Coping, Anxiety, and Pain Intensity in Patients Requiring Thoracic Surgery
Abstract
:1. Introduction
2. Materials and Methods
- Patients over 18 years of age at the moment of inclusion in the research;
- Patients hospitalized at least 1 day before surgery;
- Patients diagnosed by imaging through chest CT that require a scheduled thoracic surgery;
- Patients who understood study procedures and agreed to take part and sign the Informed Consent Form (ICF).
- Patients suffering from mental disorders that may interfere with the research methods and results;
- Patients unable to understand the research procedures or give written consent;
- Patients with stage IV lung neoplasm;
- Patients with multiple comorbidities and limited life expectancy;
- Thoracic surgical emergency.
- We used the COPE questionnaire to assess coping. Developed by Carver, Scheier, and Weintraub in 1989, the COPE scale is a self-report tool that evaluates the coping strategies of people to stress [27]. The questionnaire, validated and adapted for the Romanian population by Crașovan and Sava (2013), contains 60 items used in evaluating the 15 strategies and 4 coping styles [28]. The answer to each item can be ranked on a scale of 1 to 4, as follows: 1—usually do not do this, 2—rarely do this, 3—sometimes do this, 4—often do this.
- 2.
- The GAD-7 (General Anxiety Disorder-7) Questionnaire was employed to assess anxiety. The questionnaire includes seven items, with the answer from each item rated on a scale from 0 to 3. The final score is obtained by summing the scores of the seven items, with a higher score indicating