Ex Vivo Quantitative Evaluation of Beam Hardening Artifacts at Various Implant Locations in Cone-Beam Computed Tomography Using Metal Artifact Reduction and Noise Reduction Techniques
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Preparation and Scanning
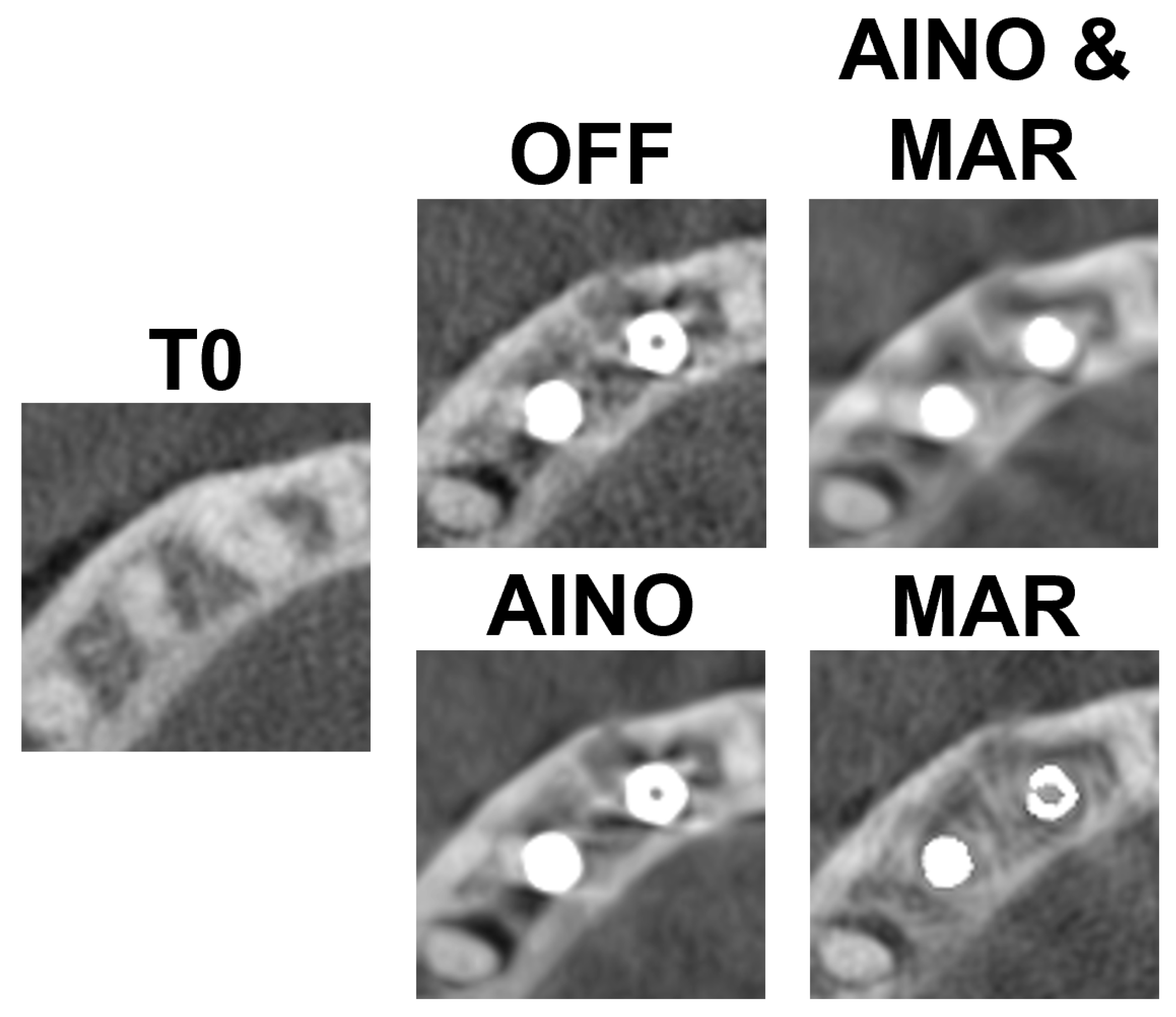
- C1—Configuration where two implants are side by side, that is, there are no teeth between the implants.
