Reliability of a Musculoskeletal Assessment for the Examination of Cervical Spine Pain and Injuries in Special Forces Combat Soldiers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
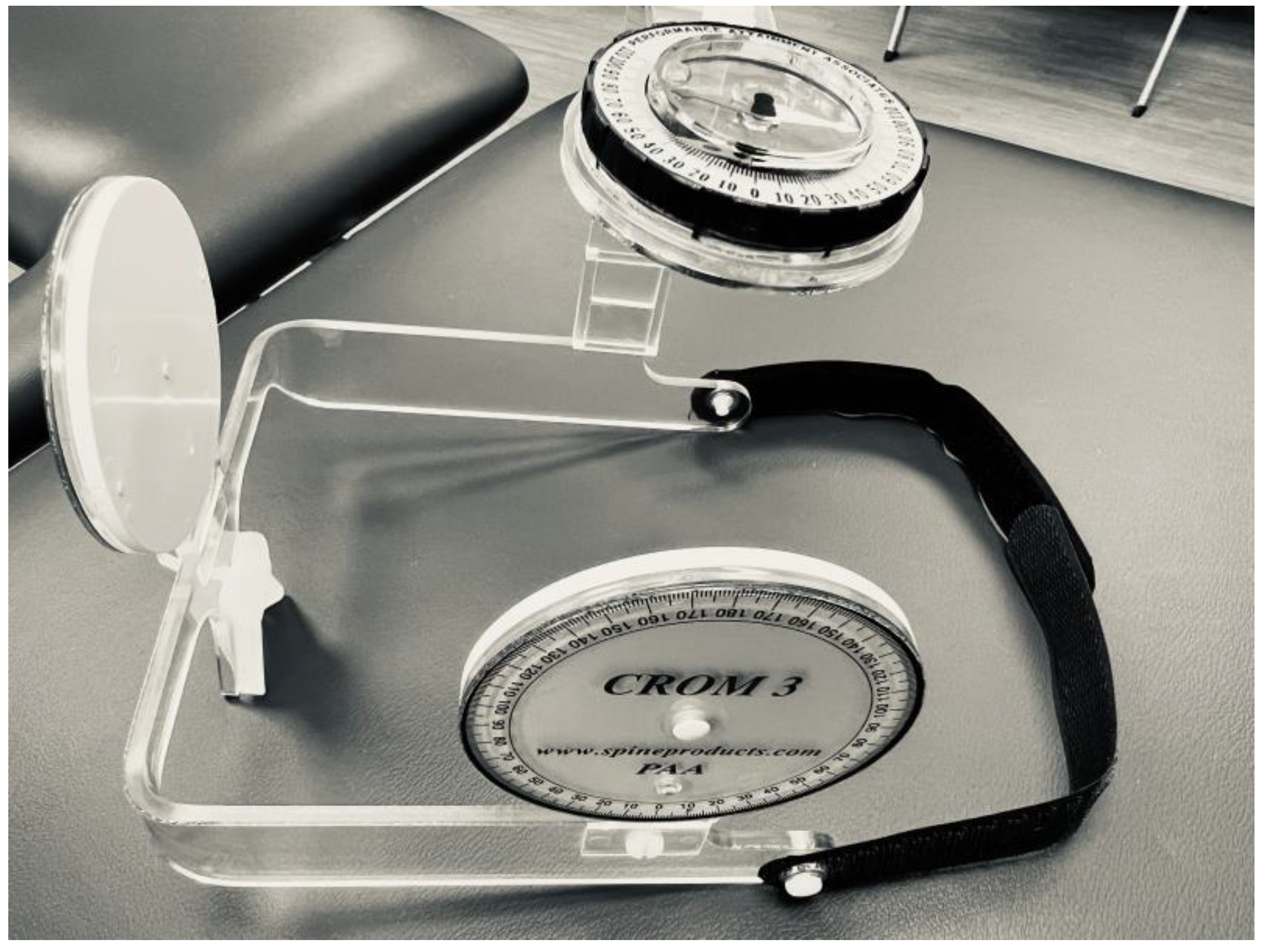
2.2. Instrumentation
2.3. Protocol Development
- Specific verbal cues during data collection such as “Ready, Set, Go, 3, 2, 1, relax”;
- Positioning of the participant during testing, such as lowering the examination table to its lowest position to maximize the tester’s mechanical advantage to resist cervical flexion and extension;
- Guidelines for placement of the HHD pad during testing;
- The decision to perform CAROM before strength testing to ensure that strength testing would not impact CAROM testing due to concerns about the potential for pain provocation;
- Verbal cues for the participant during CAROM to ensure the proper start position before each CAROM repetition/trial.
