Cardiometabolic Risk after SARS-CoV-2 Virus Infection: A Retrospective Exploratory Analysis
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Descriptive Analysis
3.2. Nonparametric Measures of Associations
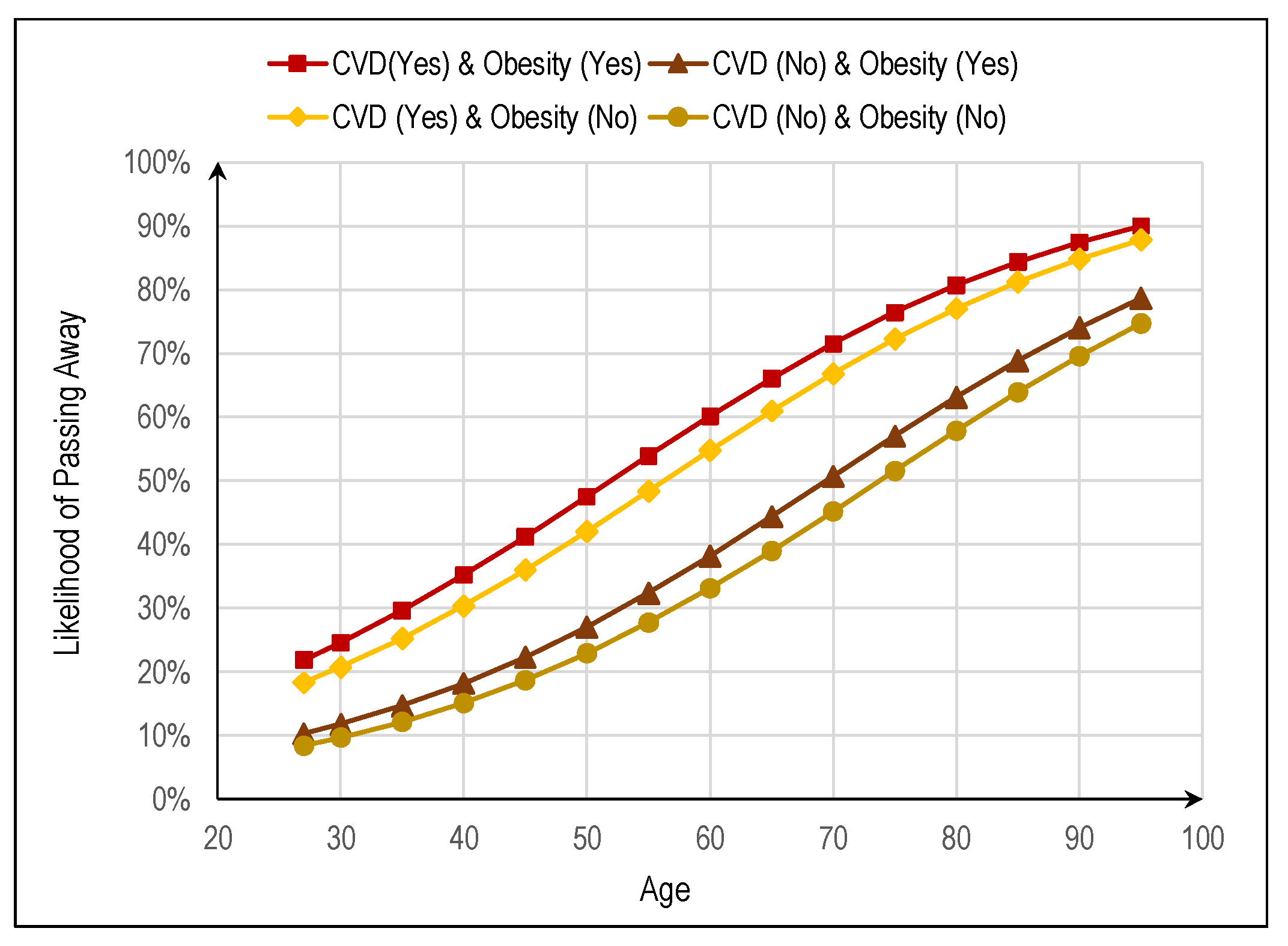
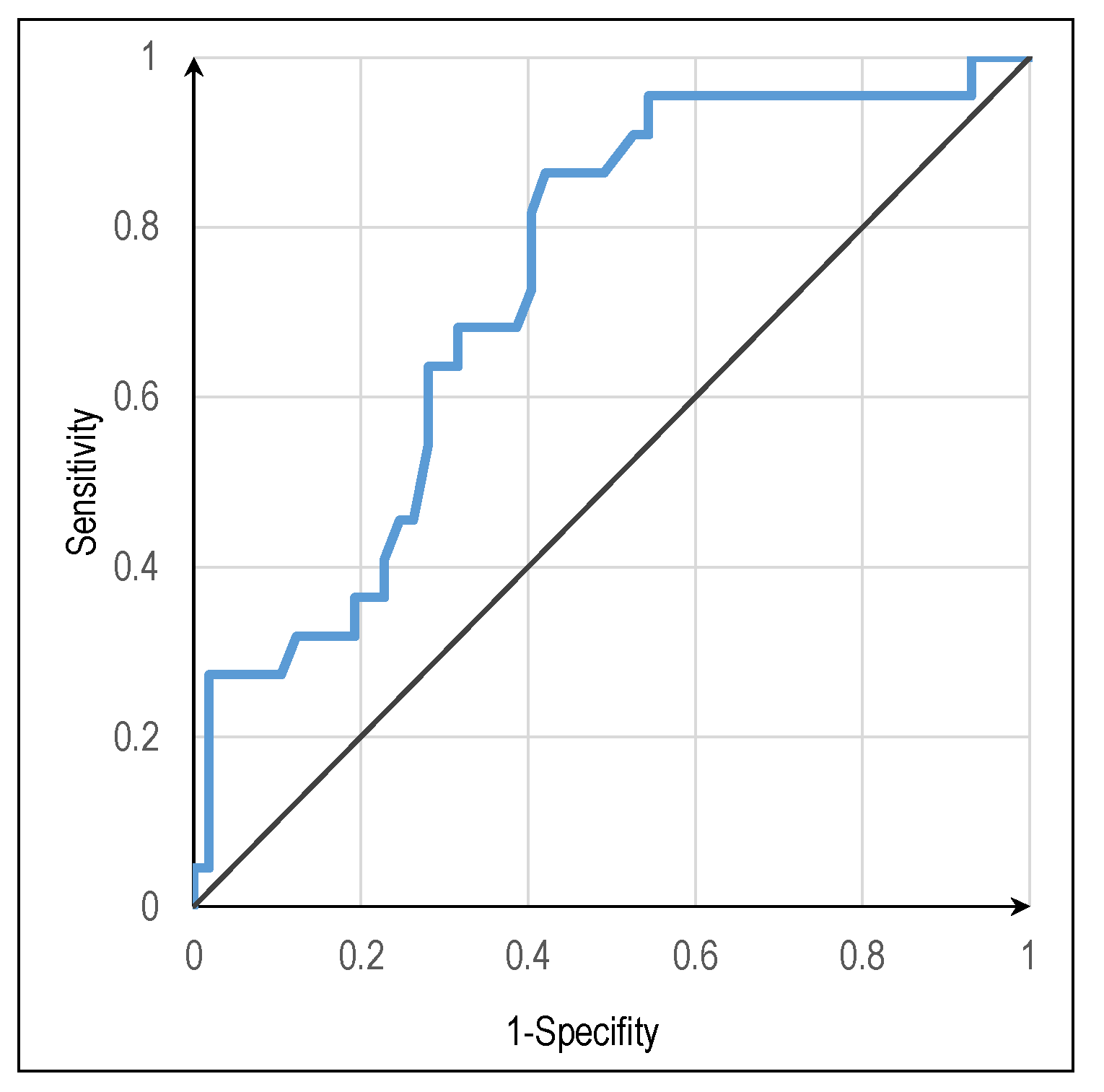
3.3. Logistic Regression Model
3.4. Multilinear Regression Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sposito, A.C.; Caramelli, B.; Fonseca, F.A.H.; Bertolami, M.C.; Afiune Neto, A.; Souza, A.D.; Lottenberg, A.M.P.; Chacra, A.P.; Faludi, A.A.; Loures-Vale, A.A.; et al. IV Diretriz Brasileira sobre Dislipidemias e Prevenção da Aterosclerose: Departamento de Aterosclerose da Sociedade Brasileira de Cardiologia. Arq. Bras. Cardiol. 2007, 88, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Pillon, N.J.; Loos, R.J.F.; Marshall, S.M.; Zierath, J.R. Metabolic consequences of obesity and type 2 diabetes: Balancing genes and environment for personalized care. Cell 2021, 184, 1530–1544. [Google Scholar] [CrossRef] [PubMed]
- Barron, E.; Bakhai, C.; Kar, P.; Weaver, A.; Bradley, D.; Ismail, H.; Knighton, P.; Holman, N.; Khunti, K.; Sattar, N.; et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: A whole-population study. Lancet Diabetes Endocrinol. 2020, 8, 813–822. [Google Scholar] [CrossRef]
