Risk Reclassification of Patients with Endometrial Cancer Based on Tumor Molecular Profiling: First Real World Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Ethics
2.3. Pathologic Processing
2.4. Cancer Gene Panel Sequencing
2.5. Immunohistochemistry and Microsatellite Instability Testing
2.6. Risk Group Classification
2.7. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.M.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef]
- Bokhman, J.V. Two pathogenetic types of endometrial carcinoma. Gynecol. Oncol. 1983, 15, 10–17. [Google Scholar] [CrossRef]
- Gilks, C.B.; Oliva, E.; Soslow, R.A. Poor interobserver reproducibility in the diagnosis of high-grade endometrial carcinoma. Am. J. Surg. Pathol. 2013, 37, 874–881. [Google Scholar] [CrossRef]
- Creutzberg, C.L.; van Putten, W.L.; Koper, P.C.; Lybeert, M.L.; Jobsen, J.J.; Warlam-Rodenhuis, C.C.; De Winter, K.A.; Lutgens, L.C.; van den Bergh, A.C.; van de Steen-Banasik, E.; et al. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: Multicentre randomised trial. PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma. Lancet 2000, 355, 1404–1411. [Google Scholar] [CrossRef]
- Nout, R.A.; Smit, V.T.; Putter, H.; Jurgenliemk-Schulz, I.M.; Jobsen, J.J.; Lutgens, L.C.; van der Steen-Banasik, E.M.; Mens, J.W.; Slot, A.; Kroese, M.C.; et al. Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): An open-label, non-inferiority, randomised trial. Lancet 2010, 375, 816–823. [Google Scholar] [CrossRef]
- Ortoft, G.; Hansen, E.S.; Bertelsen, K. Omitting adjuvant radiotherapy in endometrial cancer increases the rate of locoregional recurrences but has no effect on long-term survival: The Danish Endometrial Cancer Study. Int. J. Gynecol. Cancer 2013, 23, 1429–1437. [Google Scholar] [CrossRef]
- Thomas, G.M. A role for adjuvant radiation in clinically early carcinoma of the endometrium? Int. J. Gynecol. Cancer 2010, 20, S64–S66. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Research, N.; Kandoth, C.; Schultz, N.; Cherniack, A.D.; Akbani, R.; Liu, Y.; Shen, H.; Robertson, A.G.; Pashtan, I.; Shen, R.; et al. Integrated genomic characterization of endometrial carcinoma. Nature 2013, 497, 67–73. [Google Scholar] [CrossRef]
