Intraoperative Hypertension Is Associated with Postoperative Acute Kidney Injury after Laparoscopic Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
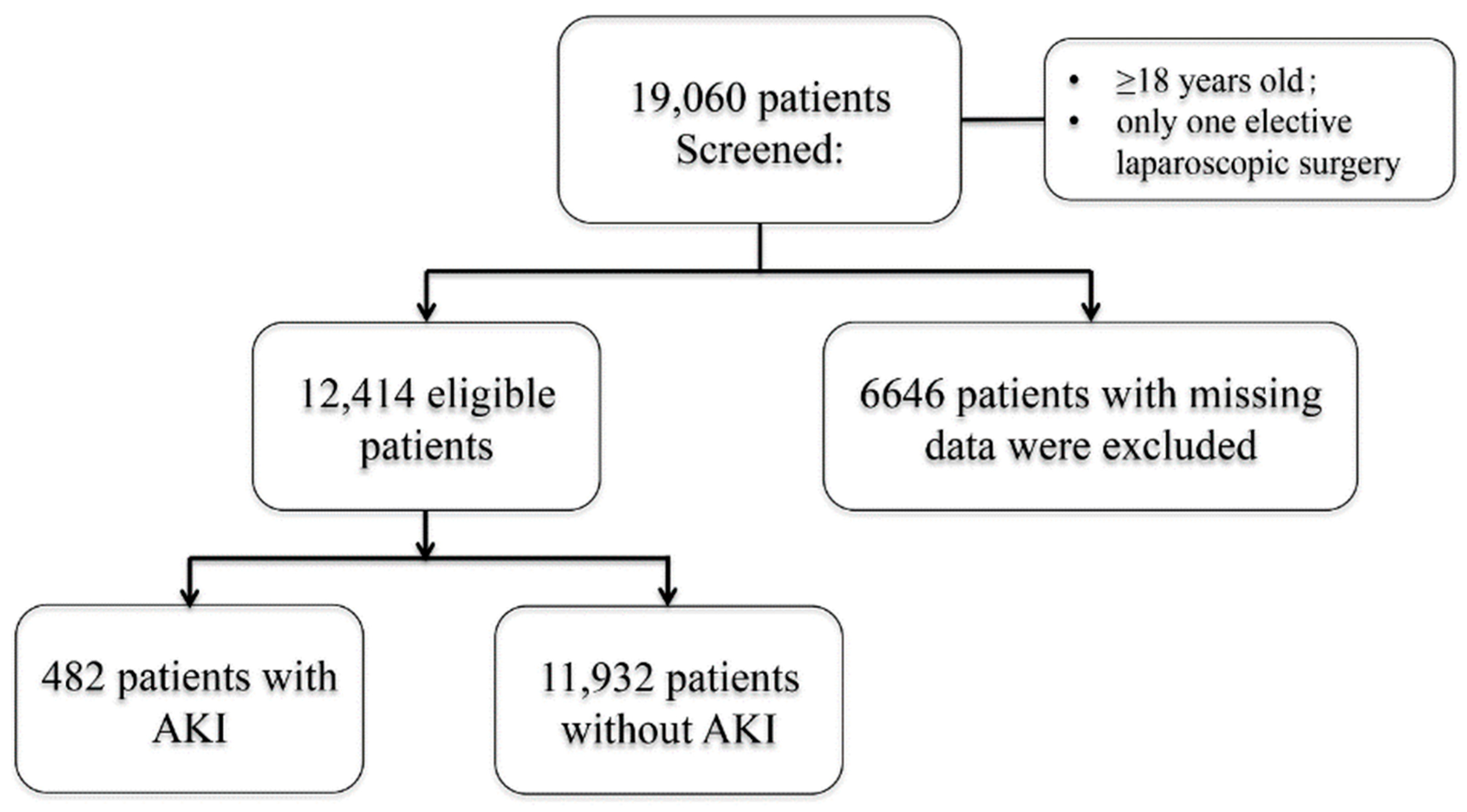
2.2. Subjects and Procedures
2.3. Intraoperative BP
2.4. Outcomes
2.5. Confounders
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Silverstein, A.; Costas-Chavarri, A.; Gakwaya, M.R.; Lule, J.; Mukhopadhyay, S.; Meara, J.G.; Shrime, M.G. Laparoscopic versus open cholecystectomy: A cost-effectiveness analysis at rwanda military hospital. World J. Surg. 2017, 41, 1225–1233. [Google Scholar] [CrossRef]
- Cox, T.C.; Huntington, C.R.; Blair, L.J.; Prasad, T.; Lincourt, A.E.; Augenstein, V.A.; Heniford, B.T. Laparoscopic appendectomy and cholecystectomy versus open: A study in 1999 pregnant patients. Surg. Endosc. 2016, 30, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Dunn, M.D.; McDougall, E.M. Renal physiology. Laparoscopic considerations. Urol. Clin. N. Am. 2000, 27, 609–614. [Google Scholar] [CrossRef] [PubMed]
- de Seigneux, S.; Klopfenstein, C.E.; Iselin, C.; Martin, P.Y. The risk of acute kidney injury following laparoscopic surgery in a chronic kidney disease patient. NDT Plus 2011, 4, 339–341. [Google Scholar] [CrossRef]
- Abdullah, H.R.; Tan, T.P.; Vaez, M.; Deb, C.; Farag, N.; Jackson, T.D.; Wong, D.T. Predictors of perioperative acute kidney injury in obese patients undergoing laparoscopic bariatric surgery: A single-centre retrospective cohort study. Obes. Surg. 2016, 26, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Gameiro, J.; Fonseca, J.A.; Marques, F.; Lopes, J.A. Management of acute kidney injury following major abdominal surgery: A contemporary review. J. Clin. Med. 2020, 9, 2679. [Google Scholar] [CrossRef]
- Zarbock, A.; Koyner, J.L.; Hoste, E.A.J.; Kellum, J.A. Update on perioperative acute kidney injury. Anesth. Analg. 2018, 127, 1236–1245. [Google Scholar] [CrossRef]
- Corredor, C.; Thomson, R.; Al-Subaie, N. Long-term consequences of acute kidney injury after cardiac surgery: A systematic review and meta-analysis. J. Cardiothorac. Vasc. Anesth. 2016, 30, 69–75. [Google Scholar] [CrossRef]