- Wang, S.; Ma, P.; Zhang, S.; Song, S.; Wang, Z.; Ma, Y.; Xu, J.; Wu, F.; Duan, L.; Yin, Z.; et al. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: A multi-centre retrospective study. Diabetologia 2020, 63, 2102–2111. [Google Scholar] [CrossRef]
- Bradley, S.A.; Banach, M.; Alvarado, N.; Smokovski, I.; Bhaskar, S.M.M. Prevalence and impact of diabetes in hospitalized COVID-19 patients: A systematic review and meta-analysis. J. Diabetes 2021, 14, 144–157. [Google Scholar] [CrossRef]
- Global Burden of Disease Study 2019. Lancet 2019, 396, 1129–1306. Available online: https://www.thelancet.com/journals/lancet/issue/vol396no10258/PIIS0140-6736(20)X0042-0# (accessed on 31 August 2022).
- de O. Benigno, F.; do Nascimento, A.N.B.; Costa, C.M.C.; dos Ramos, W.O.L.; de Araújo, H.V.S. Impacto cardiovascular em pacientes infectados com o SARS-CoV-2 (COVID-19). Rev. Eletrônica Acervo Saúde 2021, 13, e8296. [Google Scholar] [CrossRef]
- Norris, T.; Razieh, C.; Zaccardi, F.; Yates, T.; Islam, N.; Gillies, C.L.; Chudasama, Y.V.; Rowlands, A.V.; Davies, M.J.; McCann, G.P.; et al. Impact of cardiometabolic multimorbidity and ethnicity on cardiovascular/renal complications in patients with COVID-19. Heart 2022, 108, 1200–1208. [Google Scholar] [CrossRef]
- Husten, L. Global epidemic of cardiovascular disease predicted. Lancet 1998, 352, 1530. [Google Scholar] [CrossRef]
- McKee, M.; Leon, D. Global epidemic of cardiovascular disease. Lancet 1999, 353, 503. [Google Scholar] [CrossRef]
