Machine Learning for Personalized Prediction of Electrocardiogram (EKG) Use in Emergency Care
Abstract
1. Introduction
2. Methods
2.1. Study Design and Data Source
2.2. Variable Selection and Data Processing
2.3. Feature Selection and Predictive Modeling
2.4. Model Evaluation
3. Results
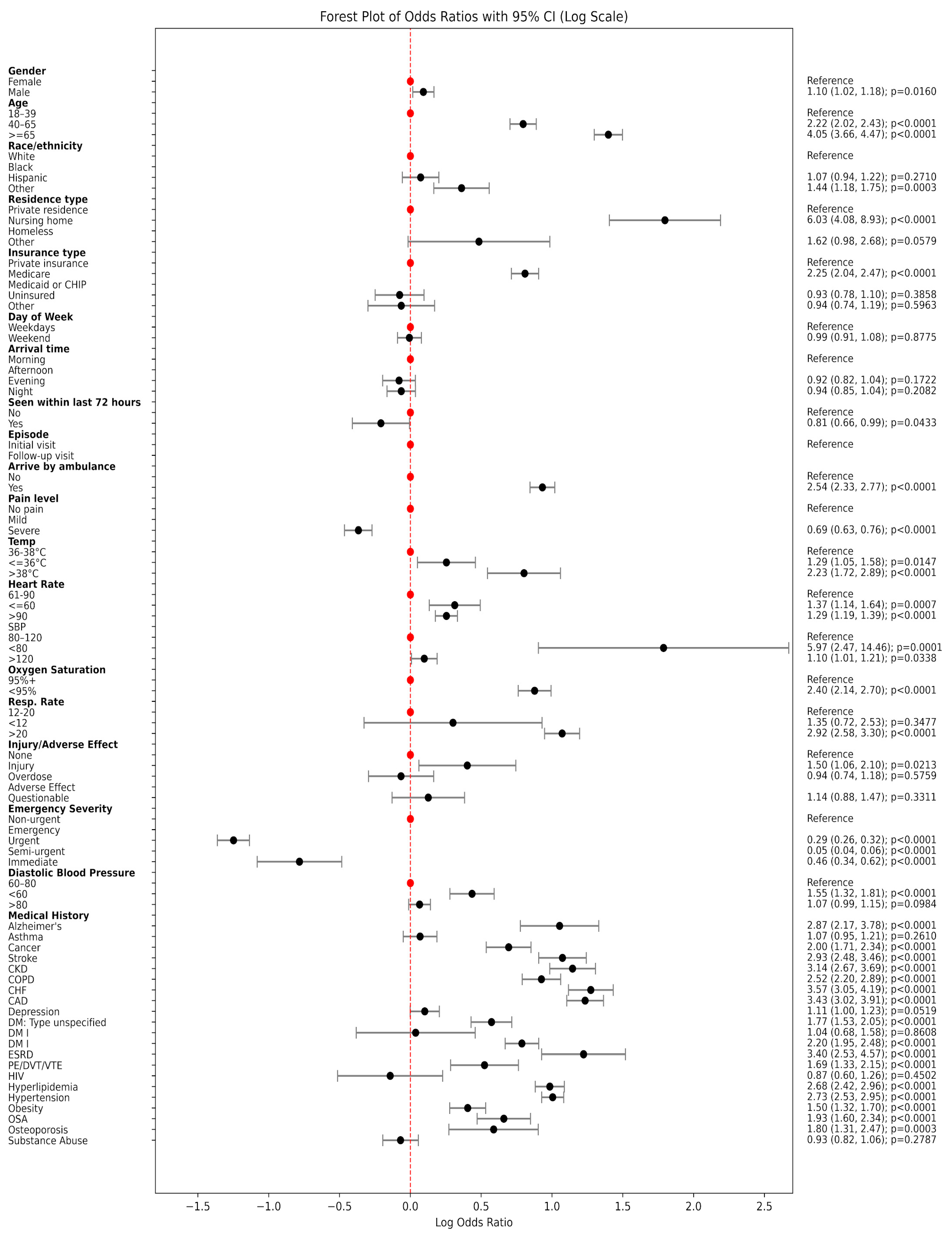
3.1. Patient Characteristics Associated with EKG Utilization
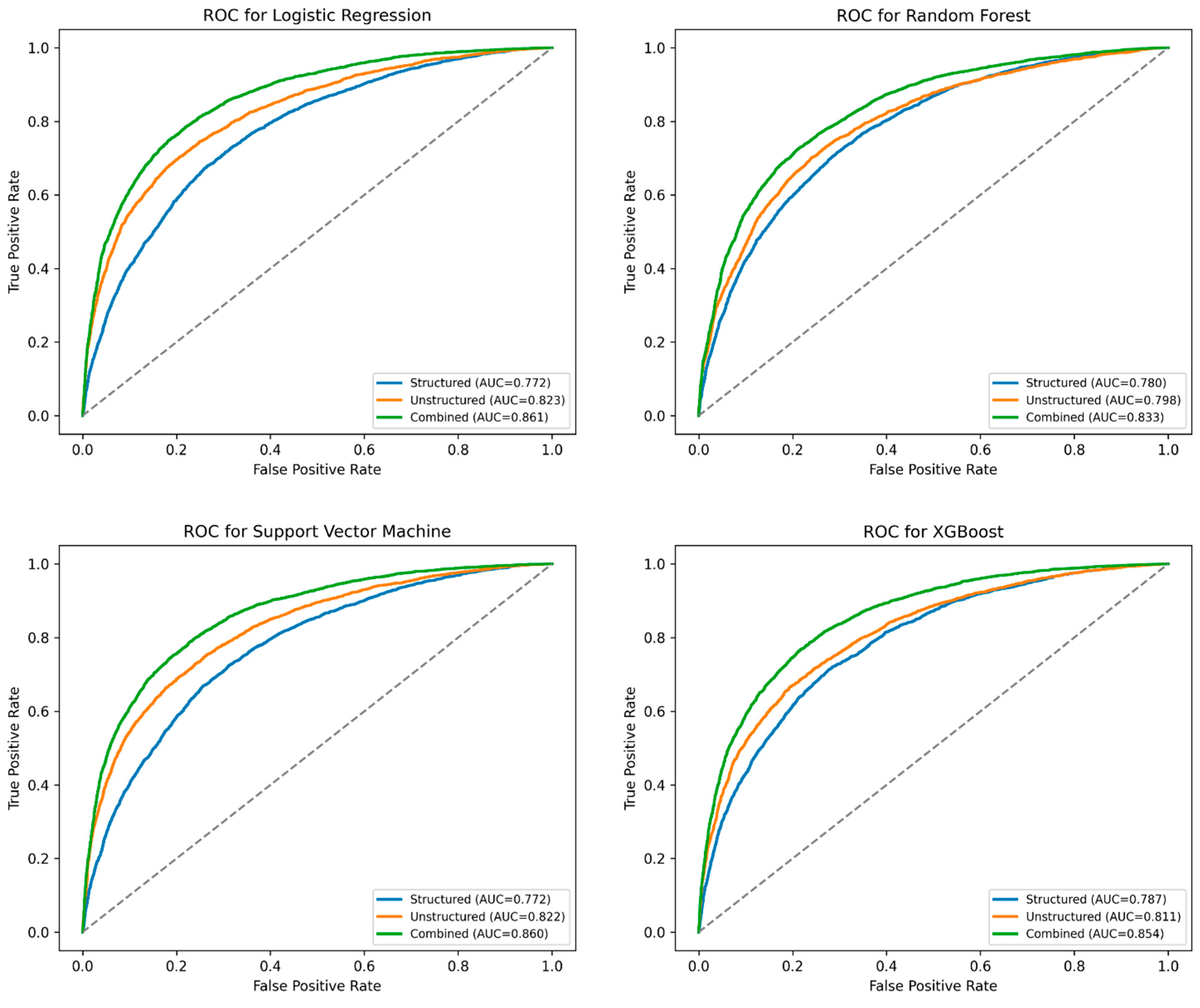
3.2. Predictive Models
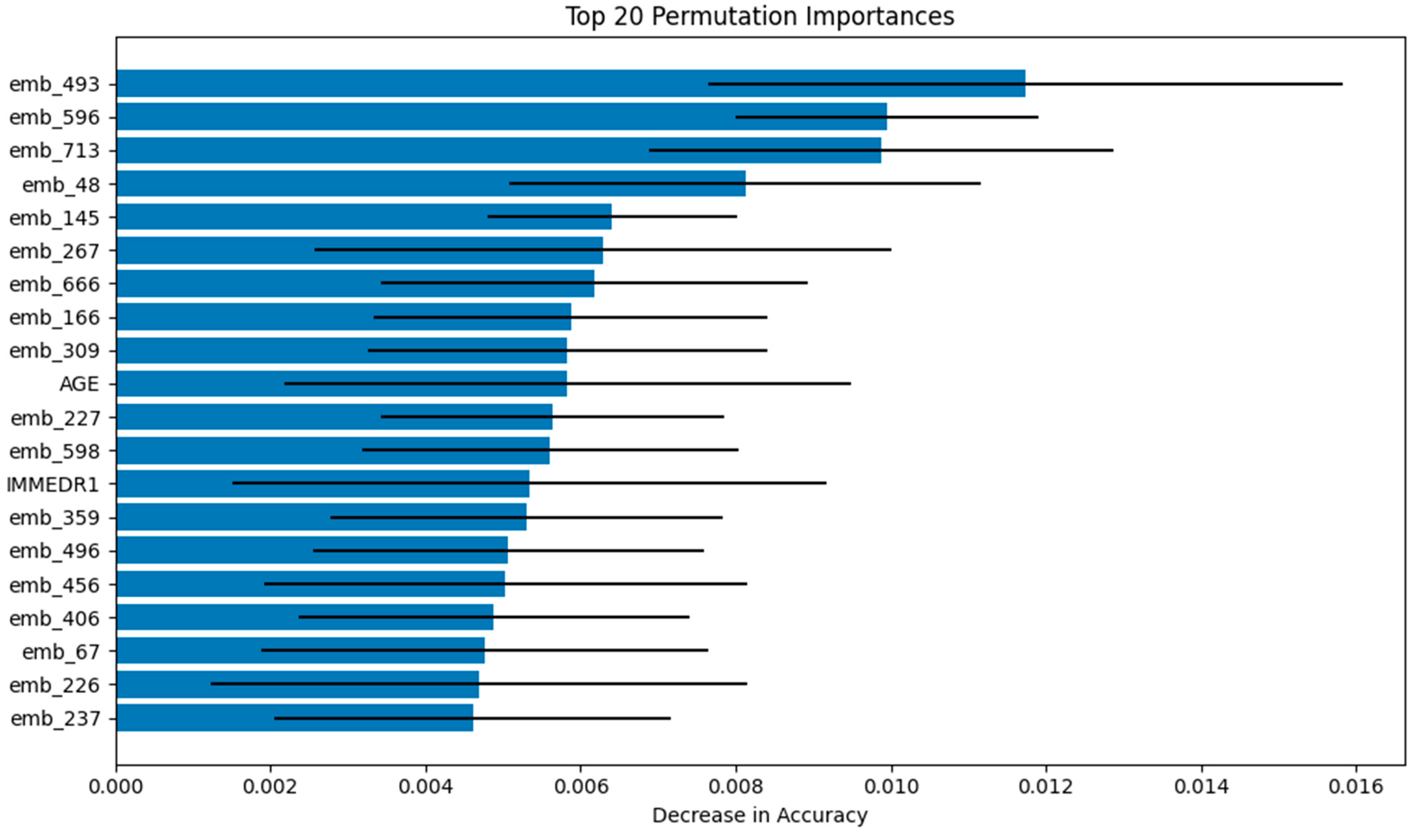
3.3. Model Interpretability
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsai, D.J.; Tsai, S.H.; Chiang, H.H.; Lee, C.C.; Chen, S.J. Development and Validation of an Artificial Intelligence Electrocardiogram Recommendation System in the Emergency Department. J. Pers. Med. 2022, 12, 700. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Zaiti, S.S.; Martin-Gill, C.; Zègre-Hemsey, J.K.; Bouzid, Z.; Faramand, Z.; Alrawashdeh, M.O.; Gregg, R.E.; Helman, S.; Riek, N.T.; Kraevsky-Phillips, K.; et al. Machine learning for ECG diagnosis and risk stratification of occlusion myocardial infarction. Nat. Med. 2023, 29, 1804–1813. [Google Scholar] [CrossRef] [PubMed]
- Adedinsewo, D.; Carter, R.E.; Attia, Z.; Johnson, P.; Kashou, A.H.; Dugan, J.L.; Albus, M.; Sheele, J.M.; Bellolio, F.; Friedman, P.A.; et al. Artificial intelligence-enabled ECG algorithm to identify patients with left ventricular systolic dysfunction presenting to the emergency department with dyspnea. Circ. Arrhythmia Electrophysiol. 2020, 13, e008437. [Google Scholar] [CrossRef] [PubMed]
