Ultrasound Images That Speak: Assessing the Therapeutic Decision in the Emergency Department Regarding the Risk–Benefit Ratio of Systemic Thrombolysis in Intermediate-High-Risk Pulmonary Embolism—A Case Report
Abstract
1. Introduction
2. Materials and Methods
2.1. Point-of-Care Blood Analysis
2.2. Point-of-Care-Ultrasound Transthoracic Echocardiography (POCUS—TTE)
2.3. Computed Tomography Pulmonary Angiography (CTPA)
3. Case Presentation
3.1. Clinical Summary
3.2. Diagnostic Findings
3.3. Therapeutic Management and Immediate ED Outcome
3.4. Cardiological Clinical Course During Hospital Stay
4. Discussion
Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| A A–a DO2 | alveolar oxygen pressure alveolar–arterial oxygen gradient |
| a/A | arterial-to-alveolar oxygen ratio |
| ABG | arterial blood gas |
| ALP | alkaline phosphatase |
| ALT | alanine aminotransferase |
| AST | aspartate aminotransferase |
| aPTT | activated partial thromboplastin time |
| BE | base excess |
| BD | direct bilirubin |
| BP | blood pressure |
| bpm | beats per minute |
| CaO2 | arterial oxygen content |
| CcO2 | end-capillary oxygen content |
| CK | creatine kinase |
| CK-MB | creatine kinase MB isoenzyme |
| Cl | chloride |
| COHb | carboxyhemoglobin |
| CRP | C-reactive protein |
| CT | computed tomography |
| CTPA | computed tomography pulmonary angiography |
| DVT | deep vein thrombosis |
| ECG | electrocardiogram |
| ED | Emergency Department |
| eGFR | estimated glomerular filtration rate |
| ESR | erythrocyte sedimentation rate |
| EU | European Union |
| FA | folic acid |
| FiO2 | fraction of inspired oxygen |
| GGT | gamma-glutamyl transferase |
| HBG | hemoglobin |
| HCO3− | bicarbonate ion |
| HCT | hematocrit |
| HDL | high-density lipoprotein cholesterol |
| HHb | deoxyhemoglobin |
| hs-CRP | high-sensitivity C-reactive protein |
| hs-cTnI | high-sensitivity cardiac troponin I |
| ICT | intracardiac thrombus |
| IMG | immature granulocytes |
| INR | international normalized ratio |
| IVC | inferior vena cava |
| K | potassium |
| LDH | lactate dehydrogenase |
| LDL | low-density lipoprotein cholesterol |
| LV | left ventricle |
| MCV | mean corpuscular volume |
| Mg | magnesium |
| MCH | mean corpuscular hemoglobin |
| MCHC mg mL mmHg µg | mean corpuscular hemoglobin concentration milligrams milliliters millimeters of mercury micrograms |
| MPV | mean platelet volume |
| Na ng | sodium nanograms |
| NT-proBNP O2 | N-terminal pro–B-type natriuretic peptide oxygen |
| O2Cap | oxygen capacity |
| O2Ct | oxygen content |
| O2Hb | oxyhemoglobin |
| PCT | procalcitonin |
| PDW | platelet distribution width |
| PE | pulmonary embolism |
| PESI | Pulmonary Embolism Severity Index |
| pH | potential of hydrogen |
| PaCO2 | arterial partial pressure of carbon dioxide |
| PaO2 pg | arterial partial pressure of oxygen picograms |
| PLT | platelets |
| POCUS | point-of-care ultrasound |
