Thromboelastography to Support Clinical Decision Making in Patients with Peripheral Artery Disease
Abstract
1. Introduction
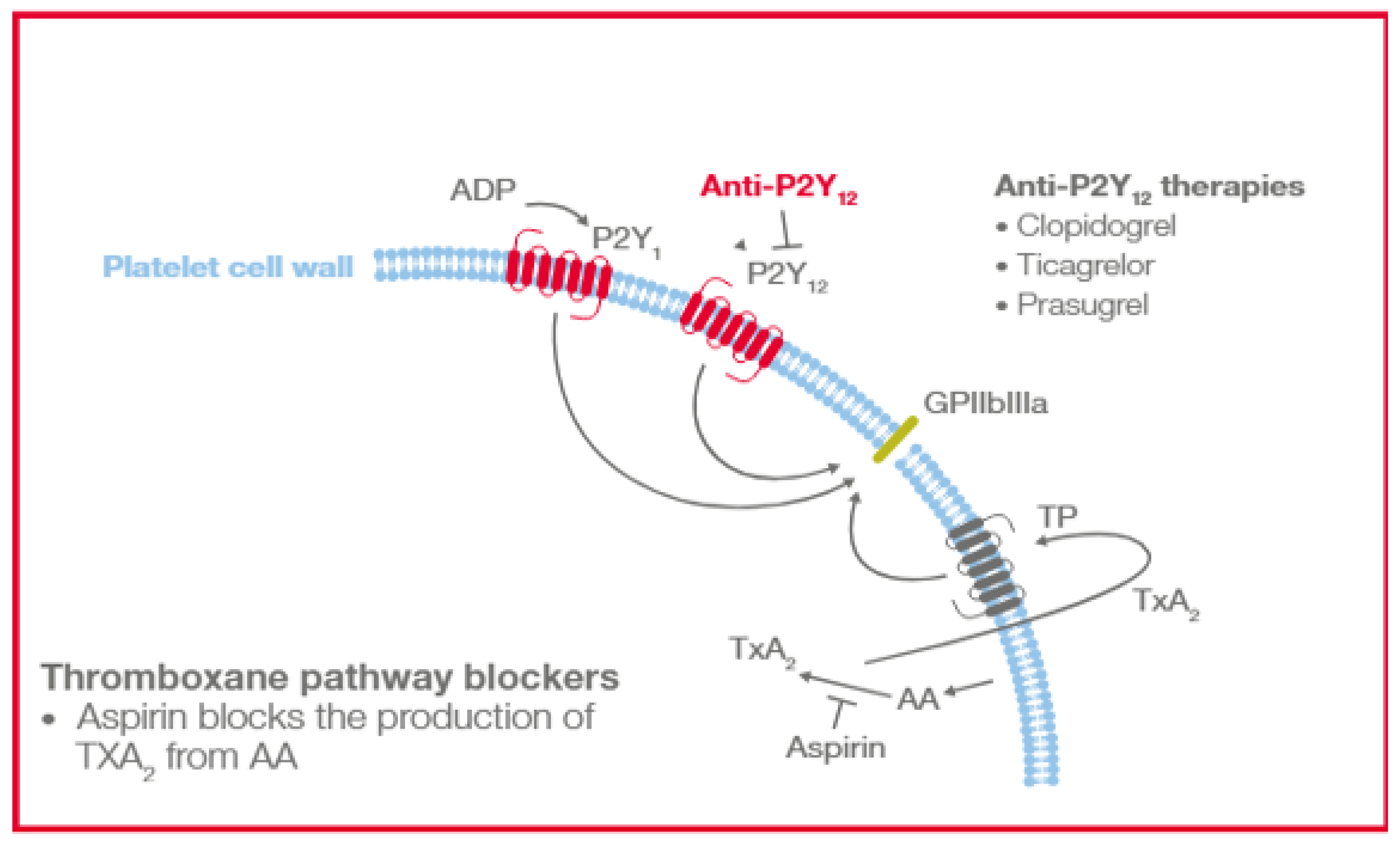
2. Antithrombotic Therapy in Patients with PAD
3. Thromboelastography Has a History of Clinical Use in Assessing Patient Hemostasis
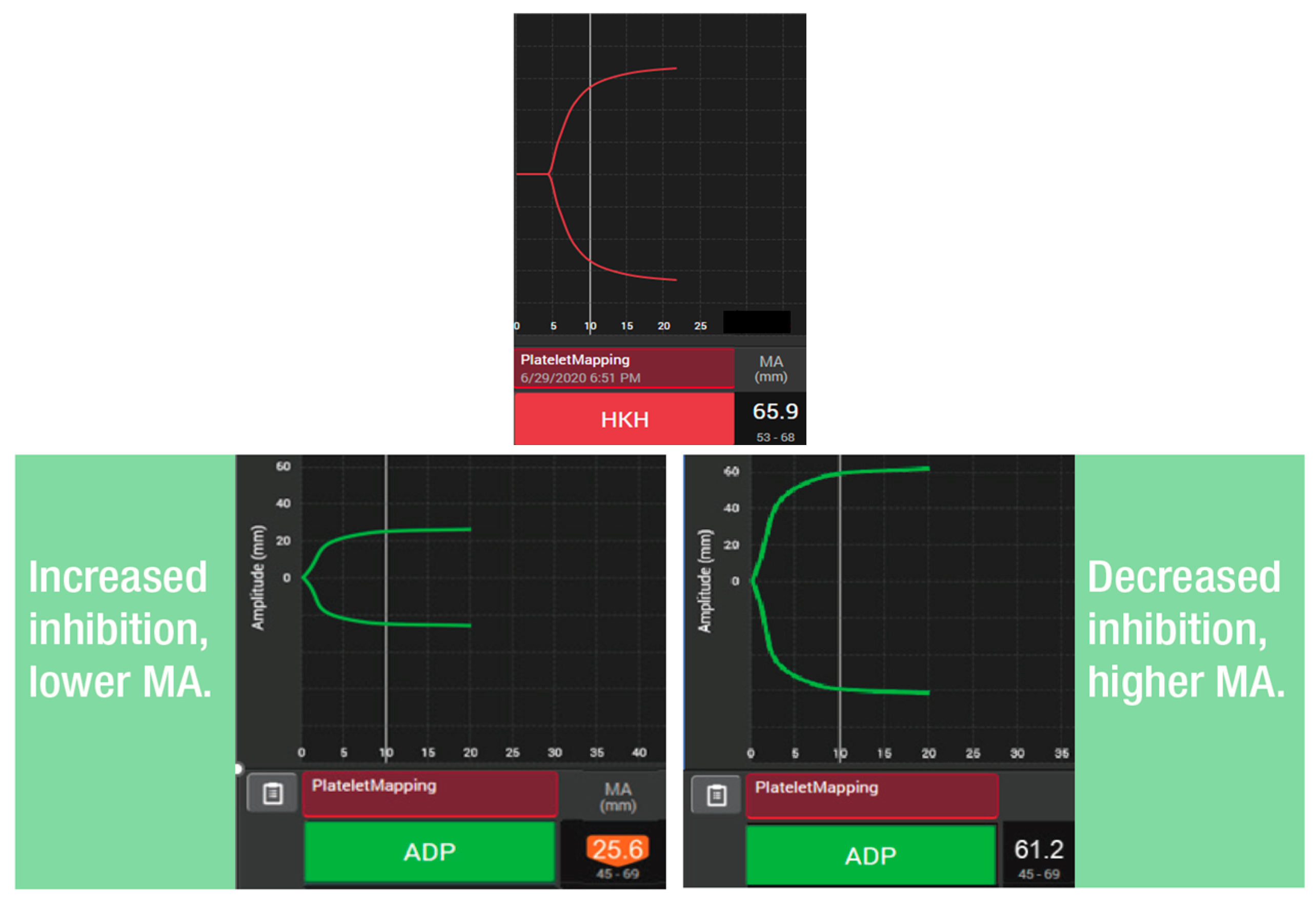
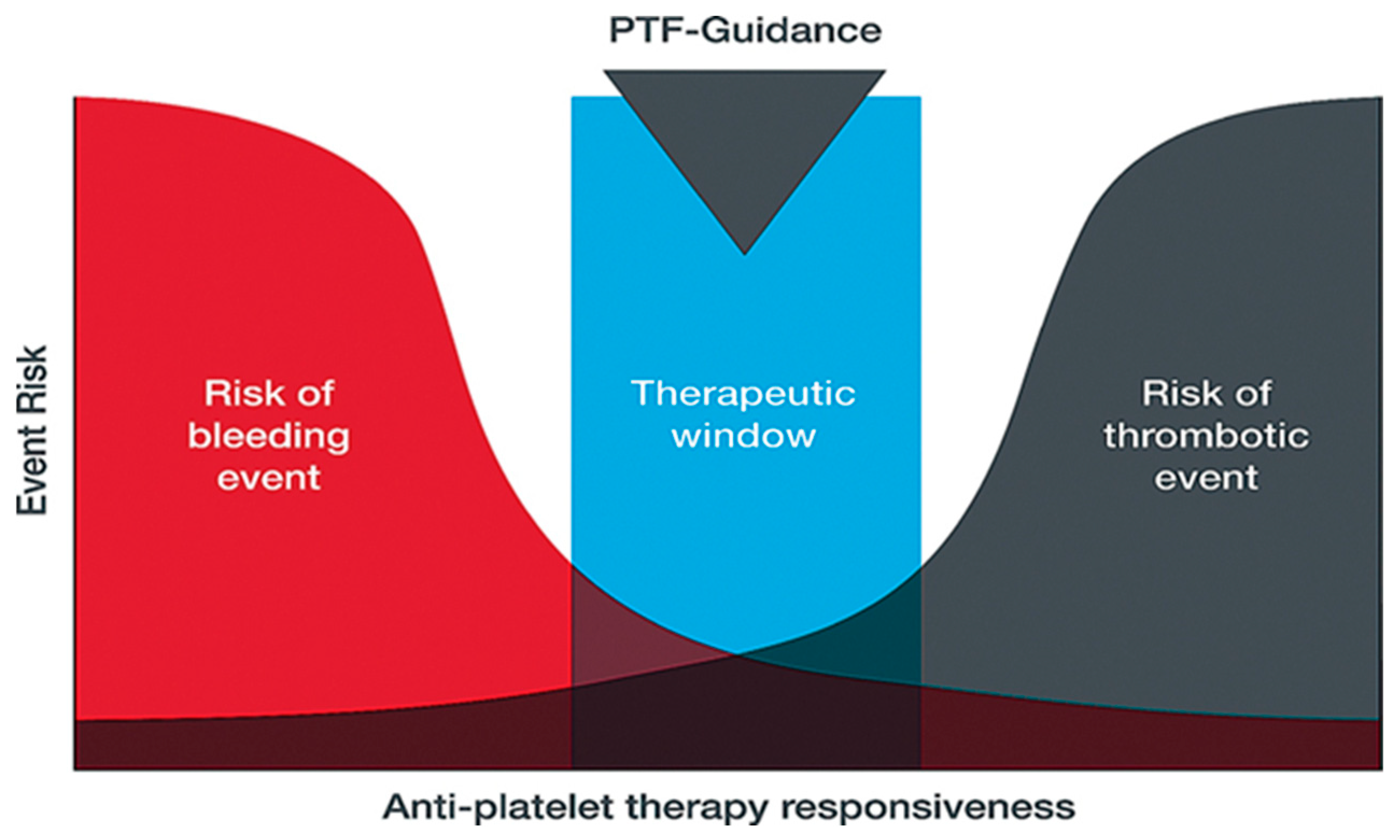
4. Assessing Platelet Function with Thromboelastography Can Provide an Analysis of Platelet Contribution to Hemostasis
5. Utility of TEG® PlateletMapping® Testing Technology in Patients with PAD
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AA | Arachidonic acid |
| ADP | Adenosine diphosphate |
| COX-1 | Cyclooxygenase-1 |
| DAPT | Dual-antiplatelet therapy |
| GPIIbIIIa, | Glycoprotein IIb/IIIa |
| HKH | Kaolin with heparinase |
| MA | Maximum amplitude |
| MACE | Major adverse cardiovascular event |
