Fertility Preservation in the Era of Immuno-Oncology: Lights and Shadows
Abstract
1. Introduction
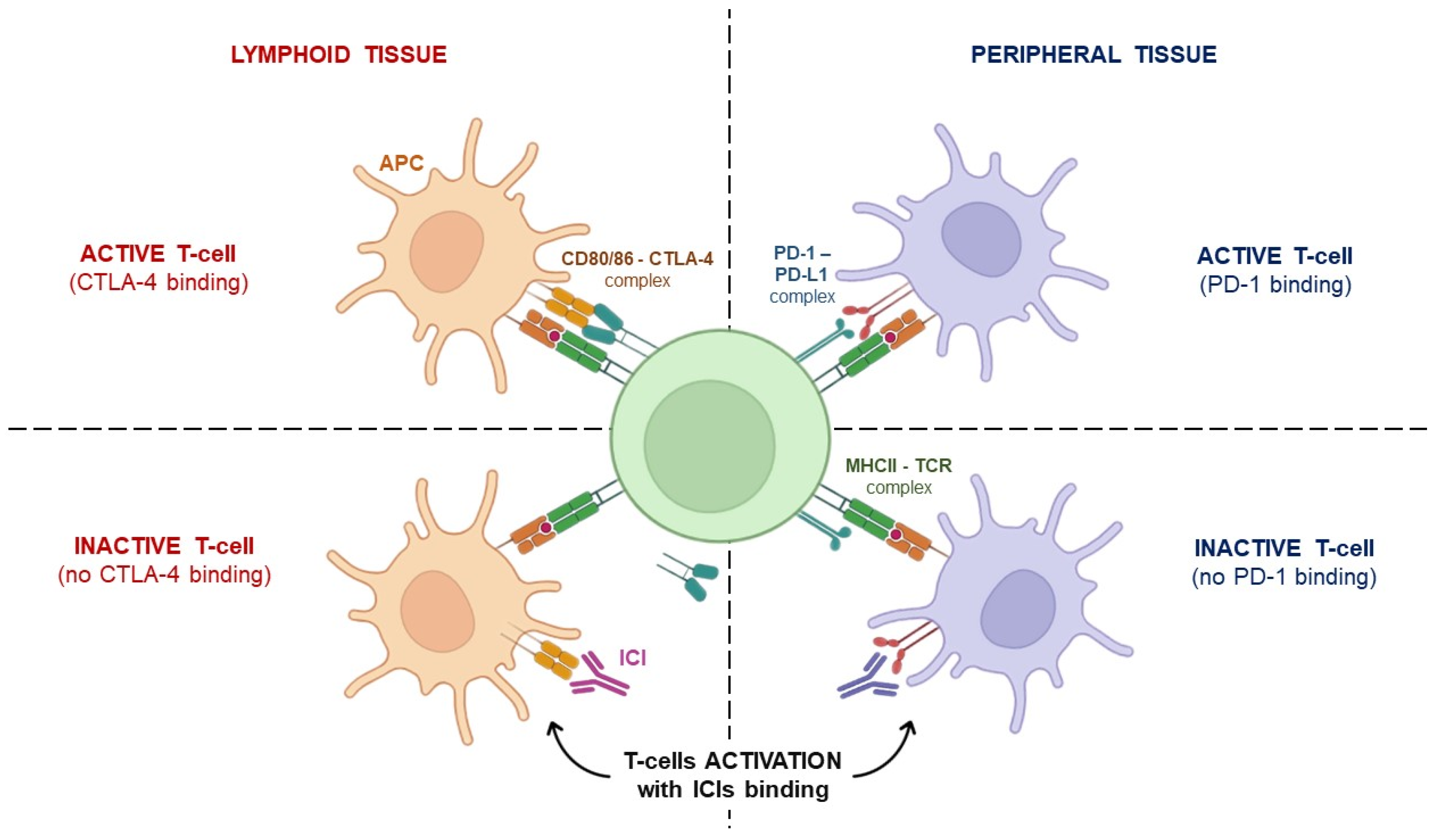
2. Immunotherapy: From Concept to Clinical Application
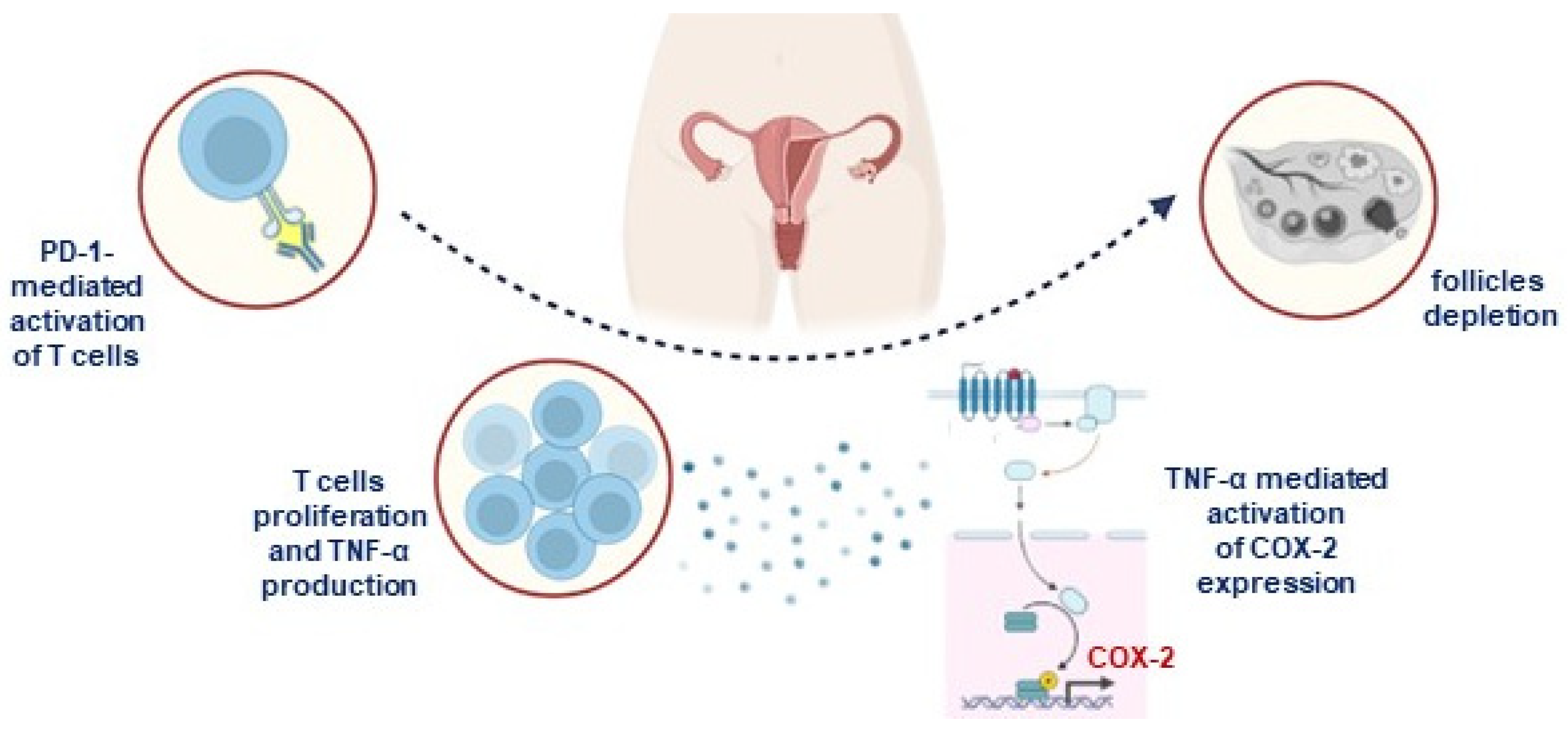
3. ICIs’ Impact on Female Fertility
4. Fertility Preservation Procedures for Immunotherapy-Treated Patients
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. “Infertility”. 2020. Available online: www.who.int/news-room/fact-sheets/detail/infertility (accessed on 8 July 2022).