2.4. Procedures
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jones, B.H.; Hansen, B.C. An armed forces epidemiological board evaluation of injuries in the military. Am. J. Prev. Med. 2000, 18, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.H.; Canham-Chervak, M.; Canada, S.; Mitchener, T.A.; Moore, S. Medical surveillance of injuries in the U.S. Military descriptive epidemiology and recommendations for improvement. Am. J. Prev. Med. 2010, 38, S42–S60. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P.; Brown, C.; Kurihara, C.; Plunkett, A.; Nguyen, C.; Strassels, S.A. Diagnoses and factors associated with medical evacuation and return to duty for service members participating in Operation Iraqi Freedom or Operation Enduring Freedom: A prospective cohort study. Lancet 2010, 375, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P.; Gallagher, R.M.; Davis, S.A.; Griffith, S.R.; Carragee, E.J. Spine-area pain in military personnel: A review of epidemiology, etiology, diagnosis, and treatment. Spine J. 2012, 12, 833–842. [Google Scholar] [CrossRef]
- Amoroso, P.J.; Bell, N.S.; Toboni, H.; Krautheim, M. A Baseline Historical Analysis of Neck and Back-Related Morbidity in the U.S. Army: Occupational Risks Potentially Related to Head-Supported Mass; U.S. Army Research Institute of Environmental Medicine: Natick, MA, USA, 2005. [Google Scholar]
- Ang, A.H.; Goh, Y.H. Idiopathic submandibular sialoceles in the neck. Otolaryngol. Head Neck Surg. 2005, 132, 517–519. [Google Scholar] [CrossRef]
- Olivier, P.E.; Du Toit, D.E. Isokinetic neck strength profile of senior elite rugby union players. J. Sci. Med. Sport 2008, 11, 96–105. [Google Scholar] [CrossRef]
- Salmon, D.M.; Harrison, M.F.; Neary, J.P. Neck pain in military helicopter aircrew and the role of exercise therapy. Aviat. Space Environ. Med. 2011, 82, 978–987. [Google Scholar] [CrossRef]
- van den Oord, M.H.; De Loose, V.; Meeuwsen, T.; Sluiter, J.K.; Frings-Dresen, M.H. Neck pain in military helicopter pilots: Prevalence and associated factors. Mil. Med. 2010, 175, 55–60. [Google Scholar] [CrossRef]
- Abt, J.P.; Sell, T.C.; Lovalekar, M.T.; Keenan, K.A.; Bozich, A.J.; Morgan, J.S.; Kane, S.F.; Benson, P.J.; Lephart, S.M. Injury epidemiology of U.S. Army Special Operations Forces. Mil. Med. 2014, 179, 1106–1112. [Google Scholar] [CrossRef]
- Estep, P.N.; Bonts, E.G.; Shivers, B.L.; Wurzbach, J.M.; Novotny, B.L.; Rybarczyk, K.; Chancey, V.C. Mass Properties Comparison of Dismounted and Ground-Mounted Head-Supported Mass Configurations to Existing Performance and Acute Injury Risk Guidelines. Mil. Med. 2019, 184, 245–250. [Google Scholar] [CrossRef]
- Songer, T.J.; LaPorte, R.E. Disabilities due to injury in the military. Am. J. Prev. Med. 2000, 18, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Litow, F.K.; Krahl, P.L. Public health potential of a disability tracking system: Analysis of U.S. Navy and Marine Corps Physical Evaluation Boards 2005–2006. Mil. Med. 2007, 12, 1270–1274. [Google Scholar] [CrossRef] [PubMed]
- Lauder, T.D.; Baker, S.P.; Smith, G.S.; Lincoln, A.E. Sports and physical training injury hospitalizations in the army. Am. J. Prev. Med. 2000, 18, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Popovich, R.M.; Gardner, J.W.; Potter, R.; Knapik, J.J.; Jones, B.H. Effect of rest from running on overuse injuries in army basic training. Am. J. Prev. Med. 2000, 18, 147–155. [Google Scholar] [CrossRef]
