Is It Wise to Forget Exercise Stress Echocardiography in the Study of Chest Pain in Children? Comment on Huang, S.-W.; Liu, Y.-K. Pediatric Chest Pain: A Review of Diagnostic Tools in the Pediatric Emergency Department. Diagnostics 2024, 14, 526
Informed Consent Statement
Conflicts of Interest
References
- Huang, S.-W.; Liu, Y.-K. Pediatric Chest Pain: A Review of Diagnostic Tools in the Pediatric Emergency Department. Diagnostics 2024, 14, 526. [Google Scholar] [CrossRef]
- Verghese, G.R.; Friedman, K.G.; Rathod, R.H.; Meiri, A.; Saleeb, S.F.; Graham, D.A.; Geggel, R.L.; Fulton, D.R. Resource Utilization Reduction for Evaluation of Chest Pain in Pediatrics Using a Novel Standardized Clinical Assessment and Management Plan (SCAMP). J. Am. Heart Assoc. 2012, 1, jah3-e000349. [Google Scholar] [CrossRef]
- Saleeb, S.F.; McLaughlin, S.R.; Graham, D.A.; Friedman, K.G.; Fulton, D.R. Resource reduction in pediatric chest pain: Standardized clinical assessment and management plan. Congenit. Heart Dis. 2018, 13, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Kane, D.A.; Friedman, K.G.; Fulton, D.R.; Geggel, R.L.; Saleeb, S.F. Needles in