- Serafin, D.; Grabarek, B.O.; Boroń, D.; Madej, A.; Cnota, W.; Czuba, B. Evaluation of the Risk of Birth Defects Related to the Use of Assisted Reproductive Technology: An Updated Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 4914. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.; Chi, D.S.; Brown, C.L.; Abu-Rustum, N.R.; Sonoda, Y.; Aghajanian, C.; Levine, D.A.; Baser, R.E.; Raviv, L.; Barakat, R.R. Cancer related infertility in survirorship. Int. J. Gynecol. Cancer 2010, 20, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Penrose, R.; Beatty, L.; Mattiske, J.; Koczwara, B. The psychosocial impact of cancer-related infertility on women: Are view and comparison. Clin. J. Oncol. Nurs. 2013, 17, 188–193. [Google Scholar] [CrossRef]
- Blumenfeld, Z.; vonWolff, M. GnRH-analogues and oral contraceptives for fertility preservation in women during chemotherapy. Hum. Reprod. Update 2008, 14, 543–552. [Google Scholar] [CrossRef]
- Farhud, D.D.; Zokaei, S.; Keykhaei, M.; Hedayati, M.; Yeganeh, M. In-vitro fertilization impact on the risk of breast cancer: Are view article. Iran. J. Public Health 2021, 50, 438–447. [Google Scholar] [CrossRef]
- Bedoschi, G.; Navarro, P.A.; Oktay, K. Chemotherapy-induced damage of ovary: Mechanisms and clinical impact. Future Oncol. 2016, 12, 2333–2344. [Google Scholar] [CrossRef] [PubMed]
- Pawłowski, P.; Ziętara, K.J.; Michalczyk, J.; Fryze, M.; Buchacz, A.; Zaucha-Prażmo, A.; Zawitkowska, J.; Torres, A.; Samardakiewicz, M. Fertility Preservation in Children and Adolescents during Oncological Treatment-A Review of Healthcare System Factors and Attitudes of Patients and Their Caregivers. Cancers 2023, 15, 4393. [Google Scholar] [CrossRef]
- Meirow, D.; Levron, J.; Eldar Geva, T.; Hardan, I.; Fridman, E.; Zalel, Y.; Schiff, E.; Dor, J. Pregnancy after transplantation of cryopreserved ovarian tissue in patient with ovarian failure after chemotherapy. N. Engl. J. Med. 2005, 353, 318–321. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.K.; Lee, S.C.; Kim, K.J.; Han, C.H.; Kim, J.H. In-vitro maturation, fertilization, and development of human germinal vesicle oocytes collected from stimulated cycles. Fertil. Steril. 2000, 74, 1153–1158. [Google Scholar] [CrossRef]
- Pacheco, F.; Oktay, K. Current success and efficiency of autologous ovarian transplantation: A meta-analysis. Reprod. Sci. 2017, 24, 1111–1120. [Google Scholar] [CrossRef]
- Dolmans, M.; Luyckx, V.; Donnez, J.; Andersen, C.; Greve, T. Risk of transferring malignant cells with transplanted frozen-thawed ovarian tissue. Fertil. Steril. 2013, 99, 1514–1522. [Google Scholar] [CrossRef] [PubMed]
- Telfer, E.E.; Grosbois, J.; Odey, Y.L.; Rosario, R.; Anderson, R.A. Making a good egg: Human oocyte health, aging, and in vitro development. Physiol. Rev. 2023, 103, 2623–2677. [Google Scholar] [CrossRef] [PubMed]
- Bendsen, E.; Byskov, A.G.; Andersen, C.Y.; Westergaard, L.G. Number of germ cells and somatic cells in human fetal ovaries during the first weeks after sex differentiation. Hum. Reprod. 2006, 21, 30–35. [Google Scholar] [CrossRef]
- Zuckerman, S. The number of oocytes in the mature ovary. Rec. Prog. Horm. Res. 1951, 6, 63–108. [Google Scholar]
- Silvestris, E.; Cafforio, P.; D‘Oronzo, S.; Felici, C.; Silvestris, F.; Loverro, G. In vitro differentiation of human oocyte-like cells from oogonial stem cells: Single-cell isolation and molecular characterization. Hum. Reprod. 2018, 33, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Del-Pozo-Lérida, S.; Salvador, C.; Martínez-Soler, F.; Tortosa, A.; Perucho, M.; Giménez-Bonafé, P. Preservation of fertility in patients with cancer (Review). Oncol. Rep. 2019, 41, 2607–2614. [Google Scholar] [CrossRef] [PubMed]