- Bucaloiu, I.D.; Kirchner, H.L.; Norfolk, E.R.; Hartle, J.E.; Perkins, R.M. Increased risk of death and de novo chronic kidney disease following reversible acute kidney injury. Kidney Int. 2012, 81, 477–485. [Google Scholar] [CrossRef]
- Zhang, W.; Wen, D.; Zou, Y.F.; Shen, P.Y.; Xu, Y.W.; Shi, H.; Xu, J.; Chen, X.N.; Chen, N. One-year survival and renal function recovery of acute kidney injury patients with chronic heart failure. Cardiorenal Med. 2015, 5, 40–47. [Google Scholar] [CrossRef]
- Moore, P.K.; Hsu, R.K.; Liu, K.D. Management of acute kidney injury: Core curriculum 2018. Am. J. Kidney Dis. 2018, 72, 136–148. [Google Scholar] [CrossRef]
- Sessler, D.I.; Bloomstone, J.A.; Aronson, S.; Berry, C.; Gan, T.J.; Kellum, J.A.; Plumb, J.; Mythen, M.G.; Grocott, M.P.W.; Edwards, M.R.; et al. Perioperative quality initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br. J. Anaesth. 2019, 122, 563–574. [Google Scholar] [CrossRef]
- Xu, N.; Long, Q.; He, T.; Liu, X.; Dai, H.; Lu, Y.; Wen, J.; Wu, Q.; Yuan, H. Association between preoperative renin-angiotensin system inhibitor use and postoperative acute kidney injury risk in patients with hypertension. Clin. Nephrol. 2018, 89, 403–414. [Google Scholar] [CrossRef]
- Liu, X.Y.; Wu, Q.Y.; Chen, Z.H.; Yan, G.Y.; Lu, Y.; Dai, H.J.; Li, Y.; Yang, P.T.; Yuan, H. Elevated triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio increased risk of hyperuricemia: A 4-year cohort study in China. Endocrine 2020, 68, 71–80. [Google Scholar] [CrossRef]
- Wen, J.; Guo, C.X.; Lu, M.G.; Lu, Y.; Huang, Y.; Liu, X.; Li, Y.; Huang, Z.J.; Zhang, Y.P.; Yuan, H. Gender-specific association between metabolic syndrome and decreased glomerular filtration rate in elderly population. Int. Urol. Nephrol. 2016, 48, 389–397. [Google Scholar] [CrossRef]
- Liu, X.; Ye, Y.; Mi, Q.; Huang, W.; He, T.; Huang, P.; Xu, N.; Wu, Q.; Wang, A.; Li, Y.; et al. A predictive model for assessing surgery-related acute kidney injury risk in hypertensive patients: A retrospective cohort study. PLoS ONE 2016, 11, e0165280. [Google Scholar] [CrossRef]
- He, P.; Wei, M.; Yao, H. Shanghai hierarchical management experience in the evaluation of maturity levels in health information interoperability standardization. Chin. Health Inform. Manag. 2016, 4, 338–341. [Google Scholar]