Hay II: Detecting Cardiac Pathology by the Pediatric Chest Pain Standardized Clinical Assessment and Management Plan. Congenit. Heart Dis. 2016, 11, 396–402. [Google Scholar] [CrossRef]
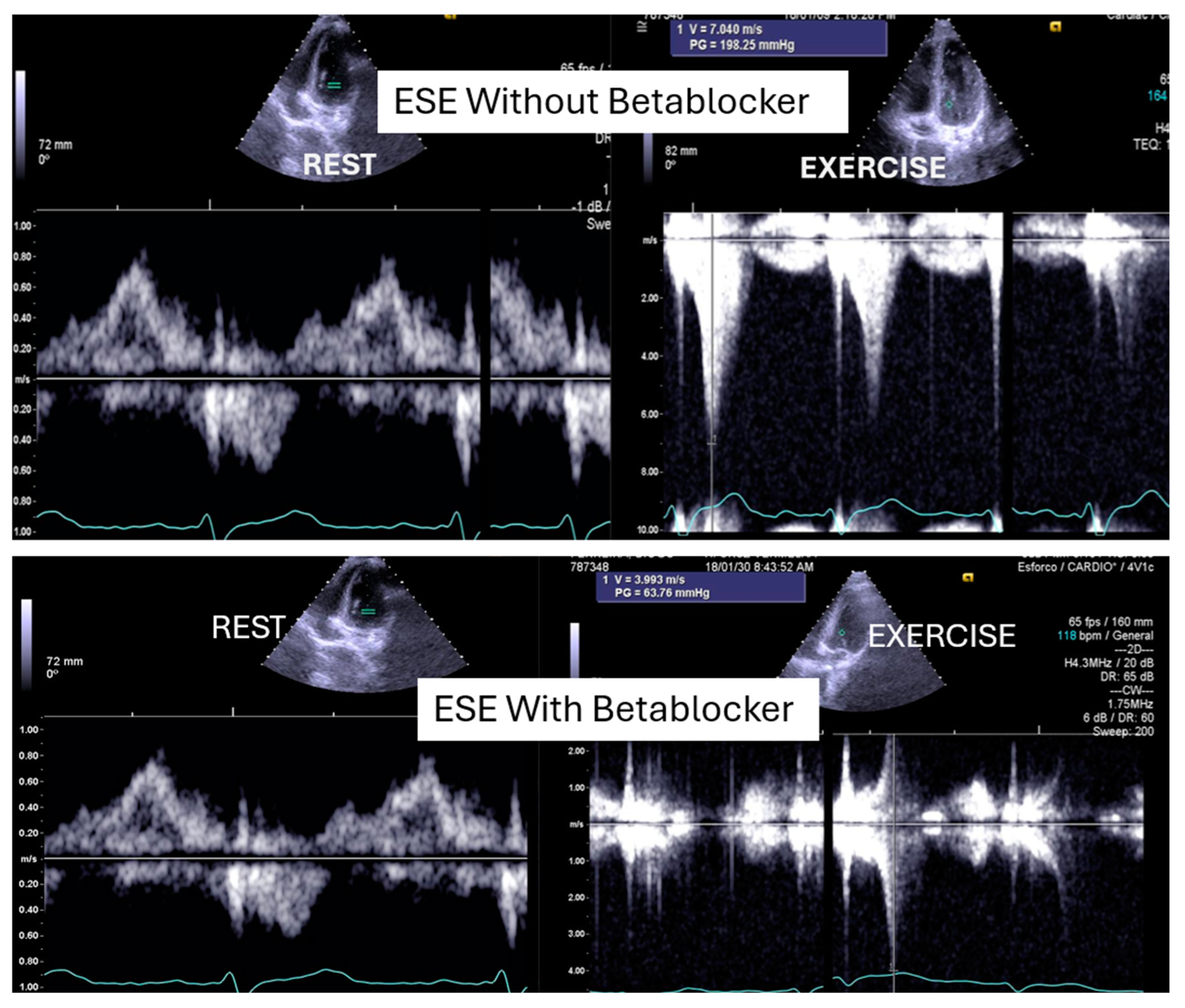
- Cotrim, C.; Palinkas, E.D.; Cotrim, N. The Importance of Left Ventricular Outflow Tract and Mid-Ventricular Gradients in Stress Echocardiography: A Narrative Review. J. Clin. Med. 2023, 12, 5292. [Google Scholar] [CrossRef] [PubMed]
- Cotrim, C.; Picano, E. Step G for Gradients in Stress Echocardiography. In Stress Echocardiography; Picano, E., Ed.; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
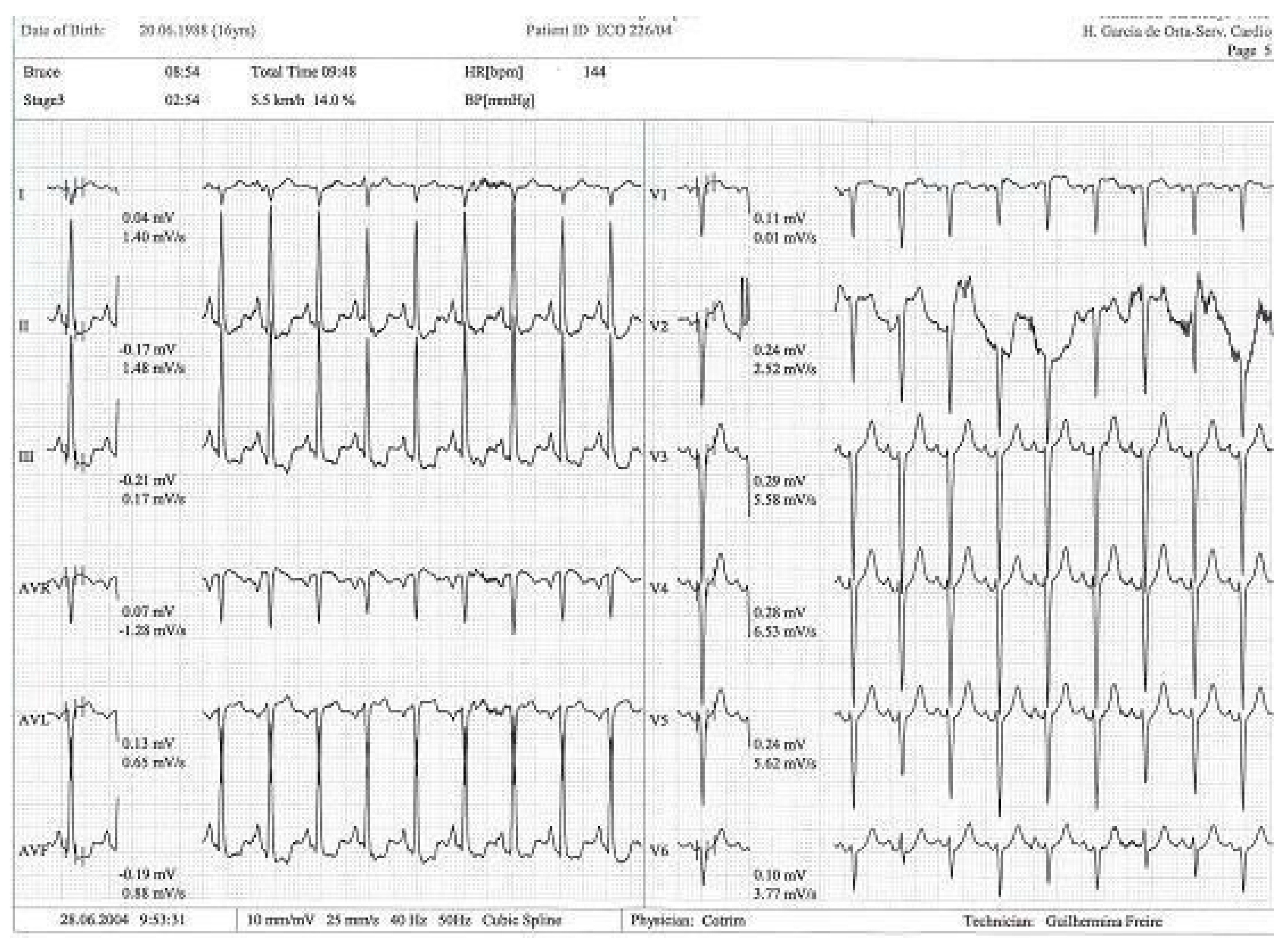
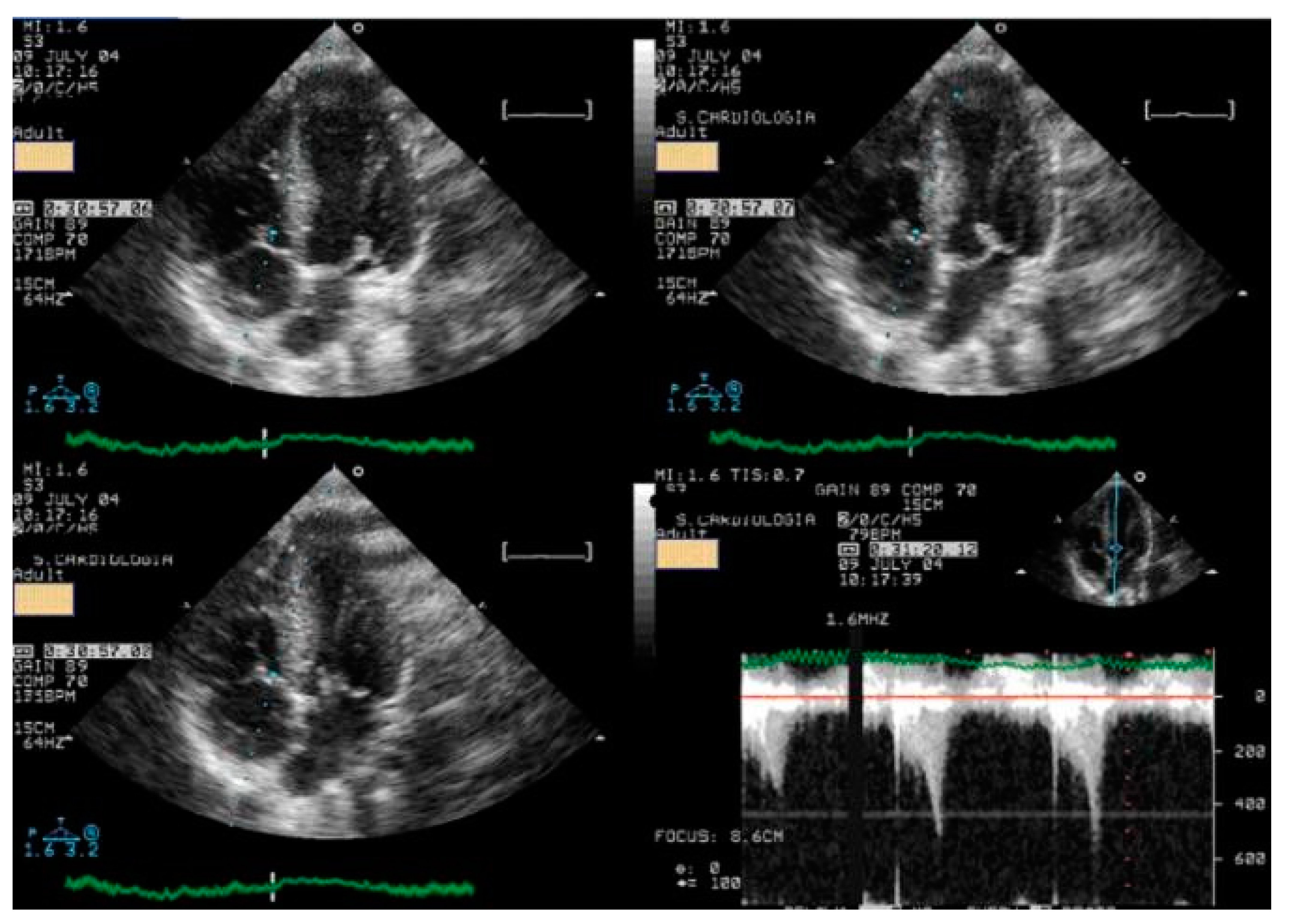
- Lopes, A.; Cotrim, C.; Martins, J.D.; Pinto, F. Exercise-induced intraventricular obstruction in a child with near syncope and chest pain during exercise. Pediatr. Cardiol. 2011, 32, 1032–1035. [Google Scholar] [CrossRef]
- Cotrim, N.; Café, H.M.; Guardado, J.; Cordeiro, P.; Cotrim, H.; Martins, R.; Baquero, L.; Cotrim, C. Clinical Application of Exercise Stress Echocardiography in an Outpatient Pediatric Population. J. Clin. Med. 2024, 13, 2191. [Google Scholar] [CrossRef] [PubMed]
