Patient-Specific Instrument Guided Double Chevron-Cut Distal Femur Osteotomy
Abstract
:1. Introduction
2. Materials and Methods
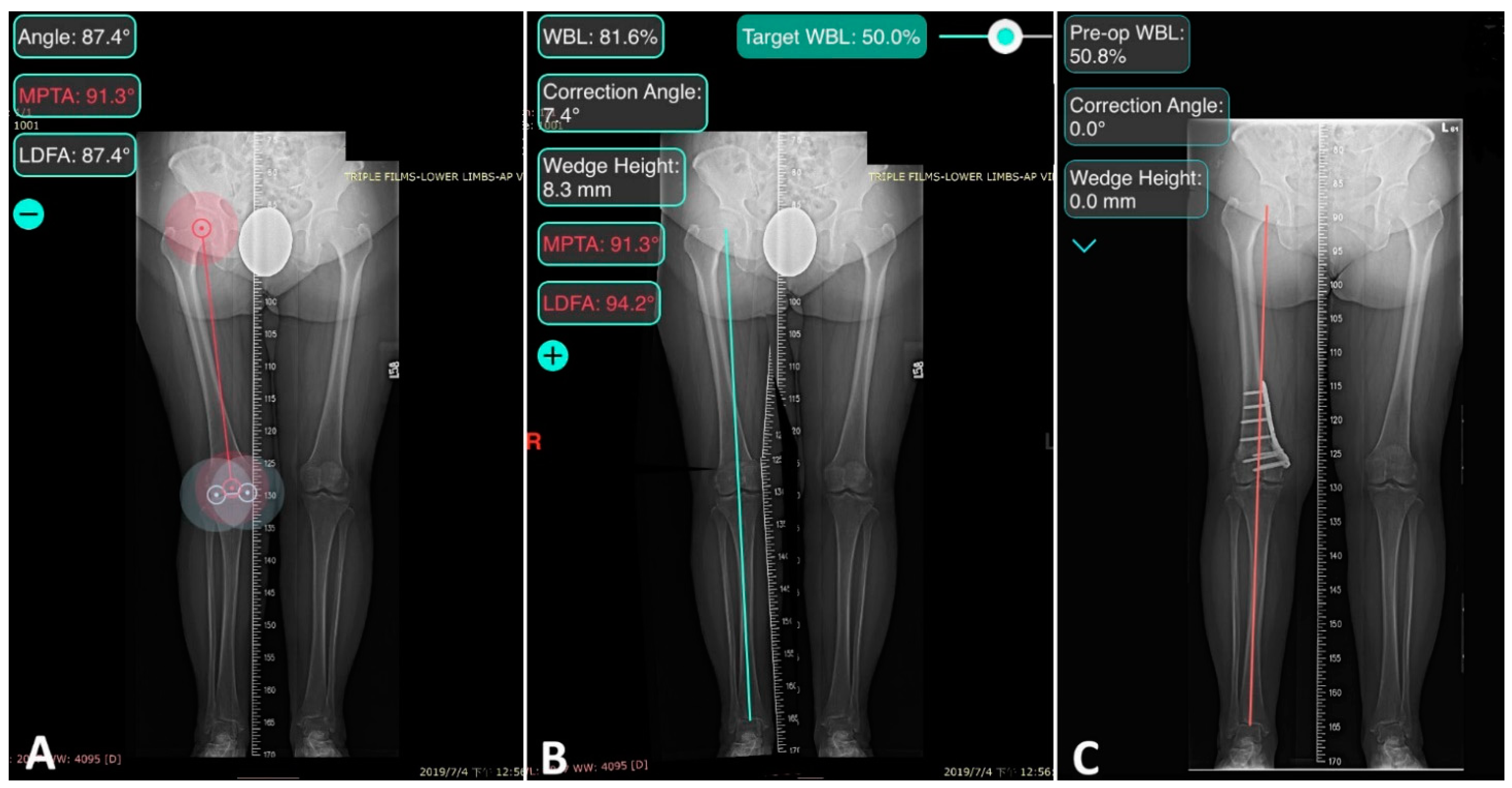
2.1. Preoperative Planning
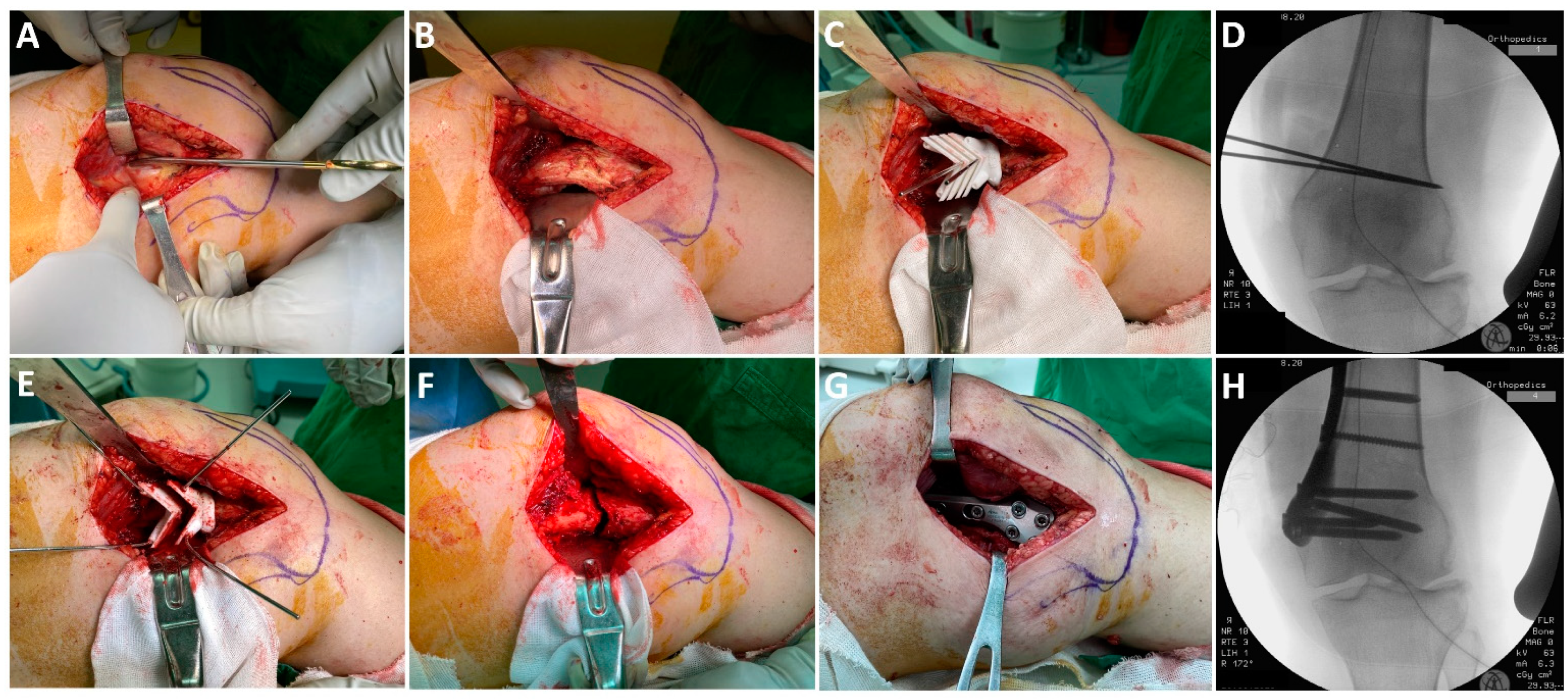
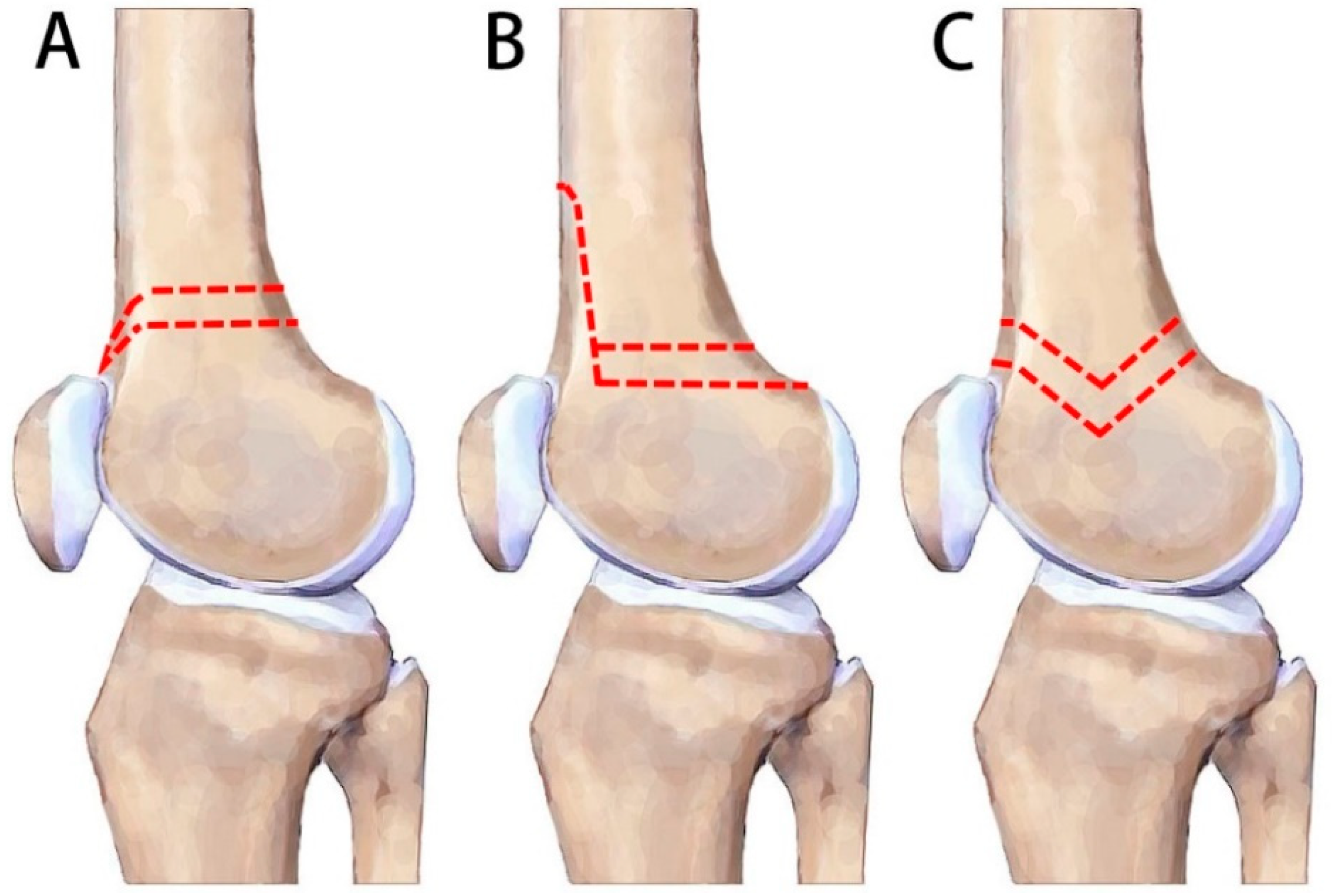
2.2. Surgical Technique
2.3. Postoperative Care
2.4. Data Collection and Radiographic Assessment
2.5. Statistics
3. Results
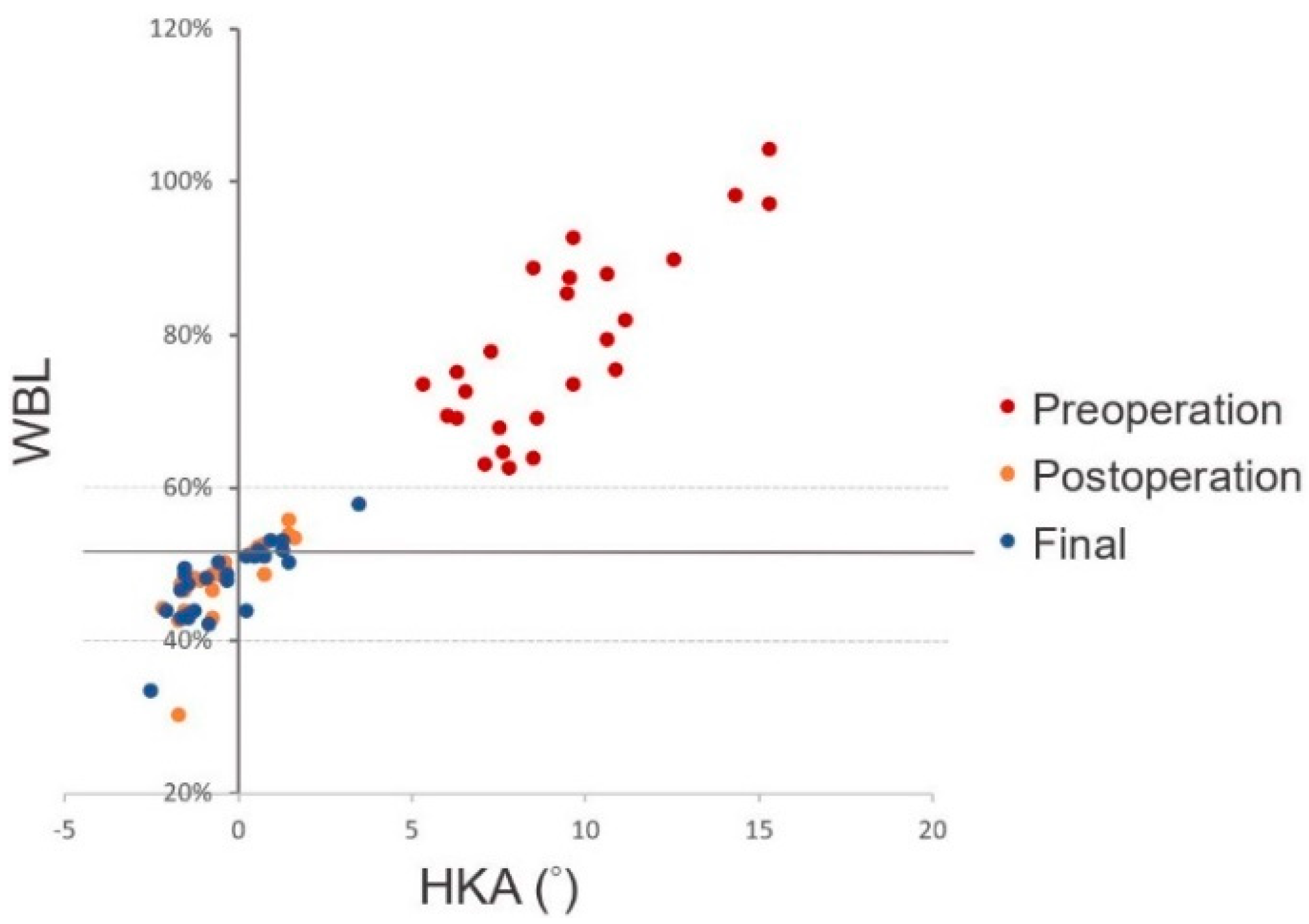
3.1. Radiological Results
3.2. Postoperative Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mirouse, G.; Dubory, A.; Roubineau, F.; Poignard, A.; Hernigou, P.; Allain, J.; Lachaniette, C.F. Failure of high tibial varus osteotomy for lateral tibio-femoral osteoarthritis with <10° of valgus: Outcomes in 19 patients. Orthop. Traumatol. Surg. Res. 2017, 103, 953–958. [Google Scholar] [CrossRef]
- Marin Morales, L.A.; Gomez Navalon, L.A.; Zorrilla Ribot, P.; Salido Valle, J.A. Treatment of osteoarthritis of the knee with valgus deformity by means of varus osteotomy. Acta Orthop. Belg. 2000, 66, 272–278. [Google Scholar]
- Wylie, J.; Jones, D.L.; Hartley, M.K.; Kapron, A.L.; Krych, A.J.; Aoki, S.K.; Maak, T.G. Distal Femoral Osteotomy for the Valgus Knee: Medial Closing Wedge Versus Lateral Opening Wedge: A Systematic Review. Arthroscopy 2016, 32, 2141–2147. [Google Scholar] [CrossRef]