- Hagenäs, I.; Jørgensen, N.; Rechnitzer, C.; Sommer, P.; Holm, M.; Schmiegelow, K.; Daugaard, G.; Jacobsen, N.; Juul, A. Clinical and biochemical correlates of successful semen collection for cryopreservation from 12–18-year-old patients: A single-center study of 86 adolescents. Hum. Reprod. 2010, 25, 2031–2038. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.A.; Mitchell, R.T.; Kelsey, T.W.; Spears, N.; Telfer, E.E.; Wallace, W.H. Cancer treatment and gonadal function: Experimental and established strategies for fertility preservation in children and young adults. Lancet Diabetes Endocrinol. 2015, 3, 556–567. [Google Scholar] [CrossRef] [PubMed]
- Neto, F.T.; Bach, P.V.; Najari, B.B.; Li, P.S.; Goldstein, M. Spermatogenesis in humans and its affecting factors. Semin. Cell Dev. Biol. 2016, 59, 10–26. [Google Scholar] [CrossRef]
- Scovell, J.M.; Benz, K.; Samarska, I.; Kohn, T.P.; Hooper, J.E.; Matoso, A.; Herati, A.S. Association of Impaired Spermatogenesis With the Use of Immune Checkpoint Inhibitors in Patients With Metastatic Melanoma. JAMA Oncol. 2020, 6, 1297–1299. [Google Scholar] [CrossRef]
- Garutti, M.; Lambertini, M.; Puglisi, F. Checkpoint inhibitors, fertility, pregnancy, and sexual life: A systematic review. ESMO Open 2021, 6, 100276. [Google Scholar] [CrossRef]
- De Vos, M.; Devroey, P.; Fauser, B.C. Primary ovarian insufficiency. Lancet 2010, 376, 911–921. [Google Scholar] [CrossRef] [PubMed]
- Silveira, L.F.; Latronico, A.C. Approach to the patient with hypogonadotropic hypogonadism. J. Clin. Endocrinol. Metab. 2013, 98, 1781–1788. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Handman, F.; Cerullo, V. Cancer immunotherapies: A hope for the uncurable? Front. Mol. Med. 2023, 3, 1140977. [Google Scholar] [CrossRef]
- Garner, H.; de Visser, K.E. Immune crosstalk in cancer progression and metastatic spread: A complex conversation. Nat. Rev. Immunol. 2020, 20, 483–497. [Google Scholar] [CrossRef] [PubMed]
- Smyth, M.J.; Thia, K.Y.; Street, S.E.; MacGregor, D.; Godfrey, D.I.; Trapani, J.A. Perforin-mediated cytotoxicity is critical for surveillance of spontaneous lymphoma. J. Exp. Med. 2000, 192, 755–760. [Google Scholar] [CrossRef] [PubMed]
- Vajdic, C.M.; van Leeuwen, M.T. Cancer incidence and risk factors after solid organ transplantation. Int. J. Cancer 2009, 125, 1747–1754. [Google Scholar] [CrossRef] [PubMed]
- Vinay, D.S.; Ryan, E.P.; Pawelec, G.; Talib, W.H.; Stagg, J.; Elkord, E.; Lichtor, T.; Decker, W.K.; Whelan, R.L.; Kumara, H.S.; et al. Immune evasion in cancer: Mechanistic basis and therapeutic strategies. Semin. Cancer Biol. 2015, 35, S185–S198. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Z. The history and advances in cancer immunotherapy: Understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell Mol. Immunol. 2020, 17, 807–821. [Google Scholar] [CrossRef]
- Leach, D.R.; Krummel, M.F.; Allison, J.P. Enhancement of antitumor immunity by CTLA-4 blockade. Science 1996, 271, 1734–1736. [Google Scholar] [CrossRef] [PubMed]
- Ledford, H. Melanoma drug wins US approval. Nature 2011, 471, 561. [Google Scholar] [CrossRef] [PubMed]
- Janjigian, Y.Y.; Shitara, K.; Moehler, M.; Garrido, M.; Salman, P.; Shen, L.; Wyrwicz, L.; Yamaguchi, K.; Skoczylas, T.; Bragagnoli, A.C.; et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): A randomised, open-label, phase 3 trial. Lancet 2021, 398, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Patel, T.H.; Brewer, J.R.; Fan, J.; Cheng, J.; Shen, Y.L.; Xiang, Y.; Zhao, H.; Lemery, S.J.; Pazdur, R.; Kluetz, P.G.; et al. FDA Approval Summary: Tremelimumab in combination with durvalumab for the treatment of patients with unresectable hepatocellular carcinoma. Clin. Cancer Res. 2023, 30, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Planchard, D.; Yokoi, T.; McCleod, M.J.; Fischer, J.R.; Kim, Y.C.; Ballas, M.; Shi, K.; Soria, J.C. A Phase III Study of Durvalumab (MEDI4736) with or without Tremelimumab for Previously Treated Patients with Advanced NSCLC: Rationale and Protocol Design of the ARCTIC Study. Clin. Lung Cancer 2016, 17, 232–236.e1. [Google Scholar] [CrossRef] [PubMed]
