Abstract
The clinical presentation of COVID-19 is extremely heterogeneous, ranging from asymptomatic to severely ill patients. Thus, host genetic factors may be involved in determining disease presentation and progression. Given that carriers of single cystic fibrosis (CF)-causing variants of the CFTR gene—CF-carriers—are more susceptible to respiratory tract infections, our aim was to determine their likelihood of undergoing severe COVID-19. We implemented a cohort study of 874 individuals diagnosed with COVID-19, during the first pandemic wave in Italy. Whole exome sequencing was performed and validated CF-causing variants were identified. Forty subjects (16 females and 24 males) were found to be CF-carriers. Among mechanically ventilated patients, CF-carriers were more represented (8.7%) and they were significantly (p < 0.05) younger (mean age 51 years) compared to noncarriers (mean age 61.42 years). Furthermore, in the whole cohort, the age of male CF-carriers was lower, compared to noncarriers (p < 0.05). CF-carriers had a relative risk of presenting an abnormal inflammatory response (CRP ≥ 20 mg/dL) of 1.69 (p < 0.05) and their hazard ratio of death at day 14 was 3.10 (p < 0.05) in a multivariate regression model, adjusted for age, sex and comorbidities. In conclusion, CF-carriers are more susceptible to the severe form of COVID-19, showing also higher risk of 14-day death.
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is one of the members of the Coronaviridae family [1] that, since December 2019, has caused pandemic outbreaks of human infections [2].
The clinical presentation of the coronavirus disease (COVID-19) is particularly heterogeneous ranging from asymptomatic [3] to critically ill patients [4]. Beside the majority of subjects presenting with mild symptoms, the reported severe cases are characterized by bilateral pneumonia associated with an extreme inflammatory response [5], hepatitis [6], pancreatic involvement [7], cardiac injury, renal failure, neurologic and thromboembolic complications [1,5,8,9].
While age and the presence of pre-existing conditions, like diabetes and cardiovascular diseases, explain to some extent the worse prognosis of certain patients [4,10], it is conceivable that host genetic factors may contribute to disease presentation and progression. In this direction, it has been identified a genetic locus, corresponding to the ABO-blood group, that is highly represented in COVID-19 patients with respiratory failure [11]. Furthermore, deletion in the gene encoding for the NKG2C receptor (KLRC2) that mediates the activation of natural killer cells, has been shown to be associated with the severe form of COVID-19 [12] and monogenic defects of immunity to SARS-CoV-2, appeared in 3.5% of patients with life-threatening COVID-19 pneumonia [13]. Additional studies aimed at detangling the host genetic complexity in determining COVID-19 susceptibility and clinical presentation are ongoing, including a global initiative [14] to which our GEN-COVID consortium belongs [15,16,17,18,19,20].
GEN-COVID is a multicenter observational study, conducted in 28 hospitals, primary care centers and public health units in Italy, performing extensive genetic and clinical characterizations of patients affected by COVID-19 [15,16,17,18,19,20]. As part of this national effort, we conducted the present study, under the hypothesis that a subset of individuals carrying single pathogenic variants of the cystic fibrosis transmembrane conductance regulator (CFTR) gene is more susceptible to the most critical form of COVID-19. CFTR is a chloride and bicarbonate channel expressed on the apical membrane of epithelial cells, mainly in lung, liver, pancreas and intestine [21], where also ACE2 (angiotensin-converting enzyme 2), the entry receptor for SARS-CoV-2 [22], is localized [23]. When both copies of the CFTR gene are mutated, patients are affected by cystic fibrosis (CF), a genetic disease characterized by high viscosity of secreted fluids and by an abnormal inflammatory response, independent but aggravated by infections [24], leading to respiratory failure and premature death [21]. Carriers of one CF-causing variant, have a reduction in CFTR expression and function, depending on the type of the pathogenic variant, and have high risk of developing CF-related conditions [25]. In particular, they are known to be significantly more susceptible to airway and sinus infections, pneumonia, pancreatic injury and hepatitis [25,26]: all conditions described in the severe form of COVID-19 [4,6,7].
Therefore, the objective here was to identify, among patients enrolled in the GEN-COVID cohort [15,16,17,18,19,20], those that are carriers of single pathogenic variants of the CFTR gene and evaluate their clinical course, in order to determine to what extent CFTR impairment contributes to COVID-19 susceptibility and severity.
2. Materials and Methods
Patient population. Patients affected by COVID-19 were recruited through the GEN-COVID multicenter study (NCT04549831) in 28 hospitals, local healthcare units and departments of preventive medicine in Italy from 8 April to 30 June 2020 [15,16,17,18,19,20]. All the enrolled patients were adults (aged ≥18 years) with SARS-CoV-2 infection confirmed by reverse transcriptase-polymerase chain reaction (PCR) assay on nasopharyngeal swab. The clinical severity of COVID-19 was assessed using a modified version of the WHO COVID-19 Outcome Scale [27], identifying the following six categories: 1, death; 2, hospitalized receiving invasive mechanical ventilation; 3, hospitalized, receiving continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) ventilation; 4, hospitalized, receiving low-flow supplemental oxygen; 5, hospitalized, not receiving supplemental oxygen; 6, not hospitalized. The GEN-COVID study was approved by the Institutional Review Board (IRB) of the Siena University Hospital (Protocol n. 16917, 16 March 2020) and by the local IRBs of all the recruiting hospitals involved. Patients or legally authorized representatives provided informed consent for participating in the study.
Whole Exome sequencing analysis and identification of CFTR pathogenic variants. Whole Exome sequencing with at least 97% coverage at 20× was performed using the Illumina NovaSeq6000 System (Illumina, San Diego, CA, USA). Library preparation was performed using the Illumina Exome Panel (Illumina) following manufacturer’s protocol. Library enrichment was tested by qPCR, and the size distribution and concentration were determined using Agilent Bioanalyzer 2100 (Agilent Technologies, Santa Clara, CA, USA). The Novaseq6000 System (Illumina) was used for DNA sequencing through 150 bp paired-end reads. Variants calling was performed according to the GATK4 best practice guidelines for joint calling, using BWA for mapping. The results of the joint call were annotated by ANNOVAR, and variants in the CFTR gene already reported as disease causing in the “CFTR2 Database-Clinical and Functional Translation of CFTR” (https://cftr2.org/, last accessed on 12 June 2021) and/or in ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/, last accessed on 12 June 2021) were selected.
