Timing of Loop Ileostomy Closure Does Not Play a Pivotal Role in Terms of Complications—Results of the Liquidation of iLEOstomy (LILEO) Study
Abstract
1. Introduction
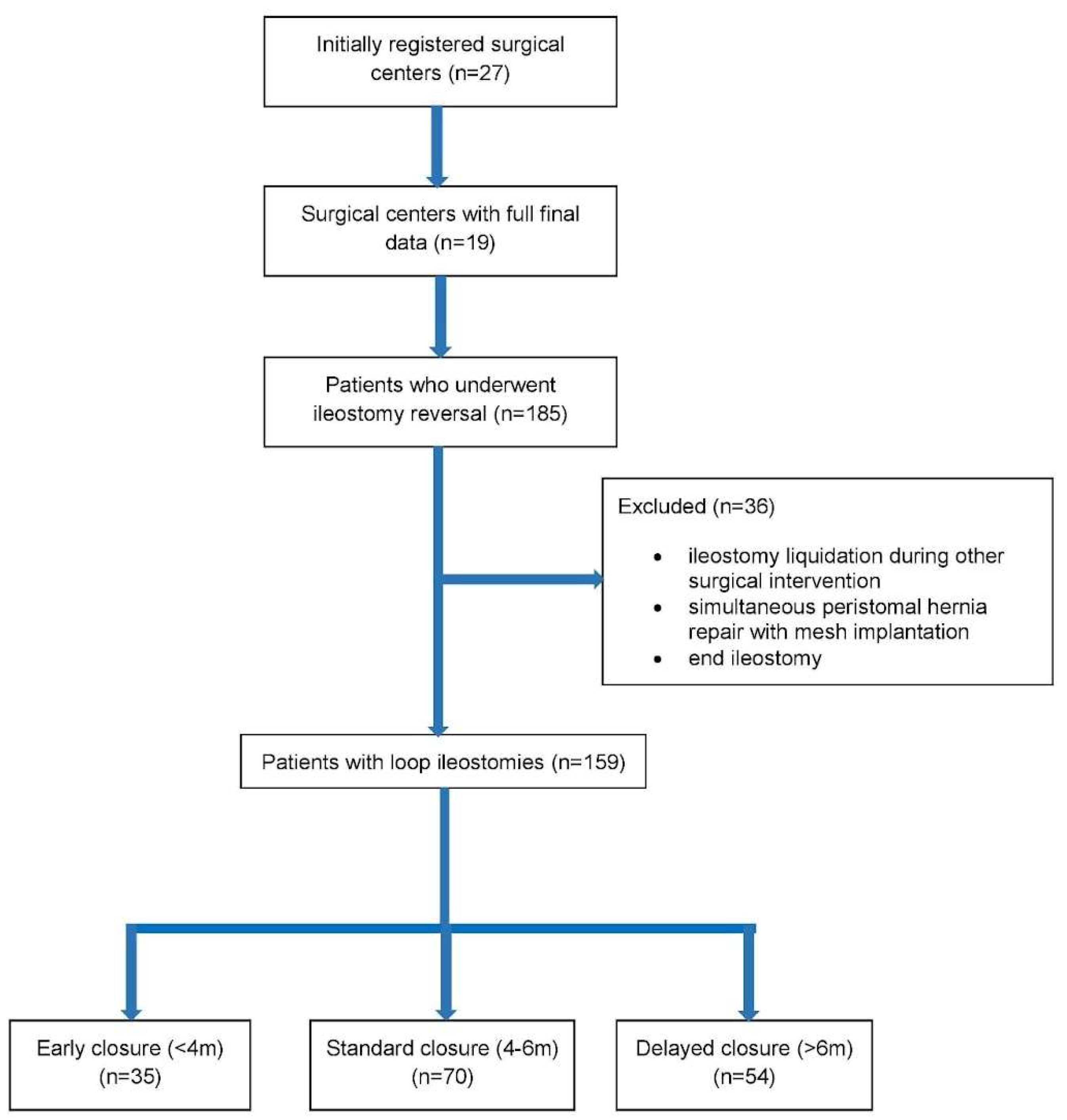
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pisarska, M.; Gajewska, N.; Małczak, P.; Wysocki, M.; Witowski, J.; Torbicz, G.; Major, P.; Mizera, M.; Dembiński, M.; Migaczewski, M.; et al. Defunctioning ileostomy reduces leakage rate in rectal cancer surgery-systematic review and meta-analysis. Oncotarget 2018, 9, 20816–20825. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chiarello, M.M.; Fransvea, P.; Cariati, M.; Adams, N.J.; Bianchi, V.; Brisinda, G. Anastomotic leakage in colorectal cancer surgery. Surg. Oncol. 2022, 40, 101708. [Google Scholar] [CrossRef] [PubMed]
- Fielding, A.; Woods, R.; Moosvi, S.R.; Wharton, R.Q.; Speakman, C.T.M.; Kapur, S.; Shaikh, I.; Hernon, J.M.; Lines, S.W.; Stearns, A.T. Renal impairment after ileostomy formation: A frequent event with long-term consequences. Color. Dis. 2020, 22, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Climent, M.; Frago, R.; Cornella, N.; Serrano, M.; Kreisler, E.; Biondo, S. Prognostic factors for complications after loop ileostomy reversal. Tech. Coloproctol. 2022, 26, 45–52. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, N.J.; Temperley, H.C.; Nugent, T.S.; Low, E.Z.; Kavanagh, D.O.; Larkin, J.O.; Mehigan, B.J.; McCormick, P.H.; Kelly, M.E. Early vs. standard reversal ileostomy: A systematic review and meta-analysis. Tech. Coloproctol. 2022, 26, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Ng, Z.Q.; Levitt, M.; Platell, C. The feasibility and safety of early ileostomy reversal: A systematic review and meta-analysis. ANZ J. Surg. 2020, 90, 1580–1587. [Google Scholar] [CrossRef] [PubMed]
- Caminsky, N.G.; Moon, J.; Morin, N.; Alavi, K.; Auer, R.C.; Bordeianou, L.G.; Chadi, S.A.; Drolet, S.; Ghuman, A.; Liberman, A.S.; et al. Patient and surgeon preferences for early ileostomy closure following restorative proctectomy for rectal cancer: Why aren’t we doing it? Surg. Endosc. 2023, 37, 669–682. [Google Scholar] [CrossRef] [PubMed]
