Downregulation of ATM and BRCA1 Predicts Poor Outcome in Head and Neck Cancer: Implications for ATM-Targeted Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture and Chemicals
2.2. RNA Purification, Reverse Transcription, and Real-Time Quantitative PCR (RT-qPCR)
2.3. Chromatin Immunoprecipitation and qPCR (ChIP-qPCR) Assay
2.4. Construction of the ATM Promoter-Luciferase Reporter and Dual Luciferase Assay
2.5. Analysis of ATM and BRCA1 mRNA Expression in BQ-associated HNC Specimens
2.6. Analysis of ATM and BRCA1 mRNA Expression in the Cancer Genome Atlas (TCGA)
2.7. Transcriptome and Gene Set Enrichment Analysis (GSEA)
2.8. Western Blot Analysis
2.9. Cell Viability and Caspase 3/7 Activity Assays
2.10. Statistical Analysis
3. Results
3.1. Areca Nut Extract (ANE) and Arecoline Inhibit the Expression of ATM and BRCA1
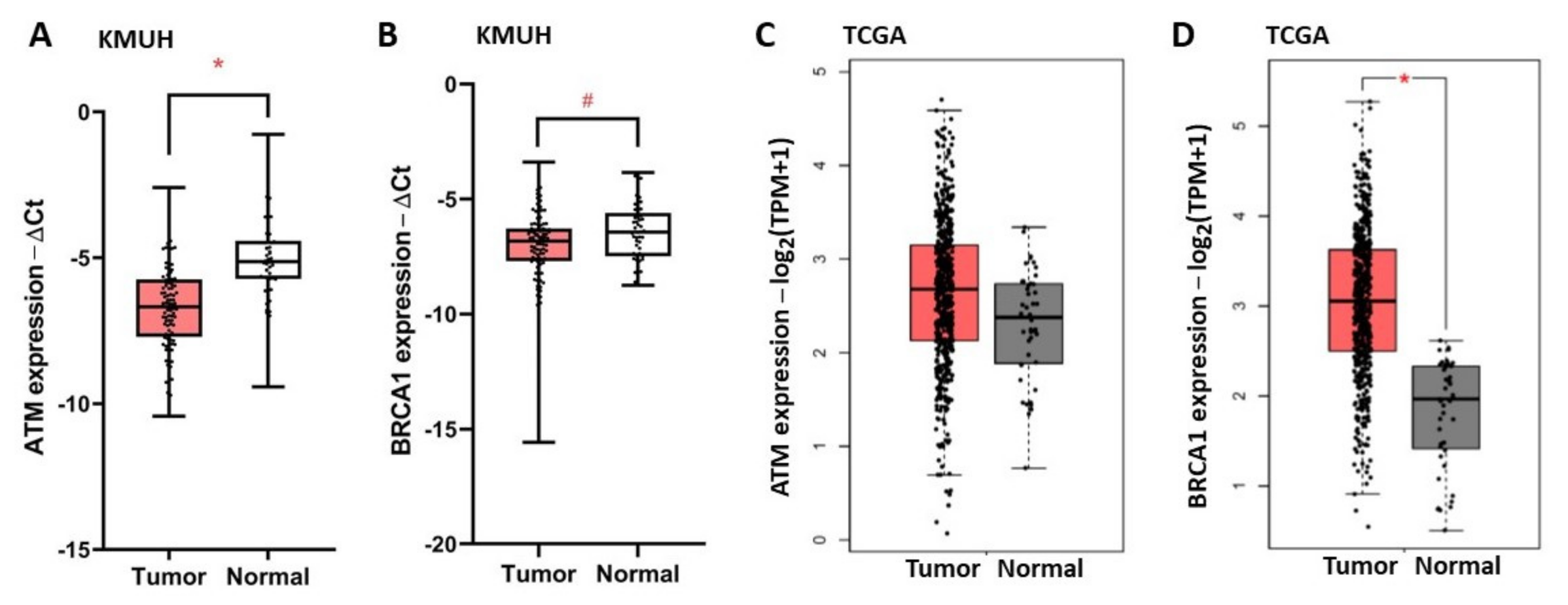
3.2. ATM and BRCA1 Are Downregulated in HNC and Are Correlated with Poor Patient Outcome
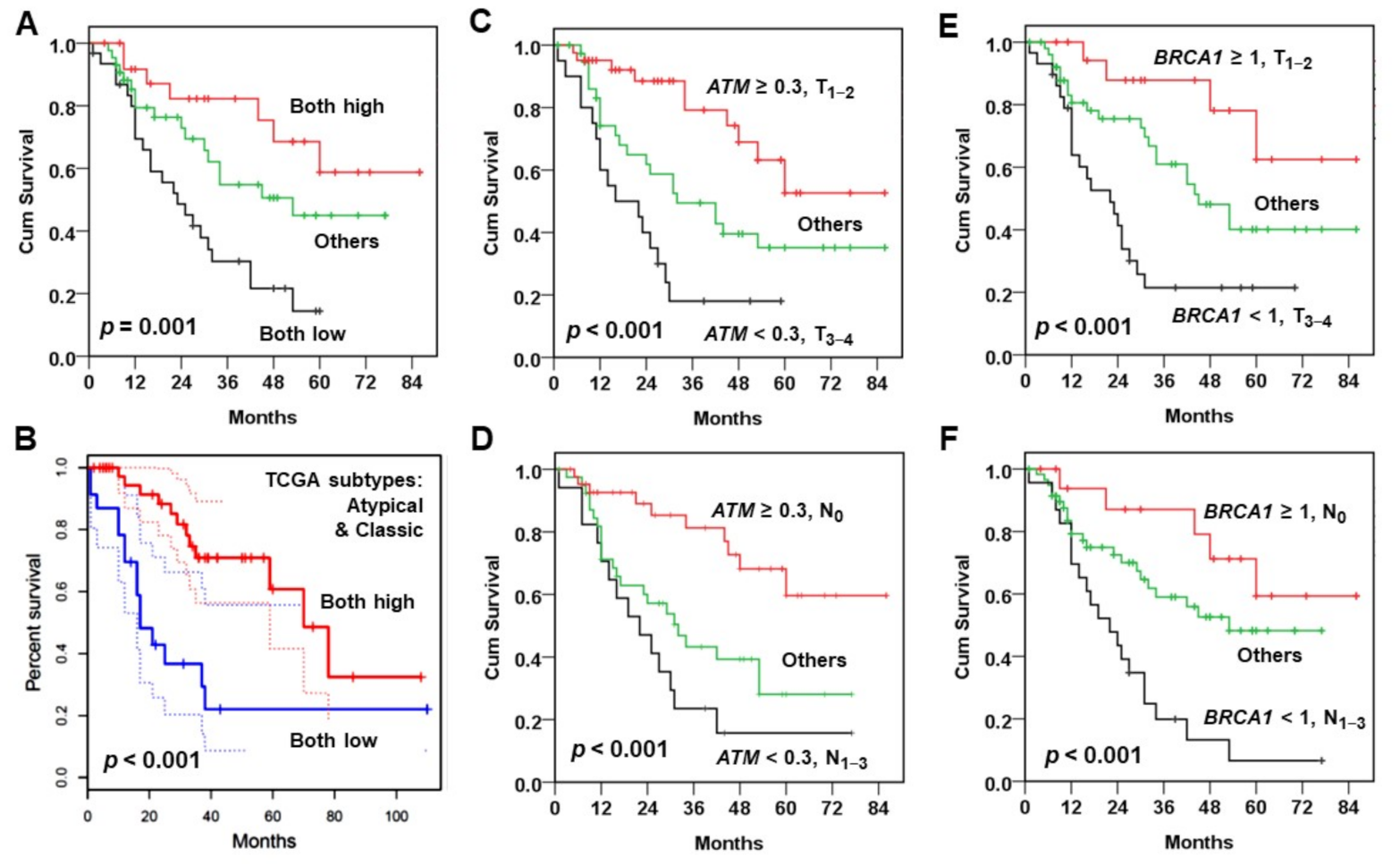
3.3. Combination of Two Prognosis Factors Improves Outcome Prediction
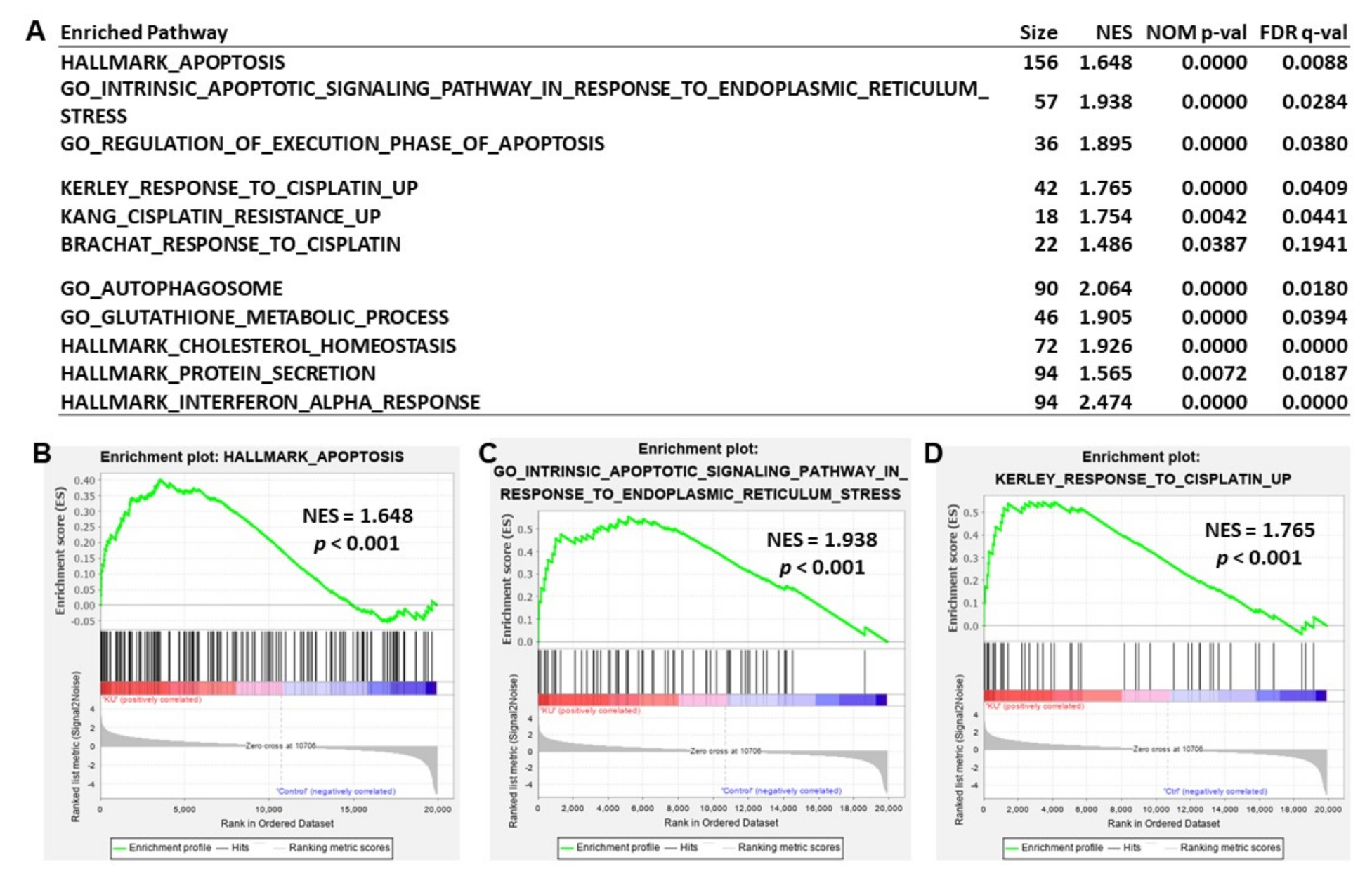
3.4. Inhibition of ATM Kinase Induces Apoptosis in Cancer Cells
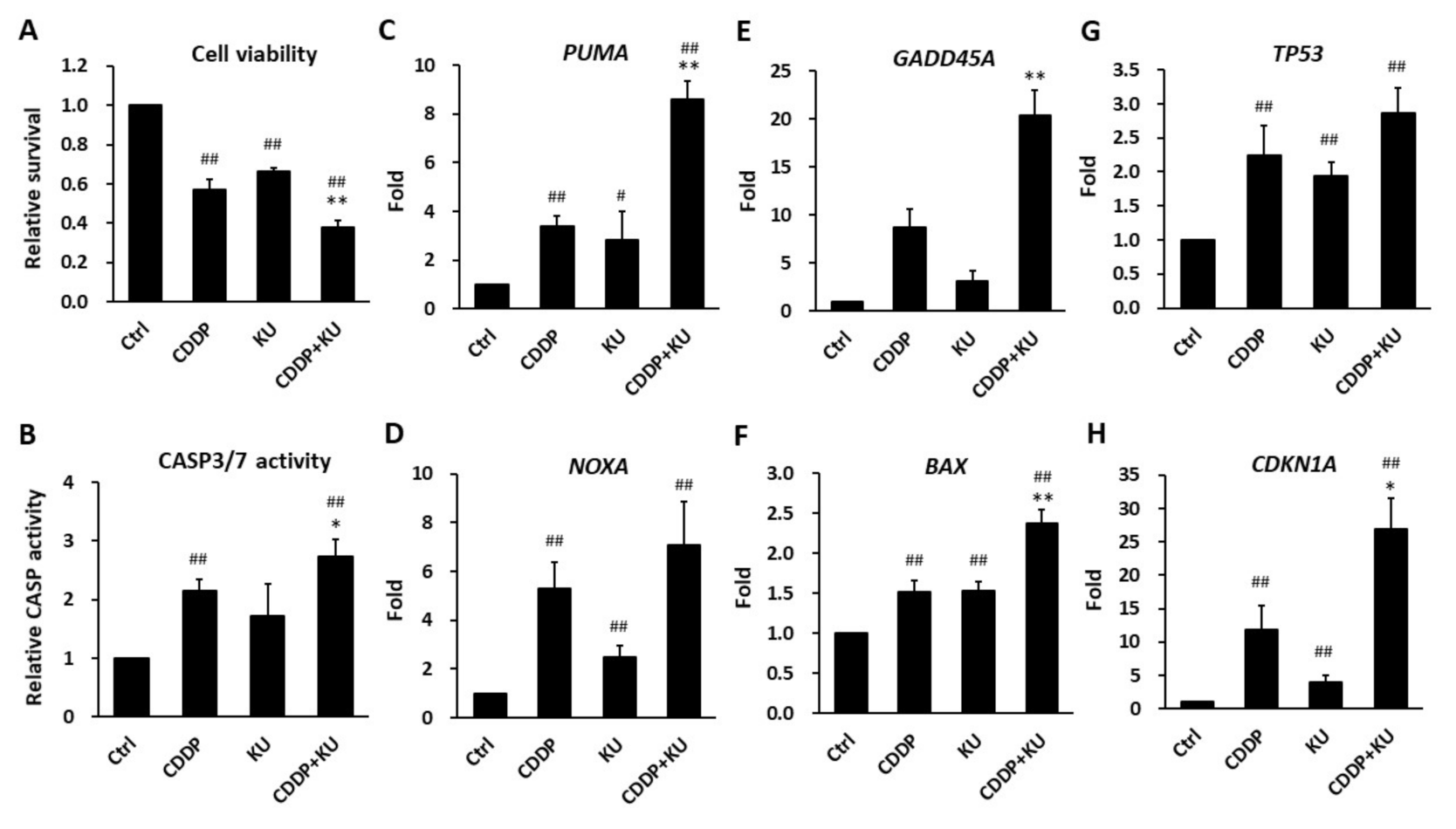
3.5. Inhibition of ATM Kinase Potentiates Cisplatin-Induced Cytotoxicity in Cancer Cells
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bartkova, J.; Horejsi, Z.; Koed, K.; Kramer, A.; Tort, F.; Zieger, K.; Guldberg, P.; Sehested, M.; Nesland, J.M.; Lukas, C.; et al. DNA damage response as a candidate anti-cancer barrier in early human tumorigenesis. Nature 2005, 434, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Gorgoulis, V.G.; Vassiliou, L.V.; Karakaidos, P.; Zacharatos, P.; Kotsinas, A.; Liloglou, T.; Venere, M.; Ditullio, R.A., Jr.; Kastrinakis, N.G.; Levy, B.; et al. Activation of the DNA damage checkpoint and genomic instability in human precancerous lesions. Nature 2005, 434, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Sancar, A.; Lindsey-Boltz, L.A.; Unsal-Kacmaz, K.; Linn, S. Molecular mechanisms of mammalian DNA repair and the DNA damage checkpoints. Annu. Rev. Biochem. 2004, 73, 39–85. [Google Scholar] [CrossRef] [PubMed]
- Deng, C.X. BRCA1: Cell cycle checkpoint, genetic instability, DNA damage response and cancer evolution. Nucleic Acids Res. 2006, 34, 1416–1426. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K.; Miki, Y. Role of BRCA1 and BRCA2 as regulators of DNA repair, transcription, and cell cycle in response to DNA damage. Cancer Sci. 2004, 95, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Deng, C.X. Roles of BRCA1 in centrosome duplication. Oncogene 2002, 21, 6222–6227. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vora, H.H.; Shah, N.G.; Patel, D.D.; Trivedi, T.I.; Choksi, T.J. BRCA1 expression in leukoplakia and carcinoma of the tongue. J. Surg. Oncol. 2003, 83, 232–240. [Google Scholar] [CrossRef]