greater anxiety severity. The sum of the seven items, and therefore the GAD-7 total score, will be a value between 0 and 21, with a total score of 5 representing mild anxiety, 10 representing moderate anxiety, and 15 representing severe anxiety [29].
- 3.
- The characteristics of pain were evaluated using the McGill Pain Questionnaire and Numeric Pain Rating Scale (NPRS).
- (a)
- The McGill Pain Questionnaire scale was utilized for the quantitative and descriptive assessment of the subjective sensation of pain. It consists of three major classes of words describing the painful experience (sensory, affective, and evaluative). It also contains a clinical pain intensity scale and other items to describe the painful sensation (miscellaneous). Pain intensity was rated on a scale from 0 to 5, whereby 0 represents the absence of pain and 5 is maximum intensity. The subscale Number of Words Chosen (NWC) was recorded following Melzack’s instructions [30].
- (b)
- The Numeric Pain Rating Scale (NPRS) is frequently applied in measuring the intensity of pain, with patients asked to select a number from 0 to 10 to indicate the severity of their pain [31].
3. Results
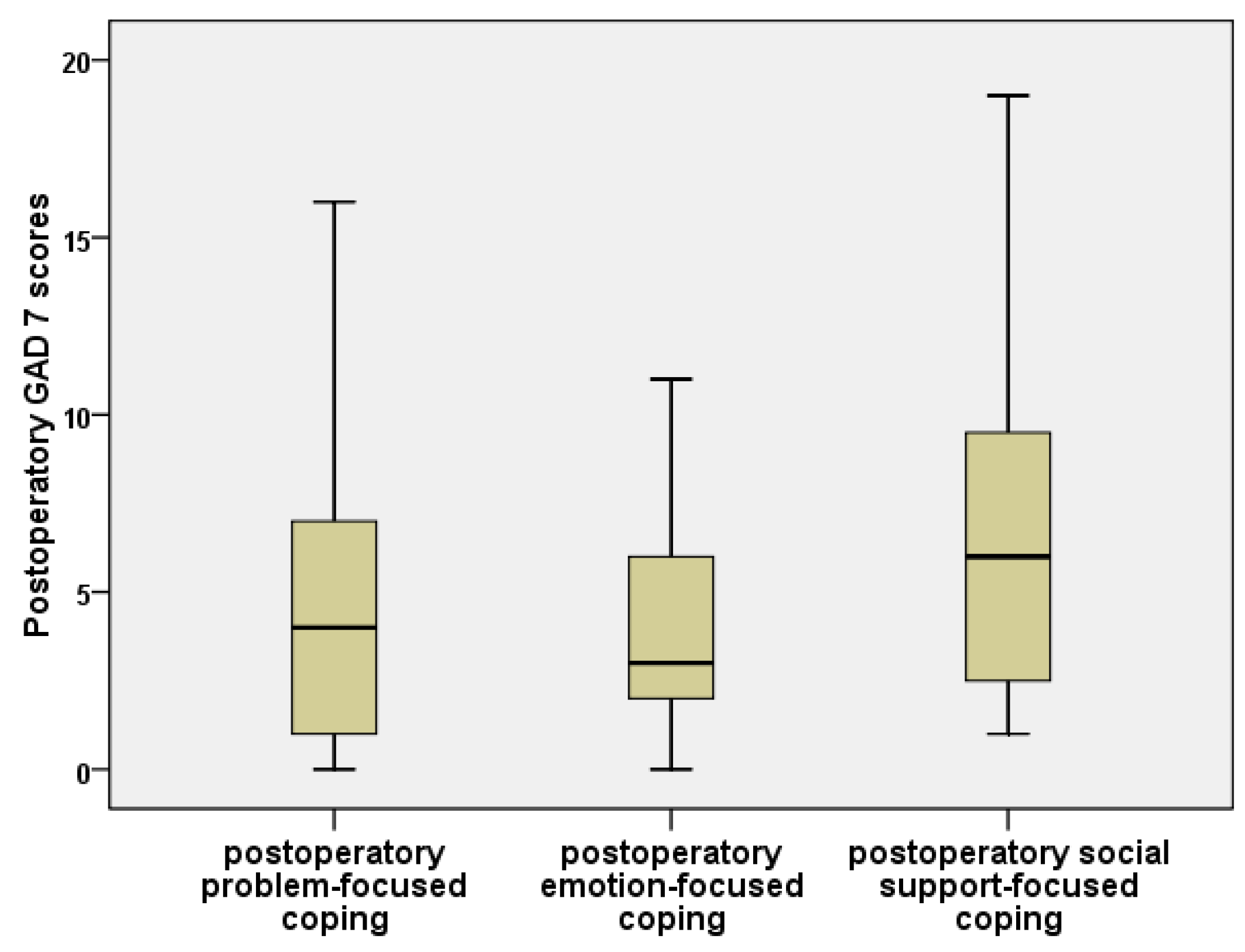
- The GAD-7 anxiety values were insignificantly higher for problem-focused coping than for emotional-focused coping (Mann–Whitney, p = 0.644);
- Problem-focused coping had significantly lower GAD-7 scores than coping centered upon social support (Mann–Whitney, p = 0.048);
- Emotion-focused coping presented significantly lower GAD-7 values than social-support coping (Mann–Whitney, p = 0.026).