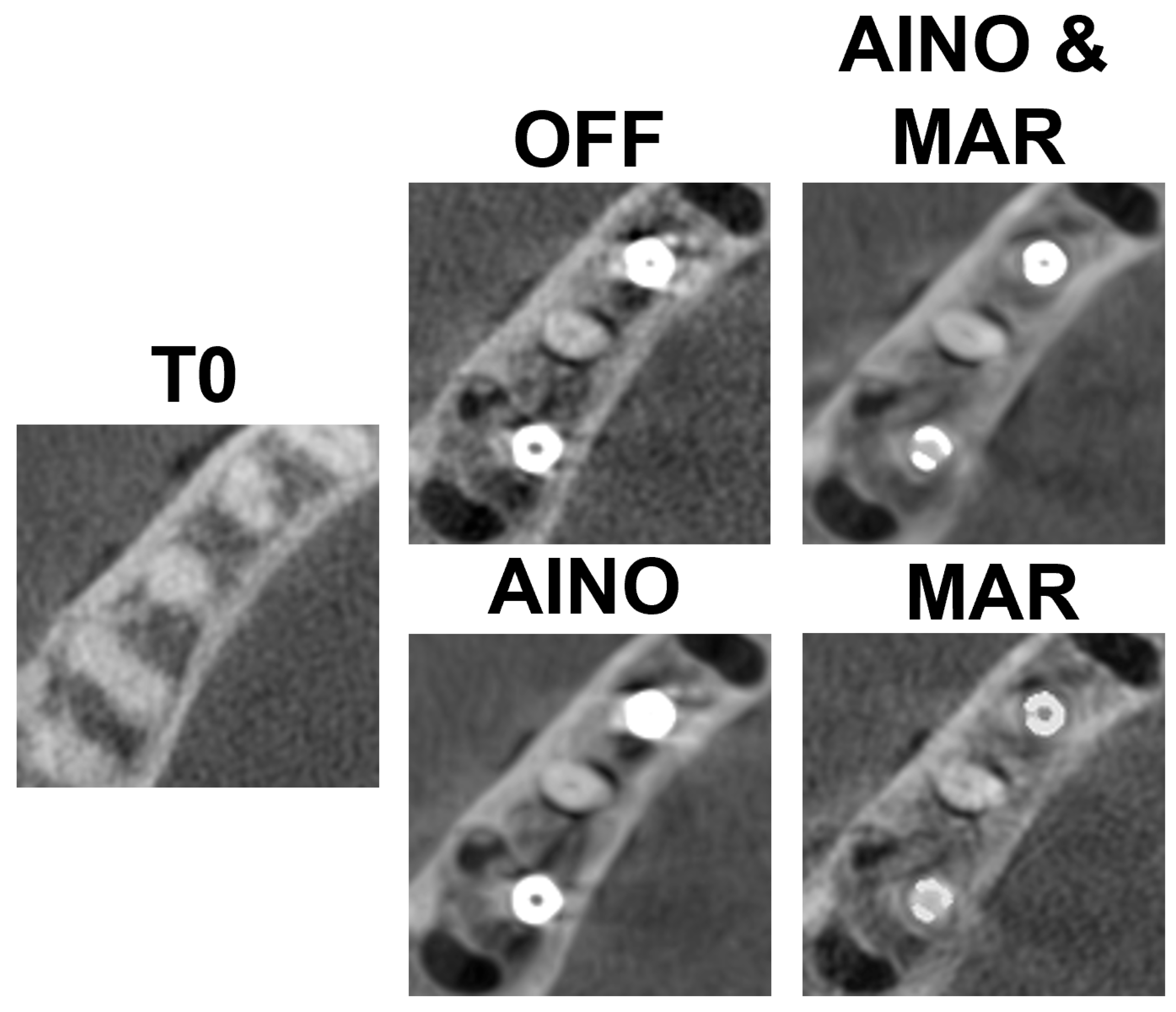
- C2—Configuration with a tooth between the implants.
2.2. Image Analysis
2.2.1. Image Registration
2.2.2. Gray Value Normalization
2.2.3. Artifact Region of Interest Selection
- Rectangular, equal width and height (10 × 10 voxels);
- Close to the implants, but not containing any part of the implant itself.
- C1—lingual, buccal and mesial to the mesial implant; lingual, buccal and distal to the distal implant; and an additional ROI between the implants (n = 7).
- C2—lingual, buccal, mesial and distal to each implant (n = 8).
