Transfer of POCUS Skills of Anesthesia Trainees from the Simulation Laboratory to Clinical Practice: A Follow-Up Pilot Evaluation After ABC US Protocol Training
Abstract
:1. Introduction
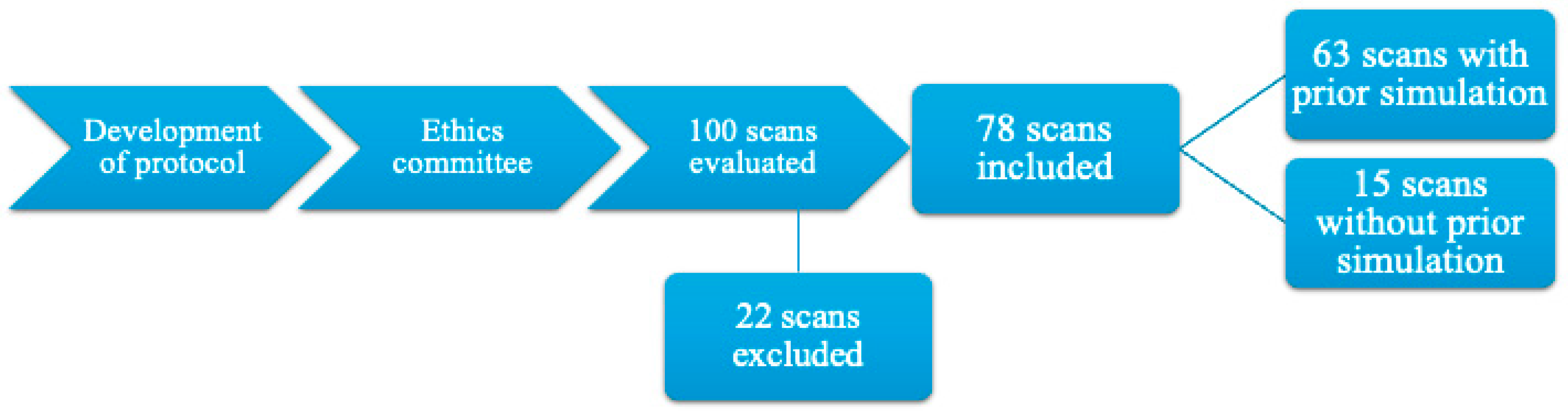
2. Materials and Methods
2.1. Protocol Development
- Point: the trainee cannot correctly use the equipment, does not apply the ultrasound gel, and does not optimize the image regarding depth, gain, and zoom.
- Points: the trainee can correctly use the equipment with assistance.
- Points: the trainee manages to use the equipment with minimum assistance.
- Points: the trainee manages to use the equipment with some assistance; for example, verbal indications on what needs to be optimized.
- Points: the trainee manages to correctly use the equipment without assistance.
- Point: the trainee does not have a structured approach to the examination.
- Points: the trainee has a structured approach with assistance.
- Points: the trainee has a structured approach with minimum assistance, like verbal indications and physical intervention.
- Points: the trainee has a structured approach with some verbal assistance.
- Points: the trainee has a structured approach without any assistance.
- Point: the trainee does not recognize the structures examined.
- Points: the trainee recognizes the structures if explained and shown to them on the screen.
- Points: the trainee recognizes the structures examined with minimal verbal assistance and minimal on-screen indications.
- Points: the trainee recognizes the structures examined with minimal verbal assistance.
- Points: the trainee recognizes the structures examined without assistance.
- Point: the trainee does not manage to establish an ultrasound diagnosis and does not correlate the findings with the clinical status of the patient.
- Points: the trainee manages to partially establish an ultrasound diagnosis and can partially correlate the findings with the clinical status of the patient with assistance.
- Points: the trainee manages to establish an ultrasound diagnosis and can correlate the findings with the clinical status of the patient with minimum assistance.
- Points: the trainee manages to establish an ultrasound diagnosis without proper correlation with the clinical status of the patient without assistance.
- Points: the trainee manages to establish an ultrasound diagnosis and can correlate the findings with the clinical status of the patient without assistance.
- Point: there is a constant need for verbal and physical assistance to perform the scan.
- Points: there is an inconstant need for verbal and physical assistance to perform the scan.