- Rudqvist, N.P.; Avagyan, M.; Chand, D. Next-generation CTLA-4 targeting molecules and combination therapy: Promising strategies for improving cancer immunotherapy. Oncoimmunology 2023, 12, 2275333. [Google Scholar] [CrossRef]
- Sharpe, A.H.; Pauken, K.E. The diverse functions of the PD1 inhibitory pathway. Nat. Rev. Immunol. 2018, 18, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Waldman, A.D.; Fritz, J.M.; Lenardo, M.J. A guide to cancer immunotherapy: From T cell basic science to clinical practice. Nat. Rev. Immunol. 2020, 20, 651–668. [Google Scholar] [CrossRef]
- Marei, H.E.; Hasan, A.; Pozzoli, G.; Cenciarelli, C. Cancer immunotherapy with immune checkpoint inhibitors (ICIs): Potential, mechanisms of resistance, and strategies for reinvigorating T cell responsiveness when resistance is acquired. Cancer Cell Int. 2023, 23, 64. [Google Scholar] [CrossRef]
- Taylor, J.; Gandhi, A.; Gray, E.; Zaenker, P. Checkpoint inhibitor immune-related adverse events: A focused review on autoantibodies and B cells as biomarkers, advancements and future possibilities. Front. Immunol. 2023, 13, 991433. [Google Scholar] [CrossRef]
- Haanen, J.; Obeid, M.; Spain, L.; Carbonnel, F.; Wang, Y.; Robert, C.; Lyon, A.R.; Wick, W.; Kostine, M.; Peters, S.; et al. Management of toxicities from Immunotherapy: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022, 33, 1217–1238. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.J.; Powers, A.C.; Johnson, D.B. Endocrine toxicities of immune checkpoint inhibitors. Nat. Rev. Endocrinol. 2021, 17, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Brahmer, J.R.; Lacchetti, C.; Schneider, B.J.; Atkins, M.B.; Brassil, K.J.; Caterino, J.M.; Chau, I.; Ernstoff, M.S.; Gardner, J.M.; Ginex, P.; et al. Management of immune-related adverse events in patients treated with immune Checkpoint inhibitor therapy: ASCO guideline update. J. Clin. Oncol. 2021, 39, 4073–4126. [Google Scholar] [CrossRef]
- Calabrese, L.; Velcheti, V. Check point immunotherapy: Good for cancer therapy, bad for rheumatic diseases. Ann. Rheum. Dis. 2017, 76, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Barron, C.C.; Stefanova, I.; Cha, Y.; Elsolh, K.; Zereshkian, A.; Gaafour, A.; McWhirter, E. Chronic immune-related adverse events in patients with cancer receiving immune checkpoint inhibitors: A systematic review. J. Immunother. Cancer 2023, 11, e006500. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.B.; Nebhan, C.A.; Moslehi, J.J.; Balko, J.M. Immune checkpoint inhibitors: Long-term implications of toxicity. Nat. Rev. Clin. Oncol. 2022, 19, 254–267. [Google Scholar] [CrossRef] [PubMed]
- Poto, R.; Troiani, T.; Criscuolo, G.; Marone, G.; Ciardiello, F.; Tocchetti, C.G.; Varricchi, G. Holistic Approach to Immune Checkpoint Inhibitor-Related Adverse Events. Front. Immunol. 2022, 13, 804597. [Google Scholar] [CrossRef] [PubMed]
- Duma, N.; Lambertini, M. It Is Time to Talk About Fertility and Immunotherapy. Oncologist 2020, 25, 277–278. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, B.C. Immune checkpoint inhibitor-related hypogonadism and infertility: A neglected issue in immuno-oncology. J. Immunother. Cancer 2021, 9, e002220. [Google Scholar] [CrossRef]