- Lee, K.W.; Tsai, Y.S.; Chiang, F.Y.; Huang, J.L.; Ho, K.Y.; Yang, Y.H.; Kuo, W.R.; Chen, M.K.; Lin, C.S. Lower ataxia telangiectasia mutated (ATM) mRNA expression is correlated with poor outcome of laryngeal and pharyngeal cancer patients. Ann. Oncol. 2011, 22, 1088–1093. [Google Scholar] [CrossRef]
- Bose, S.; Yap, L.F.; Fung, M.; Starzcynski, J.; Saleh, A.; Morgan, S.; Dawson, C.; Chukwuma, M.B.; Maina, E.; Buettner, M.; et al. The ATM tumour suppressor gene is down-regulated in EBV-associated nasopharyngeal carcinoma. J. Pathol. 2009, 217, 345–352. [Google Scholar] [CrossRef]
- Grabsch, H.; Dattani, M.; Barker, L.; Maughan, N.; Maude, K.; Hansen, O.; Gabbert, H.E.; Quirke, P.; Mueller, W. Expression of DNA double-strand break repair proteins ATM and BRCA1 predicts survival in colorectal cancer. Clin. Cancer Res. 2006, 12, 1494–1500. [Google Scholar] [CrossRef]
- He, Y.; Chen, Q.; Li, B. ATM in oral carcinogenesis: Association with clinicopathological features. J. Cancer Res. Clin. Oncol. 2008, 134, 1013–1020. [Google Scholar] [CrossRef]
- Parikh, R.A.; White, J.S.; Huang, X.; Schoppy, D.W.; Baysal, B.E.; Baskaran, R.; Bakkenist, C.J.; Saunders, W.S.; Hsu, L.C.; Romkes, M.; et al. Loss of distal 11q is associated with DNA repair deficiency and reduced sensitivity to ionizing radiation in head and neck squamous cell carcinoma. Genes Chromosomes Cancer 2007, 46, 761–775. [Google Scholar] [CrossRef]
- Bouwman, P.; Jonkers, J. The effects of deregulated DNA damage signalling on cancer chemotherapy response and resistance. Nat. Rev. Cancer 2012, 12, 587–598. [Google Scholar] [CrossRef]
- Pearl, L.H.; Schierz, A.C.; Ward, S.E.; Al-Lazikani, B.; Pearl, F.M. Therapeutic opportunities within the DNA damage response. Nat. Rev. Cancer 2015, 15, 166–180. [Google Scholar] [CrossRef]
- Husain, A.; He, G.; Venkatraman, E.S.; Spriggs, D.R. BRCA1 up-regulation is associated with repair-mediated resistance to cis-diamminedichloroplatinum(II). Cancer Res. 1998, 58, 1120–1123. [Google Scholar]
- Lafarge, S.; Sylvain, V.; Ferrara, M.; Bignon, Y.J. Inhibition of BRCA1 leads to increased chemoresistance to microtubule-interfering agents, an effect that involves the JNK pathway. Oncogene 2001, 20, 6597–6606. [Google Scholar] [CrossRef]
- Rakha, E.A.; El-Sheikh, S.E.; Kandil, M.A.; El-Sayed, M.E.; Green, A.R.; Ellis, I.O. Expression of BRCA1 protein in breast cancer and its prognostic significance. Hum. Pathol. 2008, 39, 857–865. [Google Scholar] [CrossRef]
