Advanced Doppler Ultrasound Insights: A Multicenter Prospective Study on Healthy Skin
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ultrasound Evaluation
2.3. Study Population
2.4. Duration of the Study
2.5. Statistical Analysis
3. Results
4. Discussion
5. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wortsman, X. Top Advances in Dermatologic Ultrasound. J. Ultrasound Med. 2023, 4, 521–545. [Google Scholar] [CrossRef] [PubMed]
- Janowska, A.; Oranges, T.; Granieri, G.; Romanelli, M.; Fidanzi, C.; Iannone, M.; Dini, V. Non-invasive imaging techniques in presurgical margin assessment of basal cell carcinoma: Current evidence. Skin. Res. Technol. 2023, 29, e13271. [Google Scholar] [CrossRef] [PubMed]
- Levy, J.; Barrett, D.L.; Harris, N.; Jeong, J.J.; Yang, X.; Chen, S.C. High-frequency ultrasound in clinical dermatology: A review. Ultrasound J. 2021, 13, 24. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, J.; Maschke, J.; Winkelmann, A.; Schwürzer-Voit, M.; Jenderka, K.V. Conventional ultrasound diagnostics in dermatology. Dermatol. Heidelb. Ger. 2022, 73, 563–574. [Google Scholar] [CrossRef]
- Reginelli, A.; Russo, A.; Berritto, D.; Patane, V.; Cantisani, C.; Grassi, R. Ultra-High-Frequency Ultrasound: A Modern Diagnostic Technique for Studying Melanoma. Ultraschall Med. 2023, 44, 360–378. [Google Scholar] [CrossRef]
- Giavedoni, P.; Podlipnik, S.; Fuertes de Vega, I.; Iranzo, P.; Mascaró, J.M. High-Frequency Ultrasound to Assess Activity in Connective Tissue Panniculitis. J. Clin. Med. 2021, 10, 4516. [Google Scholar] [CrossRef]
- Vargas-Mora, P.; Morgado-Carrasco, D.; Giavedoni, P. Usefulness of high-resolution ultrasound in the management of facial inflammatory dermatoses. Int. J. Dermatol. 2020, 59, e402–e404. [Google Scholar] [CrossRef] [PubMed]
