Nationwide Analysis of Glaucoma Surgeries in Fiscal Years of 2014 and 2020 in Japan
Abstract
1. Introduction
2. Subjects and Methods
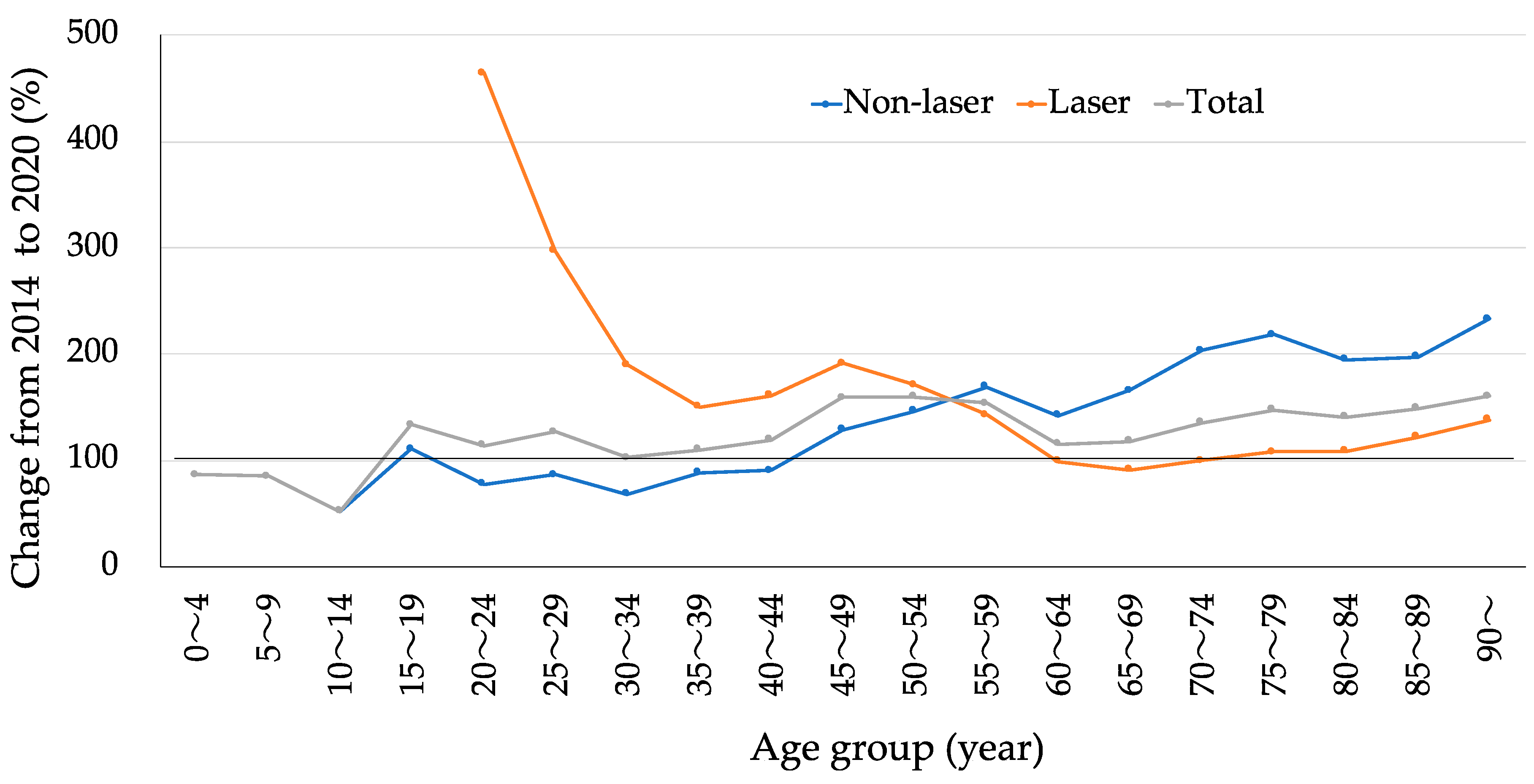
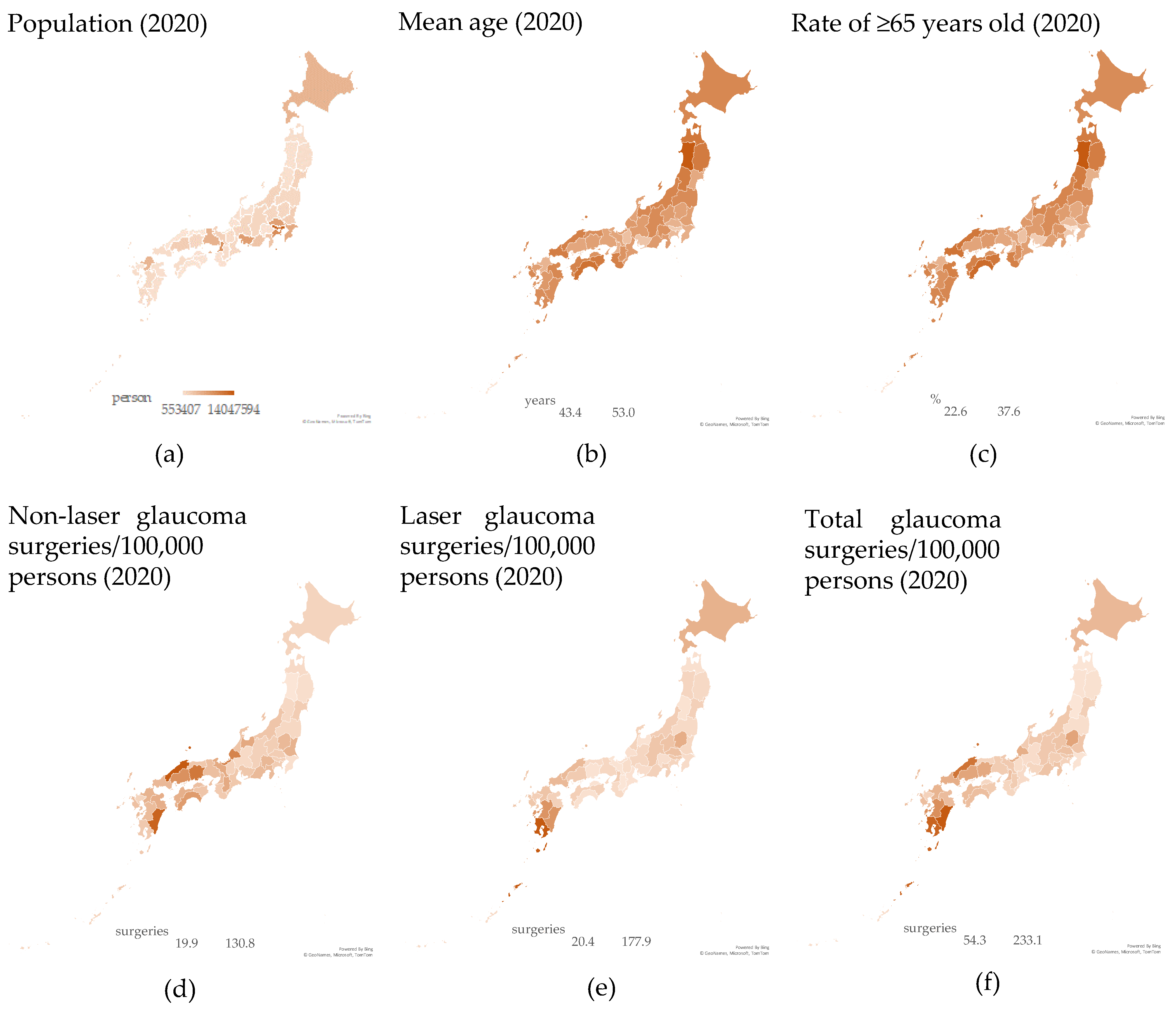
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burton, M.J.; Ramke, J.; Marques, A.P.; Bourne, R.R.A.; Congdon, N.; Jones, I.; Ah Tong, B.A.M.; Arunga, S.; Bachani, D.; Bascaran, C.; et al. The Lancet Global Health Commission on Global Eye Health: Vision beyond 2020. Lancet Glob. Health 2021, 9, e489–e551. [Google Scholar] [CrossRef] [PubMed]
- Tham, Y.C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef] [PubMed]
- Flaxman, S.R.; Bourne, R.R.A.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global causes of blindness and distance vision impairment 1990-2020: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Iwase, A.; Araie, M.; Suzuki, Y.; Abe, H.; Shirato, S.; Kuwayama, Y.; Mishima, H.K.; Shimizu, H.; Tomita, G.; et al. The Tajimi Study report 2: Prevalence of primary angle closure and secondary glaucoma in a Japanese population. Ophthalmology 2005, 112, 1661–1669. [Google Scholar] [CrossRef]
- Tanito, M. Nation-Wide Analysis of Glaucoma Medication Prescription in Fiscal Year of 2019 in Japan. J Pers Med. 2022, 12, 956. [Google Scholar] [CrossRef]
- Tanito, M.; Matsuo, M. Ab-interno trabeculotomy-related glaucoma surgeries. Taiwan J. Ophthalmol. 2019, 9, 67–71. [Google Scholar] [CrossRef]
- Tanito, M.; Matsuoka, Y. Proportion of Glaucoma Types and Surgeries Among Young, Pre-Old, Old, and Oldest-Old Age Groups or Different Sex Groups. Clin. Ophthalmol. 2022, 16, 1815–1819. [Google Scholar] [CrossRef]
- Tanito, M.; Sugihara, K.; Hara, K.; Takai, Y. Different glaucoma types and glaucoma surgeries among different age groups. Graefes Arch. Clin. Exp. Ophthalmol. 2018, 256, 2013–2014. [Google Scholar] [CrossRef]
- Fujita, A.; Hashimoto, Y.; Matsui, H.; Yasunaga, H.; Aihara, M. Recent trends in glaucoma surgery: A nationwide database study in Japan, 2011–2019. Jpn J. Ophthalmol. 2022, 66, 183–192. [Google Scholar] [CrossRef]