- Cotrim, C.; Almeida, A.G.; Carrageta, M. Exercise-induced intra-ventricular gradients as a frequent potential cause of myocardial ischemia in cardiac syndrome X patients. Cardiovasc. Ultrasound. 2008, 6, 3. [Google Scholar] [CrossRef]
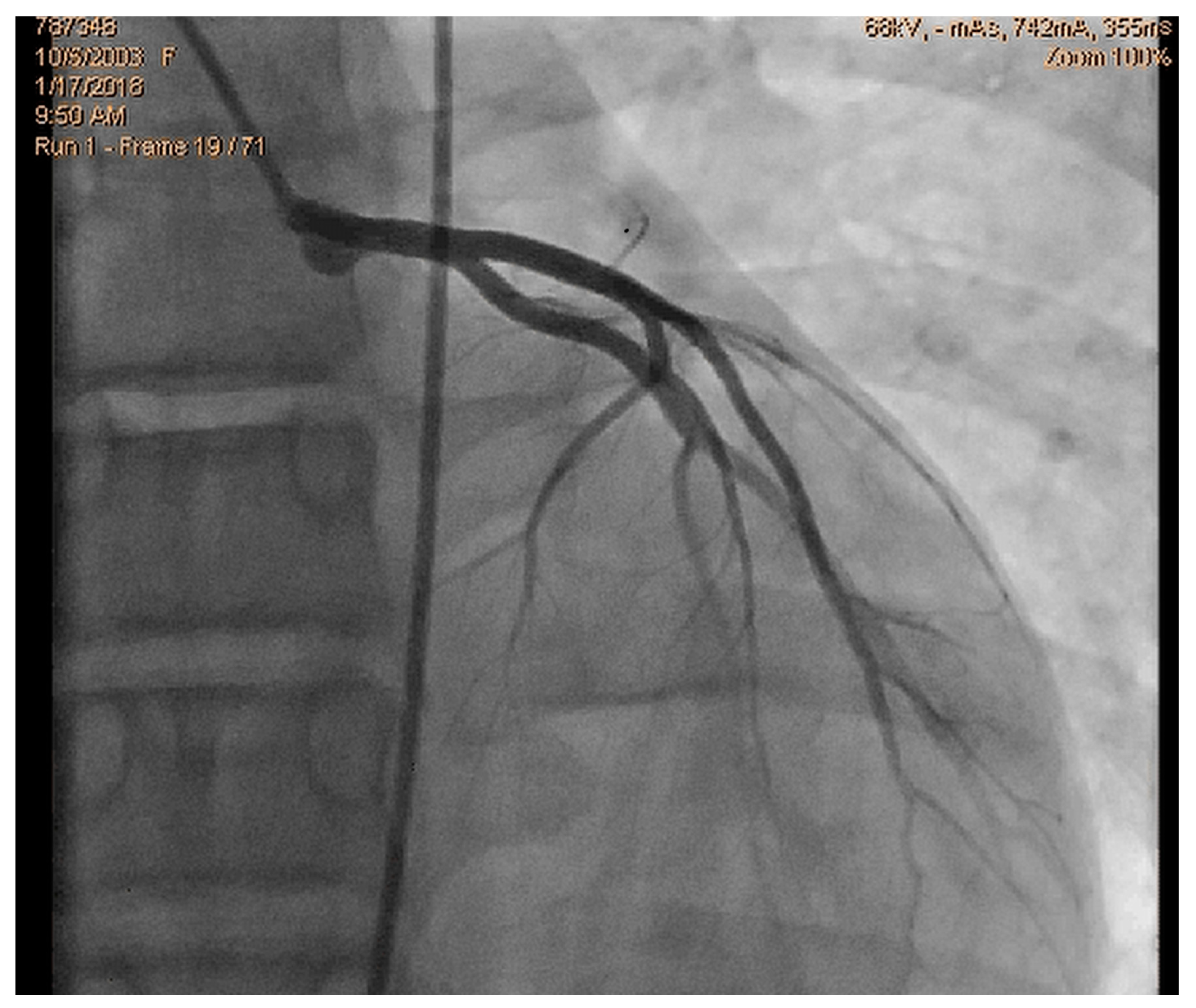
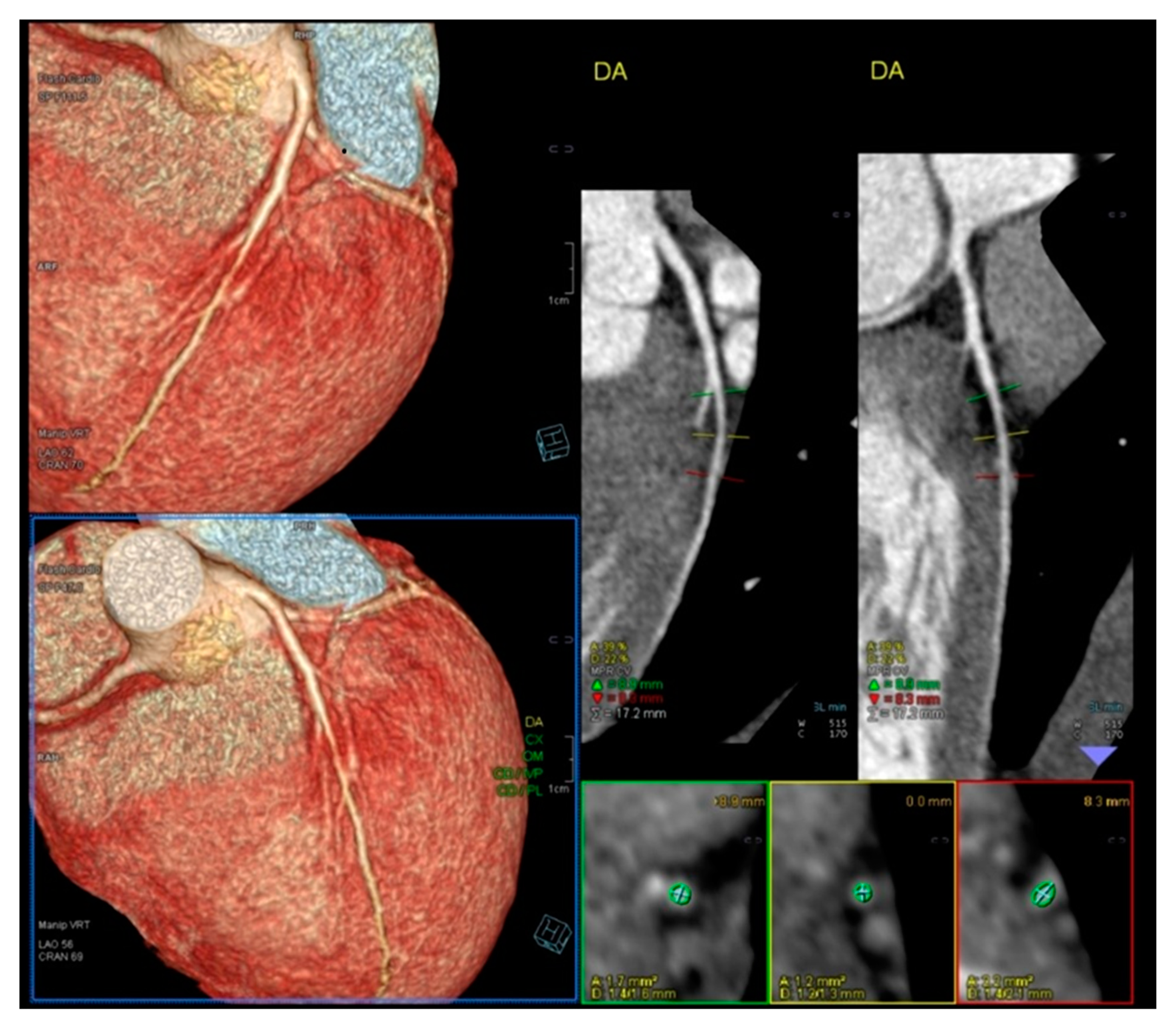
- Cotrim, N.; Castilho, B.; Cotrim, C.; Guardado, J.; Baquero, L. An Unexpected Finding in an Adolescent Rowing Athlete With Angina Pectoris—A Case Report. Clin. J. Sport Med. 2024, 35, 242–245. [Google Scholar] [CrossRef]
- Lopes, L.R.; Cotrim, C.; Cruz, I.; Picano, E.; Pinto, F.; Pereira, H. Left ventricular outflow tract obstruction as a primary phenotypic expression of hypertrophic cardiomyopathy in mutation carriers without hypertrophy. Int. J. Cardiol. 2014, 176, 1264–1267. [Google Scholar] [CrossRef]
- Cotrim, C.; Almeida, A.R.; Miranda, R.; Almeida, A.G.; Cotrim, H.; Picano, E.; Carrageta, M. Stress-induced intraventricular gradients in symptomatic athletes during upright exercise continuous wave Doppler echocardiography. Am. J. Cardiol. 2010, 106, 1808–1812. [Google Scholar] [CrossRef] [PubMed]