Statistical methods. Wilcoxon rank-sum test was applied to compare differences between two groups for not-normally distributed values while an independent Student’s t-test was used for normally distributed ones. The binary association between the presence of CF-causing variant and the COVID-19 Outcome scale was assessed using the Cochran–Armitage test for trend. The Fisher–Freeman–Halton test or Fisher exact test were used when testing association between categorical variables [28] as indicated. Relative risk (RR) of severe clinical outcome was estimated in carriers vs noncarriers, with and without adjustment for patient age. To define severe outcome, the following parameters were set: PaO2/FiO2 ≤ 250 indicating severe respiratory impairment; C Reactive Protein (CRP) ≥ 20 mg/dL; ALT and AST ≥ 40 U/L; LDH ≥ 400 U/L. Overall survival (OS) curves were estimated with the Kaplan-Meier method and compared with the log-rank test. OS time was calculated from the date of patient admission to the day of death from any cause related to COVID-19 or the discharge day for alive patients. The nonhospitalized patients were included in the analyses with an OS time equal to 1 day, as they were enrolled the same day of the nasopharyngeal swab execution and limited follow-up was performed. The same strategy was adopted for hospitalized patients lost to follow-up after the hospitalization. Cox regression analysis was used for univariable and multivariable analyses of association between OS and carrier status. Due to the low number of OS events, in multivariable Cox analysis the adjustment for confounding variables (i.e., patients’ age and sex, chronic conditions, such as hypertension, diabetes, asthma/ chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF) and coronary artery disease (CAD), malignancy, hypothyroidism, obesity, and admission period less than or greater or equal to 15 April 2020) was operated by means of a score beforehand estimated as the linear predictor from a Cox model including all the confounding variables. The admission period less than or greater or equal to 15 April 2020 was chosen as a proxy for the different hospital admission conditions in the very first pandemic period, that severely hit Italy, vs the most recent one. Continuous variables were presented as mean ± SD or median (interquartile range, IQR) as indicated.
Statistical analyses were performed with SAS (SAS Institute, Cary, NC, USA), R- (R-Foundation for Statistical Computing, Vienna, Austria) and STATA/IC 15.0 software on a mac workstation. Statistical significance was set at 5% level.
3. Results
3.1. Cohort Patients
Eight-hundred and seventy-four patients (43.13% females, 56.75% males) were studied (Table 1). The mean age was 59.9 years (SD, 15.64) and it was significantly higher in all the hospitalized categories compared to the nonhospitalized one (Table 1). In all the hospitalized categories there was a significantly higher prevalence of males compared to category 6, i.e., patients not requiring hospitalization; in particular, 74.29% of the subjects that underwent invasive mechanical ventilation were males (p < 0.001) (Table 1). The most frequent associated chronic conditions are listed in Table 1 and Supplementary Table S1.

Table 1.
Demographic and clinical characteristics of the enrolled patients.
3.2. Identified CFTR Pathogenic Variants
Seventeen CF-causing variants were identified in 41 COVID-19 patients (Supplementary Table S2). The majority of carriers (n = 13) had a genomic deletion of three base pairs resulting in the loss of phenylalanine at amino acid position 508 of the CFTR protein (Supplementary Table S2). Nobody was carrier of the TG12-5T polymorphism, nor the TG13-5T known to reduce CFTR function [29].
3.3. Demographics and Clinical Characteristics of CF Carriers
Forty patients (4.58% of the whole cohort), 26 males (65%) and 14 females (35%), were identified as carriers of one CF-causing variant in the CFTR gene while one patient (male, 52 years) was found to have two pathogenic variants (Supplementary Table S2). The following analyses were performed including only carriers of single variants. Carriers’ prevalence increased with the worsening of COVID-19 Outcome scale, peaking to 8.7% in patients undergoing invasive mechanical ventilation and being 2.54% in patients receiving low oxygen flow (Table 2). This trend was significantly evident (p < 0.0001) for patients younger than 50 years; among them, 25% of those receiving invasive mechanical ventilation were carriers. Patients carrying CF-causing variants were prevalently males in all the outcome categories except for category 1 and 3; in particular, 83.33% of carriers receiving invasive mechanical ventilation were males (Supplementary Table S3).

Table 2.
Carriers of single CFTR pathogenic variants.
Overall, male carriers were significantly younger (mean age ± SD: 53.08 ± 18.8 years) compared to noncarriers (mean age ± SEM: 60.37 ± 14.57 years) (p < 0.05) and they underwent invasive mechanical ventilation at a mean age of 51 years while noncarriers at 61.42 years (p < 0.05) (Table 3). The prevalence of comorbidities was not different between the two groups except for hypertension that was higher in not carriers (Supplementary Table S5).

Table 3.
Demographics of carriers vs noncarriers.
Patients were monitored during the whole course of the hospitalization and the worse clinical and biochemical parameters were registered. The RR of undergoing respiratory impairment (PaO2/FiO2 ≤ 250) for carriers was 1.54 (95% CI: 0.99–1.76; p = 0.053) suggesting that they were prone to develop an acute respiratory distress syndrome (ARDS) associated with widespread inflammation. Indeed, their RR of having levels of CRP ≥ 20 mg/dL (twice the upper limit) was 1.69 (95% CI: 1.06–2.29; p = 0.03) (Table 4). No significant higher risk of increased liver enzymes, and LDH was registered for carriers. All the carriers for whom the serum pancreatic profile was available (n = 3) showed a marked hyperlipasemia (serum lipase ≥ 360 U/L).

Table 4.
Outcome RR for carriers of CF-causing variants adjusted for age.