- Baudouin, C.; Rouland, J.F.; Le Pen, C. Changes in medical and surgical treatments of glaucoma between 1997 and 2000 in France. Eur. J. Ophthalmol. 2003, 13 (Suppl. S4), S53–S60. [Google Scholar] [CrossRef]
- van der Valk, R.; Schouten, J.S.; Webers, C.A.; Beckers, H.J.; van Amelsvoort, L.G.; Schouten, H.J.; Hendrikse, F.; Prins, M.H. The impact of a nationwide introduction of new drugs and a treatment protocol for glaucoma on the number of glaucoma surgeries. J. Glaucoma. 2005, 14, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Walland, M.J. Glaucoma treatment in Australia: Changing patterns of therapy 1994–2003. Clin. Exp. Ophthalmol. 2004, 32, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Arora, K.S.; Robin, A.L.; Corcoran, K.J.; Corcoran, S.L.; Ramulu, P.Y. Use of Various Glaucoma Surgeries and Procedures in Medicare Beneficiaries from 1994 to 2012. Ophthalmology 2015, 122, 1615–1624. [Google Scholar] [CrossRef]
- Yang, S.A.; Mitchell, W.; Hall, N.; Elze, T.; Lorch, A.C.; Miller, J.W.; Zebardast, N. Trends and Usage Patterns of Minimally Invasive Glaucoma Surgery in the United States: IRIS® Registry Analysis 2013–2018. Ophthalmol. Glaucoma. 2021, 4, 558–568. [Google Scholar] [CrossRef]
- Luebke, J.; Boehringer, D.; Anton, A.; Daniel, M.; Reinhard, T.; Lang, S. Trends in Surgical Glaucoma Treatment in Germany Between 2006 and 2018. Clin. Epidemiol. 2021, 13, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Rathi, S.; Andrews, C.A.; Greenfield, D.S.; Stein, J.D. Trends in Glaucoma Surgeries Performed by Glaucoma Subspecialists versus Nonsubspecialists on Medicare Beneficiaries from 2008 through 2016. Ophthalmology 2021, 128, 30–38. [Google Scholar] [CrossRef]
- Tanito, M. Microhook ab interno trabeculotomy, a novel minimally invasive glaucoma surgery. Clin. Ophthalmol. 2018, 12, 43–48. [Google Scholar] [CrossRef]
- Iwasaki, K.; Arimura, S.; Takamura, Y.; Inatani, M. Clinical practice preferences for glaucoma surgery in Japan: A survey of Japan Glaucoma Society specialists. Jpn J. Ophthalmol. 2020, 64, 385–391. [Google Scholar] [CrossRef]