- Chockalingam, A.; Campbell, N.R.; George Fodor, J. Worldwide epidemic of hypertension. Can. J. Cardiol. 2006, 22, 553–555. [Google Scholar] [CrossRef]
- Zhou, B.; Lu, Y.; Hajifathalian, K.; Bentham, J.; Di Cesare, M.; Danaei, G.; Bixby, H.; Cowan, M.J.; Ali, M.K.; Taddei, C.; et al. Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4·4 million participants. Lancet 2016, 387, 1513–1530. [Google Scholar] [CrossRef]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Volgman, A.S.; Palaniappan, L.S.; Aggarwal, N.T.; Gupta, M.; Khandelwal, A.; Krishnan, A.V.; Lichtman, J.H.; Mehta, L.S.; Patel, H.N.; Shah, K.S.; et al. Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments: A Scientific Statement from the American Heart Association. Circulation 2018, 138, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Marques, M.d.C.; Pires, R.; Perdigão, M.; Sousa, L.; Fonseca, C.; Pinho, L.G.; Lopes, M. Patient-Centered Care for Patients with Cardiometabolic Diseases: An Integrative Review. J. Pers. Med. 2021, 11, 1289. [Google Scholar] [CrossRef] [PubMed]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef] [PubMed]
- CES HESE. Comissão de Ética para a Saúde, Hospital do Espírito Santo, EPE, Évora. Available online: https://www.hevora.min-saude.pt/2021/12/09/comissao-de-etica/ (accessed on 28 August 2022).