- Kelley, P.W. ; United States. Deptartment of the Army. Office of the Surgeon General. Military Preventive Medicine: Mobilization and Deployment; Borden Institute, Walter Reed Army Medical Center: Washington, DC, USA, 2003. [Google Scholar]
- Burnett, A.F.; Naumann, F.L.; Price, R.S.; Sanders, R.H. A comparison of training methods to increase neck muscle strength. Work 2005, 25, 205–210. [Google Scholar]
- Chayrez, S.E.; Acevedo, A.; Blake, J.; Parrott, C.; Gerking, T.; Guthmann, D.; Jilek, M.; Dorcheus, J.; Zeigler, Z.; Copeland, C.; et al. Performance Optimization and Injury Mitigation for Air Force Student Fighter Pilots. Mil. Med. 2024, 189, 465–470. [Google Scholar] [CrossRef]
- Nagai, T.; Abt, J.P.; Sell, T.C.; Clark, N.C.; Smalley, B.W.; Wirt, M.D.; Lephart, S.M. Neck proprioception, strength, flexibility, and posture in pilots with and without neck pain history. Aviat. Space Environ. Med. 2014, 85, 529–535. [Google Scholar] [CrossRef]
- Nagai, T.; Keenan, K.A.; Abt, J.P.; Sell, T.C.; Smalley, B.W.; Wirt, M.D.; Lephart, S.M. Effects of Flight-Exposure and Age on Cervical and Trunk Musculoskeletal Characteristics in Army Helicopter Pilots. Int. J. Aeronaut. Sci. Aerosp. Res. 2016, 3, 123–130. [Google Scholar]
- Eagle, S.R.; Nagai, T.; Morgan, P.; Hendershot, R.; Sell, T.C. Naval Special Warfare (NSW) crewmen demonstrate diminished cervical strength and range of motion compared to NSW students. Work 2017, 58, 111–119. [Google Scholar] [CrossRef]
- Garrett, J.M.; Mastrorocco, M.; Peek, K.; van den Hoek, D.J.; McGuckian, T.B. The Relationship Between Neck Strength and Sports-Related Concussion in Team Sports: A Systematic Review With Meta-analysis. J. Orthop. Sports Phys. Ther. 2023, 53, 585–593. [Google Scholar] [CrossRef]
- Peek, K.; Andersen, J.; McKay, M.J.; Versteegh, T.; Gilchrist, I.A.; Meyer, T.; Gardner, A. The Effect of the FIFA 11 + with Added Neck Exercises on Maximal Isometric Neck Strength and Peak Head Impact Magnitude During Heading: A Pilot Study. Sports Med. 2022, 52, 655–668. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, M.; Donno, L.; Cimolin, V.; Galli, M. Cervical Range of Motion Assessment through Inertial Technology: A Validity and Reliability Study. Sensors 2023, 23, 6013. [Google Scholar] [CrossRef] [PubMed]
- Selistre, L.F.A.; Melo, C.S.; Noronha, M.A. Reliability and Validity of Clinical Tests for Measuring Strength or Endurance of Cervical Muscles: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2021, 102, 1210–1227. [Google Scholar] [CrossRef] [PubMed]
- Nagai, T.; Clark, N.C.; Abt, J.P.; Sell, T.C.; Heebner, N.R.; Smalley, B.W.; Wirt, M.D.; Lephart, S.M. The Effect of Target Position on the Accuracy of Cervical-Spine-Rotation Active Joint-Position Sense. J. Sport Rehabil. 2016, 25, 58–63. [Google Scholar] [CrossRef]
- Perrin, D.H. Isokinetic Exercise and Assessment; Human Kinetics Publishers: Champaign, IL, USA, 1993; p. x. 212p. [Google Scholar]
- Lohman, T.; Roche, A.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics: Champaign, IL, USA, 1988. [Google Scholar]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Wikstrom, E.A.; Tillman, M.D.; Smith, A.N.; Borsa, P.A. A New Force-Plate Technology Measure of Dynamic Postural Stability: The Dynamic Postural Stability Index. J. Athl. Train. 2005, 40, 305–309. [Google Scholar]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 2nd ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2000; p. xiv. 768p. [Google Scholar]