- Kommoss, S.; McConechy, M.K.; Kommoss, F.; Leung, S.; Bunz, A.; Magrill, J.; Britton, H.; Kommoss, F.; Grevenkamp, F.; Karnezis, A.; et al. Final validation of the ProMisE molecular classifier for endometrial carcinoma in a large population-based case series. Ann. Oncol. 2018, 29, 1180–1188. [Google Scholar] [CrossRef]
- Bosse, T.; Nout, R.A.; McAlpine, J.N.; McConechy, M.K.; Britton, H.; Hussein, Y.R.; Gonzalez, C.; Ganesan, R.; Steele, J.C.; Harrison, B.T.; et al. Molecular Classification of Grade 3 Endometrioid Endometrial Cancers Identifies Distinct Prognostic Subgroups. Am. J. Surg. Pathol. 2018, 42, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Bosse, T.; Peters, E.E.; Creutzberg, C.L.; Jurgenliemk-Schulz, I.M.; Jobsen, J.J.; Mens, J.W.; Lutgens, L.C.; van der Steen-Banasik, E.M.; Smit, V.T.; Nout, R.A. Substantial lymph-vascular space invasion (LVSI) is a significant risk factor for recurrence in endometrial cancer--A pooled analysis of PORTEC 1 and 2 trials. Eur. J. Cancer 2015, 51, 1742–1750. [Google Scholar] [CrossRef] [PubMed]
- Zeimet, A.G.; Reimer, D.; Huszar, M.; Winterhoff, B.; Puistola, U.; Azim, S.A.; Muller-Holzner, E.; Ben-Arie, A.; van Kempen, L.C.; Petru, E.; et al. L1CAM in early-stage type I endometrial cancer: Results of a large multicenter evaluation. J. Natl. Cancer Inst. 2013, 105, 1142–1150. [Google Scholar] [CrossRef]
- Kurnit, K.C.; Kim, G.N.; Fellman, B.M.; Urbauer, D.L.; Mills, G.B.; Zhang, W.; Broaddus, R.R. CTNNB1 (beta-catenin) mutation identifies low grade, early stage endometrial cancer patients at increased risk of recurrence. Mod. Pathol 2017, 30, 1032–1041. [Google Scholar] [CrossRef]
- Stelloo, E.; Nout, R.A.; Osse, E.M.; Jurgenliemk-Schulz, I.J.; Jobsen, J.J.; Lutgens, L.C.; van der Steen-Banasik, E.M.; Nijman, H.W.; Putter, H.; Bosse, T.; et al. Improved Risk Assessment by Integrating Molecular and Clinicopathological Factors in Early-stage Endometrial Cancer-Combined Analysis of the PORTEC Cohorts. Clin. Cancer Res. 2016, 22, 4215–4224. [Google Scholar] [CrossRef]
- de Boer, S.M.; Powell, M.E.; Mileshkin, L.; Katsaros, D.; Bessette, P.; Haie-Meder, C.; Ottevanger, P.B.; Ledermann, J.A.; Khaw, P.; Colombo, A.; et al. Adjuvant chemoradiotherapy versus radiotherapy alone for women with high-risk endometrial cancer (PORTEC-3): Final results of an international, open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2018, 19, 295–309. [Google Scholar] [CrossRef]