- Olsen, L.O.; Takiwaki, H.; Serup, J. High-frequency ultrasound characterization of normal skin. Skin thickness and echographic density of 22 anatomical sites. Skin. Res. Technol. 1995, 1, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Wortsman, X. Dermatologic Ultrasound with Clinical and Histologic Correlations. In Softcover Reprint of the Original, 1st ed.; Springer: Berlin, Germany, 2013. [Google Scholar]
- Liu, Z.; Niu, Z.; Zhang, D.; Liu, J.; Zhu, Q. Improve the dupilumab therapy evaluation with dermoscopy and high-frequency ultrasound in moderate-to-severe atopic dermatitis. Ski. Res. Technol. 2023, 29, e3260. [Google Scholar] [CrossRef] [PubMed]
- Laverde-Saad, A.; Simard, A.; Nassim, D.; Jfri, A.; Alajmi, A.; O’Brien, E.; Wortsman, X. Performance of Ultrasound for Identifying Morphological Characteristics and Thickness of Cutaneous Basal Cell Carcinoma: A Systematic Review. Dermatology 2022, 238, 692–710. [Google Scholar] [CrossRef]
- Giavedoni, P.; Pousa-Martínez, M.; Estany-Destal, A.; Ginarte, M.; Vázquez-Veiga, H.; Tamez, L.; Mascaró, J.M., Jr. Usefulness of high-frequency Doppler ultrasound skin thickness measurement for disease staging and assessing treatment response in patients with scleredema: A case-control study. J. Am. Acad. Dermatol. 2022, 86, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Bandera, A.I.; Sebaratnam, D.F.; Wargon, O.; Wong, L.C.F. Infantile hemangioma. Part 1: Epidemiology, pathogenesis, clinical presentation and assessment. J. Am. Acad. Dermatol. 2021, 85, 1379–1392. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Bandera, A.I.; Sebaratnam, D.F.; Feito Rodríguez, M.; de Lucas Laguna, R. Cutaneous ultrasound and its utility in Pediatric Dermatology: Part II-Developmental anomalies and vascular lesions. Pediatr. Dermatol. 2020, 37, 40–51. [Google Scholar] [CrossRef]