- Walter, J.R.; Xu, S.; Paller, A.S.; Choi, J.N.; Woodruff, T.K. Oncofertility considerations in adolescents and young adults given a diagnosis of melanoma: Fertility risk of food and drug administration-approved systemic therapies. J. Am. Acad. Dermatol. 2016, 75, 528–534. [Google Scholar] [CrossRef]
- Chen, Z.; Huang, J.; Kwak-Kim, J.; Wang, W. Immune checkpoint inhibitors and reproductive failures. J. Reprod. Immunol. 2023, 156, 103799. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.C.; Luan, Y.; Yu, S.Y.; Xu, J.; Coulter, D.W.; Kim, S.Y. Effects of PD-1 blockade on ovarian follicles in a prepubertal female mouse. J. Endocrinol. 2021, 252, 15–30. [Google Scholar] [CrossRef]
- Winship, A.L.; Alesi, L.R.; Sant, S.; Stringer, J.M.; Cantavenera, A.; Hegarty, T.; Requesens, C.L.; Liew, S.H.; Sarma, U.; Griffiths, M.J.; et al. Checkpoint inhibitor immunotherapy diminishes oocyte number and quality in mice. Nat. Cancer 2022, 3, 1–13. [Google Scholar] [CrossRef] [PubMed]
- de Filette, J.; Andreescu, C.E.; Cools, F.; Bravenboer, B.; Velkeniers, B. A Systematic Review and Meta-Analysis of Endocrine-Related Adverse Events Associated with Immune Checkpoint Inhibitors. Horm. Metab. Res. 2019, 51, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Lin, X.; Zheng, K.; Chen, X.; Wu, X.; Huang, Y.; Zhuang, Y. Mapping endocrine toxicity spectrum of immune checkpoint inhibitors: A disproportionality analysis using the WHO adverse drug reaction database, VigiBase. Endocrine 2020, 69, 670–681. [Google Scholar] [CrossRef] [PubMed]
- Esteves-Ferreira, S.; Rosinha, P. Immune checkpoint inhibitor-induced hypophysitis: Clinical and biochemical features. J. Cancer Res. Clin. Oncol. 2023, 149, 7925–7932. [Google Scholar] [CrossRef] [PubMed]
- Tuerxun, H.; Zhao, Y.; Li, Y.; Liu, X.; Wen, S.; Cao, J.; Cui, J.; Zhao, Y. Immune checkpoint inhibitors as a threat to reproductive function: A systematic review. Crit. Rev. Oncol. Hematol. 2023, 188, 104064. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Iwama, S.; Sugiyama, D.; Yasuda, Y.; Okuji, T.; Ito, M.; Ito, S.; Sugiyama, M.; Onoue, T.; Takagi, H.; et al. Anti-pituitary antibodies and susceptible human leukocyte antigen alleles as predictive biomarkers for pituitary dysfunction induced by immune checkpoint inhibitors. J. Immunother. Cancer 2021, 9, e002493. [Google Scholar] [CrossRef]
- Albarel, F.; Gaudy, C.; Castinetti, F.; Carré, T.; Morange, I.; Conte-Devolx, B.; Grob, J.J.; Brue, T. Long-term follow-up of ipilimumab-induced hypophysitis, a common adverse event of the anti-CTLA-4 antibody in melanoma. Eur. J. Endocrinol. 2015, 172, 195–204. [Google Scholar] [CrossRef]
- Faje, A.T.; Sullivan, R.; Lawrence, D.; Tritos, N.A.; Fadden, R.; Klibanski, A.; Nachtigall, L. Ipilimumab-induced hypophysitis: A detailed longitudinal analysis in a large cohort of patients with metastatic melanoma. J. Clin. Endocrinol. Metab. 2014, 99, 4078–4085. [Google Scholar] [CrossRef]
- Kanie, K.; Iguchi, G.; Bando, H.; Urai, S.; Shichi, H.; Fujita, Y.; Matsumoto, R.; Suda, K.; Yamamoto, M.; Fukuoka, H.; et al. Mechanistic insights into immune checkpoint inhibitor-related hypophysitis: A form of paraneoplastic syndrome. Cancer Immunol. Immunother. 2021, 70, 3669–3677. [Google Scholar] [CrossRef] [PubMed]
- Noseda, R.; Müller, L.; Bedussi, F.; Fusaroli, M.; Raschi, E.; Ceschi, A. Immune checkpoint inhibitors and pregnancy: Analysis of the VigiBase® spontaneous reporting system. Cancers 2022, 15, 173. [Google Scholar] [CrossRef]
- Poulet, F.M.; Wolf, J.J.; Herzyk, D.J.; DeGeorge, J.J. An evaluation of the impact of PD-1 pathway blockade on reproductive safety of therapeutic PD-1 inhibitors. Birth Defects Res. B Dev. Reprod. Toxicol. 2016, 107, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.E.; Nelson, A.; Stimpert, K.; Flyckt, R.L.; Thirumavalavan, N.; Baker, K.C.; Weinmann, S.C.; Hoimes, C.J. Minding the bathwater: Fertility and reproductive toxicity in the age of immuno-oncology. JCO Oncol. Pract. 2022, 18, 815–822. [Google Scholar] [CrossRef]