- Quinn, J.E.; James, C.R.; Stewart, G.E.; Mulligan, J.M.; White, P.; Chang, G.K.; Mullan, P.B.; Johnston, P.G.; Wilson, R.H.; Harkin, D.P. BRCA1 mRNA expression levels predict for overall survival in ovarian cancer after chemotherapy. Clin. Cancer Res. 2007, 13, 7413–7420. [Google Scholar] [CrossRef]
- Rosell, R.; Skrzypski, M.; Jassem, E.; Taron, M.; Bartolucci, R.; Sanchez, J.J.; Mendez, P.; Chaib, I.; Perez-Roca, L.; Szymanowska, A.; et al. BRCA1: A novel prognostic factor in resected non-small-cell lung cancer. PLoS ONE 2007, 2, e1129. [Google Scholar] [CrossRef]
- McKinnon, P.J. ATM and ataxia telangiectasia. EMBO Rep. 2004, 5, 772–776. [Google Scholar] [CrossRef]
- Jha, J.; Singh, M.K.; Singh, L.; Pushker, N.; Bajaj, M.S.; Sen, S.; Kashyap, S. Prognostic relevance of ATM protein in uveal melanoma and its association with clinicopathological factors. Int. J. Clin. Oncol. 2019, 24, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- Savva, C.; De Souza, K.; Ali, R.; Rakha, E.A.; Green, A.R.; Madhusudan, S. Clinicopathological significance of ataxia telangiectasia-mutated (ATM) kinase and ataxia telangiectasia-mutated and Rad3-related (ATR) kinase in MYC overexpressed breast cancers. Breast Cancer Res. Treat. 2019, 175, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Im, S.A.; Kim, M.A.; Cho, H.J.; Lee, D.W.; Lee, K.H.; Kim, T.Y.; Han, S.W.; Oh, D.Y.; Lee, H.J.; et al. Ataxia-telangiectasia-mutated protein expression with microsatellite instability in gastric cancer as prognostic marker. Int. J. Cancer 2014, 134, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Parameswaran, S.; Kundapur, D.; Vizeacoumar, F.S.; Freywald, A.; Uppalapati, M.; Vizeacoumar, F.J. A Road Map to Personalizing Targeted Cancer Therapies Using Synthetic Lethality. Trends Cancer 2019, 5, 11–29. [Google Scholar] [CrossRef]
- Lloyd, R.L.; Wijnhoven, P.W.G.; Ramos-Montoya, A.; Wilson, Z.; Illuzzi, G.; Falenta, K.; Jones, G.N.; James, N.; Chabbert, C.D.; Stott, J.; et al. Combined PARP and ATR inhibition potentiates genome instability and cell death in ATM-deficient cancer cells. Oncogene 2020, 39, 4869–4883. [Google Scholar] [CrossRef]
- Mateo, J.; Carreira, S.; Sandhu, S.; Miranda, S.; Mossop, H.; Perez-Lopez, R.; Nava Rodrigues, D.; Robinson, D.; Omlin, A.; Tunariu, N.; et al. DNA-Repair Defects and Olaparib in Metastatic Prostate Cancer. N. Engl. J. Med. 2015, 373, 1697–1708. [Google Scholar] [CrossRef]
