar] [PubMed]
- Kovaleva, A.; Beierlein, C.; Schmitt, M.; Kemper, C.J. Eine Kurzskala zur Messung von Impulsivität nach dem UPPSs-Ansatz: Die Skala impulsives Verhalten (I-8). In GESIS Working Papers; GESIS: Köln, Geramny, 2012; Volume 20. [Google Scholar]
- Pudel, D.; Westenhöfer, J. Fragebogen zum Essverhalten (FEV), Handanweisung; Hogrefe: Göttingen, Geramny, 1989. [Google Scholar]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new medical research council guidance. Int. J. Nurs. Stud. 2013, 50, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Dalleck, L.C.; Roos, K.A.; Byrd, B.R.; Weatherwax, R.M. Zumba Gold(®): Are the physiological responses sufficient to improve fitness in middle-age to older adults? J. Sports Sci. Med. 2015, 14, 689–690. [Google Scholar] [PubMed]
- Scharhag-Rosenberger, F.; Walitzek, S.; Kindermann, W.; Meyer, T. Differences in adaptations to 1 year of aerobic endurance training: Individual patterns of nonresponse. Scand. J. Med. Sci. Sports 2012, 22, 113–118. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine. Acsm’s Guidelines for Exercise Testing and Prescription, 8th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010; p. 380. [Google Scholar]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. American college of sports medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Delextrat, A.; Neupert, E. Physiological load associated with a Zumba fitness workout: A comparison pilot study between classes and a DVD. J. Sports Sci. 2015, 34, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cugusi, L.; Wilson, B.; Serpe, R.; Medda, A.; Deidda, M.; Gabba, S.; Satta, G.; Chiappori, P.; Mercuro, G. Cardiovascular effects, body composition, quality of life and pain after a Zumba® fitness program in italian overweight women. J. Sports Med. Phys. Fit. 2015. epub ahead of print. [Google Scholar]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martin, B.W.; Lancet Physical Activity Series Working, G. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Wilbur, J.; Vassalo, A.; Chandler, P.; McDevitt, J.; Miller, A.M. Midlife women’s adherence to home-based walking during maintenance. Nurs. Res. 2005, 54, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, K.; Ruebig, A.; Potthoff, P.; Schneider, H.P.; Strelow, F.; Heinemann, L.A.; Do, M.T. The menopause rating scale (MRS) scale: A methodological review. Health Qual. Life Outcomes 2004, 2, 1–8. [Google Scholar]
- Anderson, R.J.; Freedland, K.E.; Clouse, R.E.; Lustman, P.J. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care 2001, 24, 1069–1078. [Google Scholar] [CrossRef] [PubMed]
- Violante, R.; Santoro, S.; Gonzalez, C. [Prevalence of depression and anxiety in a cohort of 761 obese patients: Impact in adherence to therapy and its outcome]. Vertex 2011, 22, 85–93. [Google Scholar] [PubMed]
- Zeman, M.; Jirak, R.; Zak, A.; Jachymova, M.; Vecka, M.; Tvrzicka, E.; Stankova, B.; Dusejovska, M. Metabolic syndrome and depression—Clinical relations. Cas. Lek. Cesk. 2008, 147, 75–80. [Google Scholar] [PubMed]
- Almeida, O.P.; Calver, J.; Jamrozik, K.; Hankey, G.J.; Flicker, L. Obesity and metabolic syndrome increase the risk of incident depression in older men: The health in men study. Am. J. Geriatr. Psychiatry 2009, 17, 889–898. [Google Scholar] [CrossRef] [PubMed]
- Schag, K.; Schonleber, J.; Teufel, M.; Zipfel, S.; Giel, K.E. Food-related impulsivity in obesity and binge eating disorder—A systematic review. Obes. Rev. 2013, 14, 477–495. [Google Scholar] [CrossRef] [PubMed]
- Pendleton, V.R.; Goodrick, G.K.; Poston, W.S.; Reeves, R.S.; Foreyt, J.P. Exercise augments the effects of cognitive-behavioral therapy in the treatment of binge eating. Int. J. Eat. Disord. 2002, 31, 172–184. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossmeissl, A.; Lenk, S.; Hanssen, H.; Donath, L.; Schmidt-Trucksäss, A.; Schäfer, J. ZumBeat: Evaluation of a Zumba Dance Intervention in Postmenopausal Overweight Women. Sports 2016, 4, 5. https://doi.org/10.3390/sports4010005
Rossmeissl A, Lenk S, Hanssen H, Donath L, Schmidt-Trucksäss A, Schäfer J. ZumBeat: Evaluation of a Zumba Dance Intervention in Postmenopausal Overweight Women. Sports. 2016; 4(1):5. https://doi.org/10.3390/sports4010005
Chicago/Turabian StyleRossmeissl, Anja, Soraya Lenk, Henner Hanssen, Lars Donath, Arno Schmidt-Trucksäss, and Juliane Schäfer. 2016. "ZumBeat: Evaluation of a Zumba Dance Intervention in Postmenopausal Overweight Women" Sports 4, no. 1: 5. https://doi.org/10.3390/sports4010005
APA StyleRossmeissl, A., Lenk, S., Hanssen, H., Donath, L., Schmidt-Trucksäss, A., & Schäfer, J. (2016). ZumBeat: Evaluation of a Zumba Dance Intervention in Postmenopausal Overweight Women. Sports, 4(1), 5. https://doi.org/10.3390/sports4010005