- Cotrim, C.; Lopes, L.R.; Almeida, A.R.; Miranda, R.; Ana, A.G.; Cotrim, H.; Andrade, J.P.; Carrageta, M. Efficacy of beta-blocker therapy in symptomatic athletes with exercise-induced intra-ventricular gradients. Cardiovasc. Ultrasound. 2010, 8, 38. [Google Scholar] [CrossRef] [PubMed]
- Cotrim, C.; Almeida, A.G.; Carrageta, M. Clinical significance of intraventricular gradient during effort in an adolescent karate player. Cardiovasc. Ultrasound. 2007, 5, 39. [Google Scholar] [CrossRef]
- Cabrera-Bueno, F.; Gómez-Doblas, J.J.; Muñoz-García, A.; García-Pinilla, J.M.; Navarro, M.J.; de Teresa-Galván, E. Effort angina, normal coronary angiogram, and dynamic left ventricular obstruction. J. Am. Soc. Echocardiogr. 2007, 20, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Coleman, J.A.; Ashkir, Z.; Raman, B.; Bueno-Orovio, A. Mechanisms and prognostic impact of myocardial ischemia in hypertrophic cardiomyopathy. Int. J. Cardiovasc. Imaging. 2023, 39, 1979–1996. [Google Scholar] [CrossRef]