3.4. Mortality in Carriers of CF-Causing Variants
Among the 874 patients included in the study, 55 patients (6.29%) underwent exitus. Their mean age was 75.73 years (SD, 10.98) and 54.55% of them were males (Table 1). Fatal cases (category 1) showed a higher prevalence of hypertension (25.45%), cardiovascular diseases (14.55%), asthma and COPD (9.09%), malignancy (7.27%) compared to the nonhospitalized category (Supplementary Table S1).
In an univariable Cox analysis of independent risk factors related to fatal outcome at day 14 after hospital admission, CF-carrier status showed HR of 2.86 (95% CI: 1.01–8.15; p = 0.04); after adjustment for confounding variables (age, sex, comorbidities) in a multivariate Cox analysis the HR for CF carriers raised to 3.10 (95% CI: 1.09–8.85; p = 0.03) (Figure 1; Supplementary Table S5). The Kaplan–Meier estimates of 14-day survival were 85.42% (95% CI, 65.51 to 94.30) for the carriers and 93.63 % (95% CI, 90.70 to 95.66) for the noncarriers (p = 0.03 Log rank test) (Figure 1).
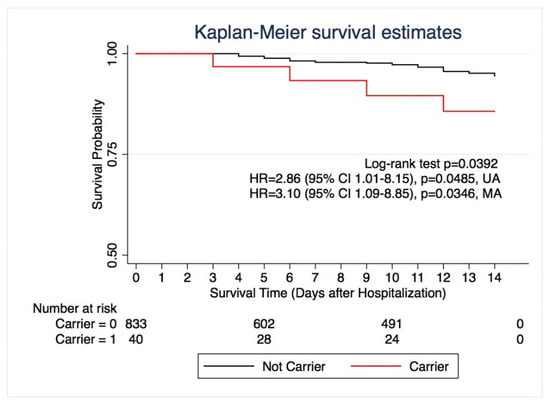
Figure 1.
Survival Study: Kaplan–Meier 14-day survival study comparing carriers of single CF-causing variants (red) and noncarriers (black). Log-rank test p = 0.0392; Univariable Cox analysis (UA) HR = 2.86; 95% CI 1.01–8.15; p = 0.0485. Multivariable Cox analysis (MA) with adjustment for confounding variables HR = 3.10; 95% CI, 1.09–8.85; p = 0.0346.
When considering only hospitalized patients, the 14-day survival was 85.15% (95% CI, 72.66–99.79) for carriers and 94.04 % (95% CI, 91.93 to 96.19) for the noncarriers (p = 0.0447 Log rank test). The HR of 14-day death for carriers was 3.06 (95% CI, 1.07–8.73; p = 0.0365) after adjustment for confounding variables.
Other independent factors for early mortality (14 days after admission) were: age ≥ 75 years (HR: 4.53; 95% CI, 2.27–9.04; p < 0.0001); LDH ≥ 400 (HR: 3.64; 95% CI, 1.30–10.22; p = 0.0141) (Supplementary Table S5). Univariable Cox analysis of independent risk factors related to fatal outcome at day 28 and 60 after hospitalization, showed a HR for CF carriers equal to 1.97 (95% CI: 0.70–5.5; p = 0.1978) and 1.70 (95% CI: 0.61–4.73; p = 0.3087) respectively (Supplementary Table S5).
4. Discussion
In the present study we described the peculiarity of the CF-carriers in-hospital clinical course, characterized by high inflammatory response, severe respiratory impairment and higher risk of 14-day in-hospital mortality.
Carriers of CF-causing variants are known to have a reduction in CFTR function of about 50% the physiological level [30,31]. Although these individuals do not have CF, they are more susceptible to numerous CF-related diseases like pancreatitis, hepatitis and respiratory tract infections [25,26,32]. In our cohort, hospitalized CF carriers develop indeed a form of COVID-19 more likely characterized by acute respiratory distress syndrome (PaO2/FiO2 ratio ≤ 250 mmHg), high inflammatory response (CRP ≥ 20 mg/dL), and, for some of them hyperlipasemia. Moreover, carriers undergoing invasive mechanical ventilation have a mean age of 51 years, being significantly younger than noncarriers in the same clinical category. Thus, those evidences suggest that CF carriers may be prone also to develop a severe manifestation of COVID-19, and even at a younger age compared to noncarriers.
In our cohort the majority (83.33%) of CF carriers mechanically ventilated were males and in all the hospitalized categories there was a higher prevalence of male individuals. Such a result confirms a world trend that identifies the male sex as a relevant risk factor for severe COVID-19 [33,34]. While our GEN-COVID consortium has shown that male individuals carrying longer androgen receptor polyQ alleles are more critically ill [19], the high expression of ACE2, the entry receptor of SARS-CoV-2 [22], in testes could also be considered a putative factor determining gender susceptibility to the severe form of the disease [35].
Although numerous studies are now ongoing to clearly understand the complex pathogenesis of severe COVID-19, the respiratory impairment seems to be triggered by both a direct cytotoxic action of SARS-CoV-2 on airway cells and by an abnormal self-perpetuating inflammatory response [5,36]. ACE2 is known to exert anti-inflammatory effects by counterbalancing the proinflammatory action of the angiotensin-converting enzyme (ACE). After the binding virus-receptor, ACE2 expression in the lung is reduced, because of its internalization, leading to a proinflammatory cascade of cytokines through the NF-kB signaling and to a consequent lung injury [36,37]. Such pathogenic mechanism of action may occur also in other organs, expressing ACE2 receptors, that are affected by COVID-19, like the gastro-intestinal tract and the pancreas [4]. Indeed, 12 to 17% of patients with COVID-19 develop an elevation of pancreatic enzymes [7,38], as some CF carriers in our cohort showing elevated levels of lipase.