| POCUS-TTE | point-of-care transthoracic echocardiography |
| PSA | prostate-specific antigen |
| PT | prothrombin time |
| RA | right atrium |
| RBC | red blood cells |
| RV | right ventricle |
| RV/LV ratio | right-to-left ventricular diameter ratio |
| SaO2 | arterial oxygen saturation |
| SO2 | oxygen saturation |
| SpO2 | peripheral oxygen saturation |
| TAPSE | tricuspid annular plane systolic excursion |
| TB | total bilirubin |
| TG | triglycerides |
| TR Vmax | tricuspid regurgitation maximum velocity |
| TSAT | transferrin saturation |
| TTE | transthoracic echocardiography |
| U.M. | unit of measure |
| USA Vitamin B12 | United States of America cobalamin |
| Vmax | maximum velocity |
| VTE | venous thromboembolism |
| WBCs WI | white blood cells Wisconsin |
References
- Rokosh, R.S.; Ranganath, N.; Yau, P.; Rockman, C.; Sadek, M.; Berland, T.; Jacobowitz, G.; Berger, J.; Maldonado, T.S. High Prevalence and Mortality Associated with Upper Extremity Deep Venous Thrombosis in Hospitalized Patients at a Tertiary Care Center. Ann. Vasc. Surg. 2020, 65, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Glazier, C.R.; Baciewicz, F.A., Jr. Epidemiology, Etiology, and Pathophysiology of Pulmonary Embolism. Int. J. Angiol. 2024, 33, 76–81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jiménez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur. Heart J. 2020, 41, 543–603. [Google Scholar] [CrossRef] [PubMed]
- de Wit, K.; D’Arsigny, C.L. Risk stratification of acute pulmonary embolism. J. Thromb. Haemost. 2023, 21, 3016–3023. [Google Scholar] [CrossRef] [PubMed]
- Machanahalli Balakrishna, A.; Reddi, V.; Belford, P.M.; Alvarez, M.; Jaber, W.A.; Zhao, D.X.; Vallabhajosyula, S. Intermediate-Risk Pulmonary Embolism: A Review of Contemporary Diagnosis, Risk Stratification and Management. Medicina 2022, 58, 1186. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Santos Martínez, L.E.; Uriona Villarroel, J.E.; Exaire Rodríguez, J.E.; Mendoza, D.; Martínez Guerra, M.L.; Pulido, T.; Bautista, E.; Castañón, A.; Sandoval, J. Tromboembolia pulmonar masiva, trombo en tránsito y disfunción ventricular derecha [Massive pulmonary embolism, thrombus in transit, and right ventricular dysfunction]. Arch. Cardiol. Mex. 2007, 77, 44–53. (In Spanish) [Google Scholar] [PubMed]
- Pappas, A.J.; Knight, S.W.; McLean, K.Z.; Bork, S.; Kurz, M.C.; Sawyer, K.N. Thrombus-in-Transit: A Case for a Multidisciplinary Hospital-Based Pulmonary Embolism System of Care. J. Emerg. Med. 2016, 51, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.L.; Salah, Z.; Halpern, N.A. Intracardiac Thrombus in Transit Detected by Point-of-Care Ultrasound. Crit. Care Nurs. Q. 2022, 45, 285–287. [Google Scholar] [CrossRef] [PubMed]
- Bajwa, A.; Farooqui, S.M.; Hussain, S.T.; Vandyck, K. Right heart thrombus in transit: Raising bar in the management of cardiac arrest. Respir. Med. Case Rep. 2022, 41, 101801. [Google Scholar] [CrossRef] [PubMed]