- Kim, Y.C.; Yang, J.-H.; Kim, H.J.; Tawonsawatruk, T.; Chang, Y.S.; Lee, J.S.; Bhandare, N.N.; Kim, K.S.; Delgado, G.D.; Nha, A.K.W. Distal Femoral Varus Osteotomy for Valgus Arthritis of the Knees: Systematic Review of Open versus Closed Wedge Osteotomy. Knee Surg. Relat. Res. 2018, 30, 3–16. [Google Scholar] [CrossRef] [Green Version]
- Cameron, H.U.; Botsford, D.J.; Park, Y.S. Prognostic factors in the outcome of supracondylar femoral osteotomy for lateral compartment osteoarthritis of the knee. Can. J. Surg. 1997, 40, 114–118. [Google Scholar]
- Edgerton, B.C.; Mariani, E.M.; Morrey, B.F. Distal femoral varus osteotomy for painful genu valgum. A five-to-11-year follow-up study. Clin. Orthop. Relat. Res. 1993, 288, 263–269. [Google Scholar]
- Mathews, J.; Cobb, A.G.; Richardson, S.; Bentley, G. Distal femoral osteotomy for lateral compartment osteoarthritis of the knee. Orthopedics 1998, 21, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Forkel, P.; Achtnich, A.; Metzlaff, S.; Zantop, T.; Petersen, W. Midterm results following medial closed wedge distal femoral osteotomy stabilized with a locking internal fixation device. Knee Surg. Sports Traumatol. Arthrosc. 2014, 23, 2061–2067. [Google Scholar] [CrossRef] [PubMed]
- Freiling, D.; van Heerwaarden, R.; Staubli, A.; Lobenhoffer, P. The medial closed-wedge osteotomy of the distal femur for the treatment of unicompartmental lateral osteoarthritis of the knee. Oper. Orthop. Traumatol. 2010, 22, 317–334. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [Green Version]