- Fukudome, I.; Maeda, H.; Okamoto, K.; Yamaguchi, S.; Fujisawa, K.; Shiga, M.; Dabanaka, K.; Kobayashi, M.; Namikawa, T.; Hanazaki, K. Early stoma closure after low anterior resection is not recommended due to postoperative complications and asymptomatic anastomotic leakage. Sci. Rep. 2023, 13, 6472. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahmadi-Amoli, H.; Rahimi, M.; Abedi-Kichi, R.; Ebrahimian, N.; Hosseiniasl, S.M.; Hajebi, R.; Rahimpour, E. Early closure compared to late closure of temporary ileostomy in rectal cancer: A randomized controlled trial study. Langenbecks Arch. Surg. 2023, 408, 234. [Google Scholar] [CrossRef] [PubMed]
- Xia, F.; Zou, Y.; Zhang, Q.; Wu, J.; Sun, Z. A novel nomogram to predict low anterior resection syndrome (LARS) after ileostomy reversal for rectal cancer patients. Eur. J. Surg. Oncol. 2023, 49, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Vogel, I.; Reeves, N.; Tanis, P.J.; Bemelman, W.A.; Torkington, J.; Hompes, R.; Cornish, J.A. Impact of a defunctioning ileostomy and time to stoma closure on bowel function after low anterior resection for rectal cancer: A systematic review and meta-analysis. Tech. Coloproctol. 2021, 25, 751–760. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kisielewski, M.; Wysocki, M.; Stefura, T.; Wojewoda, T.; Safiejko, K.; Wierdak, M.; Sachanbiński, T.; Jankowski, M.; Tkaczyński, K.; Richter, K.; et al. Preliminary results of Polish national multicenter LILEO study on ileostomy reversal. Pol. J. Surg. 2024, 96, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Krand, O.; Yalti, T.; Berber, I.; Tellioglu, G. Early vs. delayed closure of temporary covering ileostomy: A prospective study. Hepato-Gastroenterol. 2008, 55, 142–145. [Google Scholar]
- Abdalla, S.; Scarpinata, R. Early and Late Closure of Loop Ileostomies: A Retrospective Comparative Outcomes Analysis. Ostomy Wound Manag. 2018, 64, 30–35. [Google Scholar] [CrossRef]
- Khoo, T.W.; Dudi-Venkata, N.N.; Beh, Y.Z.; Bedrikovetski, S.; Kroon, H.M.; Thomas, M.L.; Sammour, T. Impact of timing of reversal of loop ileostomy on patient outcomes: A retrospective cohort study. Tech. Coloproctol. 2021, 25, 1217–1224. [Google Scholar] [CrossRef] [PubMed]
- Eskicioglu, C.; Forbes, S.S.; Aarts, M.-A.; Okrainec, A.; McLeod, R.S. Enhanced recovery after surgery (ERAS) programs for patients having colorectal surgery: A meta-analysis of randomized trials. J. Gastrointest. Surg. 2009, 13, 2321–2329. [Google Scholar] [CrossRef]
- Olson, K.A.; Fleming, R.Y.D.; Fox, A.W.; Grimes, A.E.; Mohiuddin, S.S.; Robertson, H.T.; Moxham, J.; Wolf, J.S., Jr. The Enhanced Recovery after Surgery (ERAS) Elements that Most Greatly Impact Length of Stay and Readmission. Am. Surg. 2021, 87, 473–479. [Google Scholar] [CrossRef]