- Karam, S.D.; Reddy, K.; Blatchford, P.J.; Waxweiler, T.; DeLouize, A.M.; Oweida, A.; Somerset, H.; Marshall, C.; Young, C.; Davies, K.D.; et al. Final Report of a Phase I Trial of Olaparib with Cetuximab and Radiation for Heavy Smoker Patients with Locally Advanced Head and Neck Cancer. Clin. Cancer Res. 2018, 24, 4949–4959. [Google Scholar] [CrossRef]
- Jette, N.R.; Kumar, M.; Radhamani, S.; Arthur, G.; Goutam, S.; Yip, S.; Kolinsky, M.; Williams, G.J.; Bose, P.; Lees-Miller, S.P. ATM-Deficient Cancers Provide New Opportunities for Precision Oncology. Cancers 2020, 12, 687. [Google Scholar] [CrossRef]
- Hickson, I.; Zhao, Y.; Richardson, C.J.; Green, S.J.; Martin, N.M.; Orr, A.I.; Reaper, P.M.; Jackson, S.P.; Curtin, N.J.; Smith, G.C. Identification and characterization of a novel and specific inhibitor of the ataxia-telangiectasia mutated kinase ATM. Cancer Res. 2004, 64, 9152–9159. [Google Scholar] [CrossRef]
- Riches, L.C.; Trinidad, A.G.; Hughes, G.; Jones, G.N.; Hughes, A.M.; Thomason, A.G.; Gavine, P.; Cui, A.; Ling, S.; Stott, J.; et al. Pharmacology of the ATM Inhibitor AZD0156: Potentiation of Irradiation and Olaparib Responses Preclinically. Mol. Cancer Ther. 2020, 19, 13–25. [Google Scholar] [CrossRef]
- Chow, L.Q.M. Head and Neck Cancer. N. Engl. J. Med. 2020, 382, 60–72. [Google Scholar] [CrossRef]
- Tu, H.F.; Chen, M.Y.; Lai, J.C.; Chen, Y.L.; Wong, Y.W.; Yang, C.C.; Chen, H.Y.; Hsia, S.M.; Shih, Y.H.; Shieh, T.M. Arecoline-regulated ataxia telangiectasia mutated expression level in oral cancer progression. Head Neck 2019, 41, 2525–2537. [Google Scholar] [CrossRef]
- Chiang, S.L.; Jiang, S.S.; Wang, Y.J.; Chiang, H.C.; Chen, P.H.; Tu, H.P.; Ho, K.Y.; Tsai, Y.S.; Chang, I.S.; Ko, Y.C. Characterization of arecoline-induced effects on cytotoxicity in normal human gingival fibroblasts by global gene expression profiling. Toxicol. Sci. 2007, 100, 66–74. [Google Scholar] [CrossRef]
- Lee, K.W.; Kuo, W.R.; Tsai, S.M.; Wu, D.C.; Wang, W.M.; Fang, F.M.; Chiang, F.Y.; Ho, K.Y.; Wang, L.F.; Tai, C.F.; et al. Different impact from betel quid, alcohol and cigarette: Risk factors for pharyngeal and laryngeal cancer. Int. J. Cancer 2005, 117, 831–836. [Google Scholar] [CrossRef]
- Ko, Y.C.; Huang, Y.L.; Lee, C.H.; Chen, M.J.; Lin, L.M.; Tsai, C.C. Betel quid chewing, cigarette smoking and alcohol consumption related to oral cancer in Taiwan. J. Oral Pathol. Med. 1995, 24, 450–453. [Google Scholar] [CrossRef]
- Tsai, Y.S.; Lee, K.W.; Huang, J.L.; Liu, Y.S.; Juo, S.H.; Kuo, W.R.; Chang, J.G.; Lin, C.S.; Jong, Y.J. Arecoline, a major alkaloid of areca nut, inhibits p53, represses DNA repair, and triggers DNA damage response in human epithelial cells. Toxicology 2008, 249, 230–237. [Google Scholar] [CrossRef]