- Uquillas, C.; Rossy, W.; Nathasingh, C.K.; Strauss, E.; Jazrawi, L.; Gonzalez-Lomas, G. Osteotomies about the knee: AAOS exhibit selection. J. Bone Jt. Surg. Am. 2014, 96, e199. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.L.; Thompson, S.F.; Clohisy, J.C.F. Distal Femoral Varus Osteotomy for the Management of Valgus Deformity of the Knee. JAAOS—J. Am. Acad. Orthop. Surg. 2018, 26, 313–324. [Google Scholar] [CrossRef]
- Parvizi, J.; Miller, A.G.; Gandhi, K. Multimodal pain management after total joint arthroplasty. J. Bone Jt. Surg Am. 2011, 93, 1075–1108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reising, K.; Strohm, P.C.; Hauschild, O.; Schmal, H.; Khattab, M.; Südkamp, N.P.; Niemeyer, P. Computer-assisted navigation for the intraoperative assessment of lower limb alignment in high tibial osteotomy can avoid outliers compared with the conventional technique. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 181–188. [Google Scholar] [CrossRef]
- Dawson, J.; Fitzpatrick, R.; Murray, D.; Carr, A. Questionnaire on the perceptions of patients about total knee replacement. J. Bone Jt. Surg. Br. 1998, 80, 63–69. [Google Scholar] [CrossRef]
- Scuderi, G.R.; Bourne, R.B.; Noble, P.C.; Benjamin, J.B.; Lonner, J.H.; Scott, W.N. The new Knee Society Knee Scoring System. Clin. Orthop. Relat. Res. 2012, 470, 3–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drexler, M.; Gross, A.; Dwyer, T.; Safir, O.; Backstein, D.; Chaudhry, H.; Goulding, A.; Kosashvili, Y. Distal femoral varus osteotomy combined with tibial plateau fresh osteochondral allograft for post-traumatic osteoarthritis of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1317–1323. [Google Scholar] [CrossRef]