- Latina, M.A.; Sibayan, S.A.; Shin, D.H.; Noecker, R.J.; Marcellino, G. Q-switched 532-nm Nd:YAG laser trabeculoplasty (selective laser trabeculoplasty): A multicenter, pilot, clinical study. Ophthalmology 1998, 105, 2082–2088; discussion 2089–90. [Google Scholar] [CrossRef]
- Szigiato, A.A.; Trope, G.E.; Jin, Y.; Buys, Y.M. Trends in glaucoma surgical procedures in Ontario: 1992–2012. Can. J. Ophthalmol. 2015, 50, 338–344. [Google Scholar] [CrossRef]
- Rachmiel, R.; Trope, G.E.; Chipman, M.L.; Gouws, P.; Buys, Y.M. Laser trabeculoplasty trends with the introduction of new medical treatments and selective laser trabeculoplasty. J. Glaucoma. 2006, 15, 306–309. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Vickerstaff, V.; Nathwani, N.; Garway-Heath, D.; Konstantakopoulou, E.; Ambler, G.; Bunce, C.; Wormald, R.; Barton, K.; Gazzard, G. Primary Selective Laser Trabeculoplasty for Open-Angle Glaucoma and Ocular Hypertension: Clinical Outcomes, Predictors of Success, and Safety from the Laser in Glaucoma and Ocular Hypertension Trial. Ophthalmology 2019, 126, 1238–1248. [Google Scholar] [CrossRef] [PubMed]
- Gazzard, G.; Konstantakopoulou, E.; Garway-Heath, D.; Garg, A.; Vickerstaff, V.; Hunter, R.; Ambler, G.; Bunce, C.; Wormald, R.; Nathwani, N.; et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): A multicentre randomised controlled trial. Lancet 2019, 393, 1505–1516. [Google Scholar] [CrossRef] [PubMed]
- European Glaucoma Society Terminology and Guidelines for Glaucoma, 5th Edition. Br. J. Ophthalmol. 2021, 105, 1–169. [CrossRef]
- Sarenac, T.; Bečić Turkanović, A.; Ferme, P.; Gračner, T. A Review of Selective Laser Trabeculoplasty: “The Hype Is Real”. J. Clin. Med. 2022, 11, 3879. [Google Scholar] [CrossRef]
- Souissi, S.; Le Mer, Y.; Metge, F.; Portmann, A.; Baudouin, C.; Labbé, A.; Hamard, P. An update on continuous-wave cyclophotocoagulation (CW-CPC) and micropulse transscleral laser treatment (MP-TLT) for adult and paediatric refractory glaucoma. Acta Ophthalmol. 2021, 99, e621–e653. [Google Scholar] [CrossRef]
- Newman, A.R.; Andrew, N.H. Changes in Australian practice patterns for glaucoma management. Clin. Exp. Ophthalmol. 2019, 47, 571–580. [Google Scholar] [CrossRef]