The predisposition of CF-carriers to severe COVID-19, also hypothesized by others [39], is probably related to multiple factors: i. the acidification of the airway surface liquid that impairs immune response [40]; ii. a reduced CFTR function [30,31] that upregulates the proinflammatory signaling, and that is associated with a deficiency in pro-solving mediators, known to promote the resolution of the inflammation [24] and iii. an accumulation of misfolded CFTR that may trigger NF-kB signaling [39]. Interestingly CFTR and ACE2 are known to colocalize in numerous epithelial cells, especially in the respiratory tract [23]. Thus, it is conceivable that in CF carriers the concomitant downregulation of CFTR and ACE2—having both events a proinflammatory effect—may lead to a more severe COVID-19 clinical presentation. While the hypothesized mechanisms are present, even to a larger extent, in carriers of two CF-causing variants, it’s interesting to notice that CF patients undergo, instead, a mild form of COVID-19 [41,42,43]. The explanation may lay the fact that CF patients, while costumed to always wear protective masks, are often treated with modulators that re-establish CFTR function or with other drugs, like azithromycin, that may protect against infections [41,42]. Detangling the role of CFTR in COVID-19 pathogenesis would for sure help to better understand such deadly disease, considering also that a previous GWAS study has described an intronic variant in the CFTR gene to be highly represented in patients with pneumonia [44].
One year after the first report on a novel coronavirus disease, the registered deaths have been more than 1.8 million worldwide [2]. Here we propose a novel survival study encompassing, not only demographics and clinical parameters of the patients but also their genetic profile related to CFTR. In our model, while we confirmed [45] age ≥ 75 and AST ≥ 40 U/L to be relevant risk factors for mortality at all the studied time points and at 28/60-days respectively, we identified the status of CF carrier, LDH ≥ 400, age ≥ 75—to be determinants of mortality at day 14. In particular, being a carrier of known CF-causing variants appears to be a relevant factor (HR, 3.10, CI, 1.09–8.85) determining early mortality after adjustments for age, sex and comorbidities. Importantly, at the later time-points (day-28 and day-60) CF carrier status does not appear to be anymore a risk factor for death. Such a finding reveals that COVID-19 mortality is determined by time-dependent factors and that CFTR-related early events like cytokine storm may be responsible for early death.
The current study is limited to the Caucasian race, predominant in the Italian population. However, in our opinion those findings may be transferable to the other ethnicities, considering that in-hospital mortality does not appear to differ between white and black patients [46]. A further limitation of our study sits in the number of carriers studied (n = 40) that although resulting from a cohort of 874 patients, doesn’t allow more complex epidemiological analysis. Finally, as indicated in the methods section, the follow-up of not hospitalized patients is restricted to the initial stage of the disease.
5. Conclusions
In conclusion, while more studies should be performed to understand the role of CFTR in COVID-19 pathogenesis, in our opinion, the presented results may have relevant and immediate clinical implications. Indeed, CF is one of the most frequent genetic diseases in Caucasians with an estimated prevalence of one per 25/30 individuals [21] and the numerous people are CF carriers, considering also the effective CF-screening programs ongoing globally [47]. Thus, the status of CF carrier, given its high prevalence, should be investigated in COVID-19 hospitalized patients in order to identify subjects that, being at risk of severe disease, would benefit of intensive surveillance and personalized therapy.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jpm11060558/s1, Table S1: Prevalence of comorbidities by COVID-19 outcome scale and sex; Table S2: CF-causing variants in COVID-19 patients; Table S3: Carriers of CFTR Pathogenic Variants; Table S4: Prevalence of comorbidities by carrier status; Table S5: Univariable Cox Analysis of risk factors related to fatal outcome.
Author Contributions
Conceptualization: C.G., A.R., F.M., E.F.; data curation: C.G., M.B., F.F., F.C., E.Q.-R., M.U.M., GEN-COVID Multicenter Study; formal analysis: C.G., F.V., G.D., A.G., S.A.; funding acquisition: A.R.; investigation: C.G., M.B., F.F., E.F., A.R.; methodology: E.F., L.D.S., M.P., M.L.C., D.A., G.B., N.I., S.A.; resources: A.R.; software: C.F., S.D., E.B., K.Z.; supervision: C.G., A.R., S.F.; validation: A.R., R.M., C.G.; visualization: C.G., C.F., M.B., F.F., C.F., A.R., R.M.; writing—original draft: C.G., C.F., M.B., F.F., C.F., A.R., R.M.; writing—review & editing: C.G., C.F., M.B., F.F., C.F., A.R., R.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the MIUR grant “Dipartimenti di Eccellenza 2018-2020” to the Department of Medical Biotechnologies University of Siena, Italy; the “Bando Ricerca COVID-19 Toscana” grant to the Azienda Ospedaliero Universitaria Senese; the “Intesa San Paolo 2020 charity fund” dedicated to the project NB/2020/0119 “Identificazione delle basi genetiche determinanti la variabilità clinica della risposta a COVID-19 nella popolazione italiana”; philanthropic donations to the Department of Medical Biotechnologies, University of Siena for the COVID-19 host genetics research project (D.L n.18 of 17 March 2020).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of the University of Siena, Italy (Protocol n. 16917, 16 March 2020) and by the locals IRB of participating hospitals.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available upon reasonable request to A.R.