- Wang, Y.C.; Tsai, Y.S.; Huang, J.L.; Lee, K.W.; Kuo, C.C.; Wang, C.S.; Huang, A.M.; Chang, J.Y.; Jong, Y.J.; Lin, C.S. Arecoline arrests cells at prometaphase by deregulating mitotic spindle assembly and spindle assembly checkpoint: Implication for carcinogenesis. Oral Oncol. 2010, 46, 255–262. [Google Scholar] [CrossRef]
- Tsai, Y.S.; Lin, C.S.; Chiang, S.L.; Lee, C.H.; Lee, K.W.; Ko, Y.C. Areca nut induces miR-23a and inhibits repair of DNA double-strand breaks by targeting FANCG. Toxicol. Sci. 2011, 123, 480–490. [Google Scholar] [CrossRef]
- Wang, Y.C.; Huang, J.L.; Lee, K.W.; Lu, H.H.; Lin, Y.J.; Chen, L.F.; Wang, C.S.; Cheng, Y.C.; Zeng, Z.T.; Chu, P.Y.; et al. Downregulation of the DNA Repair Gene DDB2 by Arecoline Is through p53’s DNA-Binding Domain and Is Correlated with Poor Outcome of Head and Neck Cancer Patients with Betel Quid Consumption. Cancers 2020, 12, 2053. [Google Scholar] [CrossRef]
- Lin, C.S.; Wang, Y.C.; Huang, J.L.; Hung, C.C.; Chen, J.Y. Autophagy and reactive oxygen species modulate cytotoxicity induced by suppression of ATM kinase activity in head and neck cancer cells. Oral Oncol. 2012, 48, 1152–1158. [Google Scholar] [CrossRef]
- Nair, J.; Ohshima, H.; Friesen, M.; Croisy, A.; Bhide, S.V.; Bartsch, H. Tobacco-specific and betel nut-specific N-nitroso compounds: Occurrence in saliva and urine of betel quid chewers and formation in vitro by nitrosation of betel quid. Carcinogenesis 1985, 6, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Kang, B.; Li, C.; Chen, T.; Zhang, Z. GEPIA2: An enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 2019, 47, W556–W560. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, A.; Tamayo, P.; Mootha, V.K.; Mukherjee, S.; Ebert, B.L.; Gillette, M.A.; Paulovich, A.; Pomeroy, S.L.; Golub, T.R.; Lander, E.S.; et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. USA 2005, 102, 15545–15550. [Google Scholar] [CrossRef] [PubMed]
- Nagy, A.; Lanczky, A.; Menyhart, O.; Gyorffy, B. Validation of miRNA prognostic power in hepatocellular carcinoma using expression data of independent datasets. Sci. Rep. 2018, 8, 9227. [Google Scholar] [CrossRef]
- Pant, I.; Kumar, N.; Khan, I.; Rao, S.G.; Kondaiah, P. Role of areca nut induced TGF-β and epithelial-mesenchymal interaction in the pathogenesis of oral submucous fibrosis. PLoS ONE 2015, 10, e0129252. [Google Scholar] [CrossRef]
- Networks, T.C.G.A. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015, 517, 576–582. [Google Scholar]