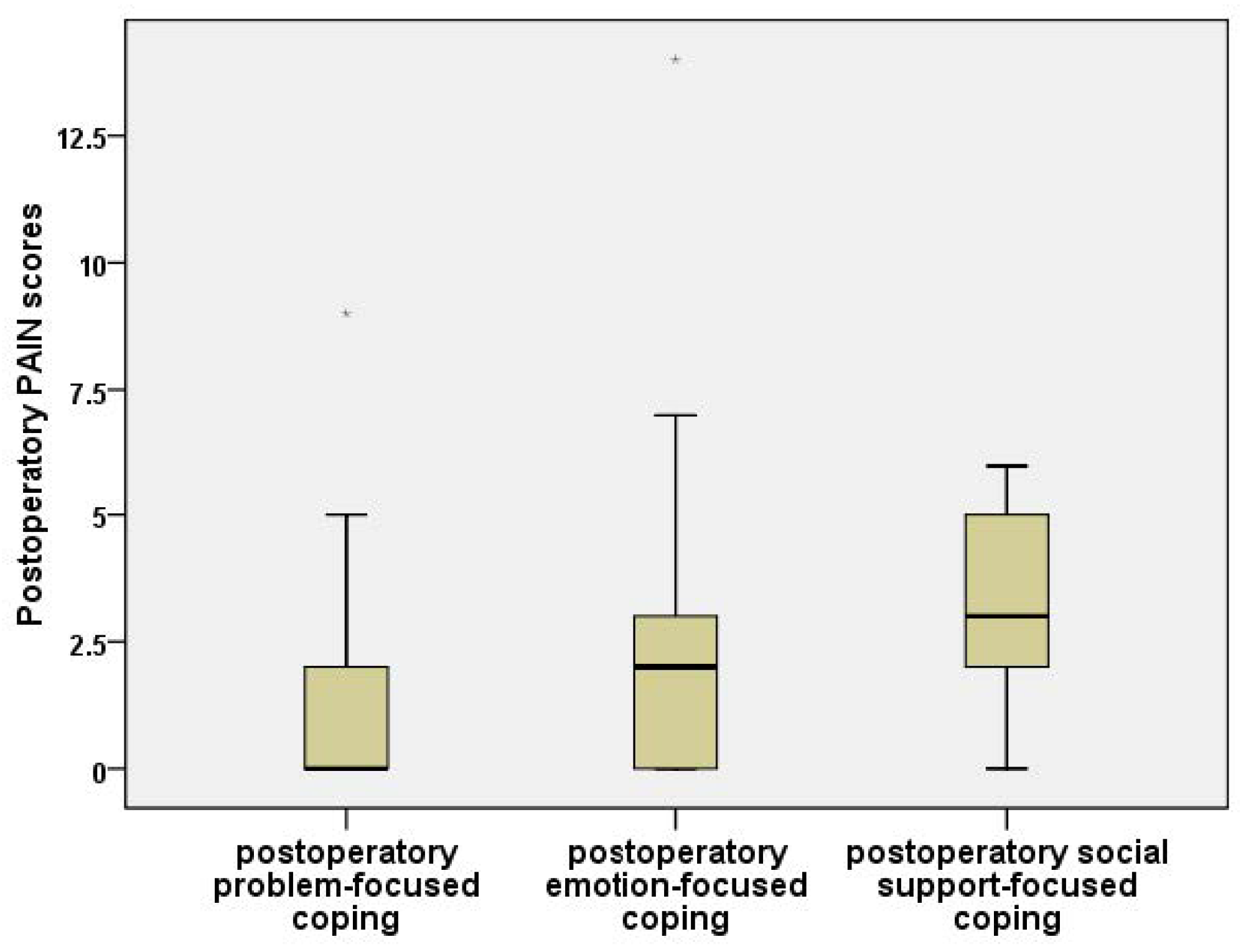
- The differences between the scores obtained for the predominantly problem-centered coping style and predominantly emotion-centered coping style were insignificant, both in the case of “total words” (Mann–Whitney U Test, p = 0.458) and for the intensity of the pain (Mann–Whitney U Test, p = 0.619);
- The scores for “total words” were significantly increased in the predominantly social-support-centered coping cases in contrast to the problem-focused coping cases (Mann–Whitney U Test, p = 0.022). The intensity of pain was significantly higher in the social-support-oriented coping cases as opposed to the problem-oriented coping cases (Mann–Whitney U Test, p = 0.004);
- The scores for “total words” (Mann–Whitney U Test, p = 0.048) and the intensity of the pain (Mann–Whitney U Test, p = 0.006) were significantly higher in the predominant social-support-oriented cases compared with the emotion-focused coping cases.