- Mittra, A.; Naqash, A.R.; Murray, J.H.; Finnigan, S.; Kwak-Kim, J.; Ivy, S.P.; Chen, A.P.; Sharon, E. Outcomes of Pregnancy During Immunotherapy Treatment for Cancer: Analysis of Clinical Trials Sponsored by the National Cancer Institute. Oncologist 2021, 26, e1883–e1886. [Google Scholar] [CrossRef]
- Oktay, K.; Harvey, B.E.; Partridge, A.H.; Quinn, G.P.; Reinecke, J.; Taylor, H.S.; Wallace, W.H.; Wang, E.T.; Loren, A.W. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 1994–2001. [Google Scholar] [CrossRef] [PubMed]
- McClam, M.; Xiao, S. Preserving Oocytes in Oncofertility. Biol. Reprod. 2022, 106, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Arslan, M.; Bocca, S.; Mirkin, S.; Barroso, G.; Stadtmauer, L.; Oehninger, S. Controlled ovarian hyperstimulation protocols for in vitro fertilization: Two decades of experience after the birth of Elizabeth Carr. Fertil. Steril. 2005, 84, 555–569. [Google Scholar] [CrossRef]
- Bonardi, B.; Massarotti, C.; Bruzzone, M.; Goldrat, O.; Mangili, G.; Anserini, P.; Spinaci, S.; Arecco, L.; Del Mastro, L.; Ceppi, M.; et al. Efficacy and Safety of Controlled Ovarian Stimulation With or Without Letrozole Co-administration for Fertility Preservation: A Systematic Review and Meta-Analysis. Front. Oncol. 2020, 10, 574669. [Google Scholar] [CrossRef]
- Vo, K.C.T.; Kawamura, K. Female Oncofertility: Current Understandings, Therapeutic Approaches, Controversies, and Future Perspectives. J. Clin. Med. 2021, 10, 5690. [Google Scholar] [CrossRef]
- Valsamakis, G.; Valtetsiotis, K.; Charmandari, E.; Lambrinoudaki, I.; Vlahos, N.F. GnRH Analogues as a Co-Treatment to Therapy in Women of Reproductive Age with Cancer and Fertility Preservation. Int. J. Mol. Sci. 2022, 23, 2287. [Google Scholar] [CrossRef] [PubMed]
- Ortmann, O.; Weiss, J.M.; Diedrich, K. Gonadotrophin-releasing hormone (GnRH) and GnRH agonists: Mechanisms of action. Reprod. Biomed. Online 2002, 5 (Suppl. 1), 1–7. [Google Scholar] [CrossRef] [PubMed]
- Practice Committee of the American Society for Reproductive Medicine. Prevention and treatment of moderate and severe ovarian hyperstimulation syndrome: A guideline. Fertil. Steril. 2016, 106, 1634–1647. [Google Scholar] [CrossRef] [PubMed]
- Ovarian Stimulation TEGGO; Bosch, E.; Broer, S.; Griesinger, G.; Grynberg, M.; Humaidan, P.; Kolibianakis, E.; Kunicki, M.; La Marca, A.; Lainas, G.; et al. ESHRE guideline: Ovarian stimulation for IVF/ICSI. Hum. Reprod. Open 2020, 2020, hoaa009. [Google Scholar] [CrossRef]
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: A committee opinion. Fertil. Steril. 2019, 112, 1022–1033. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; Pappo, A.S.; Acquazzino, M.; Allen-Rhoades, W.A.; Barnett, M.; Borinstein, S.C.; Casey, R.; Choo, S.; Chugh, R.; Dinner, S.; et al. Adolescent and Young Adult (AYA) Oncology, Version 2.2024, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2023, 21, 851–880. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.; Canning, J.; Kaneko, T.; Pru, J.K.; Tilly, J.L. Germline stem cells and follicular renewal in the postnatal mammalian ovary. Nature 2004, 428, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Green, S.H.; Zuckerman, S. Quantitative aspects of the growth of the human ovum and follicle. J. Anat. 1951, 85, 373–375. [Google Scholar] [PubMed]
- Telfer, E.; Albertini, D. The quest for human ovarian stem cells. Nat. Med. 2012, 18, 353–354. [Google Scholar] [CrossRef]
- Zou, K.; Yuan, Z.; Yang, Z.; Luo, H.; Sun, K.; Zhou, L.; Xiang, J.; Shi, L.; Yu, Q.; Zhang, Y.; et al. Production of offspring from a germline stem cell line derived from neonatal ovaries. Nat. Cell Biol. 2009, 11, 631–636. [Google Scholar] [CrossRef]
