Minimum 2-Year Radiographic and Clinical Outcomes of Unrestricted Kinematic Alignment Total Knee Arthroplasty in Patients with Excessive Varus of the Tibia Component
Abstract
:1. Introduction
2. Materials and Methods
2.1. Technique
2.2. Radiographic Analysis
2.3. Follow-Up Examination
2.4. Statistical Analysis
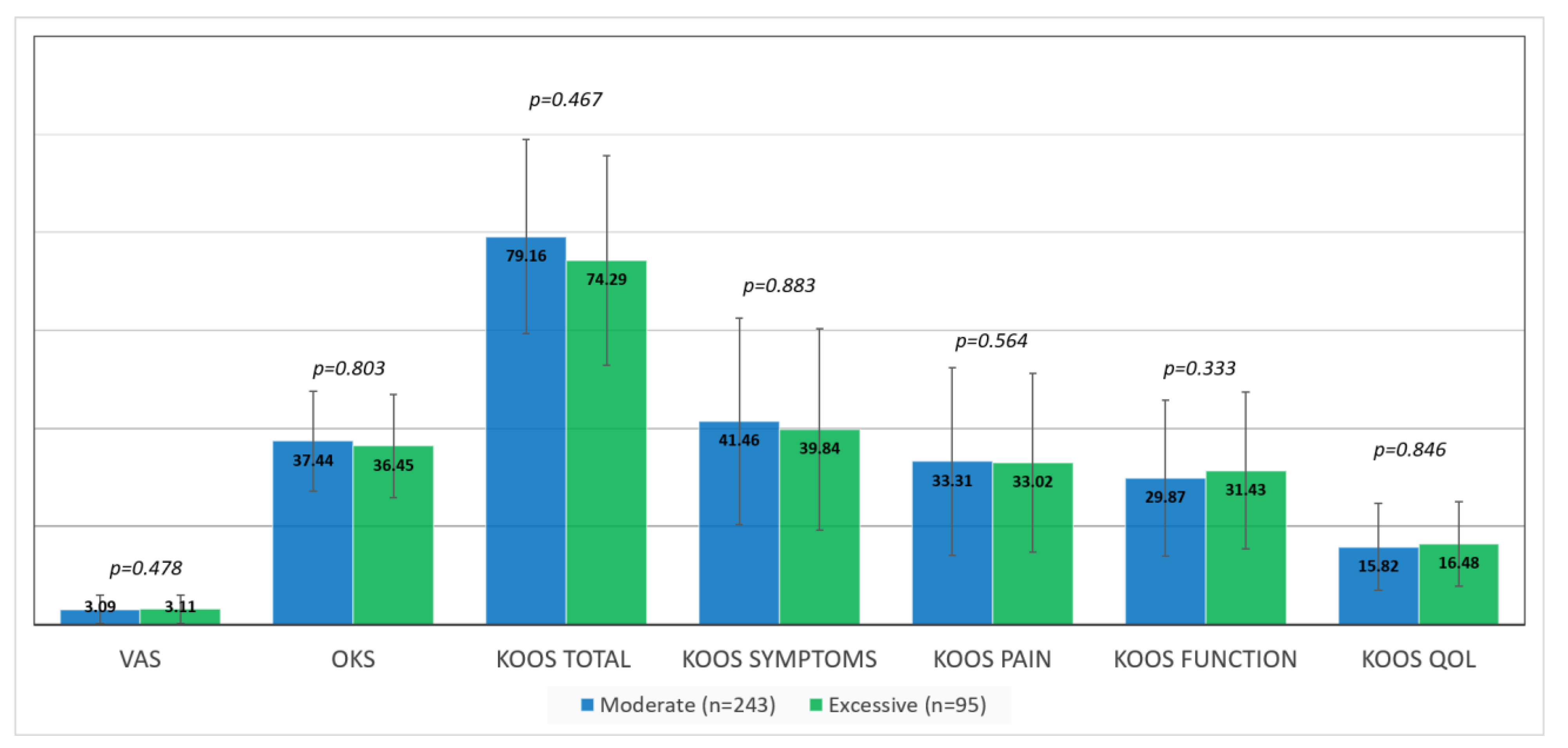
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, Y.; Jordan, J.M. Epidemiology of Osteoarthritis. Clin. Geriatr. Med. 2010, 26, 355–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sánchez Romero, E.A.; Meléndez Oliva, E.; Alonso Pérez, J.L.; Martín Pérez, S.; Turroni, S.; Marchese, L.; Villafañe, J.H. Relationship between the Gut Microbiome and Osteoarthritis Pain: Review of the Literature. Nutrients 2021, 13, 716. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Romero, E.A.; Fernández-Carnero, J.; Calvo-Lobo, C.; Ochoa Sáez, V.; Burgos Caballero, V.; Pecos-Martín, D. Is a Combination of Exercise and Dry Needling Effective for Knee OA? Pain Med. 2020, 21, 349–363. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Romero, E.A.; González-Zamorano, Y.; Arribas-Romano, A.; Martínez-Pozas, O.; Fernández Espinar, E.; Pedersini, P.; Villafañe, J.H.; Alonso Pérez, J.L.; Fernández-Carnero, J. Efficacy of Manual Therapy on Facilitatory Nociception and Endogenous Pain Modulation in Older Adults with Knee Osteoarthritis: A Case Series. Appl. Sci. 2021, 11, 1895. [Google Scholar] [CrossRef]
- Ruiz, D.; Koenig, L.; Dall, T.M.; Gallo, P.; Narzikul, A.; Parvizi, J.; Tongue, J. The direct and indirect costs to society of treatment for end-stage knee osteoarthritis. J. Bone Joint Surg. Am. 2013, 95, 1473–1480. [Google Scholar] [CrossRef] [Green Version]
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J. Bone Joint Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.J.K.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef]
- Nam, D.; Nunley, R.M.; Barrack, R.L. Patient dissatisfaction following total knee replacement. Bone Joint J. 2014, 96-B, 96–100. [Google Scholar] [CrossRef]
- Scott, C.E.H.; Oliver, W.M.; MacDonald, D.; Wade, F.A.; Moran, M.; Breusch, S.J. Predicting Dissatisfaction Following Total Knee Arthroplasty in Patients Under 55 Years of Age. Bone Joint J. 2016, 98-B, 1625–1634. Available online: https://pubmed.ncbi.nlm.nih.gov/27909124/ (accessed on 23 April 2020). [CrossRef] [Green Version]
- Batailler, C.; Swan, J.; Sappey Marinier, E.; Servien, E.; Lustig, S. New Technologies in Knee Arthroplasty: Current Concepts. J. Clin. Med. 2020, 10, 47. [Google Scholar] [CrossRef]
- Calliess, T.; Bauer, K.; Stukenborg-Colsman, C.; Windhagen, H.; Budde, S.; Ettinger, M. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: A prospective, randomized study. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1743–1748. [Google Scholar] [CrossRef]
- Yoon, J.-R.; Han, S.-B.; Jee, M.-K.; Shin, Y.-S. Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty: A meta-analysis. Medicine 2017, 96, e8157. [Google Scholar] [CrossRef]