- The NPRS pain values were insignificantly lower for problem-directed coping in comparison to emotion-directed coping (Mann–Whitney, p = 0.362);
- The problem-focused coping NPRS scores were significantly lower than the social-support-directed coping scores (Mann–Whitney, p = 0.006);
- The emotion-focused coping values were significantly lower than the social-support-oriented coping values (Mann–Whitney, p = 0.042).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607–628. [Google Scholar] [CrossRef] [Green Version]
- Salleh, M.R. Life event, stress and illness. Malaysian J. Med. Sci. 2008, 15, 9–18. [Google Scholar]
- Rosiek, A.; Kornatowski, T.; Rosiek-Kryszewska, A.; Leksowski, Ł.; Leksowski, K. Evaluation of stress intensity and anxiety level in preoperative period of cardiac patients. Biomed. Res. Int. 2016, 2016, 1248396. [Google Scholar] [CrossRef] [Green Version]
- Weeks, J.C.; Cook, E.F.; O’Day, S.J. Relationship between cancer patients predictions of prognosis and their treatment preferences. J. Am. Med. Assoc. 1998, 279, 1709–1714. [Google Scholar] [CrossRef]
- Slatore, L.G.M.M.C.G.; Wiener, R.S.; Golden, S.E.; Au, H.D. Longitudinal Assessment of Distress among Veterans with Incidental Pulmonary Nodules. Ann. Am. Thorac. Soc. 2016, 13, 1983–1991. [Google Scholar] [CrossRef] [PubMed]
- Steimer, T. The biology of fear- and anxiety-related behaviors. Dialogues Clin. Neurosci. 2020, 4, 231–249. [Google Scholar] [CrossRef]
- Kozuka, T.; Johkoh, T.; Hamada, S.; Naito, H.; Tomiyama, N.; Koyama, M.; Mihara, N.; Honda, O.; Nakamura, H.; Kudo, M. Detection of pulmonary metastases with multi-detector row CT scans of 5-mm nominal section thickness: Autopsy lung study. Radiology 2003, 226, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lin, P.Y.; Chien, C.Y.; Fang, F.M.; Wang, L.J. A comparison of psychological well-being and quality of life between spouse and non-spouse caregivers in patients with head and neck cancer: A 6-month follow-up study. Neuropsychiatr. Dis. Treat. 2018, 14, 1697–1704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanks, G.W.; Lloyd, J.W. Depression and anxiety in pain clinics. Anaesthesia 1986, 41, 326. [Google Scholar] [CrossRef]
- Segerstrom, S.C.; Miller, G.E. Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychol. Bull. 2004, 130, 601–630. [Google Scholar] [CrossRef] [Green Version]
- Henoch, I.; Bergman, B.; Gustafsson, M.; Gaston-Johansson, F.; Danielson, E. The Impact of Symptoms, Coping Capacity, and Social Support on Quality-of-Life Experience Over Time in Patients with Lung Cancer. J. Pain Symptom Manag. 2007, 34, 370–379. [Google Scholar] [CrossRef]
- Ali, A.; Altun, D.; Oguz, B.H.; Ilhan, M.; Demircan, F.; Koltka, K. The effect of preoperative anxiety on postoperative analgesia and anesthesia recovery in patients undergoing laparascopic cholecystectomy. J. Anesth. 2014, 28, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K.; Page, G.G.; Marucha, P.T.; MacCallum, R.C.; Glaser, R. Psychological influences on surgical recovery: Perspectives from psychoneuroimmunology. Am. Psychol. 1998, 53, 1209–1218. [Google Scholar] [CrossRef] [PubMed]