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hunter, A.K.; McDavid, W.D. Characterization and correction of cupping effect artifacts in cone beam CT. Dentomaxillofac. Radiol. 2012, 41, 217–223. [Google Scholar] [CrossRef]
- Schulze, R.; Heil, U.; Groβ, D.; Bruellmann, D.D.; Dranischnikow, E.; Schwanecke, U.; Schoemer, E. Artifacts in CBCT: A review. Dentomaxillofac. Radiol. 2011, 40, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Alamri, H.M.; Sadrameli, M.; Alshalhoob, M.A.; Sadrameli, M.; Alshehri, M.A. Applications of CBCT in dental practice: A review of the literature. Gen. Dent. 2012, 60, 390–400. [Google Scholar] [PubMed]
- Fontenele, R.C.; Nascimento, E.H.; Vasconcelos, T.V.; Noujeim, M.; Freitas, D.Q. Magnitude of cone beam CT image artifacts related to zirconium and titanium implants: Impact on image quality. Dentomaxillofac. Radiol. 2018, 47, 20180021. [Google Scholar] [CrossRef]
- Nakae, Y.; Sakamoto, K.; Minamoto, T.; Kamakura, T.; Ogata, Y.; Matsumoto, M.; Johkou, T. Clinical evaluation of a newly developed method for avoiding artifacts caused by dental fillings on X-ray CT. Radiol. Phys. Technol. 2008, 1, 115–122. [Google Scholar] [CrossRef]
- Nabha, W.; Hong, Y.M.; Cho, J.H.; Hwang, H.S. Assessment of metal artifacts in three-dimensional dental surface models derived by cone-beam computed tomography. Korean J. Orthod. 2014, 44, 229–235. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jin, S.O.; Kim, J.G.; Lee, S.Y.; Kwon, O.K. Bone-induced streak artifact suppression in sparse-view CT image reconstruction. Biomed. Eng. Online 2012, 11, 44. [Google Scholar] [CrossRef]
- Nagarajappa, A.K.; Dwivedi, N.; Tiwari, R. Artifacts: The downturn of CBCT image. J. Int. Soc. Prev. Community Dent. 2015, 5, 440–445. [Google Scholar] [CrossRef]
- Do, S.; Karl, W.C.; Liang, Z.; Kalra, M.; Brady, T.J.; Pien, H.H. A decomposition-based CT reconstruction formulation for reducing blooming artefacts. Phys. Med. Biol. 2011, 56, 7109–7125. [Google Scholar] [CrossRef]
- Różyło-Kalinowska, I.; Miechowicz, S.; Sarna-Boś, K.; Borowicz, J.; Kalinowski, P. Analysis of vector models in quantification of artifacts produced by standard prosthetic inlays in Cone-Beam Computed Tomography (CBCT)—A preliminary study. Postep. Hig. Med. Dosw. (Online) 2014, 68, 1343–1346. [Google Scholar] [CrossRef]
- Takeshita, W.M.; Vessoni Iwaki, L.C.; Da Silva, M.C.; Tonin, R.H. Evaluation of diagnostic accuracy of conventional and digital periapical radiography, panoramic radiography, and cone-beam computed tomography in the assessment of alveolar bone loss. Contemp. Clin. Dent. 2014, 5, 318–323. [Google Scholar] [CrossRef]
- Jones, A.A.; Cochran, D.L. Consequences of implant design. Dent. Clin. N. Am. 2006, 50, 339–360. [Google Scholar] [CrossRef] [PubMed]
- Lekholm, U.; Zarb, G. Patient selection and preparation. In Tissue Integrated Prostheses, Osseointegration in Clinical Dentistry; Branemark, P.I., Zarb, G.A., Albrektsson, T., Eds.; Quintessence: Chicago, IL, USA, 1985; pp. 199–209. [Google Scholar]
- Sawicki, P.; Zawadzki, P.J.; Regulski, P. The impact of cone-beam computed tomography exposure parameters on Peri-implant artifacts: A literature review. Cureus 2022, 14, e23035. [Google Scholar] [CrossRef]