- Points: there is a need for minimum verbal and/or physical assistance to perform the scan.
- Points: there is a need for minimum verbal assistance to perform the scan.
- Points: there is no need for assistance to perform the scan.
2.2. Ethics Committee
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| POCUS | Point-of-care ultrasound |
| ICU | Intensive care unit |
| SBET | Simulation-based education and training |
| ABC | Airway, breathing, and circulation |
References
- Buonsenso, D.; Pata, D.; Chiaretti, A. COVID-19 outbreak: Less stethoscope, more ultrasound. Lancet Respir. Med. 2020, 8, e27. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.Y.; Wang, X.T.; Zhang, L.N.; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020, 46, 849–850. [Google Scholar] [CrossRef]
- Yasukawa, K.; Minami, T. Point-of-Care Lung Ultrasound Findings in Patients with COVID-19 Pneumonia. Am. J. Trop. Med. Hyg. 2020, 102, 1198–1202. [Google Scholar] [CrossRef]
- Kulkarni, S.; Down, B.; Jha, S. Point-of-care lung ultrasound in intensive care during the COVID-19 pandemic. Clin. Radiol. 2020, 75, 710.e1–710.e4. [Google Scholar] [CrossRef]
- Savoldelli, G.L.; Burlacu, C.L.; Lazarovici, M.; Matos, F.M.; Østergaard, D.; Utstein Simulation Study Group. Integration of simulation-based education in anaesthesiology specialist training: Synthesis of results from an Utstein Meeting. Eur. J. Anaesthesiol. 2024, 41, 43–54. [Google Scholar] [CrossRef]
- Simon, R.; Petrișor, C.; Bodolea, C.; Csipak, G.; Oancea, C.; Golea, A. ABC approach proposal for POCUS in COVID-19 critically ill patients. Med. Ultrason. 2021, 23, 94–102. [Google Scholar] [CrossRef]
- Simon, R.; Petrisor, C.; Bodolea, C.; Golea, A.; Gomes, S.H.; Antal, O.; Vasian, H.N.; Moldovan, O.; Puia, C.I. Efficiency of Simulation-Based Learning Using an ABC POCUS Protocol on a High-Fidelity Simulator. Diagnostics 2024, 14, 173. [Google Scholar] [CrossRef]
- Pontet, J.; Yic, C.; Díaz-Gómez, J.L.; Rodriguez, P.; Sviridenko, I.; Méndez, D.; Noveri, S.; Soca, A.; Cancela, M. Impact of an ultrasound-driven diagnostic protocol at early intensive-care stay: A randomized-controlled trial. Ultrasound J. 2019, 11, 24. [Google Scholar] [CrossRef]
- Greenstein, Y.Y.; Littauer, R.; Narasimhan, M.; Mayo, P.H.; Koenig, S.J. Effectiveness of a Critical Care Ultrasonography Course. Chest 2017, 151, 34–40. [Google Scholar] [CrossRef]
- Lichtenstein, D.A. Lung ultrasound in the critically ill. Ann. Intensive Care 2014, 4, 1. [Google Scholar] [CrossRef]