- Barnason, S.; Zimmerman, L.; Nieveen, J. The effects of music interventions on anxiety in the patient after coronary artery bypass grafting. Heart Lung J. Acute Crit. Care 1995, 24, 124–132. [Google Scholar] [CrossRef]
- Bernatzky, G.; Presch, M.; Anderson, M.; Panksepp, J. Emotional foundations of music as a non-pharmacological pain management tool in modern medicine. Neurosci. Biobehav. Rev. 2011, 35, 1989–1999. [Google Scholar] [CrossRef]
- Arends, S.; Böhmer, A.B.; Poels, M.; Schieren, M.; Koryllos, A.; Wappler, F.; Joppich, R. Post-thoracotomy pain syndrome: Seldom severe, often neuropathic, treated unspecific, and insufficient. Pain Rep. 2020, 5, e810. [Google Scholar] [CrossRef]
- Macrae, W.A. Chronic post-surgical pain: 10 Years on. Br. J. Anaesth. 2008, 101, 77–86. [Google Scholar] [CrossRef] [Green Version]
- Soto, R.G.; Fu, E.S. Acute Pain Management for Patients Undergoing Thoracotomy. Ann. Thorac. Surg. 2003, 75, 1349–1357. Available online: https://www.annalsthoracicsurgery.org/article/S0003-4975(02)04647-7/fulltext (accessed on 16 October 2021). [CrossRef]
- Furrer, M.; Rechsteiner, R.; Eigenmann, V.; Signer, C.; Althaus, U.; Ris, H.B. Thoracotomy and thoracoscopy: Postoperative pulmonary function, pain and chest wall complaints. Eur. J. Cardio-Thoracic Surg. 1997, 12, 82–87. [Google Scholar] [CrossRef] [Green Version]
- Kol, E.; Alpar, Ş.E.; Erdoǧan, A. Preoperative education and use of analgesic before onset of pain routinely for post-thoracotomy pain control can reduce pain effect and total amount of analgesics administered postoperatively. Pain Manag. Nurs. 2014, 15, 331–339. [Google Scholar] [CrossRef]
- Liu, Y.; Petrini, M.A. Effects of music therapy on pain, anxiety, and vital signs in patients after thoracic surgery. Complement. Ther. Med. 2015, 23, 714–718. [Google Scholar] [CrossRef]
- Slatore, C.G.; Golden, S.E.; Ganzini, L.; Wiener, R.S.; Au, D.H. Distress and patient-centered communication among veterans with incidental (not screen-detected) pulmonary nodules: A cohort study. Ann. Am. Thorac. Soc. 2015, 12, 184–192. [Google Scholar] [CrossRef] [Green Version]
- Jankowska-Polańska, B.; Polański, J.; Chabowski, M.; Rosińczuk, J.; Mazur, G. Influence of Coping Strategy on Perception of Anxiety and Depression in Patients with Non-small Cell Lung Cancer. Adv. Exp. Med. Biol. 2020, 1251, 57–70. [Google Scholar] [CrossRef]
- Chabowski, M.; Jankowska-Polańska, B.; Lomper, K.; Janczak, D. The effect of coping strategy on quality of life in patients with NSCLC. Cancer Manag. Res. 2018, 10, 4085–4093. [Google Scholar] [CrossRef] [Green Version]
- Vaillo, Y.A.; Pérez, S.M.; López, P.M.; Retes, R.R. Mini-Mental Adjustment to Cancer Scale: Construct validation in Spanish breast cancer patients. J. Psychosom. Res. 2018, 114, 38–44. [Google Scholar] [CrossRef]