- Sanjay, M.; Kurien, A.S.; Abraham, M.H.; Speedie, A. The Utility of an Electrocardiogram in High-, Intermediate-, and Low-Risk Patients Presenting with Chest Pain to Emergency Department. Curr. Med. Issues 2023, 21, 44–49. [Google Scholar] [CrossRef]
- Farcas, A.M.; Joiner, A.P.; Rudman, J.S.; Ramesh, K.; Torres, G.; Crowe, R.P.; Curtis, T.; Tripp, R.; Bowers, K.; von Isenburg, M.; et al. Disparities in emergency medical services care delivery in the United States: A scoping review. Prehosp. Emerg. Care 2023, 27, 1058–1071. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, M.; Moyer, E.; Dissanayake, V.; Purim-Shem-Tov, Y.; Walker, G.; Corbin, T.; Bernard, K.; Buell, K. Disparities in troponin and ECG testing among emergency department patients with chest pain. Am. J. Emerg. Med. 2025, 93, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-H.; Lin, Y.-C.; Huang, F.-W.; Chen, D.-M.; Chung, Y.-T.; Chen, W.-K.; Wang, C.C. Using machine learning and natural language processing in triage for prediction of clinical disposition in the emergency department. BMC Emerg. Med. 2024, 24, 237. [Google Scholar] [CrossRef] [PubMed]