- Wanderley, V.A.; Freitas, D.Q.; Haiter-Neto, F.; Oliveira, M.L. Influence of Tooth Orientation on the Detection of Vertical Root Fracture in Cone-beam Computed Tomography. J. Endod. 2018, 44, 1168–1172. [Google Scholar] [CrossRef] [PubMed]
- Fontenele, R.C.; Farias Gomes, A.; Rosado, L.P.L.; Neves, F.S.; Freitas, D.Q. Mapping the expression of beam hardening artifacts produced by metal posts positioned in different regions of the dental arch. Clin. Oral Investig. 2021, 25, 571–579. [Google Scholar] [CrossRef]
- Pinto, M.G.O.; Rabelo, K.A.; Sousa Melo, S.L.; Campos, P.S.F.; Oliveira, L.S.A.F.; Bento, P.M.; Melo, D.P. Influence of exposure parameters on the detection of simulated root fractures in the presence of various intracanal materials. Int. Endod. J. 2017, 50, 586–594. [Google Scholar] [CrossRef]
- Queiroz, P.M.; Oliveira, M.L.; Groppo, F.C.; Haiter-Neto, F.; Freitas, D.Q. Evaluation of metal artifact reduction in cone-beam computed tomography images of different dental materials. Clin. Oral Investig. 2018, 22, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Gaêta-Araujo, H.; Nascimento, E.H.L.; Fontenele, R.C.; Mancini, A.X.M.; Freitas, D.Q.; Oliveira-Santos, C. Magnitude of beam-hardening artifacts produced by gutta-percha and metal posts on cone-beam computed tomography with varying tube current. Imaging Sci. Dent. 2020, 50, 1–7. [Google Scholar] [CrossRef]
- Bagis, N.; Kurt, M.H.; Evli, C.; Camgoz, M.; Atakan, C.; Peker Ozturk, H.; Orhan, K. Evaluation of a metal artifact reduction algorithm and an adaptive image noise optimization filter in the estimation of peri-implant fenestration defects using cone beam computed tomography: An in-vitro study. Oral Radiol. 2022, 38, 325–335, Erratum in Oral Radiol. 2022, 38, 336. https://doi.org/10.1007/s11282-022-00586-2. [Google Scholar] [CrossRef] [PubMed]
- Benic, G.I.; Mokti, M.; Chen, C.-J.; Weber, H.-P.; Hammerle, C.H.F.; Gallucci, G.O. Dimensions of buccal bone and mucosa at immediately placed implants after 7 years: A clinical and cone beam computed tomography study. Clin. Oral Implant. Res. 2012, 23, 560–566. [Google Scholar] [CrossRef]
- Schropp, L.; Wenzel, A.; Spin-Neto, R.; Stavropoulos, A. Fate of the buccal bone at implants placed early, delayed, or late after tooth extraction analyzed by cone beam CT: 10-year results from a randomized, controlled, clinical study. Clin. Oral Implant. Res. 2014, 26, 492–500. [Google Scholar] [CrossRef]
- Shahmirzadi, S.; Sharaf, R.A.; Saadat, S.; Moore, W.S.; Geha, H.; Tamimi, D.; Kocasarac, H.D. Assessment of the efficiency of a pre- versus post-acquisition metal artifact reduction algorithm in the presence of 3 different dental implant materials using multiple CBCT settings: An in vitro study. Imaging Sci. Dent. 2021, 51, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Parsa, A.; Ibrahim, N.; Hassan, B.; Syriopoulos, K.; van der Stelt, P. Assessment of metal artifact reduction around dental titanium implants in cone beam CT. Dentomaxillofac. Radiol. 2014, 43, 20140019. [Google Scholar] [CrossRef]
- Nascimento, E.H.L.; Fontenele, R.C.; Santaella, G.M.; Freitas, D.Q. Difference in the artifacts production and the performance of the metal artifact reduction (MAR) tool between the buccal and lingual cortical plates adjacent to zirconium dental implant. Dentomaxillofac. Radiol. 2019, 48, 20190058. [Google Scholar] [CrossRef]
