LACE Index to Predict the High Risk of 30-Day Readmission: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy and Data Sources
2.3. Study Selection and Data Extraction
2.4. Quality Assessment
2.5. Data Synthesis
3. Results
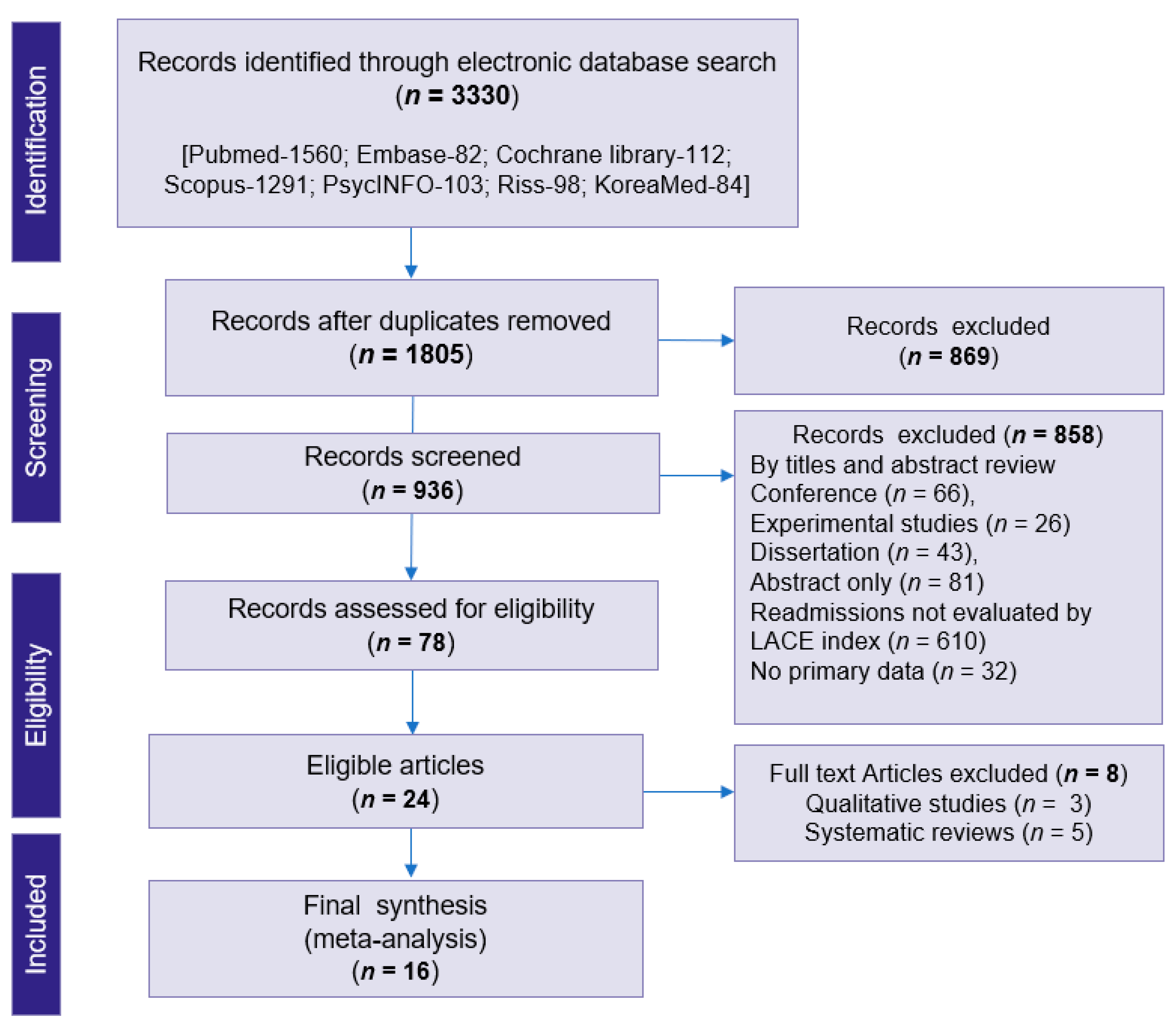
3.1. Study Selection
3.2. Characteristics of the Review Articles
3.3. Meta-Analysis
3.4. Sub Group Analysis

4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hospital Readmissions—Healthcare.gov Glossary. Available online: https://www.healthcare.gov/glossary/hospital-readmissions/ (accessed on 10 December 2021).