- Stewart, J.; Lu, J.; Goudie, A.; Arendts, G.; Meka, S.A.; Freeman, S.; Walker, K.; Sprivulis, P.; Sanfilippo, F.; Bennamoun, M.; et al. Applications of natural language processing at emergency department triage: A narrative review. PLoS ONE 2023, 18, e0279953. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, X.; Kim, J.; Patzer, R.E.; Pitts, S.R.; Patzer, A.; Schrager, J.D. Prediction of emergency department hospital admission based on natural language processing and neural networks. Methods Inf. Med. 2017, 56, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, H.; Yu, G.; Zhang, W. Machine learning-driven prediction of hospital admissions using gradient boosting and GPT-2. Digit. Health 2025, 11, 20552076251331319. [Google Scholar] [CrossRef] [PubMed]
- Cersosimo, A.; Zito, E.; Pierucci, N.; Matteucci, A.; La Fazia, V.M. A Talk with ChatGPT: The Role of Artificial Intelligence in Shaping the Future of Cardiology and Electrophysiology. J. Pers. Med. 2025, 15, 205. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, Y.; Jiang, Y.; Pacella, C.B.; Zhang, W. Integrating structured and unstructured data for predicting emergency severity: An association and predictive study using transformer-based natural language processing models. BMC Med. Inform. Decis. Mak. 2024, 24, 372. [Google Scholar] [CrossRef] [PubMed]
- Su, D.; Li, Q.; Zhang, T.; Veliz, P.; Chen, Y.; He, K.; Mahajan, P.; Zhang, X. Prediction of acute appendicitis among patients with undifferentiated abdominal pain at emergency department. BMC Med. Res. Methodol. 2022, 22, 18. [Google Scholar] [CrossRef] [PubMed]