- Elshenawy, H.; Aly, W.; Salah, N.; Nasry, S.; Anter, E.; Ekram, K. Influence of Small, Midi, Medium and Large Fields of View on Accuracy of Linear Measurements in CBCT Imaging: Diagnostic Accuracy Study. Open Access Maced. J. Med. Sci. 2019, 7, 1037–1041. [Google Scholar] [CrossRef] [PubMed]
- Eftekhar, M.; Kaviani, H.; Rouzmeh, N.; Torabinia, A.; Akbarzadeh Baghban, A. Effect of voxel size on detection of fenestration, dehiscence and furcation defects using cone-beam computed tomography. Oral Radiol. 2021, 37, 677–686. [Google Scholar] [CrossRef]
- Bauman, R.; Scarfe, W.; Clark, S.; Morelli, J.; Scheetz, J.; Farman, A. Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensions. Int. Endod. J. 2011, 44, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Dalili, Z.; Taramsari, M.; Mousavi Mehr, S.Z.; Salamat, F. Diagnostic value of two modes of cone-beam computed tomography in evaluation of simulated external root resorption: An in vitro study. Imaging Sci. Dent. 2012, 42, 19–24. [Google Scholar] [CrossRef]
- Molteni, R. Prospects and challenges of rendering tissue density in Hounsfield units for cone beam computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 105–119. [Google Scholar] [CrossRef]
- de Oliveira Pinto, M.G.; Melo, S.L.S.; Suassuna, F.C.M.; Marinho, L.E.; Leite, J.B.D.S.; Batista, A.U.D.; Bento, P.M.; Melo, D.P. Influence of size of field of view (FOV), position within the FOV, and scanning mode on the detection of root fracture and observer’s perception of artifacts in CBCT images. Dentomaxillofac. Radiol. 2021, 50, 20200563. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pauwels, R.; Jacobs, R.; Bogaerts, R.; Bosmans, H.; Panmekiate, S. Reduction of scatter-induced image noise in cone beam computed tomography: Effect of field of view size and position. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, 188–195. [Google Scholar] [CrossRef]
- Pauwels, R.; Pittayapat, P.; Sinpitaksakul, P.; Panmekiate, S. Scatter-to-primary ratio in dentomaxillofacial cone-beam CT: Effect of field of view and beam energy. Dentomaxillofac. Radiol. 2021, 50, 20200597. [Google Scholar] [CrossRef] [PubMed]
- Khosravifard, A.; Saberi, B.V.; Khosravifard, N.; Motallebi, S.; Kajan, Z.D.; Ghaffari, M.E. Application of an auto-edge counting method for quantification of metal artifacts in CBCT images: A multivariate analysis of object position, field of view size, tube voltage, and metal artifact reduction algorithm. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Wanderley, V.A.; Leite, A.F.; de Faria Vasconcelos, K.; Pauwels, R.; Müller-García, F.; Becker, K.; Oliveira, M.L.; Jacobs, R. Impact of metal artefacts on subjective perception of image quality of 13 CBCT devices. Clin. Oral Investig. 2022, 26, 4457–4466. [Google Scholar] [CrossRef]
- Gaêta-Araujo, H.; Alzoubi, T.; Vasconcelos, K.F.; Orhan, K.; Pauwels, R.; Casselman, J.W.; Jacobs, R. Cone beam computed tomography in dentomaxillofacial radiology: A two-decade overview. Dentomaxillofac. Radiol. 2020, 49, 20200145. [Google Scholar] [PubMed]
- Pinto, J.C.; de Faria Vasconcelos, K.; Leite, A.F.; Wanderley, V.A.; Pauwels, R.; Oliveira, M.L.; Jacobs, R.; Tanomaru-Filho, M. Image quality for visualization of cracks and fine endodontic structures using 10 CBCT devices with various scanning protocols and artefact conditions. Sci. Rep. 2023, 13, 4001. [Google Scholar] [CrossRef]