- Walton, M.; Wagner, J.B. Pediatric Beta Blocker Therapy: A Comprehensive Review of Development and Genetic Variation to Guide Precision-Based Therapy in Children, Adolescents, and Young Adults. Genes 2024, 15, 379. [Google Scholar] [CrossRef]
- Schranz, D. Can Pediatric Heart Failure Therapy Be Improved? Yes, It Can, But…. Paediatr. Drugs. 2022, 24, 567–571. [Google Scholar] [CrossRef]
- Cabrera-Bueno, F.; García-Pinilla, J.M.; Gómez-Doblas, J.J.; Montiel-Trujillo, A.; Rodríguez-Bailón, I.; de Teresa-Galván, E. Beta-blocker therapy for dynamic left ventricular outflow tract obstruction induced by exercise. Int. J. Cardiol. 2007, 117, 222–226. [Google Scholar] [CrossRef]
- Lau, T.K.; Navarijo, J.; Stainback, R.F. Pseudo-False-Positive exercise treadmill testing. Tex Heart Inst. J. 2001, 28, 308–311. [Google Scholar]
- Al-Nasser, F.; Duncan, A.; Sharma, R.; O’Sullivan, C.; Coats, A.J.S.; Anker, S.D.; Henein, M.Y. Beta-blocker therapy for dynamic left-ventricular outflow tract obstruction. Int. J. Cardiol. 2002, 86, 199–205. [Google Scholar] [CrossRef]
- Östman-Smith, I.; Wettrell Göran Riesenfelf, T. A cohort study of childhood hypertrophic cardiomyopathy. Improved survival following high-dose beta-adrenoceptor antagonist treatment. J. Am. Coll. Cardiol. 1999, 34, 1813–1822. [Google Scholar] [CrossRef] [PubMed]