- Lichtenstein, D.A. BLUE-protocol and FALLS-protocol: Two applications of lung ultrasound in the critically ill. Chest 2015, 147, 1659–1670. [Google Scholar] [CrossRef] [PubMed]
- Volpicelli, G.; Elbarbary, M.; Blaivas, M.; Lichtenstein, D.A.; Mathis, G.; Kirkpatrick, A.W.; Melniker, L.; Gargani, L.; Noble, V.E.; Via, G.; et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012, 38, 577–591. [Google Scholar] [CrossRef] [PubMed]
- Volpicelli, G.; Lamorte, A.; Tullio, M.; Cardinale, L.; Giraudo, M.; Stefanone, V.; Boero, E.; Nazerian, P.; Pozzi, R.; Frascisco, M.F. Point-of-care multiorgan ultrasonography for the evaluation of undifferentiated hypotension in the emergency department. Intensive Care Med. 2013, 39, 1290–1298. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.J.; Bechara, R.; Islam, S. Point-of-Care Ultrasound in the Intensive Care Unit. Clin. Chest Med. 2018, 39, 79–97. [Google Scholar] [CrossRef]
- Narasimhan, M.; Koenig, S.J.; Mayo, P.H. A Whole-Body Approach to Point of Care Ultrasound. Chest 2016, 150, 772–776. [Google Scholar] [CrossRef]
- Frankel, H.L.; Kirkpatrick, A.W.; Elbarbary, M.; Blaivas, M.; Desai, H.; Evans, D.; Summerfield, D.T.; Slonim, A.; Breitkreutz, R.; Price, S.; et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part I: General Ultrasonography. Crit. Care Med. 2015, 43, 2479–2502. [Google Scholar] [CrossRef]
- Levitov, A.; Frankel, H.L.; Blaivas, M.; Kirkpatrick, A.W.; Su, E.; Evans, D.; Summerfield, D.T.; Slonim, A.; Breitkreutz, R.; Price, S.; et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part II: Cardiac Ultrasonography. Crit. Care Med. 2016, 44, 1206–1227. [Google Scholar] [CrossRef]
- Robba, C.; Wong, A.; Poole, D.; Al Tayar, A.; Arntfield, R.T.; Chew, M.S.; Corradi, F.; Douflé, G.; Goffi, A.; Lamperti, M.; et al. Basic ultrasound head-to-toe skills for intensivists in the general and neuro intensive care unit population: Consensus and expert recommendations of the European Society of Intensive Care Medicine. Intensive Care Med. 2021, 47, 1347–1367. [Google Scholar] [CrossRef]
- Bataille, B.; Riu, B.; Ferre, F.; Moussot, P.E.; Mari, A.; Brunel, E.; Ruiz, J.; Mora, M.; Fourcade, O.; Genestal, M.; et al. Integrated use of bedside lung ultrasound and echocardiography in acute respiratory failure: A prospective observational study in ICU. Chest 2014, 146, 1586–1593. [Google Scholar] [CrossRef]
- Chen, Z.; Hong, Y.; Dai, J.; Xing, L. Incorporation of point-of-care ultrasound into morning round is associated with improvement in clinical outcomes in critically ill patients with sepsis. J. Clin. Anesth. 2018, 48, 62–66. [Google Scholar] [CrossRef]