- Ashton, C.M.; Del Junco, D.J.; Souchek, J.; Wray, N.P.; Mansyur, C.L. The association between the quality of inpatient care and early readmission. Med. Care 1997, 35, 1044–1059. [Google Scholar] [CrossRef] [PubMed]
- Weiss, A.J.; Jiang, H.J. Overview of Clinical Conditions with Frequent and Costly Hospital Readmissions by Payer, 2018. HCUP Statistical Brief #278 [Internet]. Healthcare Cost and Utilization Project—HCUP-us.ahrq.gov. Agency for Healthcare Research and Quality, Rockville, MD, USA. 2021. Available online: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb278-Conditions-Frequent-Readmissions-By-Payer-2018.pdf (accessed on 10 December 2021).
- The Canadian Institute for Health Information (CIHI), 2019–2020: Patients Urgently Readmitted to Hospital within 30 Days of Discharge. Available online: https://www.cihi.ca/en/indicators/all-patients-readmitted-to-hospital (accessed on 19 October 2021).
- Australian Commission on Safety and Quality in Health Care. National Core, Hospital-Based Outcome Indicator Specification. Available online: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/national-core-hospital-based-outcome-indicator-specification/ (accessed on 15 December 2021).
- NHS Digital [Internet]; Indicator Quality Improvement; Emergency Readmissions within 30 Days of Discharge from Hospital. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/ccg-outcomes-indicator-set/march-2020/domain-3-helping-people-to-recover-from-episodes-of-ill-health-or-following-injury-ccg/3-2-emergency-readmissions-within-30-days-of-discharge-from-hospital (accessed on 22 December 2021).
- McIlvennan, C.K.; Eapen, Z.J.; Allen, L.A. Hospital readmissions reduction program. Circulation 2015, 131, 1796–1803. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.; Le Padellec, R.; Ireland, D. Statewide validation of a patient admissions prediction tool. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; Volume 2010, pp. 3887–3890. [Google Scholar]
- Van Walraven, C.; Dhalla, I.A.; Bell, C.; Etchells, E.; Stiell, I.G.; Zarnke, K.; Austin, P.C.; Forster, A.J. Derivation, and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Can. Med. Assoc. J. 2010, 182, 551–557. [Google Scholar] [CrossRef] [Green Version]
- Gruneir, A.; Dhalla, I.A.; van Walraven, C.; Fischer, H.D.; Camacho, X.; A Rochon, P.; Anderson, G.M. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011, 5, e104–e111. [Google Scholar]
- Yazdan-Ashoori, P.; Lee, S.F.; Ibrahim, Q.; Van Spall, H.G. Utility of the LACE index at the bedside in predicting 30-day readmission or death in patients hospitalized with heart failure. Am. Heart J. 2016, 179, 51–58. [Google Scholar] [CrossRef]
- Caplan, I.F.; Zadnik Sullivan, P.; Glauser, G.; Choudhri, O.; Kung, D.; O’Rourke, D.M.; Osiemo, B.; Goodrich, S.; McClintock, S.D.; Malhotra, N.R.; et al. The LACE+ index fails to predict 30–90-day readmission for supratentorial craniotomy patients: A retrospective series of 238 surgical procedures. Clin. Neurol. Neurosurg. 2019, 182, 79–83. [Google Scholar] [CrossRef]
- Ibrahim, A.M.; Koester, C.; Al-Akchar, M.; Tandan, N.; Regmi, M.; Bhattarai, M.; Al-Bast, B.; Kulkarni, A.; Robinson, R. HOSPITAL Score, LACE Index and LACE+ Index as predictors of 30-day readmission in patients with heart failure. BMJ Evid.-Based Med. 2020, 25, 166–167. [Google Scholar] [CrossRef]
- Linzey, J.R.; Foshee, R.L.; Srinivasan, S.; Fiestan, G.O.; Mossner, J.M.; Gemmete, J.J.; Burke, J.F.; Sheehan, K.M.; Rajajee, R.; Pandey, A.S. The predictive value of the hospital score and Lace Index for an adult neurosurgical population: A prospective analysis. World Neurosurg. 2020, 137, e166–e175. [Google Scholar] [CrossRef]
- Miller, W.D.; Nguyen, K.; Vangala, S.; Dowling, E. Clinicians can independently predict 30-day hospital readmissions as well as the LACE index. BMC Health Serv. Res. 2018, 18, 32. [Google Scholar] [CrossRef] [Green Version]