- Sterling, N.W.; Brann, F.; Patzer, R.E.; Di, M.; Koebbe, M.; Burke, M.; Schrager, J.D. Prediction of emergency department resource requirements during triage: An application of current natural language processing techniques. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1676–1683. [Google Scholar] [CrossRef]
- Tootooni, M.S.; Pasupathy, K.S.; Heaton, H.A.; Clements, C.M.; Sir, M.Y. CCMapper: An adaptive NLP-based free-text chief complaint mapping algorithm. Comput. Biol. Med. 2019, 113, 103398. [Google Scholar] [CrossRef] [PubMed]
- Reimers, N.; Gurevych, I. Sentence-bert: Sentence embeddings using siamese bert-networks. arXiv 2019. [Google Scholar] [CrossRef]
- Yan, B.; Pei, M. Clinical-bert: Vision-language pre-training for radiograph diagnosis and reports generation. Proc. AAAI Conf. Artif. Intell. 2022, 36, 2982–2990. [Google Scholar] [CrossRef]
- Chiu, B.; Baker, S. Word embeddings for biomedical natural language processing: A survey. Lang. Linguist. Compass 2020, 14, e12402. [Google Scholar] [CrossRef]
- Boughorbel, S.; Jarray, F.; Homaid, A.A.; Niaz, R.; Alyafei, K. Multi-Modal Perceiver Language Model for Outcome Prediction in Emergency Department. arXiv 2023. [Google Scholar] [CrossRef]
- Cairns, C.; Kang, K. National Hospital Ambulatory Medical Care Survey: 2019 Emergency Department Summary Tables; National Center for Health Statistics: Hyattsville, MD, USA, 2022.