Acknowledgments
Authors are grateful to: the CINECA consortium for providing computational resources; the Network for Italian Genomes (NIG) (http://www.nig.cineca.it, last accessed on 12 June 2021) for its support; the COVID-19 Host Genetics Initiative (https://www.covid19hg.org/, last accessed on 12 June 2021); the Genetic Biobank of Siena, member of BBMRI-IT, Telethon Network of Genetic Biobanks (project no. GTB18001), EuroBioBank, and RD-Connect, for managing specimens. In addition, the gratitude of the Authors goes to all the patients that consented to participate in the GEN-COVID study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Appendix A
GEN-COVID Multicenter Study Members (https://sites.google.com/dbm.unisi.it/gen-covid): Rossella Tita3, Mirella Bruttini1,2,3, Susanna Croci1,2, Ilaria Meloni1,2, Anna Maria Pinto3, Maria Antonietta Mencarelli3, Caterina Lo Rizzo3, Valentina Perticaroli1,2,3, Francesca Montagnani2,9, Mario Tumbarello2,9, Gabriele Inchingolo1,2, Massimiliano Fabbiani9, Barbara Rossetti9, Giacomo Zanelli2,9, Elena Bargagli10, Laura Bergantini10, Miriana D’Alessandro10, Paolo Cameli10, David Bennett10, Federico Anedda11, Simona Marcantonio11, Sabino Scolletta11, Federico Franchi11, Maria Antonietta Mazzei12, Susanna Guerrini12, Edoardo Conticini13, Luca Cantarini13, Bruno Frediani13, Danilo Tacconi14, Chiara Spertilli Raffaelli14, Marco Feri15, Alice Donati15, Raffaele Scala16, Luca Guidelli16, Genni Spargi17, Marta Corridi17, Cesira Nencioni18, Leonardo Croci18, Gian Piero Caldarelli19, Maurizio Spagnesi20, Paolo Piacentini20, Maria Bandini20, Elena Desanctis20, Silvia Cappelli20, Anna Canaccini21, Agnese Verzuri21, Valentina Anemoli21, Agostino Ognibene22, Alessandro Pancrazi22, Maria Lorubbio22, Massimo Vaghi23, Antonella D’Arminio Monforte24, Esther Merlini24, Federica Gaia Miraglia24, Raffaele Bruno25,26, Marco Vecchia25, Stefania Mantovani25, Serena Ludovisi25,26, Massimo Girardis27, Sophie Venturelli27, Marco Sita27, Andrea Cossarizza28, Andrea Antinori29, Alessandra Vergori29, Arianna Emiliozzi29, Stefano Rusconi30,31, Matteo Siano31, Arianna Gabrieli31, Agostino Riva30,31, Daniela Francisci32,33, Elisabetta Schiaroli32, Francesco Paciosi32, Andrea Tommasi32, Pier Giorgio Scotton34, Francesca Andretta34, Sandro Panese35, Renzo Scaggiante36, Francesca Gatti36, Saverio Giuseppe Parisi37, Melania degli Antoni38, Isabella Zanella39,40, Matteo Della Monica41, Carmelo Piscopo41, Mario Capasso42,43,44, Roberta Russo42,43, Immacolata Andolfo42,43, Achille Iolascon42,43, Giuseppe Fiorentino45, Massimo Carella46, Marco Castori46, Filippo Aucella47, Pamela Raggi48, Carmen Marciano48, Rita Perna48, Matteo Bassetti49,50, Antonio Di Biagio49,50, Maurizio Sanguinetti51,52, Luca Masucci51,52, Serafina Valente53, Marco Mandalà54, Alessia Giorli54, Lorenzo Salerni54, Patrizia Zucchi55, Pierpaolo Parravicini55, Elisabetta Menatti56, Stefano Baratti57, Tullio Trotta58, Ferdinando Giannattasio58, Gabriella Coiro58, Fabio Lena59, Domenico A. Coviello60, Cristina Mussini61, Giancarlo Bosio62, Enrico Martinelli62, Sandro Mancarella63, Luisa Tavecchia63, Mary Ann Belli63, Lia Crotti64,65,66,67,68, Gianfranco Parati64,65, Nicola Picchiotti69,70, Marco Gori69,71, Maurizio Sanarico72, Stefano Ceri73, Pietro Pinoli73, Francesco Raimondi74, Filippo Biscarini75, Alessandra Stella75, Marco Rizzi76, Franco Maggiolo76, Diego Ripamonti76, Claudia Suardi77, Tiziana Bachetti78, Maria Teresa La Rovere79, Simona Sarzi-Braga80, Maurizio Bussotti81, Katia Capitani2,82, Simona Dei83, Sabrina Ravaglia84, Rosangela Artuso85, Antonio Perrella86, Francesco Bianchi2,86, Giuseppe Merla42,87, Gabriella Maria Squeo87. 9. Dept of Specialized and Internal Medicine, Tropical and Infectious Diseases Unit, Azienda Ospedaliera Universitaria Senese, Siena, Italy; 10. Unit of Respiratory Diseases and Lung Transplantation, Department of Internal and Specialist Medicine, University of Siena; 11. Dept of Emergency and Urgency, Medicine, Surgery and Neurosciences, Unit of Intensive Care Medicine, Siena University Hospital, Italy; 12. Department of Medical, Surgical and Neurosciences and Radiological Sciences, Unit of Diagnostic Imaging, University of Siena; 13. Rheumatology Unit, Department of Medicine, Surgery and Neurosciences, University of Siena, Policlinico Le Scotte, Italy; 14. Department of Specialized and Internal Medicine, Infectious Diseases Unit, San Donato Hospital Arezzo, Italy; 15. Dept of Emergency, Anesthesia Unit, San Donato Hospital, Arezzo, Italy; 16. Department of Specialized and Internal Medicine, Pneumology Unit and UTIP, San Donato Hospital, Arezzo, Italy; 17. Department of Emergency, Anesthesia Unit, Misericordia Hospital, Grosseto, Italy; 18. Department of Specialized and Internal Medicine, Infectious Diseases Unit, Misericordia Hospital, Grosseto, Italy; 19. Laboratory Medicine Department, Misericordia Hospital, Grosseto, Italy; 20. Department of Preventive Medicine, Azienda USL Toscana Sud Est, Italy; 21. Territorial Scientific Technician Department, Azienda USL Toscana Sud Est, Italy; 22. Laboratory Medicine Department, San Donato Hospital, Arezzo, Italy; 23. Chirurgia Vascolare, Ospedale Maggiore di Crema, Italy; 24. Department of Health Sciences, Clinic of Infectious Diseases, ASST Santi Paolo e Carlo, University of Milan, Italy; 25. Division of Infectious Diseases and Immunology, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; 26. Department of Internal Medicine and Therapeutics, University of Pavia, Italy; 27. Department of Anesthesia and Intensive Care, University of Modena and Reggio Emilia, Modena, Italy; 28. Department of Medical and Surgical Sciences for Children and Adults, University