- Howell, S.M.; Roth, J.D.; Hull, M.L. Kinematic Alignment in Total Knee Arthroplasty; Elsevier: Philadelphia, PA, USA, 2012. [Google Scholar]
- Sappey-Marinier, E.; Pauvert, A.; Batailler, C.; Swan, J.; Cheze, L.; Servien, E.; Lustig, S. Kinematic versus mechanical alignment for primary total knee arthroplasty with minimum 2 years follow-up: A systematic review. SICOT J. 2020, 6, 18. [Google Scholar] [CrossRef]
- Vendittoli, P.-A.; Martinov, S.; Blakeney, W.G. Restricted Kinematic Alignment, the Fundamentals, and Clinical Applications. Front. Surg. 2021, 8, 697020. [Google Scholar] [CrossRef]
- Laforest, G.; Kostretzis, L.; Kiss, M.-O.; Vendittoli, P.-A. Restricted kinematic alignment leads to uncompromised osseointegration of cementless total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 705–712. [Google Scholar] [CrossRef]
- Nisar, S.; Palan, J.; Rivière, C.; Emerton, M.; Pandit, H. Kinematic alignment in total knee arthroplasty. EFORT Open Rev. 2020, 5, 380–390. Available online: https://eor.bioscientifica.com/configurable/content/journals$002feor$002f5$002f7$002f2058-5241.5.200010.xml?t:ac=journals%24002feor%24002f5%24002f7%24002f2058-5241.5.200010.xml (accessed on 14 June 2022). [CrossRef]
- Antonios, J.K.; Korber, S.; Sivasundaram, L.; Mayfield, C.; Kang, H.P.; Oakes, D.A.; Heckmann, N.D. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: An analysis of patient and hospital factors. Arthroplast. Today 2019, 5, 88–95. [Google Scholar] [CrossRef] [Green Version]
- Schelker, B.L.; Nowakowski, A.M.; Hirschmann, M.T. What is the “safe zone” for transition of coronal alignment from systematic to a more personalised one in total knee arthroplasty? A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 419–427. [Google Scholar] [CrossRef]
- Srivastava, A.; Lee, G.; Steklov, N.; Colwell, C.; Ezzet, K.; D’Lima, D. Effect of tibial component varus on wear in total knee arthroplasty. Knee 2011, 19, 560–563. [Google Scholar] [CrossRef]
- Tibbo, M.E.; Limberg, A.K.; Perry, K.I.; Pagnano, M.W.; Stuart, M.J.; Hanssen, A.D.; Abdel, M.P. Effect of Coronal Alignment on 10-Year Survivorship of a Single Contemporary Total Knee Arthroplasty. J. Clin. Med. 2021, 10, 142. Available online: https://pubmed.ncbi.nlm.nih.gov/33406614/ (accessed on 14 June 2022). [CrossRef]
- Bar-Ziv, Y.; Lamykin, K.; Shohat, N.; Jurban, A.; Agar, G.; Ner, E.B. The “linked soft tissue guided technique”: A novel method for cutting the tibia while performing a kinematic femoral alignment in total knee arthroplasty. Ann. Jt. 2019, 4, 39. Available online: https://aoj.amegroups.com/article/view/5377/html (accessed on 9 May 2022). [CrossRef]
- Paley, D. Normal Lower Limb Alignment and Joint Orientation. In Principles of Deformity Correction; Springer: Berlin/Heidelberg, Germany, 2022; Available online: https://link.springer.com/chapter/10.1007/978-3-642-59373-4_1 (accessed on 14 June 2022).