- Mosher, C.E.; Ott, M.A.; Hanna, N.; Jalal, S.I.; Champion, V.L. Coping with physical and psychological symptoms: A qualitative study of advanced lung cancer patients and their family caregivers. Support. Care Cancer 2015, 23, 2053–2060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CCarver, S.; Scheier, M.F.; Weintraub, K.J. Assessing Coping Strategies: A Theoretically Based Approach. J. Pers. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Crașovan, D.I.; Sava, F.A. Translation, adaptation, and validation on romanian population of cope questionnaire for coping mechanisms analysis. Cogn. Brain Behav. Interdiscip. J. 2013, 17, 61–76. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melzack, R. The short-form McGill pain questionnaire. Pain 1987, 30, 191–197. [Google Scholar] [CrossRef]
- Paice, F.L.C.J.A. Validity of a verbally administered numeric rating scale to measure cancer pain intensity. Cancer Nurs. 1997, 20, 88–93. [Google Scholar] [CrossRef]
- Nelson, F.V.; Zimmerman, L.; Barnason, S.; Nieveen, J.; Schmaderer, M. The relationship and influence of anxiety on postoperative pain in the coronary artery bypass graft patient. J. Pain Symptom Manag. 1998, 15, 102–109. [Google Scholar] [CrossRef]
- Fischer, D.J.; Villines, D.; Kim, Y.O.; Epstein, J.B.; Wilkie, D.J. Anxiety, depression, and pain: Differences by primary cancer. Support. Care Cancer 2010, 18, 801–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sell, G.J.G.L.; Devlin, B.; Bourke, S.J.; Munro, N.C.; Corris, P.A. Communicating the diagnosis of lung cancer. Respir. Med. 1993, 87, 61–63. [Google Scholar] [CrossRef]
- Keefe, F.J.; Abernethy, A.P.; Campbell, L.C. Psychological approaches to understanding and treating disease-related pain. Annu. Rev. Psychol. 2005, 56, 601–630. [Google Scholar] [CrossRef]
- Akechi, T.; Kugaya, A.; Okamura, H.; Nishiwaki, Y.; Yamawaki, S.; Uchitomi, Y. Predictive factors for psychological distress in ambulatory lung cancer patients. Support. Care Cancer 1998, 6, 281–286. [Google Scholar] [CrossRef]
- Walker, M.S.; Zona, D.M.; Fisher, E.B. Depressive symptoms after lung cancer surgery: Their relation to coping style and social support. Psychooncology 2006, 15, 684–693. [Google Scholar] [CrossRef] [PubMed]
- Salminen-Tuomaala, M.; Åstedt-Kurki, P.; Rekiaro, M.; Paavilainen, E. Coping Experiences: A Pathway towards Different Coping Orientations Four and Twelve Months after Myocardial Infarction—A Grounded Theory Approach. Nurs. Res. Pract. 2012, 2012, 674783. [Google Scholar] [CrossRef]
- Tung, H.H.; Hunter, A.; Wei, J. Coping, anxiety and quality of life after coronary artery bypass graft surgery. J. Adv. Nurs. 2008, 61, 651–663. [Google Scholar] [CrossRef]
- Gil, K.M.; Abrams, M.R.; Phillips, G.; Keefe, F.J. Sickle Cell Disease Pain: Relation of Coping Strategies to Adjustment. J. Consult. Clin. Psychol. 1989, 57, 725–731. [Google Scholar] [CrossRef]
- Polański, J.; Jankowska-Polańska, B.; Mazur, G.; Chabowski, M. Strategies of Coping with Pain: Differences Associated with the Histological Type of Lung Cancer. Adv. Exp. Med. Biol. 2019, 1222, 43–53. [Google Scholar] [CrossRef]
- Genç, F.; Tan, M. Symptoms of patients with lung cancer undergoing chemotherapy and coping strategies. Cancer Nurs. 2011, 34, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Horney, D.J.; Smith, H.E.; McGurk, M.; Weinman, J.; Herold, J.; Altman, K.; Llewellyn, C.D. Associations between quality of life, coping styles, optimism, and anxiety and depression in pretreatment patients with head and neck cancer. Head Neck 2011, 33, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Kershaw, A.S.T.; Northouse, L.; Kritpracha, C.; Mood, D. Coping strategies and quality of life in women with advanced breast cancer and their family caregivers. Psychol. Health 2003, 19, 139–155. [Google Scholar] [CrossRef]