- Shorten, G.D.; De Robertis, E.; Goldik, Z.; Kietaibl, S.; Niemi-Murola, L.; Sabelnikovs, O. European Section/Board of Anaesthesiology/European Society of Anaesthesiology consensus statement on competency-based education and training in anaesthesiology. Eur. J. Anaesthesiol. 2020, 37, 421–434. [Google Scholar] [CrossRef] [PubMed]
- Zieleskiewicz, L.; Muller, L.; Lakhal, K.; Meresse, Z.; Arbelot, C.; Bertrand, P.M.; Bouhemad, B.; Cholley, B.; Demory, D.; Duperret, S.; et al. Point-of-care ultrasound in intensive care units: Assessment of 1073 procedures in a multicentric, prospective, observational study. Intensive Care Med. 2015, 41, 1638–1647. [Google Scholar] [CrossRef] [PubMed]
- Killu, K.; Coba, V.; Mendez, M.; Reddy, S.; Adrzejewski, T.; Huang, Y.; Ede, J.; Horst, M. Model Point-of-Care Ultrasound Curriculum in an Intensive Care Unit Fellowship Program and Its Impact on Patient Management. Crit. Care Res. Pract. 2014, 2014, 934796. [Google Scholar] [CrossRef]
- Atkinson, P.R.; Beckett, N.; French, J.; Banerjee, A.; Fraser, J.; Lewis, D. Does Point-of-care Ultrasound Use Impact Resuscitation Length, Rates of Intervention, and Clinical Outcomes During Cardiac Arrest? A Study from the Sonography in Hypotension and Cardiac Arrest in the Emergency Department (SHoC-ED) Investigators. Cureus 2019, 11, e4456. [Google Scholar] [CrossRef]
- Shen, J.; Singh, M.; Tran, T.T.; Bughrara, N.F.; Vo, C.; Sigakis, M.; Nikravan, S.; Tone, R.; Sandhu, C.K.; Kakazu, C.; et al. Assessment of cardiopulmonary point-of-care ultrasound objective structured clinical examinations in graduating anesthesiology residents across multiple residency programs. J. Clin. Anesth. 2023, 91, 111260. [Google Scholar] [CrossRef]
- Jensen, M.B.; Sloth, E.; Larsen, K.M.; Schmidt, M.B. Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. Eur. J. Anaesthesiol. 2004, 21, 700–707. [Google Scholar] [CrossRef]
- Green, M.; Tariq, R.; Green, P. Improving Patient Safety through Simulation Training in Anesthesiology: Where Are We? Anesthesiol. Res. Pract. 2016, 2016, 4237523. [Google Scholar] [CrossRef]
- McLean, D.; Hewitson, L.; Atkinson, P.; Lewis, D.; Fraser, J.; Verheul, G.; Mekwan, J.; Robinson, B. ULTRASIM: Ultrasound in trauma simulation. Can. J. Emerg. Med. 2019, 21, 125–128. [Google Scholar] [CrossRef]
- Wang, H.; Uraco, A.M.; Stover, J.; Hollis, N. Novel 4W (When-Where-What-What) Approach of Training Point-of-Care Ultrasound (POCUS) Application in Resuscitation with High-Fidelity Simulator. Cureus 2020, 12, e9353. [Google Scholar] [CrossRef]