- Leon-Castillo, A.; de Boer, S.M.; Powell, M.E.; Mileshkin, L.R.; Mackay, H.J.; Leary, A.; Nijman, H.W.; Singh, N.; Pollock, P.M.; Bessette, P.; et al. Molecular Classification of the PORTEC-3 Trial for High-Risk Endometrial Cancer: Impact on Prognosis and Benefit From Adjuvant Therapy. J. Clin. Oncol. 2020, 38, 3388–3397. [Google Scholar] [CrossRef]
- Creutzberg, C.L.; Leon-Castillo, A.; de Boer, S.M.; Powell, M.E.; Mileshkin, L.R.; Mackay, H.J.; Leary, A.; Nijman, H.W.; Singh, N.; Pollock, P.M.; et al. Molecular classification of the PORTEC-3 trial for high-risk endometrial cancer: Impact on adjuvant therapy. Ann. Oncol. 2019, 30, v899–v900. [Google Scholar] [CrossRef]
- Colombo, N.; Creutzberg, C.; Amant, F.; Bosse, T.; Gonzalez-Martin, A.; Ledermann, J.; Marth, C.; Nout, R.; Querleu, D.; Mirza, M.R.; et al. ESMO-ESGO-ESTRO consensus conference on endometrial cancer: Diagnosis, treatment and follow-up. Radiother. Oncol. 2015, 117, 559–581. [Google Scholar] [CrossRef]
- Kurman, R.J. WHO Classification of Tumours, 4th ed.; IARC: Lyon, France, 2014; Volume 6. [Google Scholar]
- Union for International Cancer Control. TNM Classification of Malignant Tumours, 8th ed.; Wiley Blackwell: Hoboke, NJ, USA, 2017. [Google Scholar]
- Do, H.; Dobrovic, A. Dramatic reduction of sequence artefacts from DNA isolated from formalin-fixed cancer biopsies by treatment with uracil-DNA glycosylase. Oncotarget 2012, 3, 546–558. [Google Scholar] [CrossRef] [PubMed]
- Loeb, L.A.; Kohrn, B.F.; Loubet-Senear, K.J.; Dunn, Y.J.; Ahn, E.H.; O’Sullivan, J.N.; Salk, J.J.; Bronner, M.P.; Beckman, R.A. Extensive subclonal mutational diversity in human colorectal cancer and its significance. Proc. Natl. Acad. Sci. USA 2019, 116, 26863–26872. [Google Scholar] [CrossRef]
- Yu, J.; Wang, Q.; Xue, P.; Zheng, L.; Mo, J.; Chen, L.; Yin, M.; Huang, Y.; Bao, Y.; Ding, F. A model for the impact of FFPE section thickness on gene copy number measurement by FISH. Sci. Rep. 2019, 9, 7518. [Google Scholar] [CrossRef]