- Saithna, A.; Kundra, R.; Getgood, A.; Spalding, T. Opening wedge distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. Knee 2014, 21, 172–175. [Google Scholar] [CrossRef]
- Finkelstein, J.A.; Gross, A.E.; Davis, A. Varus osteotomy of the distal part of the femur. A survivorship analysis. J. Bone Jt. Surg. Am. 1996, 78, 1348–1352. [Google Scholar] [CrossRef]
- Backstein, D.; Morag, G.; Hanna, S.; Safir, O.; Gross, A. Long-term follow-up of distal femoral varus osteotomy of the knee. J. Arthroplast. 2007, 22, 2–6. [Google Scholar] [CrossRef]
- Wang, J.W.; Hsu, C.C. Distal femoral varus osteotomy for osteoarthritis of the knee. J. Bone Jt. Surg. Am. 2005, 87, 127–133. [Google Scholar] [CrossRef]
- van der Woude, J.A.D.; Spruijt, S.; van Ginneken, B.T.J.; van Heerwaarden, R.J. Distal femoral valgus osteotomy: Bone healing time in single plane and biplanar technique. Strat. Trauma Limb Reconstr. 2016, 11, 177–186. [Google Scholar] [CrossRef] [Green Version]
- van Heerwaarden, R.; Najfeld, M.; Brinkman, M.; Seil, R.; Madry, H.; Pape, D. Wedge volume and osteotomy surface depend on surgical technique for distal femoral osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2012, 21, 206–212. [Google Scholar] [CrossRef]