- Ai, L.; Vo, Q.N.; Zuo, C.; Li, L.; Ling, W.; Suen, J.Y.; Hanna, E.; Brown, K.D.; Fan, C.Y. Ataxia-telangiectasia-mutated (ATM) gene in head and neck squamous cell carcinoma: Promoter hypermethylation with clinical correlation in 100 cases. Cancer Epidemiol. Biomark. Prev. 2004, 13, 150–156. [Google Scholar] [CrossRef][Green Version]
- Bolt, J.; Vo, Q.N.; Kim, W.J.; McWhorter, A.J.; Thomson, J.; Hagensee, M.E.; Friedlander, P.; Brown, K.D.; Gilbert, J. The ATM/p53 pathway is commonly targeted for inactivation in squamous cell carcinoma of the head and neck (SCCHN) by multiple molecular mechanisms. Oral Oncol. 2005, 41, 1013–1020. [Google Scholar] [CrossRef]
- van den Broek, G.B.; Wreesmann, V.B.; van den Brekel, M.W.; Rasch, C.R.; Balm, A.J.; Rao, P.H. Genetic abnormalities associated with chemoradiation resistance of head and neck squamous cell carcinoma. Clin. Cancer Res. 2007, 13, 4386–4391. [Google Scholar] [CrossRef]
- Choudhury, Y.; Sharan, R.N. Altered BRCA1 and BRCA2 responses and mutation of BRCA1 gene in mice exposed chronically and transgenerationally to aqueous extract of betel nut (AEBN). Environ. Toxicol. Pharmacol. 2011, 31, 57–69. [Google Scholar] [CrossRef]
- Rizos, E.; Sourvinos, G.; Spandidos, D.A. Loss of heterozygosity at 8p, 9p and 17q in laryngeal cytological specimens. Oral Oncol. 1998, 34, 519–523. [Google Scholar] [CrossRef]
- Ivanov, V.N.; Zhou, H.; Partridge, M.A.; Hei, T.K. Inhibition of ataxia telangiectasia mutated kinase activity enhances TRAIL-mediated apoptosis in human melanoma cells. Cancer Res. 2009, 69, 3510–3519. [Google Scholar] [CrossRef]
- Li, Y.; Yang, D.Q. The ATM inhibitor KU-55933 suppresses cell proliferation and induces apoptosis by blocking Akt in cancer cells with overactivated Akt. Mol. Cancer Ther. 2010, 9, 113–125. [Google Scholar] [CrossRef]
- Fujimaki, S.; Matsuda, Y.; Wakai, T.; Sanpei, A.; Kubota, M.; Takamura, M.; Yamagiwa, S.; Yano, M.; Ohkoshi, S.; Aoyagi, Y. Blockade of ataxia telangiectasia mutated sensitizes hepatoma cell lines to sorafenib by interfering with Akt signaling. Cancer Lett. 2012, 319, 98–108. [Google Scholar] [CrossRef]
- Degorce, S.L.; Barlaam, B.; Cadogan, E.; Dishington, A.; Ducray, R.; Glossop, S.C.; Hassall, L.A.; Lach, F.; Lau, A.; McGuire, T.M.; et al. Discovery of Novel 3-Quinoline Carboxamides as Potent, Selective, and Orally Bioavailable Inhibitors of Ataxia Telangiectasia Mutated (ATM) Kinase. J. Med. Chem. 2016, 59, 6281–6292. [Google Scholar] [CrossRef]
- Karlin, J.; Allen, J.; Ahmad, S.F.; Hughes, G.; Sheridan, V.; Odedra, R.; Farrington, P.; Cadogan, E.B.; Riches, L.C.; Garcia-Trinidad, A.; et al. Orally Bioavailable and Blood-Brain Barrier-Penetrating ATM Inhibitor (AZ32) Radiosensitizes Intracranial Gliomas in Mice. Mol. Cancer Ther. 2018, 17, 1637–1647. [Google Scholar] [CrossRef]