- Kim, Y.K.; Park, K.H. Comparison of 2007–2012 Korean trends in laser peripheral iridotomy and cataract surgery rates. Jpn J. Ophthalmol. 2014, 58, 40–46. [Google Scholar] [CrossRef]
- Fujita, A.; Hashimoto, Y.; Matsui, H.; Yasunaga, H.; Aihara, M. Recent Trends in Treatment and Associated Costs of Primary Angle-Closure Glaucoma: A Retrospective Cohort Study. Ophthalmol. Glaucoma. 2022, 6, 308–315. [Google Scholar] [CrossRef]
- Kiuchi, Y.; Inoue, T.; Shoji, N.; Nakamura, M.; Tanito, M. The Japan Glaucoma Society guidelines for glaucoma 5th edition. Jpn J. Ophthalmol. 2023, 67, 189–254. [Google Scholar] [CrossRef]
- Gillan, S.N.; Wilson, P.J.; Knight, D.S.; Sanders, R. Trends in Acute Primary Angle-Closure Glaucoma, Peripheral Iridotomy and Cataract Surgery in Scotland, 1998–2012. Ophthalmic Epidemiol. 2016, 23, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Breda, J.; Gonçalves-Pinho, M.; Santos, J.V.; Rocha-Sousa, A.; Abegão-Pinto, L.; Stalmans, I.; Freitas, A. Trends in Glaucoma Surgical Procedures in Portugal: A 16-Year Nationwide Study (2000–2015). J. Glaucoma. 2018, 27, 682–686. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.; Ogston, S.; Cobb, C.; MacEwen, C. Recent trends in glaucoma surgery in Scotland, England and Wales. Br. J. Ophthalmol. 2015, 99, 308–312. [Google Scholar] [CrossRef]
- Sun, M.T.; Madike, R.; Huang, S.; Cameron, C.; Selva, D.; Casson, R.J.; Wong, C.X. Changing trends in glaucoma surgery within Australia. Br. J. Ophthalmol. 2022, 106, 957–961. [Google Scholar] [CrossRef] [PubMed]
- Sugihara, K.; Fukuda, H.; Omura, T.; Tanito, M. Reasons for choice of glaucoma surgery in eyes not treated with anti-glaucoma medications. BMC Ophthalmol. 2022, 22, 145. [Google Scholar] [CrossRef]
- Boland, M.V.; Corcoran, K.J.; Lee, A.Y. Changes in Performance of Glaucoma Surgeries 1994 through 2017 Based on Claims and Payment Data for United States Medicare Beneficiaries. Ophthalmol. Glaucoma. 2021, 4, 463–471. [Google Scholar] [CrossRef]
| Code | Representative Procedures | Aggregation 1 | Aggregation 2 |
|---|---|---|---|
| K268-1 | Iridectomy | Iridectomy | Non-laser |
| K268-2 | Trabeculotomy ab externo, Trabectome, KDB, Tanito microhook, GATT, GSL | Angle surgery | |