- Osterwalder, J.; Polyzogopoulou, E.; Hoffmann, B. Point-of-Care Ultrasound-History, Current and Evolving Clinical Concepts in Emergency Medicine. Medicina 2023, 59, 2179. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alerhand, S.; Sundaram, T.; Gottlieb, M. What are the echocardiographic findings of acute right ventricular strain that suggest pulmonary embolism? Anaesth. Crit. Care Pain Med. 2021, 40, 100852. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, M.; Bay, C.; Skrocki, L.; Rahimi, F.; Mehdipour, M.; “MOPETT” Investigators. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” Trial). Am. J. Cardiol. 2013, 111, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Meyer, G.; Vicaut, E.; Danays, T.; Agnelli, G.; Becattini, C.; Beyer-Westendorf, J.; Bluhmki, E.; Bouvaist, H.; Brenner, B.; Couturaud, F.; et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N. Engl. J. Med. 2014, 370, 1402–1411. [Google Scholar] [CrossRef] [PubMed]
- Unat, Ö.S.S.; Korkmaz, P.; Çinkooğlu, A.; Can, Ö.; Soydan, E.; Bayraktaroğlu, S.; Çok, G.; Savaş, R.; Karbek Akarca, F.; Nalbantgil, S.; et al. Comparison of half-dose alteplase and LMWH in intermediate-high risk pulmonary embolism: A single-center observational study. Egypt. Heart J. 2025, 77, 74. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mahajan, K.; Negi, P.; Asotra, S.; Dev, M. Right atrial free-floating thrombus in a patient with acute pulmonary embolism. BMJ Case Rep. 2016, 2016, bcr2016215414. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pai, P.G.; Hegde, N.N.; Shah, S. Thrombus-in-transit involving all four chambers of the heart in a patient presenting with acute pulmonary embolism. J. Cardiol. Cases 2022, 26, 186–189. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gil-Rodrigo, A.; Martín-Torres, J.M.; Cano-Carratalá, S. Free-floating thrombus in transit in a patient with recurrent syncope. Emergencias 2021, 33, 244–245, (In English and Spanish). [Google Scholar] [CrossRef] [PubMed]



| Parameter Category | Test (U.M.) | ED Result | Reference Range |
|---|---|---|---|
| Hematology | WBC (109/L) | 15.44 | 4.00–10.00 |
| Neutrophils (109/L) | 11.27 | 2.00–7.00 | |
| Lymphocytes (109/L) | 2.65 | 0.80–4.00 | |
| Monocytes (109/L) | 1.48 | 0.12–1.20 | |
| Eosinophils (109/L) | 0.01 | 0.02–0.50 | |
| Basophils (109/L) | 0.03 | 0.00–0.10 | |
| IMG (109/L) | 0.15 | 0.00–999.999 | |
| RBC (1012/L) | 4.51 | 3.50–5.50 | |
| HBG (g/dL) | 15.2 | 11–16 | |
| HCT (%) | 44.8 | 37–54 | |
| MCV (fL) | 99.3 | 80–100 | |
| MHC (pg) | 33.7 | 27–34 | |
| PLT (109/L) | 207 | 100–300 | |
| MPV (fL) | 10.9 | 6.5–12 | |
| PDW | 16.8 | 16–17 | |
| PCT (%) | 0.226 | 0.108–0.282 | |
| Coagulation | aPTT (s) | 24.0 | 23.5–36.5 |
| PT (s) | 13.0 | 9–13 | |
| Prothrombin index (%) | 80 | 80–145% | |
| INR | 1.16 | 0.79–1.16 | |
| ABG at FiO2 21% | pH | 7.437 | 7.35–7.45 |