- Zhang, Y.; Fan, S.; Meng, Q.; Ma, Y.; Katiyar, P.; Schlegel, R.; Rosen, E.M. BRCA1 interaction with human papillomavirus oncoproteins. J. Biol. Chem. 2005, 280, 33165–33177. [Google Scholar] [CrossRef]
- Tryfonidis, K.; Papadaki, C.; Assele, S.; Lagoudaki, E.; Menis, J.; Koutsopoulos, A.; Trypaki, M.; Tsakalaki, E.; Sfakianaki, M.; Hasan, B.; et al. Association of BRCA1, ERCC1, RAP80, PKM2, RRM1, RRM2, TS, TSP1, and TXR1 mRNA expression levels between primary tumors and infiltrated regional lymph nodes in patients with resectable non-small cell lung cancer. Pharm. J. 2019, 19, 15–24. [Google Scholar] [CrossRef]
- Akagi, I.; Okayama, H.; Schetter, A.J.; Robles, A.I.; Kohno, T.; Bowman, E.D.; Kazandjian, D.; Welsh, J.A.; Oue, N.; Saito, M.; et al. Combination of protein coding and noncoding gene expression as a robust prognostic classifier in stage I lung adenocarcinoma. Cancer Res. 2013, 73, 3821–3832. [Google Scholar] [CrossRef]


| Gene | Forward Primer (5′ to 3′) | Reverse Primer (5′ to 3′) |
|---|---|---|
| ATM | ATAGATTGTGTAGGTTCCGATGG | CATCTTGTCTCAGGTCATCACG |
| BRCA1 | TTGTTGATGTGGAGGAGCAA | GATTCCAGGTAAGGGGTTCC |
| PUMA | GACCTCAACGCACAGTACGA | GAGATTGTACAGGACCCTCCA |
| NOXA | GGAGATGCCTGGGAAGAAG | CCTGAGTTGAGTAGCACACTCG |
| BAX | AGCAAACTGGTGCTCAAGG | TCTTGGATCCAGCCCAAC |
| GADD45A | TTTGCAATATGACTTTGGAGGA | CATCCCCCACCTTATCCAT |
| TP53 | AGGCCTTGGAACTCAAGGAT | CCCTTTTTGGACTTCAGGTG |
| CDKN1A | TCACTGTCTTGTACCCTTGTGC | GGCGTTTGGAGTGGTAGAAA |
| GAPDH | AGCCACATCGCTCAGACAC | GCCCAATACGACCAAATCC |
| Variables | ATM mRNA a | pb | BRCA1 mRNA a | pb | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| <0.3 (%) | >0.3 (%) | <1 (%) | >1 (%) | ||||||||
| Gender | Male | 34 | (36.2) | 60 | (63.8) | 0.667 c | 65 | (69.1 | 29 | (30.9) | 0.381 c |
| Female | 3 | (50.0) | 3 | (50.0) | 3 | (50.0) | 3 | (50.0) | |||
| Age | <55 | 15 | (34.9) | 28 | (65.1) | 0.703 | 30 | (69.8) | 13 | (30.2) | 0.742 |
| >55 | 22 | (38.6) | 35 | (61.4) | 38 | (66.7) | 19 | (33.3) | |||
| T | 1–2 | 17 | (29.3) | 41 | (70.7) | 0.061 | 39 | (67.2) | 19 | (32.8) | 0.848 |
| 3–4 | 20 | (47.6) | 22 | (52.4) | 29 | (69.0) | 13 | (31.0) | |||
| N | 0 | 20 | (31.7) | 43 | (68.3) | 0.156 | 45 | (71.4) | 18 | (28.6) | 0.338 |
| 1–3 | 17 | (45.9) | 20 | (54.1) | 23 | (62.2) | 14 | (37.8) | |||
| Survival | No | 26 | (55.3) | 21 | (44.7) | <0.001 | 37 | (78.7) | 10 | (21.3) | 0.030 |
| Yes | 11 | (20.8) | 42 | (79.2) | 31 | (58.5) | 22 | (41.5) | |||
| Variables | 3-yr (%) | 5-yr (%) | pa | |
|---|---|---|---|---|
| Overall | 53.1 | 37.4 | ||
| Gender | Male | 53.0 | 36.7 | 0.657 |