- Marôco, J. Análise Estatística com o SPSS Statistics (v.18-27), 8th ed.; ReportNumber: Pêro Pinheiro, Portugal, 2021. [Google Scholar]
- Medzikovic, L.; Cunningham, C.M.; Li, M.; Amjedi, M.; Hong, J.; Ruffenach, G.; Eghbali, M. Sex differences underlying preexisting cardiovascular disease and cardiovascular injury in COVID-19. J. Mol. Cell. Cardiol. 2020, 148, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Goes, M.; Lopes, M.; Marôco, J.; Oliveira, H.; Fonseca, C. Psychometric properties of the WHOQOL-BREF(PT) in a sample of elderly citizens. Health and Quality of Life Outcomes 2021, 19, 146. [Google Scholar] [CrossRef]
- Goes, M.; Lopes, M.J.; Oliveira, H.; Fonseca, C.; Marôco, J. A Nursing Care Intervention Model for Elderly People to Ascertain General Profiles of Functionality and Self Care Needs. Sci. Rep. 2020, 10, 1770. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for Europe and European Observatory on Health Systems Policies. In Health System Review: Portugal: Phase 1 Final Report; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2018; Available online: https://apps.who.int/iris/handle/10665/345635 (accessed on 19 August 2022).
- Quinaz Romana, G.; Kislaya, I.; Salvador, M.R.; Gonçalves, S.C.; Nunes, B.; Dias, C. Multimorbidity in Portugal: Results from The First National Health Examination Survey. Acta Méd. Port. 2019, 32, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.W.; Aronow, W.S.; Frishman, W.H. Coronavirus Disease 2019 and Cardiometabolic Disease. Cardiol. Rev. 2021, 30, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Mechanick, J.I.; Rosenson, R.S.; Pinney, S.P.; Mancini, D.M.; Narula, J.; Fuster, V. Coronavirus and Cardiometabolic Syndrome. J. Am. Coll. Cardiol. 2020, 76, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- Rawshani, A.; Kjölhede, E.A.; Rawshani, A.; Sattar, N.; Eeg-Olofsson, K.; Adiels, M.; Ludvigsson, J.; Lindh, M.; Gisslén, M.; Hagberg, E.; et al. Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: A nationwide retrospective cohort study. Lancet Reg. Health-Eur. 2021, 4, 100105. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, A.J.; Abdelhafiz, A.H. Cardiometabolic disease in the older person: Prediction and prevention for the generalist physician. Cardiovasc. Endocrinol. Metab. 2020, 9, 90–95. [Google Scholar] [CrossRef]
- Atamna, H.; Tenore, A.; Lui, F.; Dhahbi, J.M. Organ reserve, excess metabolic capacity, and aging. Biogerontology 2018, 19, 171–184. [Google Scholar] [CrossRef]
- Silva, G.M.d.; Pesce, G.B.; Martins, D.C.; Carreira, L.; Fernandes, C.A.M.; Jacques, A.E. Obesidade como fator agravante da COVID-19 em adultos hospitalizados: Revisão integrativa. Acta Paul. Enferm. 2021, 34, eAPE02321. [Google Scholar] [CrossRef]
- Qi, S.; Ngwa, C.; Morales Scheihing, D.A.; Al Mamun, A.; Ahnstedt, H.W.; Finger, C.E.; Colpo, G.D.; Sharmeen, R.; Kim, Y.; Choi, H.A.; et al. Sex differences in the immune response to acute COVID-19 respiratory tract infection. Biol. Sex Differ. 2021, 12, 66. [Google Scholar] [CrossRef]
- Takahashi, T.; Iwasaki, A. Sex differences in immune responses. Science 2021, 371, 347–348. [Google Scholar] [CrossRef]
- Machida, M.; Nakamura, I.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; Kojima, T.; et al. Adoption of personal protective measures by ordinary citizens during the COVID-19 outbreak in Japan. Int. J. Infect. Dis. 2020, 94, 139–144. [Google Scholar] [CrossRef]