- Chinese Society of Cardiothoracic Anesthesia; Beijing Association of Hypertension Prevention and Treatment. Experts’ consensus on perioperative hypertension management. J. Clin. Anesthesiol. 2016, 32, 295–297. [Google Scholar]
- Bijker, J.B.; van Klei, W.A.; Kappen, T.H.; van Wolfswinkel, L.; Moons, K.G.; Kalkman, C.J. Incidence of intraoperative hypotension as a function of the chosen definition: Literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 2007, 107, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Derby, S.A. Opioid conversion guidelines for managing adult cancer pain. Am. J. Nurs. 1999, 99, 62–65. [Google Scholar]
- Palevsky, P.M.; Liu, K.D.; Brophy, P.D.; Chawla, L.S.; Parikh, C.R.; Thakar, C.V.; Tolwani, A.J.; Waikar, S.S.; Weisbord, S.D. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am. J. Kidney Dis. 2013, 61, 649–672. [Google Scholar] [CrossRef]
- Matsushita, K.; Mahmoodi, B.K.; Woodward, M.; Emberson, J.R.; Jafar, T.H.; Jee, S.H.; Polkinghorne, K.R.; Shankar, A.; Smith, D.H.; Tonelli, M.; et al. Comparison of risk prediction using the CKD-EPI equation and the MDRD study equation for estimated glomerular filtration rate. JAMA 2012, 307, 1941–1951. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Chen, Y.; Wang, Y.; Liu, M. Comparison of methods dealing with category variables with missing data. Chin. J. Health Stat. 2016, 33, 186–189. [Google Scholar]
- Huang, W.W.; Zhu, W.Z.; Mu, D.L.; Ji, X.Q.; Li, X.Y.; Ma, D.; Wang, D.X. Intraoperative hypotension is associated with shortened overall survival after lung cancer surgery. BMC Anesthesiol. 2020, 20, 160. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Devereaux, P.J.; Garg, A.X.; Kurz, A.; Turan, A.; Rodseth, R.N.; Cywinski, J.; Thabane, L.; Sessler, D.I. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: Toward an empirical definition of hypotension. Anesthesiology 2013, 119, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Monk, T.G.; Bronsert, M.R.; Henderson, W.G.; Mangione, M.P.; Sum-Ping, S.T.; Bentt, D.R.; Nguyen, J.D.; Richman, J.S.; Meguid, R.A.; Hammermeister, K.E. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology 2015, 123, 307–319. [Google Scholar] [CrossRef]