- Liu, C.; Zhao, G.; Chen, K.; Lyu, J.; Chen, J.; Shi, J.; Huang, G.; Chen, F.; Wei, Y.; Wang, S.; et al. Tibial component coverage affects tibial bone resorption and patient-reported outcome measures for patients following total knee arthroplasty. J. Orthop. Surg. Res. 2021, 16, 134. Available online: https://josr-online.biomedcentral.com/articles/10.1186/s13018-021-02250-7 (accessed on 4 June 2022). [CrossRef]
- Lyman, S.; Lee, Y.-Y.; McLawhorn, A.S.; Islam, W.; MacLean, C.H. What Are the Minimal and Substantial Improvements in the HOOS and KOOS and JR Versions After Total Joint Replacement? Clin. Orthop. Relat. Res. 2018, 476, 2432–2441. [Google Scholar] [CrossRef]
- Clement, N.D.; MacDonald, D.; Simpson, A.H.R.W. The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1933–1939. [Google Scholar] [CrossRef]
- Bellemans, J.; Colyn, W.; Vandenneucker, H.; Victor, J. The Chitranjan Ranawat award: Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin. Orthop. Relat. Res. 2012, 470, 45–53. [Google Scholar] [CrossRef] [Green Version]
- Parratte, S.; Pagnano, M.W.; Trousdale, R.T.; Berry, D.J. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J. Bone Joint Surg. Am. 2010, 92, 2143–2149. [Google Scholar] [CrossRef]
- Howell, S.M.; Howell, S.J.; Kuznik, K.T.; Cohen, J.; Hull, M.L. Does A Kinematically Aligned Total Knee Arthroplasty Restore Function Without Failure Regardless of Alignment Category? Clin. Orthop. Relat. Res. 2013, 471, 1000–1007. [Google Scholar] [CrossRef] [Green Version]
- Miralles-Muñoz, F.A.; Rubio-Morales, M.; Bello-Tejada, L.; González-Parreño, S.; Lizaur-Utrilla, A.; Alonso-Montero, C. Varus alignment of the tibial component up to seven degrees is not associated with poor long-term outcomes in a neutrally aligned total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2021, 30, 2768–2775. [Google Scholar] [CrossRef]
- Sánchez-Romero, E.A.; Battaglino, A.; Campanella, W.; Turroni, S.; Bishop, M.D.; Villafañe, J.H. Impact on Blood Tests of Lower Limb Joint Replacement for the Treatment of Osteoarthritis: Hip and Knee. Top. Geriatr. Rehabil. 2021, 37, 227–229. [Google Scholar] [CrossRef]
- Eckhoff, D.; Hogan, C.; DiMatteo, L.; Robinson, M.; Bach, J. Difference between the epicondylar and cylindrical axis of the knee. Clin. Orthop. Relat. Res. 2007, 461, 238–244. Available online: https://pubmed.ncbi.nlm.nih.gov/17549027/ (accessed on 20 June 2022). [CrossRef]
- Bonner, T.J.; Eardley, W.G.P.; Patterson, P.; Gregg, P.J. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J. Bone Joint Surg. Br. 2011, 93, 1217–1222. Available online: https://pubmed.ncbi.nlm.nih.gov/21911533/ (accessed on 20 June 2022). [CrossRef] [PubMed] [Green Version]
- Howell, S.M.; Shelton, T.J.; Hull, M.L. Implant Survival and Function Ten Years After Kinematically Aligned Total Knee Arthroplasty. J. Arthroplasty 2018, 33, 3678–3684. [Google Scholar] [CrossRef] [PubMed]

| Variable | Moderate (n = 243) | Excessive (n = 95) | p-Value |
|---|---|---|---|
| Age | 70.16 (8.43) | 70.83 (8.12) | 0.221 |