- Robinson, R.; Hudali, T. The HOSPITAL score and LACE index as predictors of 30 day readmission in a retrospective study at a university-affiliated community hospital. PeerJ 2017, 5, e3137. [Google Scholar] [CrossRef] [Green Version]
- Regmi, M.R.; Bhattarai, M.; Parajuli, P.; Garcia, O.E.L.; Tandan, N.; Ferry, N.; Cheema, A.; Chami, Y.; Robinson, R. Heart Failure with Preserved Ejection Fraction and 30-Day Readmission. Clin. Med. Res. 2020, 18, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Robinson, R.D.; Johnson, C.; Zenarosa, N.R.; Jayswal, R.D.; Keithley, J.; A Delaney, K. Using the LACE index to predict hospital readmissions in congestive heart failure patients. BMC Cardiovasc. Disord. 2014, 14, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damery, S.; Combes, G. Evaluating the predictive strength of the LACE index in identifying patients at high risk of hospital readmission following an inpatient episode: A retrospective cohort study. BMJ Open 2017, 7, e016921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dobler, C.C.; Hakim, M.; Singh, S.; Jennings, M.; Waterer, G.; Garden, F.L. Ability of the LACE index to predict 30-day hospital readmissions in patients with community-acquired pneumonia. ERJ Open Res. 2020, 6, 00301–02019. [Google Scholar] [CrossRef] [PubMed]
- Hakim, M.A.; Garden, F.L.; Jennings, M.D.; Dobler, C.C. Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease. Clin. Epidemiol. 2018, 10, 51–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Labrosciano, C.; Air, T.; Tavella, R.; Beltrame, J.F.; Ranasinghe, I. Readmissions following hospitalizations for cardiovascular disease: A scoping review of the Australian literature. Aust. Health Rev. 2020, 44, 93–103. [Google Scholar] [CrossRef]
- Jang, J.G.; Ahn, J.H. Reasons and Risk Factors for Readmission Following Hospitalization for Community-acquired Pneumonia in South Korea. Tuberc. Respir. Dis. 2020, 83, 147–156. [Google Scholar] [CrossRef] [Green Version]
- Health Insurance Review & Assessment Service, “Results of Appropriateness for Risk-Standardized Readmission Ratio in 2017(Second),”. December 2018. Available online: https://www.hira.or.kr/cms/open/04/04/12/2018_10.pdf (accessed on 3 January 2022).
- Page, M.J.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Higgins, J.P.T.; Reeves, B.C.; on behalf of the Development Group for ACROBAT-NRSI. A Cochrane Risk of Bias Assessment Tool: For Non-Randomized Studies of Interventions (ACROBAT-NRSI), Version 1.0.0. 24 September 2014. Available online: http://www.bristol.ac.uk/population-health-sciences/centres/cresyda/barr/riskofbias/robins-i/acrobat-nrsi/ (accessed on 12 December 2021).
- Higgins, J.P.; Thompson, S.G.; Spiegelhalter, D.J. A re-evaluation of random-effects meta-analysis. J. R. Stat. Soc. Ser. A Stat. Soc. 2009, 172, 137–159. [Google Scholar] [CrossRef] [Green Version]
- Low, L.L.; Liu, N.; Wang, S.; Thumboo, J.; Ong, M.E.H.; Lee, K.H. Predicting 30-Day readmissions in an Asian Population: Building a Predictive Model by incorporating markers of hospitalization severity. PLoS ONE 2016, 11, e0167413. [Google Scholar] [CrossRef]
- Tan, S.Y.; Low, L.L.; Yang, Y.; Lee, K.H. Applicability of a previously validated readmission predictive index in medical patients in Singapore: A retrospective study. BMC Health Serv. Res. 2013, 13, 366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cotter, P.E.; Bhalla, V.K.; Wallis, S.J.; Biram, R.W. Predicting readmissions: Poor performance of the lace index in an older UK population. Age Ageing 2012, 41, 784–789. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Author (s) | Study Design/Data Source | Period | Target Population | Measurement /Analysis Model | Outcome | Risk of Bias | ||
|---|---|---|---|---|---|---|---|---|
| Caplan et al. [12] | RC | EMR | University hospital | 2017–2018 | Brain tumor | LACE index | 30–90 day readmission | NA |