- Zhou, M.W.; Wang, Z.H.; Chen, Z.-Y.; Xiang, J.-B.; Gu, X.-D. Advantages of Early Preventive Ileostomy Closure after Total Mesorectal Excision Surgery for Rectal Cancer: An Institutional Retrospective Study of 123 Consecutive Patients. Dig. Surg. 2017, 34, 305–311. [Google Scholar] [CrossRef]
- Sauri, F.; Sakr, A.; Kim, H.S.; Alessa, M.; Torky, R.; Zakarneh, E.; Yang, S.Y.; Kim, N.K. Does the timing of protective ileostomy closure post-low anterior resection have an impact on the outcome? A retrospective study. Asian J. Surg. 2021, 44, 374–379. [Google Scholar] [CrossRef]
- Elsner, A.T.; Brosi, P.; Walensi, M.; Uhlmann, M.; Egger, B.; Glaser, C.; Maurer, C.A. Closure of Temporary Ileostomy 2 Versus 12 Weeks after Rectal Resection for Cancer: A Word of Caution from a Prospective, Randomized Controlled Multicenter Trial. Dis. Colon. Rectum 2021, 64, 1398–1406. [Google Scholar] [CrossRef]
- Vogel, J.D.; Fleshner, P.R.; Holubar, S.D.; Poylin, V.Y.; Regenbogen, S.E.; Chapman, B.C.; Messaris, E.; Mutch, M.G.; Hyman, N.H. High Complication Rate after Early Ileostomy Closure: Early Termination of the Short Versus Long Interval to Loop Ileostomy Reversal after Pouch Surgery Randomized Trial. Dis. Colon. Rectum 2023, 66, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Morada, A.O.; Senapathi, S.H.; Bashiri, A.; Chai, S.; Cagir, B. A systematic review of primary ileostomy site malignancies. Surg. Endosc. 2022, 36, 1750–1760. [Google Scholar] [CrossRef] [PubMed]
- Hanada, M.; Chika, N.; Kamae, N.; Muta, Y.; Chikatani, K.; Ito, T.; Mori, Y.; Suzuki, O.; Hatano, S.; Iwama, T.; et al. A Case of Carcinoma of the Ileostomy Site Associated with Familial Adenomatous Polyposis-Report of a Case. Gan To Kagaku Ryoho 2021, 48, 1990–1992. (In Japanese) [Google Scholar] [PubMed]
- Wang, L.; Chen, X.; Liao, C.; Wu, Q.; Luo, H.; Yi, F.; Wei, Y.; Zhang, W. Early versus late closure of temporary ileostomy after rectal cancer surgery: A meta-analysis. Surg. Today 2021, 51, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Dulskas, A.; Petrauskas, V.; Kuliavas, J.; Bickaite, K.; Kairys, M.; Pauza, K.; Kilius, A.; Sangaila, E.; Bausys, R.; Stratilatovas, E. Quality of Life and Bowel Function Following Early Closure of a Temporary Ileostomy in Patients with Rectal Cancer: A Report from a Single-Center Randomized Controlled Trial. J. Clin. Med. 2021, 10, 768. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guidolin, K.; Jung, F.; Spence, R.; Quereshy, F.; Chadi, S.A. Extended duration of faecal diversion is associated with increased ileus upon loop ileostomy reversal. Color. Dis. 2021, 23, 2146–2153. [Google Scholar] [CrossRef]