- Parte, S.; Bhartiya, D.; Telang, J.; Daithankar, V.; Salvi, V.; Zaveri, K.; Hinduja, I. Detection characterization, and spontaneous differentiation in vitro of very. Small embryonic-like putative stem cells in adult mammalian ovary. Stem Cells Dev. 2011, 20, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, M.; Albertini, D.F.; Wallace, W.H.B.; Anderson, R.A.; Telfer, E.E. Metaphase II oocytes from human unilaminar grown in a multi- step culture system. Mol. Hum. Reprod. 2018, 24, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Egea, R.R.; Puchalt, N.G.; Escrivá, M.M.; Varghese, A.C. OMICS: Current and future perspectives in reproductive medicine and technology. J. Hum. Reprod. Sci. 2014, 7, 73–92. [Google Scholar] [CrossRef]
- Zhang, X.; Jafari, N.; Barnes, R.B.; Confino, E.; Milad, M.; Kazer, R.R. Studies of gene expression in human cumulus cells indicate pentraxin 3 as a possible marker for oocyte quality. Fertil. Steril. 2005, 83 (Suppl. 1), 1169–1179. [Google Scholar] [CrossRef] [PubMed]
- Swain, J.; VerMilyea, M.T.; Meseguer, M.; Ezcurra, D.; Fertility AI Forum Group. AI in the treatment of fertility: Key considerations. J. Assist. Reprod. Genet. 2020, 37, 2817–2824. [Google Scholar] [CrossRef] [PubMed]
- Shen, D.; Wu, G.; Suk, H.I. Deep Learning in Medical Image Analysis. Annu. Rev. Biomed. Eng. 2017, 19, 221–248. [Google Scholar] [CrossRef]
- Shin, H.C.; Roth, H.R.; Gao, M.; Lu, L.; Xu, Z.; Nogues, I.; Yao, J.; Mollura, D.; Summers, R.M. Deep Convolutional Neural Networks for Computer-Aided Detection: CNN Architectures, Dataset Characteristics and Transfer Learning. IEEE Trans. Med. Imaging 2016, 35, 1285–1298. [Google Scholar] [CrossRef]
| Method | Purpose | Results | Pros | Cons |
|---|---|---|---|---|
| Embryo cryostorage | immediate oocytes fertilization | first choice among ART | optimized efficacy | ethical problems |
| Oocyte cryopreservation | egg integrity | best choice (with embryo cryopres.) | 30–45% efficacy | 2–3 week hormone stimulation |
| GnRHa ovarian suppression | gonadotrophins inhibition | endocrine protection | outcomes in BC: >65% | adverse iatrogenic complication |
| Ovarian cortex cryopreservation | avoiding COH | ovarian function recovery in >90% of cases | suitable for prepubertal females | risk of cancer cell reimplantation |
| Ovarian stem cells | in vitro oocytes differentiation | still experimental | genetic analysis of single cell | technician expertise |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silvestris, E.; D’Oronzo, S.; Petracca, E.A.; D’Addario, C.; Cormio, G.; Loizzi, V.; Canosa, S.; Corrado, G. Fertility Preservation in the Era of Immuno-Oncology: Lights and Shadows. J. Pers. Med. 2024, 14, 431. https://doi.org/10.3390/jpm14040431
Silvestris E, D’Oronzo S, Petracca EA, D’Addario C, Cormio G, Loizzi V, Canosa S, Corrado G. Fertility Preservation in the Era of Immuno-Oncology: Lights and Shadows. Journal of Personalized Medicine. 2024; 14(4):431. https://doi.org/10.3390/jpm14040431
Chicago/Turabian StyleSilvestris, Erica, Stella D’Oronzo, Easter Anna Petracca, Claudia D’Addario, Gennaro Cormio, Vera Loizzi, Stefano Canosa, and Giacomo Corrado. 2024. "Fertility Preservation in the Era of Immuno-Oncology: Lights and Shadows" Journal of Personalized Medicine 14, no. 4: 431. https://doi.org/10.3390/jpm14040431
APA StyleSilvestris, E., D’Oronzo, S., Petracca, E. A., D’Addario, C., Cormio, G., Loizzi, V., Canosa, S., & Corrado, G. (2024). Fertility Preservation in the Era of Immuno-Oncology: Lights and Shadows. Journal of Personalized Medicine, 14(4), 431. https://doi.org/10.3390/jpm14040431