- Suen, L.K.P.; Siu, G.K.H.; Guo, Y.P.; Yeung, S.K.W.; Lo, K.Y.K.; O’Donoghue, M. The public washroom—Friend or foe? An observational study of washroom cleanliness combined with microbiological investigation of hand hygiene facilities. Antimicrob. Resist. Infect. Control 2019, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Lewis, A.M.; Moley, J.R.; Brestoff, J.R. A systematic review and meta-analysis of obesity and COVID-19 outcomes. Sci. Rep. 2021, 11, 7193. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.S.Y.; Fernando, D.I.; Chan, M.Y.; Sia, C.-H. Obesity in COVID-19: A Systematic Review and Meta-analysis. Ann. Acad. Med. Singap. 2020, 49, 996–1008. [Google Scholar] [CrossRef] [PubMed]
- Földi, M.; Farkas, N.; Kiss, S.; Zádori, N.; Váncsa, S.; Szakó, L.; Dembrovszky, F.; Solymár, M.; Bartalis, E.; Szakács, Z.; et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: A systematic review and meta-analysis. Obes. Rev. 2020, 21, e13095. [Google Scholar] [CrossRef]
- Yang, J.; Tian, C.; Chen, Y.; Zhu, C.; Chi, H.; Li, J. Obesity aggravates COVID-19: An updated systematic review and meta-analysis. J. Med. Virol. 2020, 93, 2662–2674. [Google Scholar] [CrossRef]
- Huang, Y.; Lu, Y.; Huang, Y.-M.; Wang, M.; Ling, W.; Sui, Y.; Zhao, H.-L. Obesity in patients with COVID-19: A systematic review and meta-analysis. Metabolism 2020, 113, 154378. [Google Scholar] [CrossRef]
- Pereira, M.; Rocha, L.; Sartori, L.; Souza, M.; Lima, R.; Rodrigues Júnior, A. Descriptive study of COVID-19 mortality according to sex, schooling, age, health region and historical series: State of Rio de Janeiro, January 2020 to August 2021. SciELO Prepr. 2022. [Google Scholar] [CrossRef]
- Ribeiro, M.A. COVID-19 na População Portuguesa: Uma Análise de Riscos Competitivos. Master’s Thesis, Universidade de Lisboa—Faculdade de Ciências, Lisboa, Portugal, 2022. Available online: http://hdl.handle.net/10451/53755 (accessed on 31 August 2022).
- Zheng, Z.; Peng, F.; Xu, B.; Zhao, J.; Liu, H.; Peng, J.; Li, Q.; Jiang, C.; Zhou, Y.; Liu, S.; et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020, 81, e16–e25. [Google Scholar] [CrossRef]
| Variables | N | % | Min/Max/Avg |
|---|---|---|---|
| Sex: | |||
| Male | 33 | 32.4 | |
| Female | 69 | 67.6 | |
| Age: | |||
| Male | - | - | 27/92/66.0 |
| Female | - | - | 42/94/68.3 |
| Cardiometabolic disorders: | |||
| None | 18 | 21.7 | |
| One | 14 | 16.9 | |
| Two | 19 | 22.9 | |
| Three | 22 | 26.5 | |
| Four | 10 | 12.0 | |
| Hypertension | 56 | 55.4 | |
| Dyslipidemia | 35 | 34.7 | |
| Diabetes | 30 | 29.7 | |
| Obesity | 26 | 25.7 | |
| CVD | 24 | 23.8 | |
| Days between dates of a positive COVID-19 test and hospitalization | - | - | 0/13/4.1 |
| Days between dates of hospitalization and ICU admission | - | - | 0/24/2.9 |
| Days in ICU: | - | - | 0/85/14.2 |
| Passed away | - | - | 0/53/16.2 |
| Survived | - | - | 1/85/13.5 |
| Variables | Age | Total Number of Cardiometabolic Disorders |
|---|---|---|
| Days between positive COVID-19 test and hospitalization | 0.21 (p = 0.051) 1 | 0.03 (p = 0.777) |
| Days between hospitalization and ICU admissions | 0.19 (p = 0.063) 1 | 0.09 (p = 0.389) |
| Days in ICU | 0.30 (p = 0.007) | 0.04 (p = 0.711) |
| Total number of Cardiometabolic disorders | 0.22 (p = 0.033) | - |