- Brinkman, J.M.; Hurschler, C.; Staubli, A.E.; van Heerwaarden, R.J. Axial and torsional stability of an improved single-plane and a new bi-plane osteotomy technique for supracondylar femur osteotomies. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1090–1098. [Google Scholar] [CrossRef] [PubMed]
- Nha, K.W.; Chang, Y.S.; Shon, O.-J.; Shim, B.-J.; Lee, J.S.; Song, J.S.; Bae, J.-H. Where is the Target Point to Prevent Cortical Hinge Fracture in Medial Closing-Wedge Distal Femoral Varus Osteotomy? J. Knee Surg. 2019, 32, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Muratli, K.S.; Karatosun, V.; Uzun, B.; Celik, S. Subtrochanteric shortening in total hip arthroplasty: Biomechanical comparison of four techniques. J. Arthroplast. 2014, 29, 836–842. [Google Scholar] [CrossRef] [PubMed]
- Acevedo, J.I.; Sammarco, V.J.; Boucher, H.R.; Parks, B.G.; Schon, L.C.; Myerson, M.S. Mechanical comparison of cyclic loading in five different first metatarsal shaft osteotomies. Foot Ankle Int. 2002, 23, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Gutteck, N.; Haase, K.; Kielstein, H.; Delank, K.S.; Arnold, C. Biomechanical results of percutaneous calcaneal osteotomy using two different osteotomy designs. Foot Ankle Surg. 2020, 26, 551–555. [Google Scholar] [CrossRef]
- Hofmann, S.; Lobenhoffer, P.; Staubli, A.; Van Heerwaarden, R. Osteotomies of the knee joint in patients with monocompartmental arthritis. Orthopade 2009, 38, 755–770. [Google Scholar] [CrossRef]