- Ommen, S.R.; Ho, C.Y.; Asif, I.M.; Balaji, S.; Burke, M.A.; Day, S.M.; Dearani, J.A.; Epps, K.C.; Evanovich, L.; Ferrari, V.A.; et al. 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR Guideline for the Management of Hypertrophic Cardiomyopathy: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2024, 149, e1239–e1311, Erratum in Circulation 2024, 150, e198. https://doi.org/10.1161/CIR.0000000000001277. [Google Scholar] [CrossRef] [PubMed]
- Nanni, U.; Ferroni, P.; Riondino, S.; Spila, A.; Valente, M.G.; Del Monte, G.; Roselli, M.; Guadagni, F. Convention for the Protection of Human Rights and Dignity of the Human Being with Regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine. J. Med. Philos. 2000, 25, 259–266. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cotrim, N.; Cotrim, C. Is It Wise to Forget Exercise Stress Echocardiography in the Study of Chest Pain in Children? Comment on Huang, S.-W.; Liu, Y.-K. Pediatric Chest Pain: A Review of Diagnostic Tools in the Pediatric Emergency Department. Diagnostics 2024, 14, 526. Diagnostics 2025, 15, 1106. https://doi.org/10.3390/diagnostics15091106
Cotrim N, Cotrim C. Is It Wise to Forget Exercise Stress Echocardiography in the Study of Chest Pain in Children? Comment on Huang, S.-W.; Liu, Y.-K. Pediatric Chest Pain: A Review of Diagnostic Tools in the Pediatric Emergency Department. Diagnostics 2024, 14, 526. Diagnostics. 2025; 15(9):1106. https://doi.org/10.3390/diagnostics15091106
Chicago/Turabian StyleCotrim, Nuno, and Carlos Cotrim. 2025. "Is It Wise to Forget Exercise Stress Echocardiography in the Study of Chest Pain in Children? Comment on Huang, S.-W.; Liu, Y.-K. Pediatric Chest Pain: A Review of Diagnostic Tools in the Pediatric Emergency Department. Diagnostics 2024, 14, 526" Diagnostics 15, no. 9: 1106. https://doi.org/10.3390/diagnostics15091106
APA StyleCotrim, N., & Cotrim, C. (2025). Is It Wise to Forget Exercise Stress Echocardiography in the Study of Chest Pain in Children? Comment on Huang, S.-W.; Liu, Y.-K. Pediatric Chest Pain: A Review of Diagnostic Tools in the Pediatric Emergency Department. Diagnostics 2024, 14, 526. Diagnostics, 15(9), 1106. https://doi.org/10.3390/diagnostics15091106