- Maheshwari, K.; Turan, A.; Mao, G.; Yang, D.; Niazi, A.K.; Agarwal, D.; Sessler, D.I.; Kurz, A. The association of hypotension during non-cardiac surgery, before and after skin incision, with postoperative acute kidney injury: A retrospective cohort analysis. Anaesthesia 2018, 73, 1223–1228. [Google Scholar] [CrossRef]
- Wu, X.; Jiang, Z.; Ying, J.; Han, Y.; Chen, Z. Optimal blood pressure decreases acute kidney injury after gastrointestinal surgery in elderly hypertensive patients: A randomized study: Optimal blood pressure reduces acute kidney injury. J. Clin. Anesth. 2017, 43, 77–83. [Google Scholar] [CrossRef]
- Saito, S.; Uchino, S.; Takinami, M.; Uezono, S.; Bellomo, R. Postoperative blood pressure deficit and acute kidney injury progression in vasopressor-dependent cardiovascular surgery patients. Crit. Care 2016, 20, 74. [Google Scholar] [CrossRef]
- Wolfsthal, S.D. Is blood pressure control necessary before surgery? Med. Clin. N. Am. 1993, 77, 349–363. [Google Scholar] [CrossRef]
- Huang, D.; Zhou, J.; Su, D.; Yu, W.; Chen, J. Variations of perioperative baroreflex sensitivity in hypertensive and normotensive patients. Clin. Exp. Hypertens. 2017, 39, 74–79. [Google Scholar] [CrossRef]
- Ramos, L.P.J.; Araujo, R.B.; Castro, M.; Ramos, M.; Cunha, E.S.J.A.; Iglesias, A.C. Hemodynamic evaluation of elderly patients during laparoscopic cholecystectomy. Rev. Colégio Bras. Cir. 2018, 45, e1659. [Google Scholar] [CrossRef]
- Kalmar, A.F.; Foubert, L.; Hendrickx, J.F.; Mottrie, A.; Absalom, A.; Mortier, E.P.; Struys, M.M. Influence of steep Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br. J. Anaesth. 2010, 104, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Ono, N.; Nakahira, J.; Nakano, S.; Sawai, T.; Minami, T. Changes in cardiac function and hemodynamics during robot-assisted laparoscopic prostatectomy with steep head-down tilt: A prospective observational study. BMC Res. Notes 2017, 10, 341. [Google Scholar] [CrossRef]
- Wu, X.; Jiang, Z.; Chen, Z. Intraoperative mean arterial pressure: What is the magic level really favorable for renal function? J. Clin. Anesth. 2018, 47, 45–46. [Google Scholar] [CrossRef]