- Rodríguez-Padilla, Á.; Morales-Martín, G.; Perez-Quintero, R.; Gomez-Salgado, J.; Balongo-Garcia, R.; Ruiz-Frutos, C. Postoperative Ileus after Stimulation with Probiotics before Ileostomy Closure. Nutrients 2021, 13, 626. [Google Scholar] [CrossRef] [PubMed]
- Beamish, E.L.; Johnson, J.; Shih, B.; Killick, R.; Dondelinger, F.; McGoran, C.; Brewster-Craig, C.; Davies, A.; Bhowmick, A.; Rigby, R.J. Delay in loop ileostomy reversal surgery does not impact upon post-operative clinical outcomes. Complications are associated with an increased loss of microflora in the defunctioned intestine. Gut Microbes 2023, 15, 2199659. [Google Scholar]
- Garfinkle, R.; Demian, M.; Sabboobeh, S.; Moon, J.; Hulme-Moir, M.; Liberman, A.S.; Feinberg, S.; Hayden, D.M.; Chadi, S.A.; Demyttenaere, S.; et al. Bowel stimulation before loop ileostomy closure to reduce postoperative ileus: A multicenter, single-blinded, randomized controlled trial. Surg. Endosc. 2023, 37, 3934–3943. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lloyd, A.J.; Hardy, N.P.; Jordan, P.; Ryan, E.J.; Whelan, M.; Clancy, C.; O’Riordan, J.; Kavanagh, D.O.; Neary, P.; Sahebally, S.M. Efferent limb stimulation prior to loop ileostomy closure: A systematic review and meta-analysis. Tech. Coloproctol. 2023, 28, 15. [Google Scholar] [CrossRef] [PubMed]
- Bhatti, S.; Malik, Y.J.; Changazi, S.H.; Rahman, U.A.; Malik, A.A.; Butt, U.I.; Umar, M.; Farooka, M.W.; Ayyaz, M. Role of Chewing Gum in Reducing Postoperative Ileus after Reversal of Ileostomy: A Randomized Controlled Trial. World J. Surg. 2021, 45, 1066–1070. [Google Scholar] [CrossRef] [PubMed]
- Hajibandeh, S.; Hajibandeh, S.; Kennedy-Dalby, A.; Rehman, S.; Zadeh, R.A. Purse-string skin closure versus linear skin closure techniques in stoma closure: A comprehensive meta-analysis with trial sequential analysis of randomised trials. Int. J. Color. Dis. 2018, 33, 1319–1332. [Google Scholar] [CrossRef] [PubMed]