- Jacquet, C.; Chan-Yu-Kin, J.; Sharma, A.; Argenson, J.-N.; Parratte, S.; Ollivier, M. “More accurate correction using “patient-specific” cutting guides in opening wedge distal femur varization osteotomies. Int. Orthop. 2018, 43, 2285–2291. [Google Scholar] [CrossRef] [PubMed]
- Arnal-Burró, J.; Pérez-Mañanes, R.; Gallo-Del-Valle, E.; Igualada-Blazquez, C.; Cuervas-Mons, M.; Vaquero-Martín, J. Three dimensional-printed patient-specific cutting guides for femoral varization osteotomy: Do it yourself. Knee 2017, 24, 1359–1368. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Lv, W.; Wang, Y.; Ma, B.; Cui, W.; Liu, Z.; Han, K. Three dimensional patient-specific printed cutting guides for closing-wedge distal femoral osteotomy. Int. Orthop. 2018, 43, 619–624. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Value |
|---|---|
| Sex (men:women ratio) | 3:20 |
| Age (years, mean and range) | 64 (47–80) |
| Involved extremity (Right:Left) | 15:11 |
| BMI (mean ± SD and range) | 27 ± 5 (19–37) |
| Smoking | 3 |
| Kellgren–Lawrence grade | |
| 1 | 12 |
| 2 | 11 |
| 3 | 2 |
| Follow up (months, mean ± SD and range) | 17 ± 8 (12–37) |
| Value | |
|---|---|
| Operative time (minutes) | 58.8 ± 18.3 |
| Intraoperative radiograph (number) | 6.2 ± 1.3 |
| Preoperative Hb (g/dL) | 13.5 ± 1.3 |
| Hb level on postoperative day 1 (g/dL) | 12.1 ± 1.2 |
| Outcomes | Values | ||
|---|---|---|---|
| Pre-Operation | Post-Operation | p-Value | |
| Active ROM (°) | 131 ± 4 | 128 ± 10 | 0.18 |