| Variables | B1 | S.E. 2 | 3 | d.f.4 | p | Exp(B) 5 | 95% CI for Exp(B) 6 |
|---|---|---|---|---|---|---|---|
| Sex | 0.163 | 0.663 | 0.061 | 1 | 0.806 | 1.177 | [0.321; 4.318] |
| Age | 0.046 | 0.026 | 4.017 | 1 | 0.045 | 1.047 | [1.003; 1.098] |
| Obesity | 0.338 | 0.755 | 3.039 | 1 | 0.081 | 1.402 | [0.978; 4.686] |
| Diabetes | 0.803 | 0.604 | 1.769 | 1 | 0.183 | 2.232 | [0.684; 7.288] |
| Dyslipidemia | 0.142 | 0.604 | 0.155 | 1 | 0.694 | 1.153 | [0.266 3.835] |
| Hypertension | 0.052 | 0.607 | 0.007 | 1 | 0.932 | 1.053 | [0.289; 3.120] |
| CVD | 0.988 | 0.623 | 2.767 | 1 | 0.096 | 2.686 | [0.816; 9.939] |
| Constant | −3.763 | 1.809 | 4.326 | 1 | 0.038 | 0.023 | - |
| Independent Variables | B1 | S.E. 2 | Standardized B 3 | t | p |
|---|---|---|---|---|---|
| Sex | −1.898 | 0.919 | −0.213 | −2.065 | 0.042 |
| Age | 0.038 | 0.038 | 0.108 | 1.000 | 0.320 |
| Obesity | −1.302 | 0.993 | −0.140 | −1.312 | 0.193 |
| Diabetes | −1.301 | 0.946 | −0.144 | −1.375 | 0.173 |
| Dyslipidemia | −0.668 | 1.006 | −0.078 | −0.664 | 0.508 |
| Hypertension | 1.098 | 0.885 | 0.131 | 1.240 | 0.218 |
| CVD | 0.719 | 1.042 | 0.076 | 0.690 | 0.492 |
| Constant | 5.894 | 0.878 | - | 6.709 | <0.001 |
| Independent Variables | B1 | S.E. 2 | Standardized B 3 | t | p |
|---|---|---|---|---|---|
| Sex | 0.291 | 0.928 | 0.034 | 0.313 | 0.755 |
| Age | 0.009 | 0.039 | 0.026 | 0.227 | 0.821 |
| Obesity | −1.875 | 0.904 | −0.206 | −2.075 | 0.041 |
| Diabetes | 0.604 | 0.902 | 0.069 | 0.670 | 0.505 |
| Dyslipidemia | 1.008 | 0.903 | 0.120 | 1.116 | 0.267 |
| Hypertension | 0.038 | 0.910 | 0.005 | 0.041 | 0.967 |
| CVD | 0.316 | 1.008 | 0.034 | 0.314 | 0.754 |
| Constant | 2.919 | 0.568 | - | 5.137 | <0.001 |
| Independent Variables | B1 | S.E. 2 | Standardized B 3 | t | p |
|---|---|---|---|---|---|
| Sex | −0.401 | 3.556 | −0.014 | −0.113 | 0.911 |
| Age | 0.277 | 0.131 | 0.236 | 2.119 | 0.037 |
| Obesity | 3.310 | 3.783 | 0.107 | 0.875 | 0.385 |
| Diabetes | 4.535 | 3.503 | 0.151 | 1.295 | 0.200 |
| Dyslipidemia | 1.863 | 3.504 | 0.065 | 0.532 | 0.597 |
| Hypertension | 6.055 | 3.457 | 0.220 | 1.752 | 0.084 4 |
| CVD | −4.548 | 3.809 | −0.142 | −1.194 | 0.237 |
| Constant | −3.889 | 8.726 | - | −6.575 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pires, R.; Pedrosa, M.; Marques, M.; Goes, M.; Oliveira, H.; Godinho, H. Cardiometabolic Risk after SARS-CoV-2 Virus Infection: A Retrospective Exploratory Analysis. J. Pers. Med. 2022, 12, 1758. https://doi.org/10.3390/jpm12111758
Pires R, Pedrosa M, Marques M, Goes M, Oliveira H, Godinho H. Cardiometabolic Risk after SARS-CoV-2 Virus Infection: A Retrospective Exploratory Analysis. Journal of Personalized Medicine. 2022; 12(11):1758. https://doi.org/10.3390/jpm12111758
Chicago/Turabian StylePires, Rute, Miguel Pedrosa, Maria Marques, Margarida Goes, Henrique Oliveira, and Hélder Godinho. 2022. "Cardiometabolic Risk after SARS-CoV-2 Virus Infection: A Retrospective Exploratory Analysis" Journal of Personalized Medicine 12, no. 11: 1758. https://doi.org/10.3390/jpm12111758
APA StylePires, R., Pedrosa, M., Marques, M., Goes, M., Oliveira, H., & Godinho, H. (2022). Cardiometabolic Risk after SARS-CoV-2 Virus Infection: A Retrospective Exploratory Analysis. Journal of Personalized Medicine, 12(11), 1758. https://doi.org/10.3390/jpm12111758