- Santo, L.; Kang, K. National Hospital Ambulatory Medical Care Survey: 2019 National Summary Tables; National Center for Health Statistics: Hyattsville, MD, USA, 2023.
- Muselli, M.; Cofini, V.; Mammarella, L.; Carmignani, C.; Fabiani, L.; Desideri, G.; Necozione, S. The impact of COVID-19 pandemic on emergency services. Ann. Ig. Med. Prev. Comunità 2022, 34, 248–258. [Google Scholar]

| EKG Use | |||
|---|---|---|---|
| No | Yes | p Value | |
| 9105 (69.4%) | 4010 (30.6%) | ||
| Gender | 0.0168 | ||
| Female | 4980 (54.7%) | 2102 (52.4%) | |
| Male | 4125 (45.3%) | 1908 (47.6%) | |
| Age | <0.0001 | ||
| 18–39 | 4222 (46.4%) | 937 (23.4%) | |
| 40–65 | 3233 (35.5%) | 1591 (39.7%) | |
| > 65 | 1650 (18.1%) | 1482 (37.0%) | |
| Race/ethnicity | <0.0001 | ||
| White | 5273 (57.9%) | 2464 (61.4%) | |
| Black | 2192 (24.1%) | 831 (20.7%) | |
| Hispanic | 1298 (14.3%) | 529 (13.2%) | |
| Other | 342 (3.8%) | 186 (4.6%) | |
| Residence type | <0.0001 | ||
| Private residence | 8597 (94.4%) | 3794 (94.6%) | |
| Nursing home | 129 (1.4%) | 137 (3.4%) | |
| Homeless | 267 (2.9%) | 47 (1.2%) | |
| Other | 112 (1.2%) | 32 (0.8%) | |
| Insurance type | <0.0001 | ||
| Private insurance | 2445 (26.9%) | 1037 (25.9%) | |
| Medicare | 2652 (29.1%) | 1791 (44.7%) | |
| Medicaid or CHIP | 2921 (32.1%) | 878 (21.9%) | |
| Uninsured | 736 (8.1%) | 205 (5.1%) | |
| Other | 351 (3.9%) | 99 (2.5%) | |
| Day of Week | 0.8945 | ||
| Weekdays | 6691 (73.5%) | 2952 (73.6%) | |
| Weekend | 2414 (26.5%) | 1058 (26.4%) | |
| Arrival time | 0.3963 | ||
| Morning | 2544 (27.9%) | 1143 (28.5%) | |
| Afternoon | 2956 (32.5%) | 1342 (33.5%) | |
| Evening | 1418 (15.6%) | 594 (14.8%) | |
| Night | 2187 (24.0%) | 931 (23.2%) | |
| Seen within last 72 h | 0.0483 | ||
| No | 8736 (95.9%) | 3877 (96.7%) | |
| Yes | 369 (4.1%) | 133 (3.3%) | |
| Episode | <0.0001 | ||
| Initial visit | 8400 (92.3%) | 3803 (94.8%) | |
| Follow-up visit | 705 (7.7%) | 207 (5.2%) | |
| Arrive by ambulance | <0.0001 | ||
| No | 7689 (84.4%) | 2732 (68.1%) | |
| Yes | 1416 (15.6%) | 1278 (31.9%) | |
| Pain level | <0.0001 | ||
| No pain | 1933 (21.2%) | 1191 (29.7%) | |
| Mild | 4758 (52.3%) | 2086 (52.0%) | |
| Severe | 2414 (26.5%) | 733 (18.3%) | |
| Temperature | <0.0001 | ||
| 36–38 °C | 8717 (95.7%) | 3746 (93.4%) | |
| < 36 °C | 267 (2.9%) | 148 (3.7%) | |
| >38 °C | 121 (1.3%) | 116 (2.9%) | |
| Heart Rate | <0.0001 | ||
| 61–90 | 5544 (60.9%) | 2187 (54.5%) | |