- Cheung, C.C.; Banerjee, D.; Barnes, P.J.; Berendt, R.C.; Butany, J.; Canil, S.; Clarke, B.A.; El-Zimaity, H.; Garratt, J.; Geldenhuys, L.; et al. Canadian Association of Pathologists-Association canadienne des pathologistes National Standards Committee for High Complexity Testing/Immunohistochemistry: Guidelines for the preparation, release, and storage of unstained archived diagnostic tissue sections for immunohistochemistry. Am. J. Clin. Pathol. 2014, 142, 629–633. [Google Scholar] [CrossRef]
- Wang, H.L.; Kim, C.J.; Koo, J.; Zhou, W.; Choi, E.K.; Arcega, R.; Chen, Z.E.; Wang, H.; Zhang, L.; Lin, F. Practical Immunohistochemistry in Neoplastic Pathology of the Gastrointestinal Tract, Liver, Biliary Tract, and Pancreas. Arch. Pathol. Lab. Med. 2017, 141, 1155–1180. [Google Scholar] [CrossRef]
- Umar, A.; Boland, C.R.; Terdiman, J.P.; Syngal, S.; de la Chapelle, A.; Ruschoff, J.; Fishel, R.; Lindor, N.M.; Burgart, L.J.; Hamelin, R.; et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J. Natl. Cancer Inst. 2004, 96, 261–268. [Google Scholar] [CrossRef]
- Concin, N.; Matias-Guiu, X.; Vergote, I.; Cibula, D.; Mirza, M.R.; Marnitz, S.; Ledermann, J.; Bosse, T.; Chargari, C.; Fagotti, A.; et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int. J. Gynecol. Cancer 2020, 31. [Google Scholar] [CrossRef]
- Pecorelli, S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int. J. Gynaecol. Obstet. 2009, 105, 103–104. [Google Scholar] [CrossRef]
- Van Gool, I.C.; Rayner, E.; Osse, E.M.; Nout, R.A.; Creutzberg, C.L.; Tomlinson, I.P.M.; Church, D.N.; Smit, V.; de Wind, N.; Bosse, T.; et al. Adjuvant Treatment for POLE Proofreading Domain-Mutant Cancers: Sensitivity to Radiotherapy, Chemotherapy, and Nucleoside Analogues. Clin. Cancer Res. 2018, 24, 3197–3203. [Google Scholar] [CrossRef]
- Le, D.T.; Uram, J.N.; Wang, H.; Bartlett, B.R.; Kemberling, H.; Eyring, A.D.; Skora, A.D.; Luber, B.S.; Azad, N.S.; Laheru, D.; et al. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N. Engl. J. Med. 2015, 372, 2509–2520. [Google Scholar] [CrossRef]
- Marabelle, A.; Le, D.T.; Ascierto, P.A.; Di Giacomo, A.M.; De Jesus-Acosta, A.; Delord, J.P.; Geva, R.; Gottfried, M.; Penel, N.; Hansen, A.R.; et al. Efficacy of Pembrolizumab in Patients With Noncolorectal High Microsatellite Instability/Mismatch Repair-Deficient Cancer: Results From the Phase II KEYNOTE-158 Study. J. Clin. Oncol. 2020, 38, 1–10. [Google Scholar] [CrossRef]