of Modena and Reggio Emilia, Modena, Italy; 29. HIV/AIDS Department, National Institute for Infectious Diseases, IRCCS, Lazzaro Spallanzani, Rome, Italy; 30. III Infectious Diseases Unit, ASST-FBF-Sacco, Milan, Italy; 31. Department of Biomedical and Clinical Sciences Luigi Sacco, University of Milan, Milan, Italy; 32. Infectious Diseases Clinic, Department of Medicine, Azienda Ospedaliera di Perugia and University of Perugia, Santa Maria Hospital, Perugia, Italy; 33. Infectious Diseases Clinic, “Santa Maria” Hospital, University of Perugia, Perugia, Italy; 34. Department of Infectious Diseases, Treviso Hospital, Local Health Unit 2 Marca Trevigiana, Treviso, Italy; 35. Clinical Infectious Diseases, Mestre Hospital, Venezia, Italy; 36. Infectious Diseases Clinic, ULSS1, Belluno, Italy; 37. Department of Molecular Medicine, University of Padova, Italy; 38. Department of Infectious and Tropical Diseases, University of Brescia and ASST Spedali Civili Hospital, Brescia, Italy; 39. Department of Molecular and Translational Medicine, University of Brescia, Italy; 40. Clinical Chemistry Laboratory, Cytogenetics and Molecular Genetics Section, Diagnostic Department, ASST Spedali Civili di Brescia, Italy; 41. Medical Genetics and Laboratory of Medical Genetics Unit, A.O.R.N. “Antonio Cardarelli”, Naples, Italy; 42. Department of Molecular Medicine and Medical Biotechnology, University of Naples Federico II, Naples, Italy; 43. CEINGE Biotecnologie Avanzate, Naples, Italy; 44. IRCCS SDN, Naples, Italy; 45. Unit of Respiratory Physiopathology, AORN dei Colli, Monaldi Hospital, Naples, Italy; 46. Division of Medical Genetics, Fondazione IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo, Italy; 47. Department of Medical Sciences, Fondazione IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo, Italy; 48. Clinical Trial Office, Fondazione IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo, Italy; 49. Department of Health Sciences, University of Genova, Genova, Italy; 50. Infectious Diseases Clinic, Policlinico San Martino Hospital, IRCCS for Cancer Research Genova, Italy; 51. Microbiology, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Catholic University of Medicine, Rome, Italy; 52. Department of Laboratory Sciences and Infectious Diseases, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy; 53. Department of Cardiovascular Diseases, University of Siena, Siena, Italy; 54. Otolaryngology Unit, University of Siena, Italy; 55. Department of Internal Medicine, ASST Valtellina e Alto Lario, Sondrio, Italy; 56. Study Coordinator Oncologia Medica e Ufficio Flussi, Sondrio, Italy; 57. Department of Infectious and Tropical Diseases, University of Padova, Padova, Italy; 58. First Aid Department, Luigi Curto Hospital, Polla, Salerno, Italy; 59. Local Health Unit-Pharmaceutical Department of Grosseto, Toscana Sud Est Local Health Unit, Grosseto, Italy; 60. U.O.C. Laboratorio di Genetica Umana, IRCCS Istituto G. Gaslini, Genova, Italy; 61. Infectious Diseases Clinics, University of Modena and Reggio Emilia, Modena, Italy; 62. Department of Respiratory Diseases, Azienda Ospedaliera di Cremona, Cremona, Italy; 63. U.O.C. Medicina, ASST Nord Milano, Ospedale Bassini, Cinisello Balsamo (MI), Italy; 64. Istituto Auxologico Italiano, IRCCS, Department of Cardiovascular, Neural and Metabolic Sciences, San Luca Hospital, Milan, Italy; 65. Department of Medicine and Surgery, University of Milano-Bicocca, Milan, Italy; 66. Istituto Auxologico Italiano, IRCCS, Center for Cardiac Arrhythmias of Genetic Origin, Milan, Italy; 67. Istituto Auxologico Italiano, IRCCS, Laboratory of Cardiovascular Genetics, Milan, Italy; 68. Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart-ERN GUARD-Heart; 69. University of Siena, DIISM-SAILAB, Siena, Italy; 70. Department of Mathematics, University of Pavia, Pavia, Italy; 71. University Cote d’Azur, Inria, CNRS, I3S, Maasai; 72. Independent Data Scientist, Milan, Italy; 73. Department of Electronics, Information and Bioengineering (DEIB), Politecnico di Milano, Milano, Italy; 74. Scuola Normale Superiore, Pisa, Italy; 75. CNR-Consiglio Nazionale delle Ricerche, Istituto di Biologia e Biotecnologia Agraria (IBBA), Milano, Italy; 76. Unit of Infectious Diseases, ASST Papa Giovanni XXIII Hospital, Bergamo, Italy; 77. Fondazione per la ricerca Ospedale di Bergamo, Bergamo, Italy; 78. Direzione Scientifica, Istituti Clinici Scientifici Maugeri IRCCS, Pavia, Italy; 79. Istituti Clinici Scientifici Maugeri IRCCS, Department of Cardiology, Institute of Montescano, Pavia, Italy; 80. Istituti Clinici Scientifici Maugeri, IRCCS, Department of Cardiac Rehabilitation, Institute of Tradate (VA), Italy; 81. Istituti Clinici Scientifici Maugeri IRCCS, Department of Cardiology, Institute of Milan, Milan, Italy; 82. Core Research Laboratory, ISPRO, Florence, Italy; 83. Health Management, Azienda USL Toscana Sudest, Tuscany, Italy; 84. IRCCS C. Mondino Foundation, Pavia, Italy; 85. Medical Genetics Unit, Meyer Children’s University Hospital, Florence, Italy; 86. Department of Medicine, Pneumology Unit, Misericordia Hospital, Grosseto, Italy; 87. Laboratory of Regulatory and Functional Genomics, Fondazione IRCCS Casa Sollievo della Sofferenza, San Giovanni Rotondo (Foggia), Italy.
References
- Lopes-Pacheco, M.; Silva, P.L.; Cruz, F.F.; Battaglini, D.; Robba, C.; Pelosi, P.; Morales, M.M.; Caruso Neves, C.; Rocco, P.R.M. Pathogenesis of Multiple Organ Injury in COVID-19 and Potential Therapeutic Strategies. Front. Physiol. 2021, 12, 1–23. [Google Scholar] [CrossRef]
- WHO Coronavirus Disease 2019 (COVID-19) Situation Report. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 12 June 2021).