| < 60 | 365 (4.0%) | 197 (4.9%) | |
| >90 | 3196 (35.1%) | 1626 (40.5%) | |
| SBP | <0.0001 | ||
| 80–120 | 2064 (22.7%) | 839 (20.9%) | |
| <80 | 7 (0.1%) | 17 (0.4%) | |
| >120 | 7034 (77.3%) | 3154 (78.7%) | |
| DBP | <0.0001 | ||
| 60–80 | 4326 (47.5%) | 1799 (44.9%) | |
| <60 | 459 (5.0%) | 295 (7.4%) | |
| >80 | 4319 (47.4%) | 1916 (47.8%) | |
| Oxygen Saturation | <0.0001 | ||
| 95%+ | 8443 (92.7%) | 3374 (84.1%) | |
| <95% | 662 (7.3%) | 636 (15.9%) | |
| Resp. Rate | <0.0001 | ||
| 12–20 | 8556 (94.0%) | 3392 (84.6%) | |
| <12 | 28 (0.3%) | 15 (0.4%) | |
| >20 | 521 (5.7%) | 603 (15.0%) | |
| Injury/Adverse Effect | |||
| None | 2661 (29.2%) | 491 (12.2%) | |
| Injury | 84 (0.9%) | 55 (1.4%) | |
| Overdose | 256 (2.8%) | 105 (2.6%) | |
| Adverse Effect | 5923 (65.1%) | 3269 (81.5%) | |
| Questionable | 181 (2.0%) | 90 (2.2%) | |
| Emergency Severity | <0.0001 | ||
| Immediate | 118 (1.3%) | 84 (2.1%) | |
| Emergency | 579 (6.4%) | 902 (22.5%) | |
| Urgent | 6374 (70.0%) | 2847 (71.0%) | |
| Semi-urgent | 1793 (19.7%) | 146 (3.6%) | |
| Non-urgent | 241 (2.6%) | 31 (0.8%) | |
| Medical History | |||
| Alzheimer’s disease/Dementia | 92 (1.0%) | 114 (2.8%) | <0.0001 |
| Asthma | 955 (10.5%) | 447 (11.1%) | 0.2741 |
| Cancer | 356 (3.9%) | 302 (7.5%) | <0.0001 |
| Cerebrovascular disease/History of stroke (CVA) | 262 (2.9%) | 320 (8.0%) | <0.0001 |
| Chronic kidney disease (CKD) | 277 (3.0%) | 360 (9.0%) | <0.0001 |
| Chronic obstructive pulmonary disease (COPD) | 450 (4.9%) | 465 (11.6%) | <0.0001 |
| Congestive heart failure (CHF) | 276 (3.0%) | 403 (10.0%) | <0.0001 |
| Coronary artery disease (CAD) | 438 (4.8%) | 593 (14.8%) | <0.0001 |
| Depression | 1331 (14.6%) | 639 (15.9%) | 0.0551 |
| Diabetes mellitus (DM)-Type unspecified | 466 (5.1%) | 350 (8.7%) | <0.0001 |
| Diabetes mellitus (DM))-Type I | 70 (0.8%) | 32 (0.8%) | 0.9462 |
| Diabetes mellitus (DM)-Type II | 654 (7.2%) | 583 (14.5%) | <0.0001 |
| End-stage renal disease (ESRD) | 75 (0.8%) | 110 (2.7%) | <0.0001 |
| Pulmonary embolism (PE), DVT, or venous thromboembolism (VTE) | 162 (1.8%) | 119 (3.0%) | <0.0001 |
| HIV infection/AIDS | 102 (1.1%) | 39 (1.0%) | 0.5068 |
| Hyperlipidemia | 869 (9.5%) | 883 (22.0%) | <0.0001 |
| Hypertension | 2347 (25.8%) | 1952 (48.7%) | <0.0001 |
| Obesity (BMI ≥ 30) | 674 (7.4%) | 429 (10.7%) | <0.0001 |
| Obstructive sleep apnea (OSA) | 248 (2.7%) | 206 (5.1%) | <0.0001 |
| Osteoporosis | 89 (1.0%) | 70 (1.7%) | 0.0003 |