| PaCO2 (mmHg) | 20.9 | 35–45 | |
| PaO2 (mmHg) | 86.8 | 75–100 | |
| SaO2 (%) | 95 | 95–99 | |
| O2Hb (%) | 92.5 | 94–98 | |
| COHb (%) | 1.9 | 0.5–1.5 | |
| HHb (%) | 5.2 | 0.4–3 | |
| O2Cap (mL/dL) | 21.4 | 20 | |
| A (mmHg) | 118.5 | Calculated alveolar formula | |
| O2Ct (mL/dL) | 21 | 18–22 | |
| A-aDO2 (mmHg) | 31.7 | <30 in older adults | |
| a/A | 0.7 | >0.75 | |
| PaO2/FiO2 | 415.3 | >300 | |
| CcO2 (mL/dL) | 21.4 | Calculated formula | |
| CaO2 (mL/dL) | 20.5 | 18–22 | |
| HCO3− (mmol/L) | 14.1 | 22–26 | |
| BE (mmol/L) | −10.7 | −2 to +2 | |
| Lactate (mmol/L) | 1.8 | <2.0 | |
| Gap (mmol/L) | 19.5 | 8–12 | |
| Liver Function | ALT (U/L) | 80 | <50 |
| AST (U/L) | 113 | <50 | |
| BD (mg/dL) | 0.43 | <0.2 | |
| TB (mg/dL) | 1.67 | 0.3–1.2 | |
| Muscle Injury | CK (U/L) | 86 | <171 |
| CK-MB (U/L) | 36 | <24 | |
| Cellular Injury | LDH (U/L) | 521 | <248 |
| Inflammation | hs-CRP mg/L | >30 | <5 |
| Renal Function | Creatinine (mg/dL) | 1.70 | 0.67–1.17 |
| eGFR (mL/min/1.73 m2) | 41.1 | >60 | |
| Urea (mg/dL) | 87 | 17–43 | |
| Glycemic Status | Glucose (mg/dL) | 176 | 74–106 |
| Electrolytes | Na (mmol/L) | 139 | 136–146 |
| K (mmol/L) | 4.38 | 3.5–5.1 | |
| Cl (mmol/L) | 97 | 101–109 | |
| Mg (mmol/L) | 0.44 | 0.42–0.59 |
| Wells Score—Parameters, Points and Risk Classification | |||
| Clinical signs and symptoms of DVT | No | 1.5 points | Low risk group |
| PE is the first diagnosis OR equally likely | No | ||
| Heart rate > 100 bpm | Yes | ||
| Immobilization at least 3 days OR surgery in the previous 4 weeks | No | ||
| Previous, objectively diagnosed PE or DVT | No | ||
| Hemoptysis | No | ||
| Malignancy or treatment within 6 months or palliative | No | ||
| Geneva Score—Parameters, Points and Risk Classification | |||
| Age > 65 | Yes | 6 points | Moderate risk group |
| Previous DVT or PE | No | ||
| Surgery (under general anesthesia) or lower limb fracture in past month | No | ||
| Active malignant condition Solid or hematologic malignant condition, currently active or considered cured < 1 year | No | ||
| Unilateral lower limb pain | No | ||
| Hemoptysis | No | ||
| Heart rate | Yes | ||
| Pain on lower limb palpation and unilateral edema | No | ||
| Simplified PESI—Parameters, Points and Risk Classification | |||
| Age, years > 80 | No | 0 points | Low risk group |
| History of cancer | No | ||
| History of chronic cardiopulmonary disease | No | ||
| Heart rate ≥ 110 bpm | No | ||
| Systolic BP ≥ 100 mmHg | No | ||
| O2 saturation > 90% | No | ||
| BOVA Score—Parameters, Points and Risk Classification | |||
| Systolic BP > 100 mmHg | Yes | ||
| Elevated cardiac troponin | Yes | 4 points | Intermediate risk |
| RV dysfunction | Yes | ||
| Heart rate ≥ 110 bpm | No | ||
| Biomerkers—Parameters, Values and Risk Classification | |||
| D-dimer (µg/mL) | 3.76 | high | Suggestive of thrombosis |
| hs-cTnI (ng/mL) | 119 | high | Intermediate-high-risk |