- Ostermann, M.; Liu, K. Pathophysiology of AKI. Best Pract. Res. Clin. Anaesthesiol. 2017, 31, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, T.M.; Giraud, G.D.; Togioka, B.M.; Jones, D.B.; Cigarroa, J.E. Cardiovascular and ventilatory consequences of laparoscopic surgery. Circulation 2017, 135, 700–710. [Google Scholar] [CrossRef]
- Nguyen, N.T.; Cronan, M.; Braley, S.; Rivers, R.; Wolfe, B.M. Duplex ultrasound assessment of femoral venous flow during laparoscopic and open gastric bypass. Surg. Endosc. 2003, 17, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Shuto, K.; Kitano, S.; Yoshida, T.; Bandoh, T.; Mitarai, Y.; Kobayashi, M. Hemodynamic and arterial blood gas changes during carbon dioxide and helium pneumoperitoneum in pigs. Surg. Endosc. 1995, 9, 1173–1178. [Google Scholar] [CrossRef]
- Ali, N.A.; Eubanks, W.S.; Stamler, J.S.; Gow, A.J.; Lagoo-Deenadayalan, S.A.; Villegas, L.; El-Moalem, H.E.; Reynolds, J.D. A method to attenuate pneumoperitoneum-induced reductions in splanchnic blood flow. Ann. Surg. 2005, 241, 256–261. [Google Scholar] [CrossRef]
- Miki, Y.; Iwase, K.; Kamiike, W.; Taniguchi, E.; Sakaguchi, K.; Sumimura, J.; Matsuda, H.; Nagai, I. Laparoscopic cholecystectomy and time-course changes in renal function. The effect of the retraction method on renal function. Surg. Endosc. 1997, 11, 838–841. [Google Scholar] [CrossRef] [PubMed]
- Srisawat, N.; Kongwibulwut, M.; Laoveeravat, P.; Lumplertgul, N.; Chatkaew, P.; Saeyub, P.; Latthaprecha, K.; Peerapornratana, S.; Tiranathanagul, K.; Eiam-Ong, S.; et al. The role of intraoperative parameters on predicting laparoscopic abdominal surgery associated acute kidney injury. BMC Nephrol. 2018, 19, 289. [Google Scholar] [CrossRef] [PubMed]
- Huen, S.C.; Parikh, C.R. Predicting acute kidney injury after cardiac surgery: A systematic review. Ann. Thorac. Surg. 2012, 93, 337–347. [Google Scholar] [CrossRef] [PubMed]


| MAP | IOTH | IOH | |
|---|---|---|---|
| Definition | MAP = (SBP + 2 × DBP)/3, where SBP is systolic blood pressure and DBP is diastolic blood pressure | Acute intraoperative hypertension. Acute elevations in blood pressure (≥30% or ≥140/90 mmHg or MAP ≥ 105 mmHg) during the operation. | Acute intraoperative hypotension. The intraoperative MAP decreases by more than 40% with MAP < 70 mmHg at the same time, or an isolated MAP < 60 mmHg. |