- Halip, I.A.; Vâţă, D.; Statescu, L.; Salahoru, P.; Patraşcu, A.I.; Temelie Olinici, D.; Tarcau, B.; Popescu, I.A.; Mocanu, M.; Constantin, A.M.; et al. Assessment of Basal Cell Carcinoma Using Dermoscopy and High Frequency Ultrasound Examination. Diagnostics 2022, 12, 735. [Google Scholar] [CrossRef]
- Gimeno-Ribes, M.E.; Toll, A.; Garcia, A.; Giavedoni, P. Usefulness of High-Frequency Doppler Ultrasound in Dermatofibrosarcoma Protuberans: A Retrospective Case Series. J. Ultrasound Med. 2023, 42, 2171–2173. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.Q.; Wang, L.F.; Li, X.L.; Wang, Q.; Li, M.X.; Ma, Y.Y.; Xiang, L.H.; Guo, L.H.; Xu, H.X. High-frequency ultrasound in the diagnosis of the spectrum of cutaneous squamous cell carcinoma: Noninvasively distinguishing actinic keratosis, Bowen’s Disease, and invasive squamous cell carcinoma. Skin. Res. Technol. 2021, 27, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Belfiore, M.P.; Reginelli, A.; Russo, A.; Russo, G.M.; Rocco, M.P.; Moscarella, E.; Ferrante, M.; Sica, A.; Grassi, R.; Cappabianca, S. Usefulness of High-Frequency Ultrasonography in the Diagnosis of Melanoma: Mini Review. Front. Oncol. 2021, 11, 673026. [Google Scholar] [CrossRef]
- Xiong, Y.Q.; Ma, S.J.; Mo, Y.; Huo, S.T.; Wen, Y.Q.; Chen, Q. Comparison of dermoscopy and reflectance confocal microscopy for the diagnosis of malignant skin tumours: A meta-analysis. J. Cancer Res. Clin. Oncol. 2017, 143, 1627–1635. [Google Scholar] [CrossRef]