- Fontenele, R.C.; Farias Gomes, A.; Nejaim, Y.; Freitas, D.Q. Do the tube current and metal artifact reduction influence the diagnosis of vertical root fracture in a tooth positioned in the vicinity of a zirconium implant? A CBCT study. Clin. Oral Investig. 2021, 25, 2229–2235. [Google Scholar] [CrossRef]
- Salemi, F.; Jamalpour, M.R.; Eskandarloo, A.; Tapak, L.; Rahimi, N. Efficacy of Metal Artifact Reduction Algorithm of Cone-Beam Computed Tomography for Detection of Fenestration and Dehiscence around Dental Implants. J. Biomed. Phys. Eng. 2021, 11, 305–314. [Google Scholar] [CrossRef]
- Schulze, R. CBCT artefact-burden of zirconia-based as compared to titanium implants for different beam energies: An analytical approach. Sci. Rep. 2022, 12, 15276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vasconcelos, T.V.; Leandro Nascimento, E.H.; Bechara, B.B.; Freitas, D.Q.; Noujeim, M. Influence of Cone Beam Computed Tomography Settings on Implant Artifact Production: Zirconia and Titanium. Int. J. Oral Maxillofac. Implant. 2019, 34, 1114–1120. [Google Scholar] [CrossRef]


| Region of Interest | C1 | C2 |
| (Mean ± SD) | (Mean ± SD) | |
| Between implants | 1.885 ± 0.316 | NA |
| Distal implant | ||
| Lingual side | 2.690 ± 0.484 | 2.621 ± 0.069 |
| Buccal side | 3.273 ± 0.171 | 1.397 ± 0.106 |
| Distal side | 1.863 ± 0.144 | 1.227 ± 0.069 |
| Mesial side | NA | 1.489 ± 0.101 |
| Mesial implant | ||
| Lingual side | 2.906 ± 0.266 | 2.957 ± 0.105 |
| Buccal side | 2.920 ± 0.497 | 2.987 ± 0.099 |
| Distal side | NA | 1.808 ± 0.053 |
| Mesial side | 2.762 ± 0.235 | 2.875 ± 0.080 |
| Region of Interest | C0 | OFF | AINO+ | AINO+MAR high | p-Value 1 | p-Value 2 | p-Value 3 |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||||
| Between implant | 1.885 ± 0.316 | 2.283 ± 0.082 | 1.674 ± 0.422 | 2.214 ± 0.214 | 0.012 | <0.001 | 0.001 |
| Median (IQR) | 1.850 (1.669–2.178) | 2.296 (2.204–2.356) | 1.510 (1.373–2.169) | 2.186 (2.027–2.361) | |||
| Distal implant | |||||||
| Lingual | 2.690 ± 0.484 | 3.089 ± 0.059 | 2.939 ± 0.444 | 3.126 ± 0.113 | 0.575 | 0.156 | >0.999 |
| Median (IQR) | 2.795 (2.249–3.161) | 3.122 (3.025–3.136) | 3.104 (2.488–3.245) | 3.118 (3.016–3.238) | |||
| Buccal | 3.273 ± 0.171 | 3.978 ± 0.082 | 3.323 ± 0.103 | 3.354 ± 0.155 | <0.001 | 0.371 | 0.154 |
| Median (IQR) | 3.306 (3.253–3.370) | 4.003 (3.913–4.030) | 3.344 (3.205–3.424) | 3.401 (3.234–3.463) | |||
| Distal | 1.863 ± 0.144 | 2.129 ± 0.184 | 1.985 ± 0.193 | 2.275 ± 0.183 | 0.006 | 0.040 | 0.001 |
| Median (IQR) | 1.884 (1.724–1.995) | 2.065 (1.990–2.300) | 1.978 (1.854–2.167) | 2.257 (2.121–2.419) | |||
| Mesial implant | |||||||
| Lingual | 2.906 ± 0.266 | 2.991 ± 0.025 | 2.837 ± 0.249 | 2.682 ± 0.387 | 0.717 | 0.575 | 0.062 |
| Median (IQR) | 2.849 (2.682–3.183) | 2.983 (2.969–3.016) | 2.878 (2.634–3.058) | 2.649 (2.337–3.096) | |||
| Buccal | 2.920 ± 0.497 | 4.402 ± 0.060 | 2.700 ± 0.306 | 2.742 ± 0.290 | <0.001 | 0.575 | 0.137 |
| Median (IQR) | 2.788 (2.497–3.399) | 4.388 (4.350–4.462) | 2.581 (2.481–2.976) | 2.614 (2.543–3.028) | |||
| Mesial | 2.762 ± 0.235 | 2.464 ± 0.134 | 2.713 ± 0.128 | 2.684 ± 0.123 | 0.015 | 0.550 | 0.482 |
| Median (IQR) | 2.780 (2.558–2.998) | 2.381 (2.373–2.596) | 2.726 (2.613–2.789) | 2.663 (2.588–2.749) | |||