- Oran, D.P.; Topol, E.J. Prevalence of Asymptomatic SARS-CoV-2 Infection. Ann. Intern. Med. 2020, M20-3012. [Google Scholar] [CrossRef]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19). JAMA 2020, 324, 782. [Google Scholar] [CrossRef] [PubMed]
- Mahmudpour, M.; Roozbeh, J.; Keshavarz, M.; Farrokhi, S.; Nabipour, I. COVID-19 cytokine storm: The anger of inflammation. Cytokine 2020, 133, 155151. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, S.; Liu, H.; Li, W.; Lin, F.; Jiang, L.; Li, X.; Xu, P.; Zhang, L.; Zhao, L.; et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J. Hepatol. 2020, 73, 807–816. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Wang, H.; Fan, J.; Zhang, Y.; Wang, H.; Zhao, Q. Pancreatic Injury Patterns in Patients With Coronavirus Disease 19 Pneumonia. Gastroenterology 2020, 159, 367–370. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (Lond. Engl.) 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef]
- Severe Covid-19 GWAS Group; Ellinghaus, D.; Degenhardt, F.; Bujanda, L.; Buti, M.; Albillos, A.; Invernizzi, P.; Fernández, J.; Prati, D.; Baselli, G.; et al. Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N. Engl. J. Med. 2020, 383, 1522–1534. [Google Scholar] [CrossRef]
- Vietzen, H.; Zoufaly, A.; Traugott, M.; Aberle, J.; Aberle, S.W.; Puchhammer-Stöckl, E. Deletion of the NKG2C receptor encoding KLRC2 gene and HLA-E variants are risk factors for severe COVID-19. Genet. Med. 2021, 1–5. [Google Scholar] [CrossRef]
- Zhang, Q.; Liu, Z.; Moncada-Velez, M.; Chen, J.; Ogishi, M.; Bigio, B.; Yang, R.; Arias, A.A.; Zhou, Q.; Han, J.E.; et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science 2020, 370. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Host Genetics Initiative. The COVID-19 Host Genetics Initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic. Eur. J. Hum. Genet. 2020, 28, 715–718. [Google Scholar] [CrossRef] [PubMed]
- Benetti, E.; Giliberti, A.; Emiliozzi, A.; Valentino, F.; Bergantini, L.; Fallerini, C.; Anedda, F.; Amitrano, S.; Conticini, E.; Tita, R.; et al. Clinical and molecular characterization of COVID-19 hospitalized patients. PLoS ONE 2020, 15, e0242534. [Google Scholar] [CrossRef]
- Benetti, E.; Tita, R.; Spiga, O.; Ciolfi, A.; Birolo, G.; Bruselles, A.; Doddato, G.; Giliberti, A.; Marconi, C.; Musacchia, F.; et al. ACE2 gene variants may underlie interindividual variability and susceptibility to COVID-19 in the Italian population. Eur. J. Hum. Genet. 2020, 28, 1602–1614. [Google Scholar] [CrossRef] [PubMed]
- Pairo-Castineira, E.; Clohisey, S.; Klaric, L.; Bretherick, A.D.; Rawlik, K.; Pasko, D.; Walker, S.; Parkinson, N.; Fourman, M.H.; Russell, C.D.; et al. Genetic mechanisms of critical illness in Covid-19. Nature 2020. [Google Scholar] [CrossRef]
- Daga, S.; Fallerini, C.; Baldassarri, M.; Fava, F.; Valentino, F.; Doddato, G.; Benetti, E.; Furini, S.; Giliberti, A.; Tita, R.; et al. Employing a systematic approach to biobanking and analyzing clinical and genetic data for advancing COVID-19 research. Eur. J. Hum. Genet. 2021. [Google Scholar] [CrossRef]
- Baldassarri, M.; Picchiotti, N.; Fava, F.; Fallerini, C.; Benetti, E.; Daga, S.; Valentino, F.; Doddato, G.; Furini, S.; Giliberti, A.; et al. Shorter androgen receptor polyQ alleles protect against life-threatening COVID-19 disease in European males. EBioMedicine 2021, 65. [Google Scholar] [CrossRef]
- Fallerini, C.; Daga, S.; Mantovani, S.; Benetti, E.; Picchiotti, N.; Francisci, D.; Paciosi, F.; Schiaroli, E.; Baldassarri, M.; Fava, F.; et al. Association of toll-like receptor 7 variants with life-threatening COVID-19 disease in males: Findings from a nested case-control study. Elife 2021, 10. [Google Scholar] [CrossRef]
- Elborn, J.S. Cystic fibrosis. Lancet 2016, 388, 2519–2531. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020. [Google Scholar] [CrossRef]
- Hamming, I.; Timens, W.; Bulthuis, M.L.C.; Lely, A.T.; Navis, G.J.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Roesch, E.A.; Nichols, D.P.; Chmiel, J.F. Inflammation in cystic fibrosis: An update. Pediatr. Pulmonol. 2018, 53, S30–S50. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.C.; Comellas, A.P.; Hornick, D.B.; Stoltz, D.A.; Cavanaugh, J.E.; Gerke, A.K.; Welsh, M.J.; Zabner, J.; Polgreen, P.M. Cystic fibrosis carriers are at increased risk for a wide range of cystic fibrosis-related conditions. Proc. Natl. Acad. Sci. USA 2020, 117, 1621–1627. [Google Scholar] [CrossRef] [PubMed]
- Polgreen, P.M.; Brown, G.D.; Hornick, D.B.; Ahmad, F.; London, B.; Stoltz, D.A.; Comellas, A.P. CFTR heterozygotes are at increased risk of respiratory infections: A population-based study. Open Forum Infect. Dis. 2018, 5, 1–7. [Google Scholar] [CrossRef]
- WHO R&D Blueprint novel Coronavirus COVID-19 Therapeutic Trial Synopsis. 2020. Available online: https://www.who.int/publications/i/item/covid-19-therapeutic-trial-synopsis (accessed on 23 May 2021).