- Nwaneshiudu, A.; Kuschal, C.; Sakamoto, F.H.; Anderson, R.R.; Schwarzenberger, K.; Young, R.C. Introduction to confocal microscopy. J. Investig. Dermatol. 2012, 132, e3. [Google Scholar] [CrossRef] [PubMed]
- Csuka, E.A.; Ward, S.C.; Ekelem, C.; Csuka, D.A.; Ardigò, M.; Mesinkovska, N.A. Reflectance Confocal Microscopy, Optical Coherence Tomography, and Multiphoton Microscopy in Inflammatory Skin Disease Diagnosis. Lasers Surg. Med. 2021, 53, 776–797. [Google Scholar] [CrossRef] [PubMed]
- Fernando, A.; Laura, N.; Pablo, F.; Gastón, R. Ultrasound-guided fine-needle aspiration biopsy in skin lesions. Skin. Res. Technol. 2019, 25, 399–401. [Google Scholar] [CrossRef]
- López-Llunell, C.; Romaní, J.; Roé, E.; Giavedoni, P.; Vidal, D.; Wortsman, X. Ultrasonographic Patterns of Cutaneous Sarcoidosis. J. Ultrasound Med. 2021, 40, 2521–2526. [Google Scholar] [CrossRef]
- Romaní, J.; Giavedoni, P.; Roé, E.; Vidal, D.; Luelmo, J.; Wortsman, X. Inter- and Intra-rater Agreement of Dermatologic Ultrasound for the Diagnosis of Lobular and Septal Panniculitis. J. Ultrasound Med. 2020, 39, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Marti-Marti, I.; Morgado-Carrasco, D.; Podlipnik, S.; Rizo-Potau, D.; Bosch-Amate, X.; Lledó, G.M.; Suárez-Lledó, M.; Espinosa, G.; Martínez, C.; Mascaró, J.M., Jr.; et al. Usefulness of high-frequency ultrasonography in the evaluation and monitoring of sclerosing dermatoses: A cohort study. Clin. Exp. Dermatol. 2022, 47, 351–358. [Google Scholar] [CrossRef]
- Giavedoni, P.; Martinez, C.; Podlipnik, S.; Suárez-Lleidó, M.; Martí-Martí, I.; Morgado-Carrasco, D.; Rovira, M.; Fernández-Avilés, F.; Gutiérrez, G.; Rosiñol, L.; et al. Assessment of Sclerodermoid Chronic Graft-versus-host Disease with Colour Doppler Ultrasound. Acta. Derm. Venereol. 2021, 10, adv00395. [Google Scholar] [CrossRef] [PubMed]