| Damery et al. [19] | RC | EMR | University hospital | 2013–2014 | All cause | LACE index | 30-day readmission | Low |
| Dobler et al. [20] | RC | EMR | Tertiary hospital | 2006–2016 | Pneumonia | LACE index | 30-day readmission | Low |
| Gruneir et al. [10] | RC | Data base | OHIP | 2007 | All cause | LACE index | 30-day readmission | Low |
| Hakim et al. [21] | RC | EMR | University hospital | 2006–2016 | COPD | LACE index | 30-day readmission | Low |
| Ibrahim et al. [13] | RC | EMR | University hospital | 2016–2018 | HF | HOSPITAL Score, LACE index, LACE+ index | 30-day readmission | Moderate |
| Labrosciano et al. [22] | RC | Data base | NHS—PAS | 2017–2019 | All cause | LACE index | age-specific readmissions | Low |
| Linzey et al. [14] | RC | EMR | University hospital | 2017 | Nuro surgery | LACE index | 30-day readmission | NA |
| Miller et al. [15] | Survey | EMR | Referral hospital | 2015 | All cause | LACE index | 30-day readmission | Low |
| Robinson et al. [16] | RC | EMR | University hospital | 2015–2016 | All cause | LACE index, HOSPITAL score | 30-day readmission | Moderate |
| Regmi et al. [17] | RC | EMR | University hospital | 2016–2018 | HF | HOSPITAL score, LACE index, and RAHF scale | 30-day readmission | Moderate |
| Wang et al. [18] | RC | EMR | Public hospital | 2011–2015 | HF | LACE index | 30-day readmission | Low |
| Yazdan et al. [11] | PC | EMR | University hospital | 2012–2013 | HF | LACE index | 30-day readmission | Low |
| Low et al. [29] | RC | EMR | Public hospital | 2012 | COPD | LACE index | 30-day readmission | Low |
| Tan et al. [30] | RC | EMR | Tertiary hospital | 2006–2010 | All cause | LACE index | 30-day readmission | Moderate |
| Cotter et al. [31] | RC | EMR | University hospital | 2010 | All cause | LACE index | 30-day readmission | Low |
| Studies | Age (Mean) | Sex (Female, %) | 30-Day Readmission | C-Stat | ||
|---|---|---|---|---|---|---|
| Total | Yes | No | ||||
| Caplan et al. [12] | 62 | 50 | 238 | 31 | 207 | 0.69 |
| Damery et al. [19] | 55 | 63 | 84,815 | 4541 | 84,815 | 0.81 |
| Dobler et al. [20] | 62 | NA | 4508 | 636 | 3872 | 0.57 |
| Gruneir et al. [10] | 65 | 68 | 26,045 | 8854 | 17,191 | NA |
| Hakim et al. [21] | 59 | 55 | 2662 | 847 | 1815 | 0.63 |
| Ibrahim et al. [13] | 68 | 63 | 692 | 189 | 503 | 0.57 |
| Labrosciano et al. [22] | 98 | 40 | 829 | 98 | 731 | 0.62 |
| Linzey et al. [14] | 58 | 51 | 1242 | 104 | 1138 | 0.62 |
| Miller et al. [15] | 65 | 44 | 359 | 78 | 281 | 0.68 |
| Robinson et al. [16] | 62 | 48 | 432 | 35 | 397 | 0.58 |
| Regmi et al. [17] | 67 | 60 | 1370 | 507 | 863 | 0.67 |
| Wang et al. [18] | 57 | 47 | 253 | 62 | 191 | 0.56 |
| Yazdan et al. [11] | 73 | 45 | 378 | 105 | 273 | 0.59 |
| Low et al. [29] | 67 | 55 | 5862 | 572 | 5290 | 0.63 |
| Tan et al. [30] | ≥21 | 59 | 143,376 | 15,826 | 111,724 | 0.72 |
| Cotter et al. [31] | 85 | 50 | 507 | 90 | 417 | 0.55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajaguru, V.; Han, W.; Kim, T.H.; Shin, J.; Lee, S.G. LACE Index to Predict the High Risk of 30-Day Readmission: A Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 545. https://doi.org/10.3390/jpm12040545
Rajaguru V, Han W, Kim TH, Shin J, Lee SG. LACE Index to Predict the High Risk of 30-Day Readmission: A Systematic Review and Meta-Analysis. Journal of Personalized Medicine. 2022; 12(4):545. https://doi.org/10.3390/jpm12040545
Chicago/Turabian StyleRajaguru, Vasuki, Whiejong Han, Tae Hyun Kim, Jaeyong Shin, and Sang Gyu Lee. 2022. "LACE Index to Predict the High Risk of 30-Day Readmission: A Systematic Review and Meta-Analysis" Journal of Personalized Medicine 12, no. 4: 545. https://doi.org/10.3390/jpm12040545
APA StyleRajaguru, V., Han, W., Kim, T. H., Shin, J., & Lee, S. G. (2022). LACE Index to Predict the High Risk of 30-Day Readmission: A Systematic Review and Meta-Analysis. Journal of Personalized Medicine, 12(4), 545. https://doi.org/10.3390/jpm12040545