- Polański, J.; Chabowski, M.; Chudiak, A.; Uchmanowicz, B.; Janczak, D.; Rosińczuk, J.; Mazur, G. Intensity of anxiety and depression in patients with lung cancer in relation to quality of life. Adv. Exp. Med. Biol. 2018, 1023, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Prasertsri, N.; Holden, J.; Keefe, F.J.; Wilkie, D.J. Repressive coping style: Relationships with depression, pain, and pain coping strategies in lung cancer out patients. Lung Cancer 2011, 71, 235–240. [Google Scholar] [CrossRef] [Green Version]
- Kuo, T.; Ma, F.-C. Symptom Distresses and Coping Strategies in Patients with Non-small Cell Lung Cancer. Cancer Nurs. 2002, 25, 309–317. [Google Scholar] [CrossRef]
- Shimizu, K.; Nakaya, N.; Saito-Nakaya, K.; Akechi, T.; Ogawa, A.; Fujisawa, D.; Sone, T.; Yoshiuchi, K.; Goto, K.; Iwasaki, M.; et al. Personality traits and coping styles explain anxiety in lung cancer patients to a greater extent than other factors. Jpn. J. Clin. Oncol. 2015, 45, 456–463. [Google Scholar] [CrossRef] [Green Version]
- Oancea, C.; Suciu, C.; Timar, B.; Papava, I.; Raica, M.; Burlacu, O. The reciprocal relationship between coping mechanisms and lung cancer diagnosis: Findings of a prospective study. Cancer Manag. Res. 2018, 10, 33–40. [Google Scholar] [CrossRef] [Green Version]
- Papava, I.; Oancea, C.; Enatescu, V.R.; Bredicean, A.C.; Dehelean, L.; Romosan, R.S.; Timar, B. The impact of coping on the somatic and mental status of patients with COPD: A cross-sectional study. Int. J. COPD 2016, 11, 1343–1351. [Google Scholar] [CrossRef] [Green Version]
- Scharloo, M.; Kaptein, A.A.; Weinman, J.A.; Willems, L.N.A.; Rooijmans, H.G.M. Physical and psychological correlates of functioning in patients with chronic obstructive pulmonary disease. J. Asthma 2000, 37, 17–29. [Google Scholar] [CrossRef] [PubMed]


| Variable | No Cancer (n = 50) | Cancer (n = 40) | p-Value |
|---|---|---|---|
| Age (mean ± std. dev.) | 46.8 ± 13.29 | 62 ± 8.07 | <0.001 *,(a) |
| Sex (Masculine) n (%) | 24 (48%) | 22 (55%) | 0.532 (b) |
| Marital Status (Yes) n (%) | 39 (78%) | 30 (75%) | 0.805 (b) |
| Higher education (Yes) n (%) | 15 (30%) | 6 (15%) | 0.133 (b) |
| With activity (student, employed) n (%) | 30 (60%) | 10 (25%) | 0.001 *,(b) |
| Environment (urban) n (%) | 30 (60%) | 27 (67.5%) | 0.514 (b) |
| Smoke (Yes) n (%) | 12 (24%) | 10 (25%) | 0.913 (b) |
| Variable | Thoracoscopy (n = 8) | Mini Thoracotomy (n = 27) | Thoracotomy (n = 55) | p-Value Kruskal–Wallis Test |
|---|---|---|---|---|
| GAD-7— postoperative | 2 (4.8) | 4 (6.0) | 5 (6.0) | 0.459 |
| McGill—Sensory postoperative | 0 (1.0) | 1 (1.0) | 1 (1.0) | 0.392 |
| McGill—Affective postoperative | 0 (1.0) | 1 (1.0) | 1 (1.0) | 0.370 |
| McGill—Evaluative postoperative | 0 (1.0) | 1 (1.0) | 1 (1.0) | 0.392 |
| McGill—Miscellaneous postoperative | 0 (1.0) | 1 (1.0) | 1 (1.0) | 0.392 |