| Groups | The entire study population was divided into 9 groups based on intraoperative mean MAP: <70 mmHg, 70–75 mmHg, 75–80 mmHg, 80–85 mmHg, 85–90 mmHg, 90–95 mmHg, 95–100 mmHg, 100–105 mmHg, and ≥105 mmHg. | All patients were divided into two groups based on whether IOTH occurred. | All patients were divided into two groups based on whether IOH occurred. |
| Subgroups | 1. According to different periods of surgery, we explored associations between intraoperative blood pressure and AKI during anesthesia induction (i.e., the time between intubation and skin incision), after skin incision (specifically, 30 min after skin incision), and during emergence from general anesthesia (the time between completion of surgery and extubation). | ||
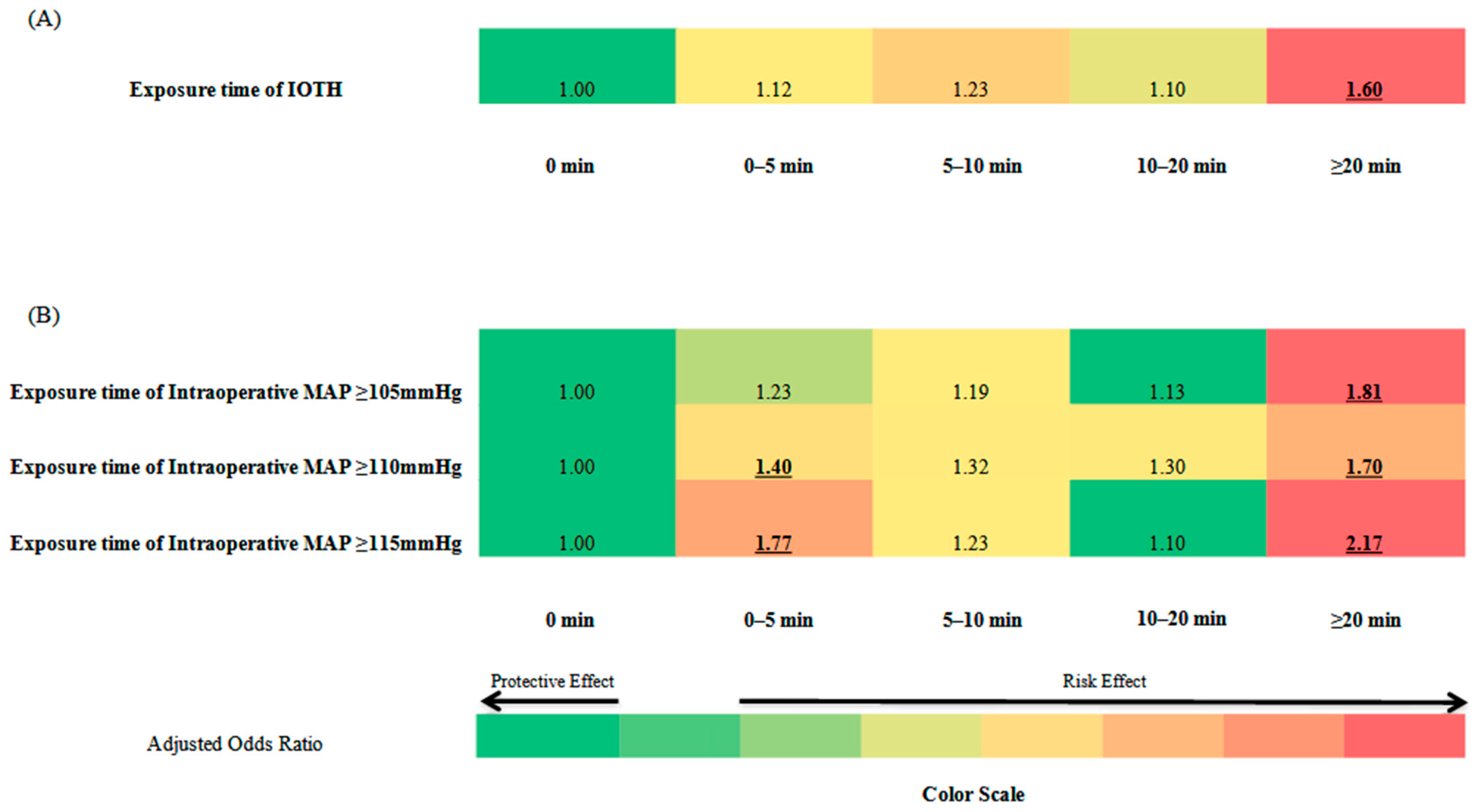
| 2. We categorized patients as having spent 0, 1–5, 6–10, 11–20, or more than 20 min of cumulative IOTH time, a MAP of more than 105, more than 110, more than 115. Associations between intraoperative hypertension and AKI were estimated for the different exposure times in the aforementioned different periods of surgery. | |||
| Postoperative Acute Kidney Injury | Total | ||
|---|---|---|---|
| Yes (n = 482) | No (n = 11,932) | ||
| Age (years) * | 48.7 ± 13.8 | 44.0 ± 14.0 | 44.2 ± 14.1 |
| Male sex (%) * | 38.8 | 9.2 | 10.4 |
| Weight (kg) | 56.8 ± 10.0 | 56.8 ± 9.5 | 56.8 ± 9.5 |
| Preoperative SBP (mmHg) * | 121.0 ± 17.5 | 118.4 ± 15.5 | 118.5 ± 15.6 |
| Preoperative DBP (mmHg) * | 75.4 ± 10.8 | 75.1 ± 9.8 | 75.1 ± 9.8 |
| Preoperative MAP (mmHg) * | 90.6 ± 12.1 | 89.5 ± 10.8 | 89.6 ± 10.9 |
| eGFR (%) * | |||
| <30 mL/min/1.73 m2 | 2.3 | 0.6 | 0.6 |
| 30–60 mL/min/1.73 m2 | 2.9 | 4.1 | 4.1 |
| ≥60 mL/min/1.73 m2 | 94.8 | 95.3 | 95.3 |
| ASA physical status (%) * | |||
| I | 23.4 | 16.2 | 16.5 |
| II | 59.3 | 68.9 | 68.5 |
| III | 16.8 | 14.2 | 14.3 |
| IV | 0.4 | 0.7 | 0.7 |
| Intraoperative vital signs | |||
| Mean SBP (mmHg) * | 119.1 ± 14.1 | 113.1 ± 11.7 | 113.3 ± 11.9 |
| Mean DBP (mmHg) * | 72.0 ± 9.5 | 68.5 ± 8.1 | 68.6 ± 8.1 |
| Mean MAP (mmHg) * | 87.7 ± 10.3 | 83.4 ± 8.7 | 83.5 ± 8.8 |