- McBride, L.; James, R.S.; Alsop, S.; Oxford, S.W. Intra and Inter-Rater Reliability of a Novel Isometric Test of Neck Strength. Sports 2022, 11, 2. [Google Scholar] [CrossRef]

| Session 1 | Session 2 | ||||||
|---|---|---|---|---|---|---|---|
| Tester 1 | Tester 2 | Tester 2 | |||||
| Mean | Standard Deviation | Mean | Standard Deviation | Mean | Standard Deviation | ||
| Strength | Extension (Newtons) | 164.6 | 54.6 | 185.3 | 52.2 | 202.2 | 60.3 |
| Flexion (Newtons) | 79.4 | 32.1 | 81.0 | 31.2 | 78.5 | 30.2 | |
| Right Rotation (Newtons) | 116.4 | 37.2 | 122.5 | 26.9 | 133.1 | 30.1 | |
| Left Rotation (Newtons) | 118.5 | 44.0 | 124.0 | 31.4 | 124.9 | 29.6 | |
| Right Lateral Flexion (Newtons) | 117.5 | 40.6 | 136.9 | 32.7 | 137.0 | 38.1 | |
| Left Lateral Flexion (Newtons) | 124.5 | 47.2 | 128.2 | 32.9 | 131.2 | 31.6 | |
| Range of Motion | Extension (Degrees) | 72.1 | 17.5 | 72.8 | 15.4 | 72.0 | 12.8 |
| Flexion (Degrees) | 63.5 | 11.7 | 63.8 | 11.1 | 64.2 | 10.9 | |
| Right Rotation (Degrees) | 69.3 | 7.9 | 66.3 | 12.8 | 66.2 | 11.1 | |
| Left Rotation (Degrees) | 71.6 | 8.5 | 68.3 | 11.6 | 70.7 | 9.6 | |
| Right Lateral Flexion (Degrees) | 46.0 | 8.4 | 48.0 | 9.2 | 47.6 | 7.0 | |
| Left Lateral Flexion (Degrees) | 47.7 | 8.6 | 49.8 | 9.8 | 49.3 | 9.3 | |
| Inter-Rater | Intra-Rater | ||||||
|---|---|---|---|---|---|---|---|
| ICC | SEM | MDC | ICC | SEM | MDC | ||
| Strength | Extension (Newtons) | 0.83 | 21.9 | 30.9 | 0.93 | 14.4 | 20.4 |
| Flexion (Newtons) | 0.96 | 6.1 | 8.7 | 0.95 | 6.7 | 9.5 | |
| Right Rotation (Newtons) | 0.83 | 13.1 | 18.5 | 0.90 | 8.8 | 12.5 | |
| Left Rotation (Newtons) | 0.89 | 12.3 | 17.4 | 0.97 | 5.3 | 7.4 | |
| Right Lateral Flexion (Newtons) | 0.70 | 20.4 | 28.9 | 0.95 | 7.7 | 10.9 | |
| Left Lateral Flexion (Newtons) | 0.89 | 13.0 | 18.4 | 0.95 | 6.7 | 9.5 | |
| Range of Motion | Extension (Degrees) | 0.94 | 3.4 | 4.8 | 0.92 | 4.4 | 6.2 |
| Flexion (Degrees) | 0.94 | 2.5 | 3.5 | 0.87 | 4.0 | 5.6 | |
| Right Rotation (Degrees) | 0.90 | 3.6 | 5.1 | 0.85 | 4.0 | 5.7 | |
| Left Rotation (Degrees) | 0.93 | 2.8 | 4.0 | 0.85 | 3.9 | 5.5 | |
| Right Lateral Flexion (Degrees) | 0.85 | 3.0 | 4.3 | 0.81 | 3.7 | 5.2 | |
| Left Lateral Flexion (Degrees) | 0.88 | 3.3 | 4.6 | 0.86 | 3.4 | 4.8 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sell, T.C.; Zerega, R. Reliability of a Musculoskeletal Assessment for the Examination of Cervical Spine Pain and Injuries in Special Forces Combat Soldiers. Sports 2024, 12, 255. https://doi.org/10.3390/sports12090255
Sell TC, Zerega R. Reliability of a Musculoskeletal Assessment for the Examination of Cervical Spine Pain and Injuries in Special Forces Combat Soldiers. Sports. 2024; 12(9):255. https://doi.org/10.3390/sports12090255
Chicago/Turabian StyleSell, Timothy C., and Ryan Zerega. 2024. "Reliability of a Musculoskeletal Assessment for the Examination of Cervical Spine Pain and Injuries in Special Forces Combat Soldiers" Sports 12, no. 9: 255. https://doi.org/10.3390/sports12090255
APA StyleSell, T. C., & Zerega, R. (2024). Reliability of a Musculoskeletal Assessment for the Examination of Cervical Spine Pain and Injuries in Special Forces Combat Soldiers. Sports, 12(9), 255. https://doi.org/10.3390/sports12090255