- Talhouk, A.; McConechy, M.K.; Leung, S.; Yang, W.; Lum, A.; Senz, J.; Boyd, N.; Pike, J.; Anglesio, M.; Kwon, J.S.; et al. Confirmation of ProMisE: A simple, genomics-based clinical classifier for endometrial cancer. Cancer 2017, 123, 802–813. [Google Scholar] [CrossRef]
- Pergialiotis, V.; Haidopoulos, D.; Tzortzis, A.S.; Antonopoulos, I.; Thomakos, N.; Rodolakis, A. The impact of waiting intervals on survival outcomes of patients with endometrial cancer: A systematic review of the literature. Eur. J. Obset. Gynecol. Reprod. Biol. 2020, 246, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, R., II; Hanna, R.K.; Jacobsen, G.; Elshaikh, M.A. Interval between hysterectomy and start of radiation treatment is predictive of recurrence in patients with endometrial carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Leon-Castillo, A.; Gilvazquez, E.; Nout, R.; Smit, V.T.; McAlpine, J.N.; McConechy, M.; Kommoss, S.; Brucker, S.Y.; Carlson, J.W.; Epstein, E.; et al. Clinicopathological and molecular characterisation of ‘multiple-classifier’ endometrial carcinomas. J. Pathol. 2020, 250, 312–322. [Google Scholar] [CrossRef] [PubMed]
| Antigen | Clone/Clonality | Dilution of Primary Antibody | Company |
|---|---|---|---|
| MLH1 | M1/mouse monoclonal | Ready to use | Ventana Medical Systems |
| PMS2 | EPR3947/rabbit monoclonal | Ready to use | Cell Marque (Rocklin, CA, USA) |
| MSH2 | G219-1129/mouse monoclonal | Ready to use | Cell Marque |
| MSH6 | 44/mouse monoclonal | Ready to use | Cell Marque |
| L1CAM | 14.10/mouse monoclonal | 1:100 | BioLegend (San Diego, CA, USA) |
| Variable | No. (%)/Median (Range) |
|---|---|
| No. of patients analyzed | 40 |
| Patient age | 62.1 (29.9–83.6) |
| BMI | 28.5 (18.3–46.0) |
| FIGO Stage | |
| Ia | 18 (45.0) |
| Ib | 12 (30.0) |
| II | 7 (17.5) |
| IIIc1 | 2 (5.9) |
| IIIc2 | 1 (2.5) |
| Nodal involvement | |
| Nx | 4 (10.0) |
| N0 | 29 (72.5)) |
| N1 | 3 (7.5) |
| N0 (i+) | 4 (10.0) |
| Tumor grading | |
| G1 | 15 (37.5) |
| G2 | 13 (32.5) |
| G3 | 12 (30.0) |
| LVSI | |
| No LVSI | 23 (57.5) |
| Mild LVSI | 14 (35.0) |