| NT-proBNP (pg/mL) | 15.136 | high | Intermediate-high-risk |
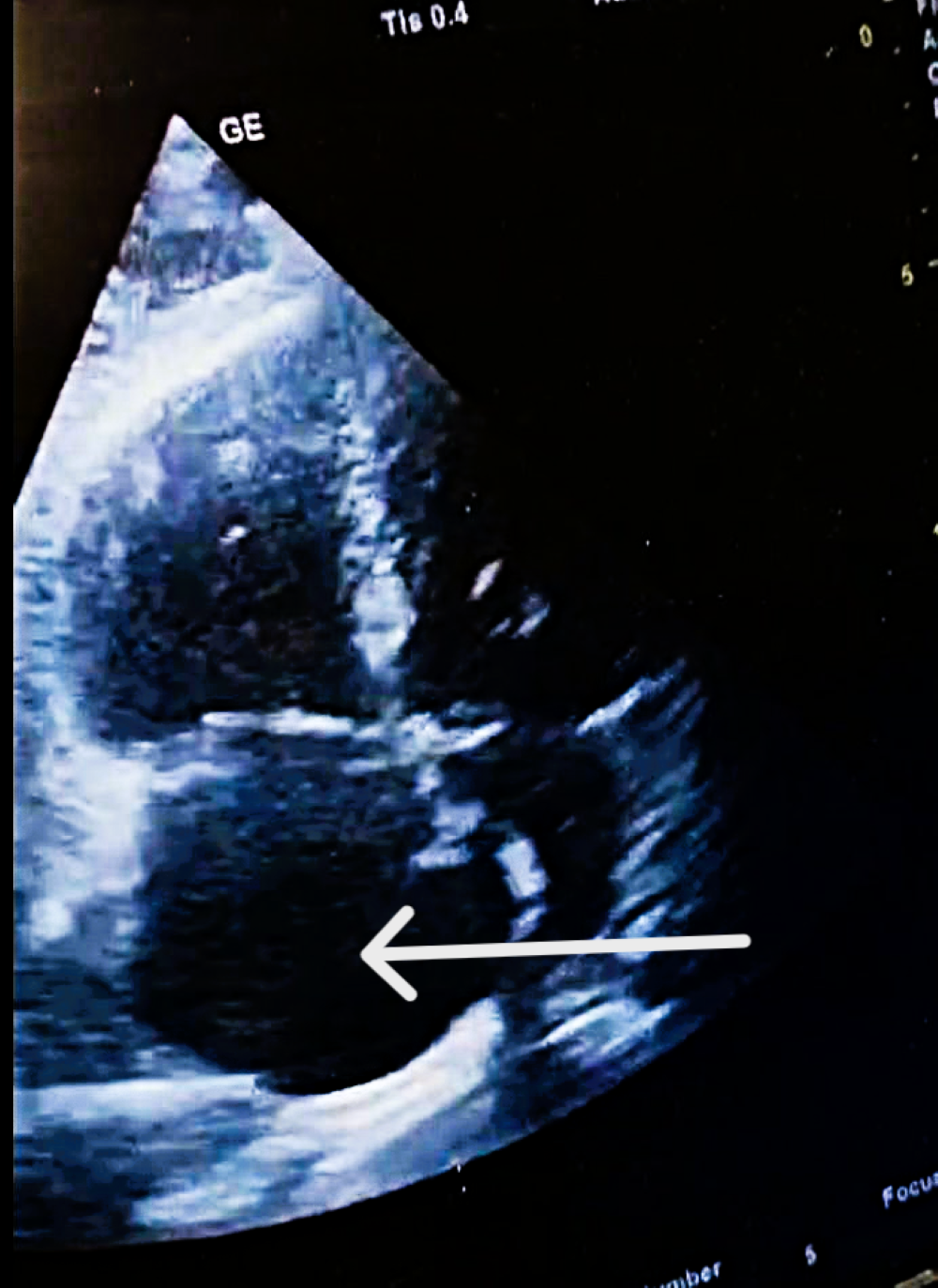
| POCUS-TTE—Parameters, Values and Risk Classification | |||
| RV/LV ratio | 1.39 | high | Intermediate-high-risk |
| TAPSE (mm) | 12 | low | Intermediate-high-risk |
| Parameter | Measurement | Interpretation |
|---|---|---|
| RV diameter | 46 mm (below tricuspid/pulmonary annulus) | Marked RV dilation |
| LV diameter | 33 mm | Normal size |
| RV/LV ratio | >1 | Consistent with acute RV pressure overload |
| RA size | Dilated | Elevated right-sided pressures |
| Pulmonary trunk diameter | 31 mm | Mild dilation; acute pulmonary hypertension |
| Tricuspid regurgitation, Vmax | 3.2 m/s | Increased RV pressure |
| RV—RA gradient | 40 mmHg | Significant RV overload |
| TAPSE | 12 mm | Markedly reduced RV systolic function |
| IVC | 19 mm, <50% collapse | Elevated RA pressure |
| Interventricular septum | Paradoxical motion | “D-shaped” LV; RV overload |
| Mobile RA thrombus | Large, serpentine, prolapsing through tricuspid | High embolic risk |
| Proximal DVT end | Lower third of superficial femoral vein | Non-adherent, unstable |
| Thrombus mobility | Free-floating, unstable | High embolization potential |
| Popliteal vein thrombosis | Nearly occlusive thrombus | Consistent with acute DVT |
| DVT extension | Distal into medial posterior tibial vein | Reflects propagation of DVT |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Golea, A.; Tat, R.M.; Adam, C.; Luka, S.; Stoia, M.A.; Vesa, Ș.C. Ultrasound Images That Speak: Assessing the Therapeutic Decision in the Emergency Department Regarding the Risk–Benefit Ratio of Systemic Thrombolysis in Intermediate-High-Risk Pulmonary Embolism—A Case Report. Diagnostics 2026, 16, 48. https://doi.org/10.3390/diagnostics16010048
Golea A, Tat RM, Adam C, Luka S, Stoia MA, Vesa ȘC. Ultrasound Images That Speak: Assessing the Therapeutic Decision in the Emergency Department Regarding the Risk–Benefit Ratio of Systemic Thrombolysis in Intermediate-High-Risk Pulmonary Embolism—A Case Report. Diagnostics. 2026; 16(1):48. https://doi.org/10.3390/diagnostics16010048
Chicago/Turabian StyleGolea, Adela, Raluca Mihaela Tat, Carina Adam, Sonia Luka, Mirela Anca Stoia, and Ștefan Cristian Vesa. 2026. "Ultrasound Images That Speak: Assessing the Therapeutic Decision in the Emergency Department Regarding the Risk–Benefit Ratio of Systemic Thrombolysis in Intermediate-High-Risk Pulmonary Embolism—A Case Report" Diagnostics 16, no. 1: 48. https://doi.org/10.3390/diagnostics16010048
APA StyleGolea, A., Tat, R. M., Adam, C., Luka, S., Stoia, M. A., & Vesa, Ș. C. (2026). Ultrasound Images That Speak: Assessing the Therapeutic Decision in the Emergency Department Regarding the Risk–Benefit Ratio of Systemic Thrombolysis in Intermediate-High-Risk Pulmonary Embolism—A Case Report. Diagnostics, 16(1), 48. https://doi.org/10.3390/diagnostics16010048