- Freeman, G.H.; Halton, J.H. Note on an Exact Treatment of Contingency, Goodness of Fit and Other Problems of Significance. Biometrika 1951, 38, 141. [Google Scholar] [CrossRef] [PubMed]
- Groman, J.D.; Hefferon, T.W.; Casals, T.; Bassas, L.; Estivill, X.; Des Georges, M.; Guittard, C.; Koudova, M.; Fallin, M.D.; Nemeth, K.; et al. Variation in a Repeat Sequence Determines Whether a Common Variant of the Cystic Fibrosis Transmembrane Conductance Regulator Gene Is Pathogenic or Benign. Am. J. Hum. Genet. 2004, 74, 176–179. [Google Scholar] [CrossRef]
- Gabriel, S.E.; Brigman, K.N.; Koller, B.H.; Boucher, R.C.; Stutts, M.J. Cystic fibrosis heterozygote resistance to cholera toxin in the cystic fibrosis mouse model. Science 1994, 266, 107–109. [Google Scholar] [CrossRef] [PubMed]
- Trapnell, B.C.; Chu, C.S.; Paakko, P.K.; Banks, T.C.; Yoshimura, K.; Ferrans, V.J.; Chernick, M.S.; Crystal, R.G. Expression of the cystic fibrosis transmembrane conductance regulator gene in the respiratory tract of normal individuals and individuals with cystic fibrosis. Proc. Natl. Acad. Sci. USA. 1991, 88, 6565–6569. [Google Scholar] [CrossRef]
- Cohn, J.A.; Friedman, K.J.; Noone, P.G.; Knowles, M.R.; Silverman, L.M.; Jowell, P.S. Relation between Mutations of the Cystic Fibrosis Gene and Idiopathic Pancreatitis. N. Engl. J. Med. 1998, 339, 653–658. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020, 11. [Google Scholar] [CrossRef]
- Jin, J.M.; Bai, P.; He, W.; Wu, F.; Liu, X.F.; Han, D.M.; Liu, S.; Yang, J.K. Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Front. Public Health 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Saksena, S.; Sadri-Ardekani, H. ACE2 receptor expression in testes: Implications in coronavirus disease 2019 pathogenesis. Biol. Reprod. 2020, 103, 449–451. [Google Scholar] [CrossRef]
- Tay, M.Z.; Poh, C.M.; Rénia, L.; MacAry, P.A.; Ng, L.F.P. The trinity of COVID-19: Immunity, inflammation and intervention. Nat. Rev. Immunol. 2020, 20, 363–374. [Google Scholar] [CrossRef]
- Kuba, K.; Imai, Y.; Rao, S.; Gao, H.; Guo, F.; Guan, B.; Huan, Y.; Yang, P.; Zhang, Y.; Deng, W.; et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 2005, 11, 875–879. [Google Scholar] [CrossRef] [PubMed]
- McNabb-Baltar, J.; Jin, D.X.; Grover, A.S.; Redd, W.D.; Zhou, J.C.; Hathorn, K.E.; McCarty, T.R.; Bazarbashi, A.N.; Shen, L.; Chan, W.W. Lipase Elevation in Patients With COVID-19. Am. J. Gastroenterol. 2020, 115, 1286–1288. [Google Scholar] [CrossRef] [PubMed]
- Sarantis, P.; Koustas, E.; Papavassiliou, A.G.; Karamouzis, M.V. Are cystic fibrosis mutation carriers a potentially highly vulnerable group to COVID-19? J. Cell. Mol. Med. 2020, 24, 13542–13545. [Google Scholar] [CrossRef]
- Shah, V.S.; Ernst, S.; Tang, X.X.; Karp, P.H.; Parker, C.P.; Ostedgaard, L.S.; Welsh, M.J. Relationships among CFTR expression, HCO3- secretion, and host defense may inform gene- and cell-based cystic fibrosis therapies. Proc. Natl. Acad. Sci. USA 2016, 113, 5382–5387. [Google Scholar] [CrossRef]
- Bezzerri, V.; Lucca, F.; Volpi, S.; Cipolli, M. Does cystic fibrosis constitute an advantage in COVID-19 infection? Ital. J. Pediatr. 2020, 46, 1–3. [Google Scholar] [CrossRef]
- Colombo, C.; Burgel, P.-R.; Gartner, S.; van Koningsbruggen-Rietschel, S.; Naehrlich, L.; Sermet-Gaudelus, I.; Southern, K.W. Impact of COVID-19 on people with cystic fibrosis. Lancet. Respir. Med. 2020, 8, e35–e36. [Google Scholar] [CrossRef]
- Cosgriff, R.; Ahern, S.; Bell, S.C.; Brownlee, K.; Burgel, P.-R.; Byrnes, C.; Corvol, H.; Cheng, S.Y.; Elbert, A.; Faro, A.; et al. A multinational report to characterise SARS-CoV-2 infection in people with cystic fibrosis. J. Cyst. Fibros. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.H.; Shaw, D.M.; Petty, L.E.; Graff, M.; Bohlender, R.J.; Polikowsky, H.G.; Zhong, X.; Kim, D.; Buchanan, V.L.; Preuss, M.H.; et al. Host genetic effects in pneumonia. Am. J. Hum. Genet. 2020, 1–8. [Google Scholar] [CrossRef]
- Chen, R.; Liang, W.; Jiang, M.; Guan, W.; Zhan, C.; Wang, T.; Tang, C.; Sang, L.; Liu, J.; Ni, Z.; et al. Risk Factors of Fatal Outcome in Hospitalized Subjects With Coronavirus Disease 2019 From a Nationwide Analysis in China. Chest 2020, 158, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Price-Haywood, E.G.; Burton, J.; Fort, D.; Seoane, L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. N. Engl. J. Med. 2020, 382, 2534–2543. [Google Scholar] [CrossRef] [PubMed]
- Castellani, C.; Massie, J.; Sontag, M.; Southern, K.W. Newborn screening for cystic fibrosis. Lancet Respir. Med. 2016, 4, 653–661. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).