- Hajibandeh, S.; Hajibandeh, S.; Maw, A. Purse-string skin closure versus linear skin closure in people undergoing stoma reversal. Cochrane Database Syst. Rev. 2024, 3, CD014763. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wierdak, M.; Pisarska-Adamczyk, M.; Wysocki, M.; Major, P.; Kołodziejska, K.; Nowakowski, M.; Vongsurbchart, T.; Pędziwaitr, M. Prophylactic negative-pressure wound therapy after ileostomy reversal for the prevention of wound healing complications in colorectal cancer patients: A randomized controlled trial. Tech. Coloproctol. 2021, 25, 185–193. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harries, R.L.; Ansell, J.; Codd, R.J.; Williams, G.L. A systematic review of Clostridium difficile infection following reversal of ileostomy and colostomy. Color. Dis. 2021, 23, 1837–1848. [Google Scholar]
- Richards, S.J.G.; Udayasiri, D.K.; Jones, I.T.; Hastie, I.A.; Chandra, R.; McCormick, J.; Chittleborough, T.J.; Read, D.J.; Hayes, I.P. Delayed ileostomy closure increases the odds of Clostridium difficile infection. Color. Dis. 2021, 23, 3213–3219. [Google Scholar] [CrossRef]
- Cheng, H.-H.; Shao, Y.-C.; Lin, C.-Y.; Chiang, T.-W.; Chen, M.-C.; Chiu, T.-Y.; Huang, Y.-L.; Chen, C.-C.; Chen, C.-P.; Chiang, F.-F. Impact of chemiotherapy on surgical outcomes in ileostomy reversal: A propensity score matching study from a single center. Tech. Coloproctol. 2023, 12, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
| Early Closure (<4 m) | Standard Closure (4–6 m) | Delayed Closure (>6 m) | p | |
| Number of patients, n (%) | 35 | 70 | 54 | |
| Demographics | ||||
| Females, n (%) | 19 (54.3%) | 16 (22.9%) | 18 (33.3%) | <0.05 |
| Males, n (%) | 16 (45.7%) | 54 (77.1%) | 36 (66.7%) | |
| Median age, (q1–q3) | 65 (57–71) | 64 (54–69) | 66 (59–71) | 0.635 |
| Median BMI, kg/m2 (q1–q3) | 25.5 (22.4–27.2) | 26.4 (23–29.2) | 26.2 (23.5–28.4) | 0.313 |
| ASA 1, n (%) | 1 (2.9%) | 6 (8.6%) | 2 (3.7%) | 0.55 |
| ASA 2, n (%) | 20 (57.1%) | 44 (62.8%) | 33 (61.1%) | |
| ASA 3, n (%) | 14 (40%) | 20 (28.6%) | 19 (35.2%) | |
| Ischemic heart disease, n (%) | 3 (8.6%) | 6 (8.6%) | 6 (11.1) | 0.87 |
| Hypertension, n (%) | 17 (48.6%) | 32 (45.7%) | 23 (42.6%) | 0.85 |
| Diabetes, n (%) | 4 (11.4%) | 7 (10%) | 8 (14.8%) | 0.71 |
| Ileostomy created by specialist, n (%) | 32 (91.4%) | 69 (98.6%) | 52 (96.3%) | 00.19 |
| Ileostomy created by trainee, n (%) | 3 (8.6%) | 1 (1.4%) | 2 (3.7%) | |
| Parameter Analyzed | Early | Standard | Delayed | p |
|---|---|---|---|---|
| Ileostomy reversal performed by specialist | 23 (65.7%) | 39 (55.7%) | 38 (70.4%) | 0.45 |
| Ileostomy reversal performed by trainee | 12 (34.3%) | 30 (42.9%) | 15 (27.8%) | |
| Ileostomy reversal started by trainee but converted to specialist | - | 1 (1.4%) | 1 (1.9%) | |