| CV of MAP | 12.3 ± 3.3 | 12.1 ± 3.3 | 12.1 ± 3.3 |
| IOTH (n, %) * | 291, 60.4% | 5491, 46.0% | 5782, 46.6% |
| IOH (n, %) * | 133, 27.6% | 4134, 34.6% | 4267, 34.4% |
| Heart rate (beats/minute) * | 72.1 ± 10.1 | 70.2 ± 8.9 | 70.3 ± 9.0 |
| Preoperative complications | |||
| History of hypertension (%) * | 18.3 | 11.6 | 11.8 |
| Presence of diabetes (%) * | 10.8 | 5.0 | 5.2 |
| Presence of COPD (%) | 0.6 | 1.1 | 1.1 |
| Presence of malignant tumor (%) * | 6.2 | 2.1 | 2.3 |
| Preoperative medications | |||
| CCBs (%) * | 8.5 | 2.2 | 2.6 |
| RASIs (%) * | 0.8 | 0.3 | 0.3 |
| β-Receptor antagonists (%) * | 1.5 | 0.2 | 0.3 |
| α-Receptor antagonists (%) * | 1.2 | 0.2 | 0.3 |
| Diuretics (%) | 0.0 | 0.1 | 0.1 |
| Oral antidiabetic drugs (%) * | 1.0 | 0.2 | 0.3 |
| Insulin (%) * | 5.6 | 2.8 | 2.9 |
| Contrast drugs (%) * | 1.5 | 0.4 | 0.5 |
| Lipid-lowering drugs (%) * | 1.9 | 0.3 | 0.3 |
| Preoperative laboratory tests | |||
| Neutrophils (*109/L) | 4.3 ± 2.5 | 4.1 ± 2.3 | 4.1 ± 2.3 |
| Lymphocytes (*109/L) | 1.8 ± 0.7 | 1.8 ± 0.7 | 1.8 ± 0.7 |
| Red blood cells (*1012/L) * | 4.1 ± 0.6 | 4.2 ± 0.5 | 4.2 ± 0.5 |
| Hemoglobin (g/L)* | 120.1 ± 20.6 | 121.8 ± 18.5 | 121.7 ± 18.6 |
| Blood platelets (*109/L) | 223.8 ± 75.9 | 230.3 ± 76.8 | 230.1 ± 76.8 |
| Glucose (mmol/L) * | 5.2 ± 1.9 | 4.9 ± 1.2 | 4.9 ± 1.3 |
| Uric acid (µmol/L) * | 264.3 ± 95.6 | 260.9 ± 80.6 | 261.0 ± 81.2 |
| BUN (mmol/L) * | 4.8 ± 2.9 | 4.4 ± 1.6 | 4.4 ± 1.7 |
| Albumin (g/L) * | 40.6 ± 4.9 | 41.4 ± 4.2 | 41.4 ± 4.3 |
| LDL-C (mmol/L) | 2.5 ± 0.6 | 2.5 ± 0.5 | 2.5 ± 0.5 |
| Total cholesterol (mmol/L) | 4.6 ± 0.8 | 4.6 ± 0.7 | 4.6 ± 0.7 |
| ALT (u/L) * | 17.0 (12.8, 27.3) | 16.0 (12.0, 24.0) | 16.0 (12.0, 24.0) |
| AST (u/L) | 19.0 (17.0, 26.0) | 19.0 (16.0, 23.0) | 19.0 (16.0, 23.0) |
| Intraoperative medications | |||
| Midazolam (mg) | 2.0 (1.0, 3.0) | 2.0 (2.0, 3.0) | 2.0 (2.0, 3.0) |
| Anesthetic-inducing alfentanils a (mg) | 1.5 (0.5, 2.0) | 1.0 (0.0, 2.5) | 1.0 (0.0, 2.5) |
| Sevoflurane (mL) | 15.0 (5.8, 20.0) | 15.0 (5.0, 20.0) | 15.0 (5.0, 20.0) |
| Propofol (mL) | 48.1 (35.0, 50.0) | 48.1 (30.0, 50.0) | 48.1 (30.0, 50.0) |
| Alfentanils a (mg) * | 17.0 (14.4, 28.0) | 15.0 (13.5, 19.0) | 15.0 (13.5, 20.0) |