- Wortsman, X.; Reyes-Baraona, F.; Ramirez-Cornejo, C.; Ferreira-Wortsman, C.; Caposiena Caro, R.D.; Molina-Leyva, A.; Arias-Santiago, S.; Giavedoni, P.; Martorell, A.; Romani, J.; et al. Can Ultrasound Examinations Generate Pain in Hidradenitis Suppurativa Patients? Results from a Multicentric Cross-Sectional Study. Dermatology 2023, 239, 277–282. [Google Scholar] [CrossRef]
- Martorell, A.; Segura Palacios, J.M. Ultrasound examination of hidradenitis suppurativa. Actas. Dermosifiliogr. 2015, 106 (Suppl. S1), 49–59. [Google Scholar] [CrossRef] [PubMed]
- Grand, D.; Frew, J.W.; Navrazhina, K.; Krueger, J.G. Doppler ultrasound-based noninvasive biomarkers in hidradenitis suppurativa: Evaluation of analytical and clinical validity. Br. J. Dermatol. 2021, 184, 688–696. [Google Scholar] [CrossRef]
- Costa, I.M.C.; Pompeu, C.B.; Mauad, E.B.S.; Costa, M.C.; Guimarães de Freitas Lima, V.; Pompeu, M.F.; Tinoco Regattieri, N.A. High-frequency ultrasound as a non-invasive tool in predicting early hidradenitis suppurativa fistulization in comparison with the Hurley system. Skin. Res. Technol. 2021, 27, 291–292. [Google Scholar] [CrossRef]
| Ultrasound Technician Expertise | |
|---|---|
| In training | 7 (58.4%) |
| Expert | 5 (41.6%) |
| Years of experience | 4.0 (3.0–7.0) |
| Reason for Dermatology visit | |
| Skin disease | 1 (0.7%) |
| Healthy volunteer | 151 (99%) |
| Axillary temperature °C | 36.20 (35.95–36.50) |
| Room temperature °C | 24 (23–24) |
| Gender | |
| Female | 107 (70%) |
| Male | 45 (30%) |
| Weight | 63 (55–73) |
| Age | 35 (27–52) |
| Ethnic | |
| African American | 3 (2.0%) |
| Caucasians | 149 (98%) |
| Phototype | |
| I | 6 (4.0%) |
| II | 40 (27%) |