| Female | 53.3 | - | ||
| Age | <55 | 38.9 | 18.5 | 0.037 |
| >55 | 61.1 | 46.5 | ||
| T | 1–2 | 31.9 | 28.3 | 0.002 |
| 3–4 | 70.5 | 44.2 | ||
| N | 0 | 33.2 | 22.8 | 0.004 |
| 1–3 | 67.5 | 47.7 | ||
| ATM b | <0.3 | 33.7 | 20.2 | 0.001 |
| >0.3 | 67.2 | 49.5 | ||
| BRCA1 b | <1 | 42.3 | 28.9 | 0.012 |
| >1 | 75.2 | 56.7 | ||
| Variables | HR | 95% CI | p | |
|---|---|---|---|---|
| T | T3–4 vs. T1–2 | 2.046 | 1.116–3.752 | 0.021 |
| N | N1–3 vs. N0 | 2.085 | 1.096–3.966 | 0.025 |
| ATM | <0.3 vs. >0.3 | 1.895 | 1.026–3.501 | 0.041 |
| BRCA1 | <1 vs. >1 | 2.163 | 1.037–4.511 | 0.040 |
| Variables | HR | 95% CI | p |
|---|---|---|---|
| ATM<0.3 & BRCA1<1 | 4.195 | 1.779–9.892 | 0.001 |
| ATM > 0.3 & BRCA1 < 1 or ATM < 0.3 & BRCA1 > 1 | 1.815 | 0.747–4.406 | 0.188 |
| ATM > 0.3 & BRCA1 > 1 | 1 | ||
| ATM < 0.3 &T3–4 | 5.519 | 2.456–12.405 | <0.001 |
| ATM > 0.3 & T3–4 or ATM < 0.3 & T1–2 | 2.483 | 1.162–5.304 | 0.019 |
| ATM > 0.3 & T1–2 | 1 | ||
| ATM < 0.3 & N1–3 | 5.143 | 2.202–12.015 | <0.001 |
| ATM > 0.3 & N1–3 or ATM < 0.3 & N0 | 3.001 | 1.406–6.407 | 0.005 |
| ATM > 0.3 & N0 | 1 | ||
| BRCA1 < 1 & T3–4 | 6.517 | 2.204–19.264 | 0.001 |
| BRCA1 > 1 & T3–4 or BRCA1 < 1 & T1–2 | 2.839 | 0.965–8.358 | 0.058 |
| BRCA1 > 1 & T1–2 | 1 | ||
| BRCA1 < 1 & N1–3 | 5.543 | 2.005–15.326 | 0.001 |
| BRCA1 > 1 & N1–3 or BRCA1 < 1 & N0 | 1.963 | 0.738–5.220 | 0.177 |
| BRCA1 > 1 & N0 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.-C.; Lee, K.-W.; Tsai, Y.-S.; Lu, H.-H.; Chen, S.-Y.; Hsieh, H.-Y.; Lin, C.-S. Downregulation of ATM and BRCA1 Predicts Poor Outcome in Head and Neck Cancer: Implications for ATM-Targeted Therapy. J. Pers. Med. 2021, 11, 389. https://doi.org/10.3390/jpm11050389
Wang Y-C, Lee K-W, Tsai Y-S, Lu H-H, Chen S-Y, Hsieh H-Y, Lin C-S. Downregulation of ATM and BRCA1 Predicts Poor Outcome in Head and Neck Cancer: Implications for ATM-Targeted Therapy. Journal of Personalized Medicine. 2021; 11(5):389. https://doi.org/10.3390/jpm11050389
Chicago/Turabian StyleWang, Yu-Chu, Ka-Wo Lee, Yi-Shan Tsai, Hsing-Han Lu, Si-Yun Chen, Hsin-Ying Hsieh, and Chang-Shen Lin. 2021. "Downregulation of ATM and BRCA1 Predicts Poor Outcome in Head and Neck Cancer: Implications for ATM-Targeted Therapy" Journal of Personalized Medicine 11, no. 5: 389. https://doi.org/10.3390/jpm11050389
APA StyleWang, Y.-C., Lee, K.-W., Tsai, Y.-S., Lu, H.-H., Chen, S.-Y., Hsieh, H.-Y., & Lin, C.-S. (2021). Downregulation of ATM and BRCA1 Predicts Poor Outcome in Head and Neck Cancer: Implications for ATM-Targeted Therapy. Journal of Personalized Medicine, 11(5), 389. https://doi.org/10.3390/jpm11050389