- Zeng, Q.; Wang, K.; Liu, W.X.; Zeng, J.Z.; Li, X.L.; Zhang, Q.F.; Ren, S.Q.; Xu, W.M. Efficacy of high-fidelity simulation in advanced life support training: A systematic review and meta-analysis of randomized controlled trials. BMC Med. Educ. 2023, 23, 664. [Google Scholar] [CrossRef]
- Takeda, K.; Kasai, H.; Tajima, H.; Hayama, N.; Saito, M.; Kawame, C.; Suzuki, T. Effectiveness of Lung Ultrasound Training Utilizing a High-Fidelity Simulator. ATS Sch. 2023, 5, 133–141. [Google Scholar] [CrossRef]
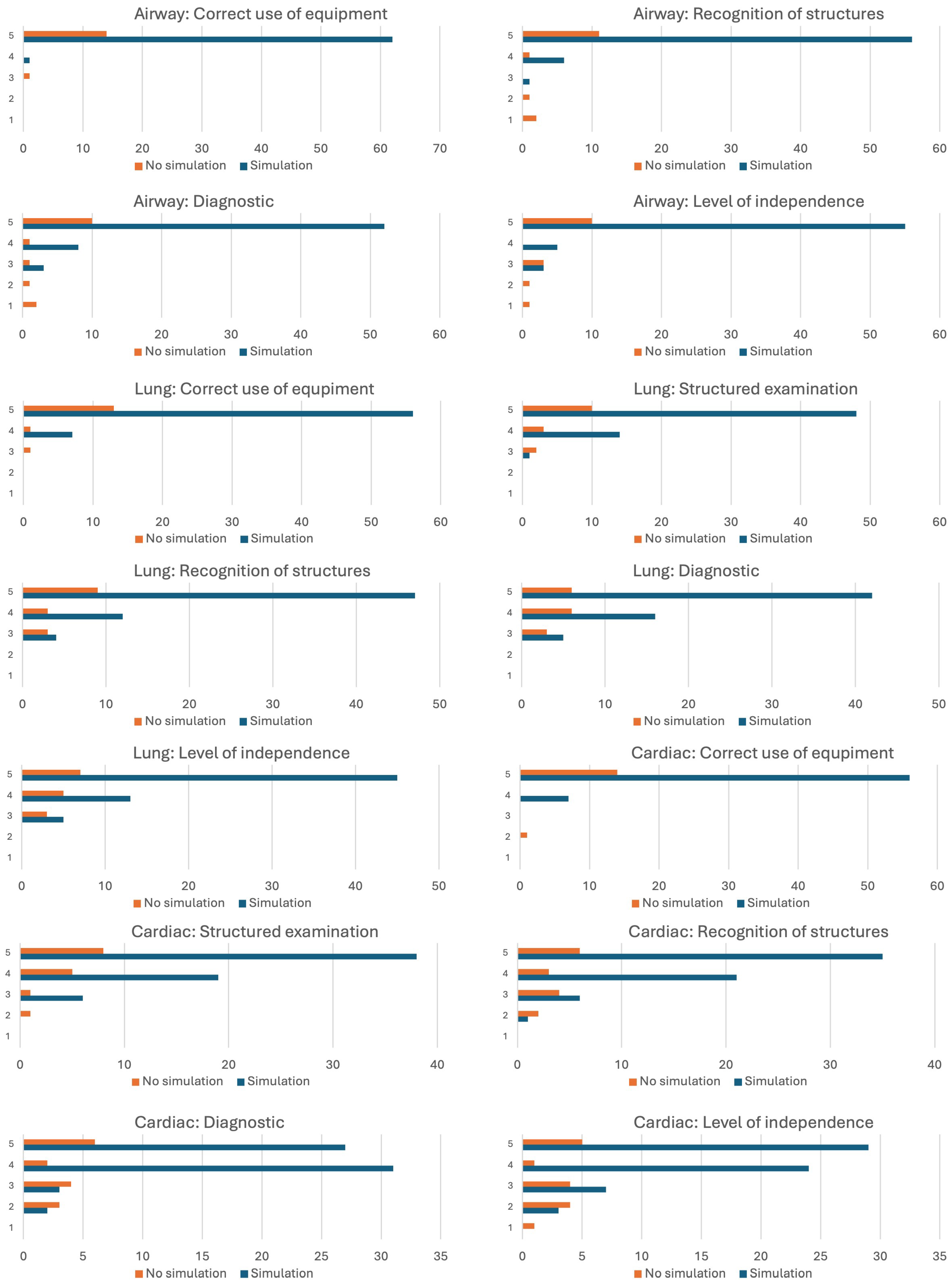
| Simulation | Mean | Std. Dev. | Coeff. of Variation | Variance | Shapiro–Wilk | p-Value of Shapiro–Wilk | |
|---|---|---|---|---|---|---|---|
| Airway: Correct use of equipment | yes | 4.984 | 0.126 | 0.025 | 0.016 | 0.106 | <0.001 |
| no | 4.867 | 0.516 | 0.106 | 0.267 | 0.284 | <0.001 | |
| Airway: Recognition of structures | yes | 4.873 | 0.381 | 0.078 | 0.145 | 0.372 | <0.001 |
| no | 4.200 | 1.521 | 0.362 | 2.314 | 0.576 | <0.001 | |
| Airway: Diagnostic | yes | 4.778 | 0.522 | 0.109 | 0.272 | 0.476 | <0.001 |
| no | 4.067 | 1.534 | 0.377 | 2.352 | 0.654 | <0.001 | |
| Airway: Level of independence | yes | 4.825 | 0.493 | 0.102 | 0.243 | 0.397 | <0.001 |
| no | 4.133 | 1.356 | 0.328 | 1.838 | 0.685 | <0.001 | |
| Lung: Correct use of equipment | yes | 4.889 | 0.317 | 0.065 | 0.100 | 0.364 | <0.001 |
| no | 4.800 | 0.561 | 0.117 | 0.314 | 0.421 | <0.001 | |
| Lung: Structured examination | yes | 4.746 | 0.474 | 0.100 | 0.225 | 0.555 | <0.001 |
| no | 4.533 | 0.743 | 0.164 | 0.552 | 0.663 | <0.001 | |
| Lung: Recognition of structures | yes | 4.683 | 0.591 | 0.126 | 0.349 | 0.577 | <0.001 |
| no | 4.400 | 0.828 | 0.188 | 0.686 | 0.705 | <0.001 | |
| Lung: Diagnostic | yes | 4.587 | 0.638 | 0.139 | 0.408 | 0.653 | <0.001 |
| no | 4.200 | 0.775 | 0.184 | 0.600 | 0.806 | 0.004 | |
| Lung: Level of independence | yes | 4.635 | 0.630 | 0.136 | 0.397 | 0.610 | <0.001 |
| no | 4.267 | 0.799 | 0.187 | 0.638 | 0.783 | 0.002 | |
| Cardiac: Correct use of equipment | yes | 4.889 | 0.317 | 0.065 | 0.100 | 0.364 | <0.001 |
| no | 4.800 | 0.775 | 0.161 | 0.600 | 0.284 | <0.001 | |
| Cardiac: Structured examination | yes | 4.508 | 0.669 | 0.148 | 0.448 | 0.700 | <0.001 |
| no | 4.333 | 0.900 | 0.208 | 0.810 | 0.748 | <0.001 | |
| Cardiac: Recognition of structures | yes | 4.429 | 0.734 | 0.166 | 0.539 | 0.737 | <0.001 |
| no | 3.867 | 1.125 | 0.291 | 1.267 | 0.840 | 0.012 | |
| Cardiac: Diagnostic | yes | 4.317 | 0.714 | 0.165 | 0.510 | 0.748 | <0.001 |
| no | 3.733 | 1.223 | 0.328 | 1.495 | 0.823 | 0.007 | |
| Cardiac: Level of independence | yes | 4.254 | 0.842 | 0.198 | 0.709 | 0.783 | <0.001 |