| III | 85 (57%) |
| IV | 17 (11%) |
| V | 1 (0.7%) |
| Smokers (packs/year) | |
| 0 | 126 (83%) |
| 0–10 | 20 (13%) |
| 10–20 | 2 (1.3%) |
| >20 | 4 (2.6%) |
| Actinic damage | |
| I | 117 (77%) |
| II | 30 (20%) |
| III | 5 (3%) |
| No pathological history | 139 (91.4%) |
| Arterial hypertension | 11 (7.2%) |
| Type II diabetes mellitus | 1 (0.7%) |
| Chronic renal failure | 1 (0.7%) |
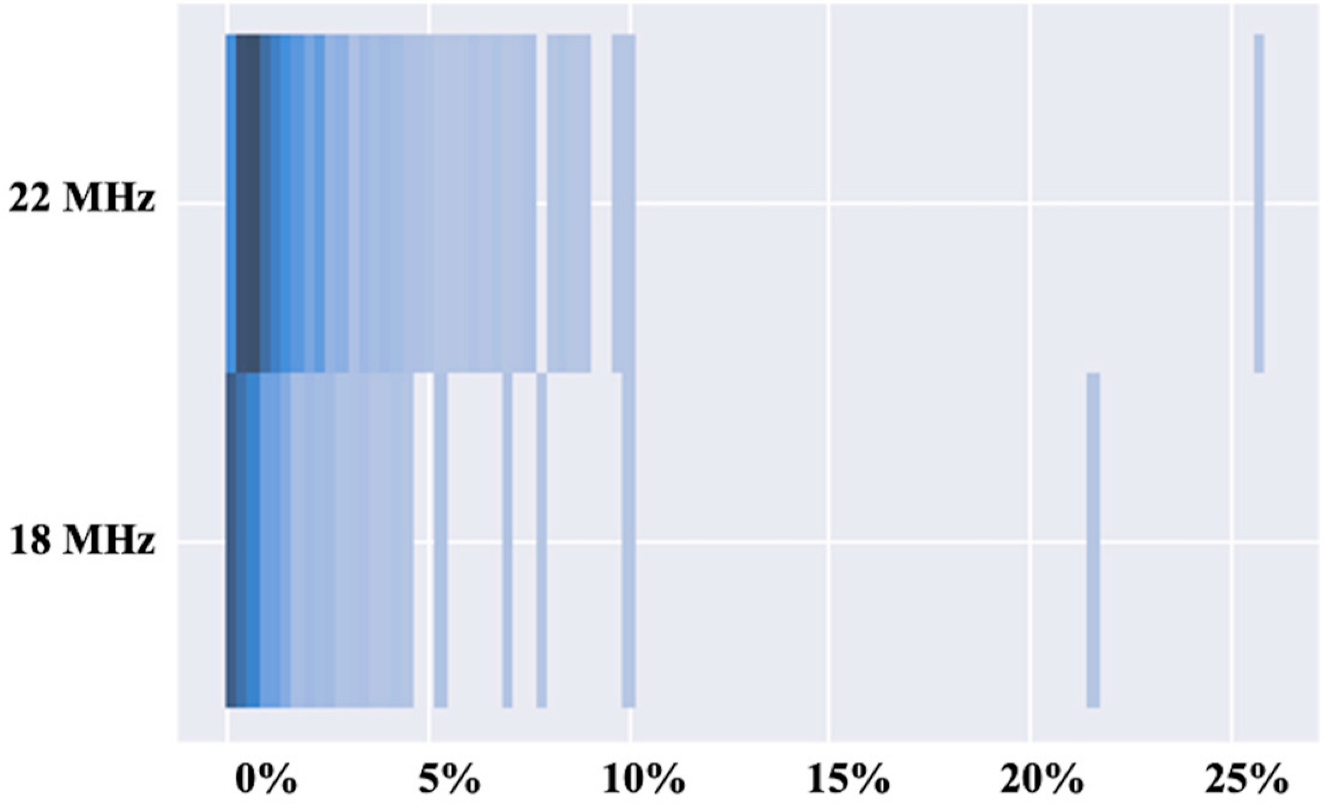
| 18 MHz Probe N = 67 | 22 MHz Probe N = 105 | |
|---|---|---|
| Doppler Type | ||
| Color | 35 (52%) | 71 (68%) |
| Power | 32 (48%) | 34 (32%) |
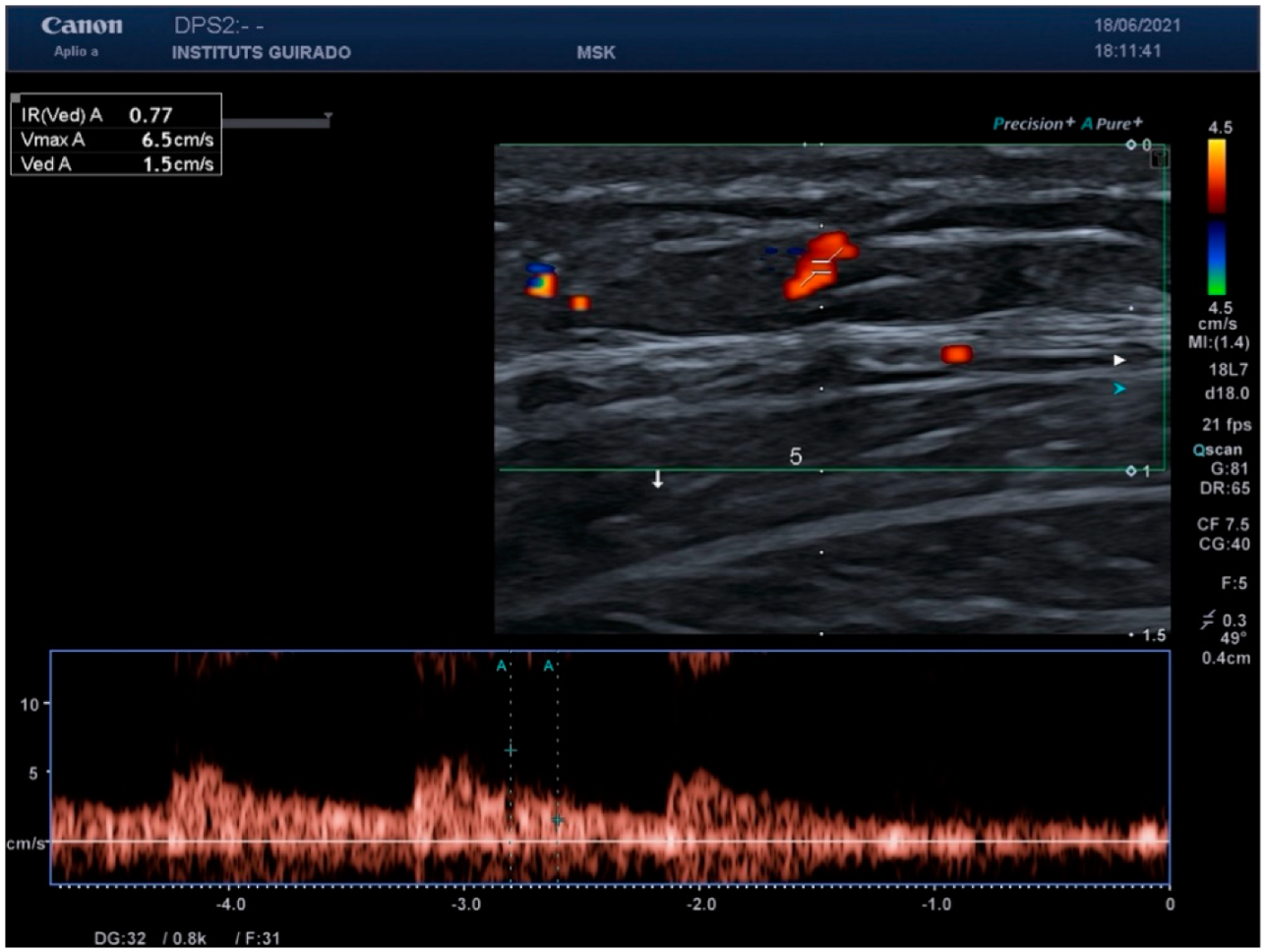
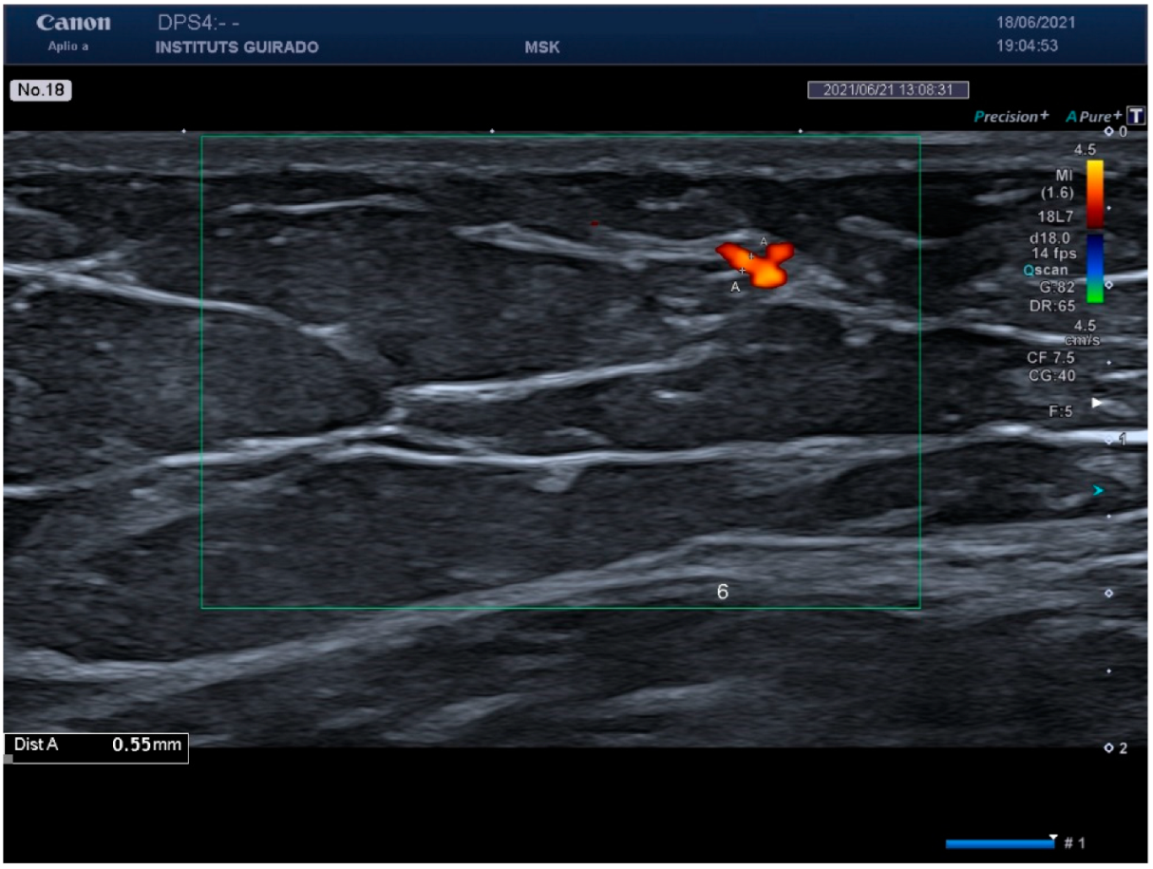
| Nasolabial fold | ||
| Peak systolic (cm/s) | 6.5 (5.7–8.8) | 4.6 (3.5–6.8) |
| Resistance index | 0.71 (0.67–0.74) | 0.68 (0.59–0.75) |
| Vessel diameter (mm) | 0.78 (0.58–0.99) | 0.52 (0.37–0.78) |
| Malar region | ||
| Peak systolic (cm/s) | 2.80 (1.55–3.30) | 1.60 (0.90–2.60) |
| Resistance index | 0.73 (0.68–0.75) | 0.70 (0.60–0.80) |
| Vessel diameter (mm) | 0.53 (0.45–0.59) | 0.46 (0.36–0.65) |
| Flank | ||
| Peak systolic (cm/s) | 8.4 (6.8–9.5) | 4.7 (3.7–6.2) |
| Resistance index | 0.70 (0.65–0.74) | 0.67 (0.60–0.80) |
| Vessel diameter (mm) | 0.78 (0.44–0.95) | 0.48 (0.34–0.67) |
| Thigh | ||
| Peak systolic (cm/s) | 8.2 (6.4–9.9) | 5.0 (4.1–6.4) |
| Resistance index | 0.73 (0.69–0.80) | 0.68 (0.58–0.73) |
| Vessel diameter (mm) | 0.66 (0.52–0.81) | 0.53 (0.38–0.77) |
| Neckline | ||
| Peak systolic (cm/s) | 6.6 (5.5–7.6) | 4.2 (3.2–6.3) |
| Resistance index | 0.75 (0.70–0.78) | 0.68 (0.60–0.80) |
| Vessel diameter (mm) | 0.55 (0.47–0.94) | 0.47 (0.37–0.61) |
| Arm | ||
| Peak systolic (cm/s) | 6.30 (4.30–7.45) | 3.70 (2.55–5.03) |