| Substantial LVSI | 3 (7.5) |
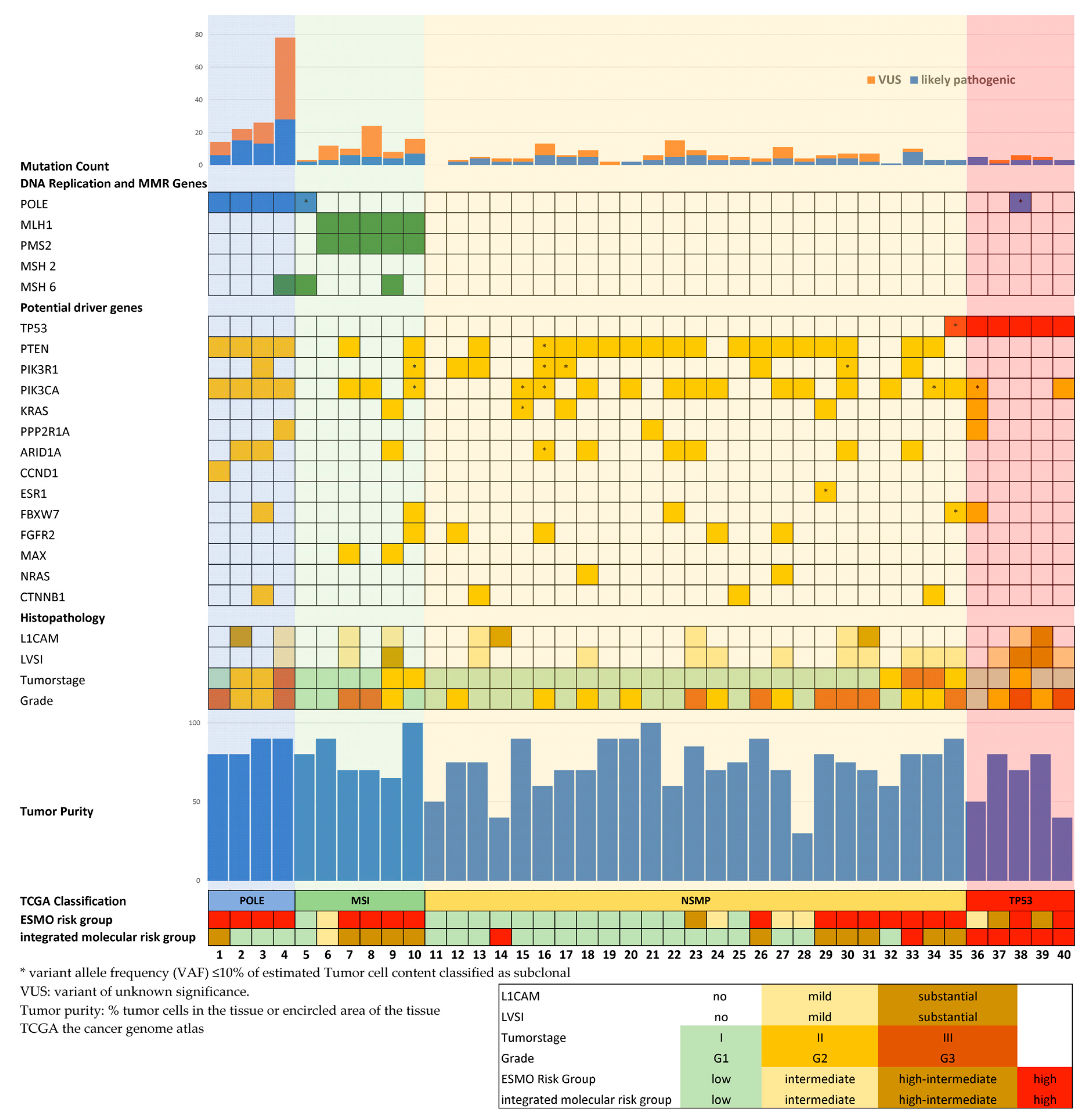
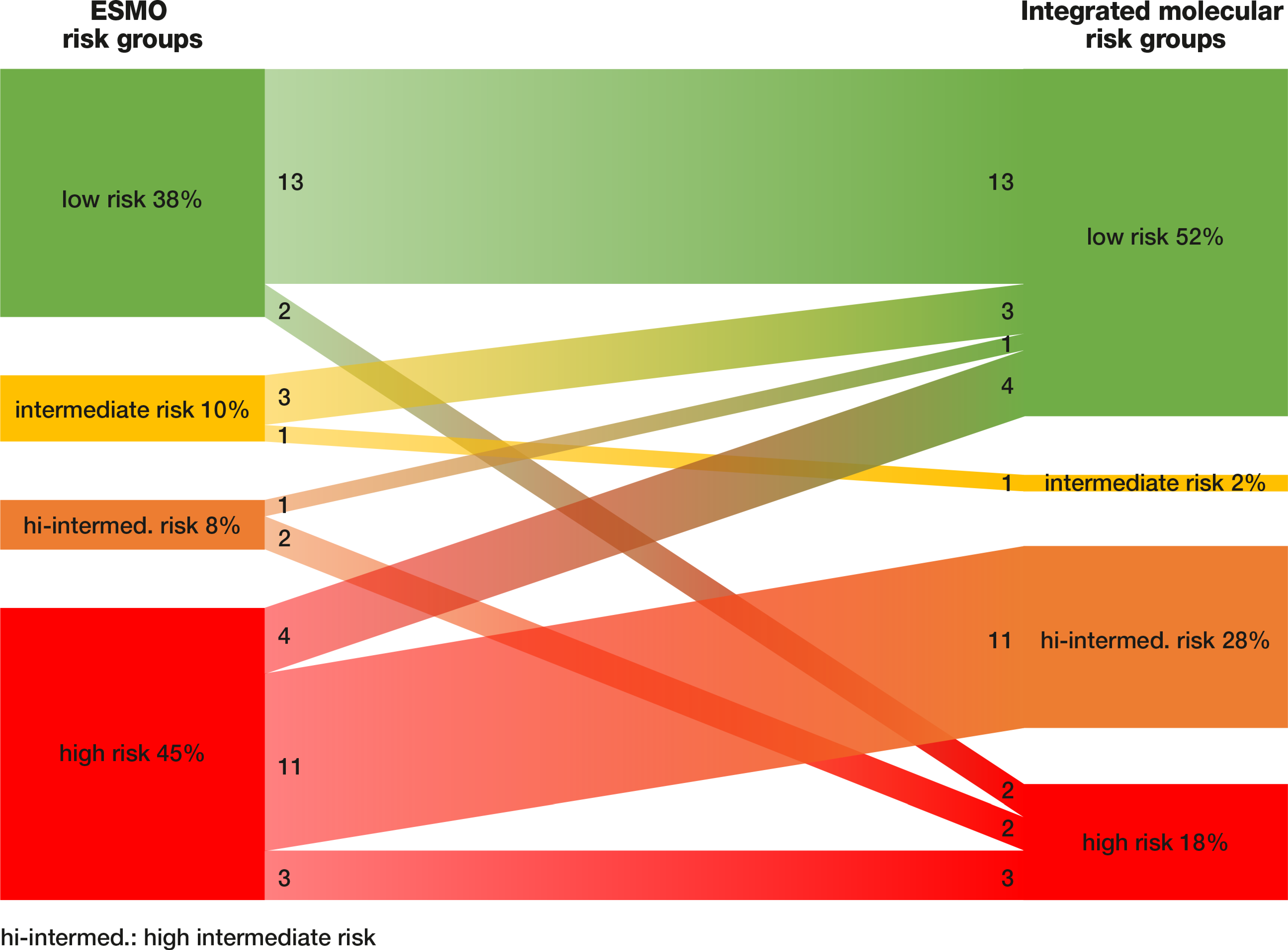
| ESMO Risk Group | Molecular Subtypes | Integrated Molecular Risk Group | ||||||
|---|---|---|---|---|---|---|---|---|
| POLE | MSI | NSMP | TP53 | Low | Intermediate | High–Intermediate | High | |
| Low | 0 (0.0) | 1 (6.7) | 13 (86.7) | 1 (6.7) | 13 (86.7) | 0 (0.0) | 0 (0.0) | 2 (13.3) |
| Intermediate | 0 (0.0) | 1 (25.0) | 3 (75.0) | 0 (0.0) | 3 (75.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) |
| High–intermediate | 0 (0.0) | 0 (0.0) | 1 (33.3) | 2 (66.6) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 2 (66.7) |
| High | 4 (22.2) | 4 (22.2) | 8 (44.4) | 2 (11.1) | 4 (22.2) | 0 (0.0) | 11 (61.1) | 3 (16.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oberndorfer, F.; Moling, S.; Hagelkruys, L.A.; Grimm, C.; Polterauer, S.; Sturdza, A.; Aust, S.; Reinthaller, A.; Müllauer, L.; Schwameis, R. Risk Reclassification of Patients with Endometrial Cancer Based on Tumor Molecular Profiling: First Real World Data. J. Pers. Med. 2021, 11, 48. https://doi.org/10.3390/jpm11010048
Oberndorfer F, Moling S, Hagelkruys LA, Grimm C, Polterauer S, Sturdza A, Aust S, Reinthaller A, Müllauer L, Schwameis R. Risk Reclassification of Patients with Endometrial Cancer Based on Tumor Molecular Profiling: First Real World Data. Journal of Personalized Medicine. 2021; 11(1):48. https://doi.org/10.3390/jpm11010048
Chicago/Turabian StyleOberndorfer, Felicitas, Sarah Moling, Leonie Annika Hagelkruys, Christoph Grimm, Stephan Polterauer, Alina Sturdza, Stefanie Aust, Alexander Reinthaller, Leonhard Müllauer, and Richard Schwameis. 2021. "Risk Reclassification of Patients with Endometrial Cancer Based on Tumor Molecular Profiling: First Real World Data" Journal of Personalized Medicine 11, no. 1: 48. https://doi.org/10.3390/jpm11010048
APA StyleOberndorfer, F., Moling, S., Hagelkruys, L. A., Grimm, C., Polterauer, S., Sturdza, A., Aust, S., Reinthaller, A., Müllauer, L., & Schwameis, R. (2021). Risk Reclassification of Patients with Endometrial Cancer Based on Tumor Molecular Profiling: First Real World Data. Journal of Personalized Medicine, 11(1), 48. https://doi.org/10.3390/jpm11010048