| K268-6 | iStent | ||
| K268-3 | Trabeculectomy, NPT | Filtration surgery | |
| K268-4 | ExPRESS shunt | ||
| K268-5 | Ahmed, Bearveldt | Tube shunt | |
| K272 | Cyclocryotherapy | Ciliary coagulation | |
| K271 | Cyclophotocoagulation, micropulse cyclophotocoagulation | Laser | |
| K270 | LI, LGP | Iris laser | |
| K273 | LTP, SLT | Gonio-laser |
| Procedure | 2014 | 2020 | Change (%) |
|---|---|---|---|
| Aggregation 1 | |||
| Iridectomy | 1608 | 1209 | 75 |
| Angle surgery | 10,957 | 35,759 | 326 |
| Filtration surgery | 19,844 | 19,909 | 100 |
| Tube shunt | 817 | 3129 | 383 |
| Ciliary coagulation | 631 | 3085 | 489 |
| Iris laser | 43,518 | 33,661 | 77 |
| Gonio-laser | 10,644 | 23,903 | 225 |
| Aggregation 2 | |||
| Non-laser | 33,340 | 60,108 | 180 |
| Laser | 54,679 | 60,547 | 111 |
| Total | 88,019 | 120,655 | 137 |
| Per 100,000 capita | |||
| Non-laser | - | 47.6 | - |
| Laser | - | 48.0 | - |
| Total | - | 95.6 | - |
| Parameters | Prefectural Population (Person) | Prefectural Mean Age (Years) | Prefectural Rate of ≥65-Year-Olds (%) | |||
|---|---|---|---|---|---|---|
| Non-laser/100,000 persons | ρ = −0.17 | p = 0.24 | ρ = 0.01 | p = 0.95 | ρ = 0.08 | p = 0.58 |
| Laser/100,000 persons | 0.26 | 0.08 | −0.02 | 0.92 | 0.01 | 0.93 |
| Total/100,000 persons | 0.06 | 0.67 | 0.02 | 0.9 | 0.08 | 0.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanito, M. Nationwide Analysis of Glaucoma Surgeries in Fiscal Years of 2014 and 2020 in Japan. J. Pers. Med. 2023, 13, 1047. https://doi.org/10.3390/jpm13071047
Tanito M. Nationwide Analysis of Glaucoma Surgeries in Fiscal Years of 2014 and 2020 in Japan. Journal of Personalized Medicine. 2023; 13(7):1047. https://doi.org/10.3390/jpm13071047
Chicago/Turabian StyleTanito, Masaki. 2023. "Nationwide Analysis of Glaucoma Surgeries in Fiscal Years of 2014 and 2020 in Japan" Journal of Personalized Medicine 13, no. 7: 1047. https://doi.org/10.3390/jpm13071047
APA StyleTanito, M. (2023). Nationwide Analysis of Glaucoma Surgeries in Fiscal Years of 2014 and 2020 in Japan. Journal of Personalized Medicine, 13(7), 1047. https://doi.org/10.3390/jpm13071047