| Resistance index | 0.71 (0.69–0.73) | 0.70 (0.61–0.76) |
| Vessel diameter (mm) | 0.64 (0.43–0.85) | 0.42 (0.33–0.59) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giavedoni, P.; Romaní, J.; de Cabo, F.; García-Martínez, F.J.; Quintana-Codina, M.; Roè-Crespo, E.; Fuertes de Vega, I.; Soria-Gili, X.; Aguayo-Ortiz, R.; Garbayo-Salmons, P.; et al. Advanced Doppler Ultrasound Insights: A Multicenter Prospective Study on Healthy Skin. Diagnostics 2025, 15, 569. https://doi.org/10.3390/diagnostics15050569
Giavedoni P, Romaní J, de Cabo F, García-Martínez FJ, Quintana-Codina M, Roè-Crespo E, Fuertes de Vega I, Soria-Gili X, Aguayo-Ortiz R, Garbayo-Salmons P, et al. Advanced Doppler Ultrasound Insights: A Multicenter Prospective Study on Healthy Skin. Diagnostics. 2025; 15(5):569. https://doi.org/10.3390/diagnostics15050569
Chicago/Turabian StyleGiavedoni, Priscila, Jorge Romaní, Francisco de Cabo, Francisco Javier García-Martínez, Mónica Quintana-Codina, Esther Roè-Crespo, Irene Fuertes de Vega, Xavier Soria-Gili, Rafael Aguayo-Ortiz, Patricia Garbayo-Salmons, and et al. 2025. "Advanced Doppler Ultrasound Insights: A Multicenter Prospective Study on Healthy Skin" Diagnostics 15, no. 5: 569. https://doi.org/10.3390/diagnostics15050569
APA StyleGiavedoni, P., Romaní, J., de Cabo, F., García-Martínez, F. J., Quintana-Codina, M., Roè-Crespo, E., Fuertes de Vega, I., Soria-Gili, X., Aguayo-Ortiz, R., Garbayo-Salmons, P., Castillo, G., Vidal-Sarró, D., Mollet, J., Serra, L., Gonzalez, C., López-Trujillo, E., Just, M., Combalia, M., Podlipnik, S., ... Wortsman, X. (2025). Advanced Doppler Ultrasound Insights: A Multicenter Prospective Study on Healthy Skin. Diagnostics, 15(5), 569. https://doi.org/10.3390/diagnostics15050569