| McGill—“Total words” postoperative | 0 (1.0) | 1 (1.0) | 1 (1.0) | 0.430 |
| McGill—Intensity of postoperative pain | 0 (1.0) | 1 (2.0) | 1 (2.0) | 0.377 |
| McGill—Total postoperative | 0 (1.0) | 1 (1.0) | 1 (1.0) | 0.392 |
| Numeric Pain Rating Scale (NPRS) | 0 (2.0) | 2 (4.0) | 2 (3.0) | 0.274 |
| Duration of surgical intervention | 90 (33.8) | 90 (30.0) | 180 (120.0) | <0.001 * |
| Variable | Coping Focused on Problem (n = 37) | Coping Focused on Emotion (n = 33) | Coping Focused on Social Support (n = 20) | p-Value Kruskal–Wallis Test |
|---|---|---|---|---|
| GAD-7 | 4 (7.0) | 3 (5.0) | 6 (8.0) | 0.028 * |
| McGill—Sensory postoperative | 0 (1.0) | 1 (1.0) | 1 (0.0) | 0.134 |
| McGill—Affective postoperative | 0 (1.0) | 1 (1.0) | 1 (0.0) | 0.152 |
| McGill—Evaluative postoperative | 0 (1.0) | 1 (1.0) | 1 (0.0) | 0.134 |
| McGill—Miscellaneous postoperative | 0 (1.0) | 1 (1.0) | 1 (0.0) | 0.134 |
| McGill—“Total words” postoperative | 0 (1.0) | 1 (1.0) | 1 (0.0) | 0.042 * |
| McGill—Intensity of postoperative pain | 0 (1.0) | 1 (1.0) | 2 (1.0) | 0.007 * |
| McGill—Total postoperative | 0 (1.0) | 1 (1.0) | 1 (0.0) | 0.134 |
| Numeric Pain Rating Scale (NPRS) | 0 (3.0) | 2 (3.0) | 3 (3.0) | 0.022 * |
| Duration of surgical intervention | 120 (130.0) | 115 (118.0) | 117.5 (83.0) | 0.993 |
| Variable | Without Anxiety (n = 37) | Mild Anxiety(n = 33) | Moderate Anxiety (n = 8) | Severe Anxiety (n = 6) | p-Value Kruskal–Wallis Test |
|---|---|---|---|---|---|
| NPRS postoperative | 2 (3.0) | 1 (3.0) | 0 (4.0) | 3.5 (5.0) | 0.253 |
| McGill—Sensory postoperative | 1 (1.0) | 0.5 (1.0) | 0 (1.0) | 1 (1.0) | 0.186 |
| McGill—Affective postop | 1 (1.0) | 0.5 (1.0) | 0 (1.0) | 1 (2.0) | 0.178 |
| McGill—Evaluative postoperative | 1 (1.0) | 0.5 (1.0) | 0 (1.0) | 1 (1.0) | 0.186 |
| McGill—Intensity of postoperative pain | 1 (2.0) | 0.5 (2.0) | 0 (1.0) | 1 (2.0) | 0.160 |
| McGill—Total postoperative | 1 (1.0) | 0.5 (1.0) | 0 (1.0) | 1 (1.0) | 0.186 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasan, E.M.; Calma, C.L.; Tudor, A.; Oancea, C.; Tudorache, V.; Petrache, I.A.; Tudorache, E.; Papava, I. Coping, Anxiety, and Pain Intensity in Patients Requiring Thoracic Surgery. J. Pers. Med. 2021, 11, 1221. https://doi.org/10.3390/jpm11111221
Hasan EM, Calma CL, Tudor A, Oancea C, Tudorache V, Petrache IA, Tudorache E, Papava I. Coping, Anxiety, and Pain Intensity in Patients Requiring Thoracic Surgery. Journal of Personalized Medicine. 2021; 11(11):1221. https://doi.org/10.3390/jpm11111221
Chicago/Turabian StyleHasan, Elisei Moise, Crenguta Livia Calma, Anca Tudor, Cristian Oancea, Voicu Tudorache, Ioan Adrian Petrache, Emanuela Tudorache, and Ion Papava. 2021. "Coping, Anxiety, and Pain Intensity in Patients Requiring Thoracic Surgery" Journal of Personalized Medicine 11, no. 11: 1221. https://doi.org/10.3390/jpm11111221
APA StyleHasan, E. M., Calma, C. L., Tudor, A., Oancea, C., Tudorache, V., Petrache, I. A., Tudorache, E., & Papava, I. (2021). Coping, Anxiety, and Pain Intensity in Patients Requiring Thoracic Surgery. Journal of Personalized Medicine, 11(11), 1221. https://doi.org/10.3390/jpm11111221