| Median LOS, IQD (days) | 5 (4–8) | 5,5 (4–6) | 6 (5–8) | 0.22 |
| Complication | 12 (34.3%) | 17 (24.3%) | 18 (33.3%) | 0.43 |
| 30-day reoperation | 3 (8.6%) | 2 (2.9%) | 5 (9.3%) | 0.28 |
| Parameter Analyzed | Early | Standard | Delayed | p |
|---|---|---|---|---|
| Clavien–Dindo grade 1, n (%) | 6 (17.1%) | 6 (8.6%) | 1 (1.9%) | 0.07 |
| Clavien–Dindo grade 2, n (%) | 2 (5.7%) | 5 (7.1%) | 10 (18.5%) | |
| Clavien–Dindo grade 3, n (%) | 3 (8.6%) | 6 (8.6%) | 6 (11.1%) | |
| Clavien–Dindo grade 4, n (%) | - | - | 1 (1.9%) | |
| Clavien–Dindo grade 5, n (%) | 1 (2.9%) | - | - | |
| Wound infection, n (%) | 9 (25.7%) | 9 (12.9%) | 4 (7.4%) | 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kisielewski, M.; Pisarska-Adamczyk, M.; Dowgiałło-Gornowicz, N.; Nawacki, Ł.; Serednicki, W.; Wierdak, M.; Wilczek, J.; Safiejko, K.; Juchimiuk, M.; Domurat, M.; et al. Timing of Loop Ileostomy Closure Does Not Play a Pivotal Role in Terms of Complications—Results of the Liquidation of iLEOstomy (LILEO) Study. J. Pers. Med. 2024, 14, 934. https://doi.org/10.3390/jpm14090934
Kisielewski M, Pisarska-Adamczyk M, Dowgiałło-Gornowicz N, Nawacki Ł, Serednicki W, Wierdak M, Wilczek J, Safiejko K, Juchimiuk M, Domurat M, et al. Timing of Loop Ileostomy Closure Does Not Play a Pivotal Role in Terms of Complications—Results of the Liquidation of iLEOstomy (LILEO) Study. Journal of Personalized Medicine. 2024; 14(9):934. https://doi.org/10.3390/jpm14090934
Chicago/Turabian StyleKisielewski, Michał, Magdalena Pisarska-Adamczyk, Natalia Dowgiałło-Gornowicz, Łukasz Nawacki, Wojciech Serednicki, Mateusz Wierdak, Jerzy Wilczek, Kamil Safiejko, Marcin Juchimiuk, Marian Domurat, and et al. 2024. "Timing of Loop Ileostomy Closure Does Not Play a Pivotal Role in Terms of Complications—Results of the Liquidation of iLEOstomy (LILEO) Study" Journal of Personalized Medicine 14, no. 9: 934. https://doi.org/10.3390/jpm14090934
APA StyleKisielewski, M., Pisarska-Adamczyk, M., Dowgiałło-Gornowicz, N., Nawacki, Ł., Serednicki, W., Wierdak, M., Wilczek, J., Safiejko, K., Juchimiuk, M., Domurat, M., Pierko, J., Mucha, M., Fiedorowicz, W., Wysocki, M., Ladziński, M., Zdrojewski, M., Sachańbiński, T., Wojewoda, T., Chochla, V., ... LILEO Study Group. (2024). Timing of Loop Ileostomy Closure Does Not Play a Pivotal Role in Terms of Complications—Results of the Liquidation of iLEOstomy (LILEO) Study. Journal of Personalized Medicine, 14(9), 934. https://doi.org/10.3390/jpm14090934