| Region of Interest | C0 | OFF | AINO+ | AINO+MAR high | p-Value 1 | p-Value 2 | p-Value 3 |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||||
| Distal implant | |||||||
| Lingual | 2.621 ± 0.069 | 2.409 ± 0.029 | 2.583 ± 0.031 | 2.361 ± 0.055 | <0.001 | 0.005 | <0.001 |
| Median (IQR) | 2.643 (2.569–2.662) | 2.404 (2.388–2.433) | 2.587 (2.566–2.609) | 2.359 (2.322–2.409) | |||
| Buccal | 1.397 ± 0.106 | 3.567 ± 0.117 | 1.434 ± 0.086 | 1.495 ± 0.135 | <0.001 | 0.006 | 0.067 |
| Median (IQR) | 1.398 (1.339–1.498) | 3.496 (3.477–3.691) | 1.453 (1.359–1.489) | 1.438 (1.413–1.556) | |||
| Distal | 1.227 ± 0.069 | 1.698 ± 0.163 | 1.227 ± 0.035 | 1.744 ± 0.106 | <0.001 | 0.989 | <0.001 |
| Median (IQR) | 1.222 (1.185–1.277) | 1.674 (1.546–1.862) | 1.223 (1.202–1.247) | 1.764 (1.669–1.834) | |||
| Mesial | 1.489 ± 0.101 | 2.001 ± 0.081 | 1.477 ± 0.096 | 1.838 ± 0.114 | <0.001 | 0.267 | <0.001 |
| Median (IQR) | 1.483 (1.420–1.575) | 1.968 (1.932–2.087) | 1.487 (1.426–1.537) | 1.841 (1.798–1.899) | |||
| Mesial implant | |||||||
| Lingual | 2.957 ± 0.105 | 2.787 ± 0.096 | 2.942 ± 0.094 | 2.751 ± 0.132 | <0.001 | 0.209 | <0.001 |
| Median (IQR) | 2.974 (2.945–3.014) | 2.769 (2.702–2.881) | 2.946 (2.890–3.011) | 2.741 (2.656–2.820) | |||
| Buccal | 2.987 ± 0.099 | 3.428 ± 0.128 | 3.023 ± 0.098 | 2.953 ± 0.168 | <0.001 | 0.003 | 0.001 |
| Median (IQR) | 2.992 (2.927–3.075) | 3.398 (3.312–3.560) | 3.006 (2.949–3.092) | 2.936 (2.814–3.068) | |||
| Distal | 1.808 ± 0.053 | 2.259 ± 0.088 | 1.776 ± 0.044 | 2.304 ± 0.071 | <0.001 | 0.029 | <0.001 |
| Median (IQR) | 1.803 (1.786–1.847) | 2.283 (2.185–2.321) | 1.774 (1.751–1.801) | 2.313 (2.245–2.373) | |||
| Mesial | 2.875 ± 0.080 | 2.406 ± 0.042 | 2.864 ± 0.070 | 2.519 ± 0.140 | <0.001 | 0.353 | <0.001 |
| Median (IQR) | 2.886 (2.831–2.924) | 2.416 (2.368–2.440) | 2.869 (2.827–2.903) | 2.559 (2.404–2.636) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evli, C.; Önder, M.; Pauwels, R.; Kurt, M.H.; Koçyiğit, İ.D.; Yazıcı, G.; Orhan, K. Ex Vivo Quantitative Evaluation of Beam Hardening Artifacts at Various Implant Locations in Cone-Beam Computed Tomography Using Metal Artifact Reduction and Noise Reduction Techniques. Diagnostics 2025, 15, 3201. https://doi.org/10.3390/diagnostics15243201
Evli C, Önder M, Pauwels R, Kurt MH, Koçyiğit İD, Yazıcı G, Orhan K. Ex Vivo Quantitative Evaluation of Beam Hardening Artifacts at Various Implant Locations in Cone-Beam Computed Tomography Using Metal Artifact Reduction and Noise Reduction Techniques. Diagnostics. 2025; 15(24):3201. https://doi.org/10.3390/diagnostics15243201
Chicago/Turabian StyleEvli, Cengiz, Merve Önder, Ruben Pauwels, Mehmet Hakan Kurt, İsmail Doruk Koçyiğit, Gökhan Yazıcı, and Kaan Orhan. 2025. "Ex Vivo Quantitative Evaluation of Beam Hardening Artifacts at Various Implant Locations in Cone-Beam Computed Tomography Using Metal Artifact Reduction and Noise Reduction Techniques" Diagnostics 15, no. 24: 3201. https://doi.org/10.3390/diagnostics15243201
APA StyleEvli, C., Önder, M., Pauwels, R., Kurt, M. H., Koçyiğit, İ. D., Yazıcı, G., & Orhan, K. (2025). Ex Vivo Quantitative Evaluation of Beam Hardening Artifacts at Various Implant Locations in Cone-Beam Computed Tomography Using Metal Artifact Reduction and Noise Reduction Techniques. Diagnostics, 15(24), 3201. https://doi.org/10.3390/diagnostics15243201