| Sex (female) | 164 (67.5%) | 57 (60.0%) | 0.205 |
| BMI (kg/m2) | 31.65 (5.03) | 31.27 (5.48) | 0.699 |
| CCI | 0.85 (1.10) | 0.712 (1.06) | 0.674 |
| Anesthesia (spinal) | 180 (74.1%) | 65 (68.4%) | 0.343 |
| Operative duration | 82.39 (20.35) | 84.77 (21.76) | 0.238 |
| LOS | 4.32 (2.69) | 4.49 (10.21) | 0.105 |
| Extension | 4.11 (5.21) | 4.42 (5.71) | 0.785 |
| Flexion | 109.08 (15.94) | 111.54 (16.23) | 0.483 |
| VAS | 8.07 (1.43) | 8.05 (1.47) | 0.969 |
| OKS | 13.78 (7.75) | 13.45 (7.64) | 0.283 |
| KOOS TOTAL | 28.22 (15.22) | 30.52 (14.31) | 0.606 |
| Time to Follow Up (m) | 41.25 (9.52) | 36.65 (8.77) | <0.001 |
| Preoperative | Postoperative | |||||
|---|---|---|---|---|---|---|
| Moderate (n = 243) | Excessive (n = 95) | p-Value | Moderate (n = 243) | Excessive (n = 95) | p-Value | |
| MPTA | 85.76° (3.38°) | 83.67° (3.35°) | <0.001 | 87.96° (2.07°) | 82.63° (1.83°) | <0.001 |
| LDFA | 89.36° (3.87°) | 89.69° (4.12°) | 0.49 | 85.22° (4.16°) | 83.34° (3.79°) | <0.001 |
| HKA * | −9.47° (4.59°) | −11.31° (5.95°) | 0.002 | −1.99° (3.4°) | −3.13° (2.57°) | 0.010 |
| Slope | 10.68° (5.34°) | 11.41° (6.31°) | 0.058 | 7.17° (4.08°) | 6.89° (3.58°) | 0.553 |
| MCID | Moderate (n = 243) | Excessive (n = 95) | p-Value |
|---|---|---|---|
| OKS | 228 (93.8%) | 93 (98.4%) | 0.287 |
| KOOS Symptoms | 204 (84.0%) | 78 (82.0%) | 0.691 |
| KOOS Pain | 178 (73.1%) | 79 (83.6%) | 0.114 |
| KOOS Function | 207 (85.3%) | 79 (83.6%) | 0.834 |
| KOOS QOL | 215 (88.5%) | 86 (90.2%) | 0.814 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bar Ziv, Y.; Essa, A.; Lamykin, K.; Chacar, N.; Livshits, G.; Khatib, S.; Comaya, Y.; Shohat, N. Minimum 2-Year Radiographic and Clinical Outcomes of Unrestricted Kinematic Alignment Total Knee Arthroplasty in Patients with Excessive Varus of the Tibia Component. J. Pers. Med. 2022, 12, 1206. https://doi.org/10.3390/jpm12081206
Bar Ziv Y, Essa A, Lamykin K, Chacar N, Livshits G, Khatib S, Comaya Y, Shohat N. Minimum 2-Year Radiographic and Clinical Outcomes of Unrestricted Kinematic Alignment Total Knee Arthroplasty in Patients with Excessive Varus of the Tibia Component. Journal of Personalized Medicine. 2022; 12(8):1206. https://doi.org/10.3390/jpm12081206
Chicago/Turabian StyleBar Ziv, Yaron, Ahmad Essa, Konstantin Lamykin, Najib Chacar, Gilad Livshits, Salah Khatib, Yoav Comaya, and Noam Shohat. 2022. "Minimum 2-Year Radiographic and Clinical Outcomes of Unrestricted Kinematic Alignment Total Knee Arthroplasty in Patients with Excessive Varus of the Tibia Component" Journal of Personalized Medicine 12, no. 8: 1206. https://doi.org/10.3390/jpm12081206
APA StyleBar Ziv, Y., Essa, A., Lamykin, K., Chacar, N., Livshits, G., Khatib, S., Comaya, Y., & Shohat, N. (2022). Minimum 2-Year Radiographic and Clinical Outcomes of Unrestricted Kinematic Alignment Total Knee Arthroplasty in Patients with Excessive Varus of the Tibia Component. Journal of Personalized Medicine, 12(8), 1206. https://doi.org/10.3390/jpm12081206