| no | 3.333 | 1.397 | 0.419 | 1.952 | 0.863 | 0.027 | |
| Duration of examination | yes | 13.476 | 4.724 | 0.351 | 22.318 | 0.952 | 0.015 |
| no | 16.200 | 6.971 | 0.430 | 48.600 | 0.912 | 0.148 |
| U | p | Rank-Biserial Correlation | |
|---|---|---|---|
| Airway: Correct use of equipment | 497.000 | 0.266 | 0.052 |
| Airway: Recognition of structures | 556.000 | 0.082 | 0.177 |
| Airway: Diagnostic | 566.500 | 0.092 | 0.199 |
| Airway: Level of independence | 585.500 | 0.028 * | 0.239 |
| Lung: Correct use of equipment | 486.500 | 0.757 | 0.030 |
| Lung: Structured examination | 530.000 | 0.342 | 0.122 |
| Lung: Recognition of structure | 553.500 | 0.196 | 0.171 |
| Lung: Diagnostic | 607.500 | 0.048 * | 0.286 |
| Lung: Level of independence | 596.500 | 0.06 | 0.262 |
| Cardiac: Correct use of equipment | 455.000 | 0.682 | −0.037 |
| Cardiac: Structured examination | 512.500 | 0.567 | 0.085 |
| Cardiac: Recognition of structure | 602.500 | 0.07 | 0.275 |
| Cardiac: Diagnostic | 590.000 | 0.107 | 0.249 |
| Cardiac: Level of independence | 648.500 | 0.018 * | 0.372 |
| Duration of evaluation | 336.000 | 0.082 | −0.289 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simon, R.; Petrișor, C.; Bodolea, C.; Antal, O.; Băncișor, M.; Moldovan, O.; Puia, I.C. Transfer of POCUS Skills of Anesthesia Trainees from the Simulation Laboratory to Clinical Practice: A Follow-Up Pilot Evaluation After ABC US Protocol Training. Diagnostics 2025, 15, 354. https://doi.org/10.3390/diagnostics15030354
Simon R, Petrișor C, Bodolea C, Antal O, Băncișor M, Moldovan O, Puia IC. Transfer of POCUS Skills of Anesthesia Trainees from the Simulation Laboratory to Clinical Practice: A Follow-Up Pilot Evaluation After ABC US Protocol Training. Diagnostics. 2025; 15(3):354. https://doi.org/10.3390/diagnostics15030354
Chicago/Turabian StyleSimon, Robert, Cristina Petrișor, Constantin Bodolea, Oana Antal, Marta Băncișor, Orlanda Moldovan, and Ion Cosmin Puia. 2025. "Transfer of POCUS Skills of Anesthesia Trainees from the Simulation Laboratory to Clinical Practice: A Follow-Up Pilot Evaluation After ABC US Protocol Training" Diagnostics 15, no. 3: 354. https://doi.org/10.3390/diagnostics15030354
APA StyleSimon, R., Petrișor, C., Bodolea, C., Antal, O., Băncișor, M., Moldovan, O., & Puia, I. C. (2025). Transfer of POCUS Skills of Anesthesia Trainees from the Simulation Laboratory to Clinical Practice: A Follow-Up Pilot Evaluation After ABC US Protocol Training. Diagnostics, 15(3), 354. https://doi.org/10.3390/diagnostics15030354