| Substance abuse or dependence | 928 (10.2%) | 384 (9.6%) | 0.2929 |
| Model | Feature Set | Accuracy | Precision | Sensitivity | Specificity | AUC | Best Parameter |
|---|---|---|---|---|---|---|---|
| Logistic Regression (LR) | Combined | 0.794 | 0.637 | 0.755 | 0.811 | 0.861 | {‘C’: 0.1, ‘penalty’: ‘l2’, ‘solver’: ‘lbfgs’} |
| Unstructured | 0.766 | 0.600 | 0.703 | 0.793 | 0.823 | {‘C’: 0.1, ‘penalty’: ‘l2’, ‘solver’: ‘lbfgs’} | |
| Structured | 0.717 | 0.530 | 0.679 | 0.734 | 0.772 | {‘C’: 0.01, ‘penalty’: ‘l2’, ‘solver’: ‘lbfgs’} | |
| Random Forest (RF) | Combined | 0.770 | 0.604 | 0.722 | 0.792 | 0.833 | {‘max_depth’: 10, ‘min_samples_split’: 2, ‘n_estimators’: 200} |
| Unstructured | 0.742 | 0.563 | 0.700 | 0.761 | 0.798 | {‘max_depth’: 10, ‘min_samples_split’: 5, ‘n_estimators’: 200} | |
| Structured | 0.709 | 0.517 | 0.715 | 0.706 | 0.780 | {‘max_depth’: 10, ‘min_samples_split’: 5, ‘n_estimators’: 200} | |
| Support Vector Machine (SVM) | Combined | 0.777 | 0.605 | 0.786 | 0.774 | 0.860 | {‘C’: 0.1} |
| Unstructured | 0.751 | 0.572 | 0.730 | 0.760 | 0.822 | {‘C’: 0.1} | |
| Structured | 0.699 | 0.506 | 0.725 | 0.688 | 0.772 | {‘C’: 0.1} | |
| XG Boosting (XGB) | Combined | 0.778 | 0.609 | 0.768 | 0.783 | 0.854 | {‘learning_rate’: 0.1, ‘max_depth’: 3, ‘n_estimators’: 200, ‘subsample’: 1.0} |
| Unstructured | 0.721 | 0.532 | 0.711 | 0.725 | 0.787 | {‘learning_rate’: 0.1, ‘max_depth’: 3, ‘n_estimators’: 100, ‘subsample’: 0.8} | |
| Structured | 0.763 | 0.601 | 0.667 | 0.805 | 0.811 | {‘learning_rate’: 0.1, ‘max_depth’: 3, ‘n_estimators’: 200, ‘subsample’: 0.8} |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Zhang, X. Machine Learning for Personalized Prediction of Electrocardiogram (EKG) Use in Emergency Care. J. Pers. Med. 2025, 15, 358. https://doi.org/10.3390/jpm15080358
Wang H, Zhang X. Machine Learning for Personalized Prediction of Electrocardiogram (EKG) Use in Emergency Care. Journal of Personalized Medicine. 2025; 15(8):358. https://doi.org/10.3390/jpm15080358
Chicago/Turabian StyleWang, Hairong, and Xingyu Zhang. 2025. "Machine Learning for Personalized Prediction of Electrocardiogram (EKG) Use in Emergency Care" Journal of Personalized Medicine 15, no. 8: 358. https://doi.org/10.3390/jpm15080358
APA StyleWang, H., & Zhang, X. (2025). Machine Learning for Personalized Prediction of Electrocardiogram (EKG) Use in Emergency Care. Journal of Personalized Medicine, 15(8), 358. https://doi.org/10.3390/jpm15080358