| OKS score | 27.6 ± 11.7 | 39.1 ± 7.5 | 0.03 * |
| KSS score | 92.1 ± 13.0 | 143.9 ± 10.2 | <0.001 * |
| Outcomes | Values | ||
|---|---|---|---|
| Pre-Operation | 2 Days Post-Operation (p Value) | Final (p Value) | |
| WBL ratio (%) | 78.7 ± 12.0 | 48.7 ± 2.9 (<0.001) * | 48.1 ± 3.8 (0.44) |
| HKA (°) | 9.3 ± 2.8 | −0.5 ± 1.1 (<0.001) * | −0.3 ± 1.4 (0.58) |
| LDFA (°) | 83.6 ± 1.9 | 91.4 ± 3.5 (<0.001) * | 90.8 ± 3.7 (0.32) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.-C.; Chen, K.-J.; Lin, K.-Y.; Lee, O.K.-S.; Yang, J.C.-S. Patient-Specific Instrument Guided Double Chevron-Cut Distal Femur Osteotomy. J. Pers. Med. 2021, 11, 959. https://doi.org/10.3390/jpm11100959
Huang Y-C, Chen K-J, Lin K-Y, Lee OK-S, Yang JC-S. Patient-Specific Instrument Guided Double Chevron-Cut Distal Femur Osteotomy. Journal of Personalized Medicine. 2021; 11(10):959. https://doi.org/10.3390/jpm11100959
Chicago/Turabian StyleHuang, Yen-Chun, Kuan-Jung Chen, Kuan-Yu Lin, Oscar Kuang-Sheng Lee, and Jesse Chieh-Szu Yang. 2021. "Patient-Specific Instrument Guided Double Chevron-Cut Distal Femur Osteotomy" Journal of Personalized Medicine 11, no. 10: 959. https://doi.org/10.3390/jpm11100959
APA StyleHuang, Y.-C., Chen, K.-J., Lin, K.-Y., Lee, O. K.-S., & Yang, J. C.-S. (2021). Patient-Specific Instrument Guided Double Chevron-Cut Distal Femur Osteotomy. Journal of Personalized Medicine, 11(10), 959. https://doi.org/10.3390/jpm11100959