| NSAIDs (%) | 50.2 | 52.4 | 52.3 |
| Dexmedetomidine (%) | 6.0 | 7.8 | 7.7 |
| Rocuronium (mg) | 0.0 (0.0, 40.0) | 0.0 (0.0, 40.0) | 0.0 (0.0, 40.0) |
| Cisatracurium (mg) * | 7.5 (0.0, 13.0) | 5.0 (0.0, 10.0) | 5.0 (0.0, 10.0) |
| Vasoactive drugs (%) * | 14.9 | 7.1 | 7.4 |
| Blood transfusion (%) * | 17.0 | 9.7 | 10.0 |
| Transfusion volume (mL) * | 2200 (1600, 3100) | 1600 (1300, 2500) | 1600 (1450, 2600) |
| Other intraoperative information | |||
| Invasive BP monitoring (%) * | 43.8 | 27.4 | 28.0 |
| Intraoperative blood loss ≥ 1000 mL (%) * | 6.2 | 2.6 | 2.7 |
| Operation time (hours) * | 2.2 (1.4, 3.2) | 1.7 (1.1, 2.5) | 1.7 (1.1, 2.6) |
| Duration of intubation (hours) * | 3.3 (2.2, 4.3) | 2.4 (1.8, 3.4) | 2.4 (1.8, 3.4) |
| Postoperative hospital stay (days) * | 8.0 (5.0, 11.0) | 5.0 (4.0, 9.0) | 5.0 (4.0, 9.0) |
| The rate of converting to open abdominal surgery (%) * | 4.4 | 1.3 | 1.4 |
| Transfer to ICU after surgery (%) * | 3.3 | 0.7 | 0.8 |
| Type of surgery (%) * | |||
| General abdominal surgery | 45.9 | 29.8 | 30.4 |
| Urology surgery | 14.3 | 4.6 | 4.9 |
| Gynecological surgery | 39.8 | 65.6 | 64.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, Y.; Li, B.; Ouyang, W.; Jiang, G.; Tang, H.; Liu, X. Intraoperative Hypertension Is Associated with Postoperative Acute Kidney Injury after Laparoscopic Surgery. J. Pers. Med. 2023, 13, 541. https://doi.org/10.3390/jpm13030541
Tang Y, Li B, Ouyang W, Jiang G, Tang H, Liu X. Intraoperative Hypertension Is Associated with Postoperative Acute Kidney Injury after Laparoscopic Surgery. Journal of Personalized Medicine. 2023; 13(3):541. https://doi.org/10.3390/jpm13030541
Chicago/Turabian StyleTang, Yongzhong, Bo Li, Wen Ouyang, Guiping Jiang, Hongjia Tang, and Xing Liu. 2023. "Intraoperative Hypertension Is Associated with Postoperative Acute Kidney Injury after Laparoscopic Surgery" Journal of Personalized Medicine 13, no. 3: 541. https://doi.org/10.3390/jpm13030541
APA StyleTang, Y., Li, B., Ouyang, W., Jiang, G., Tang, H., & Liu, X. (2023). Intraoperative Hypertension Is Associated with Postoperative Acute Kidney Injury after Laparoscopic Surgery. Journal of Personalized Medicine, 13(3), 541. https://doi.org/10.3390/jpm13030541