| MALE | Major adverse limb event |
| MAPT | Mono-antiplatelet therapy |
| P2Y12 | Purinergic G protein-coupled receptor |
| PAD | Peripheral artery disease |
| PAR-1 | Protease-activated receptor 1 |
| PCI | Percutaneous coronary intervention |
| TP | Human TXA2 receptor |
| TXA2 | Thromboxane A2 |
References
- Shu, J.; Santulli, G. Update on peripheral artery disease: Epidemiology and evidence-based facts. Atherosclerosis 2018, 275, 379–381. [Google Scholar] [CrossRef]
- Global Burden of Disease (GBD) Peripheral Artery Disease Collaborators. Global burden of peripheral artery disease and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob. Health 2023, 11, e1553–e1565. [Google Scholar] [CrossRef] [PubMed]
- Hiatt, W.R. Medical treatment of peripheral arterial disease and claudication. N. Engl. J. Med. 2001, 344, 1608–1621. [Google Scholar] [CrossRef] [PubMed]
- Kullo, I.J.; Rooke, T.W. Peripheral Artery Disease. N. Engl. J. Med. 2016, 374, 861–871. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Weissler, E.H.; Long, C.A.; Williams, Z.F.; Dua, A.; Southerland, K.W. Sex-based differences in outcomes after lower extremity bypass for chronic limb-threatening ischemia. Atherosclerosis 2023, 384, 117157. [Google Scholar] [CrossRef]
- Pabon, M.; Cheng, S.; Altin, S.E.; Sethi, S.S.; Nelson, M.D.; Moreau, K.L.; Hamburg, N.; Hess, C.N. Sex Differences in Peripheral Artery Disease. Circ. Res. 2022, 130, 496–511. [Google Scholar] [CrossRef]
- Criqui, M.H.; Matsushita, K.; Aboyans, V.; Hess, C.N.; Hicks, C.W.; Kwan, T.W.; McDermott, M.M.; Misra, S.; Ujueta, F.; on behalf of the American Heart Association Council on Epidemiology and Prevention; et al. Lower Extremity Peripheral Artery Disease: Contemporary Epidemiology, Management Gaps, and Future Directions: A Scientific Statement from the American Heart Association. Circulation 2021, 144, e171–e191. [Google Scholar] [CrossRef]
- Soyoye, D.O.; Abiodun, O.O.; Ikem, R.T.; Kolawole, B.A.; Akintomide, A.O. Diabetes and peripheral artery disease: A review. World J. Diabetes 2021, 12, 827–838. [Google Scholar] [CrossRef]
- Majumdar, M.; Hall, R.P.; Feldman, Z.; Goudot, G.; Sumetsky, N.; Jessula, S.; Kirshkaln, A.; Bellomo, T.; Chang, D.; Cardenas, J.; et al. Predicting Arterial Thrombotic Events Following Peripheral Revascularization Using Objective Viscoelastic Data. J. Am. Heart Assoc. 2023, 12, e027790. [Google Scholar] [CrossRef]
- Hartmann, J.; Hermelin, D.; Levy, J.H. Viscoelastic testing: An illustrated review of technology and clinical applications. Res. Pract. Thromb. Haemost. 2023, 7, 100031. [Google Scholar] [CrossRef]
- Gurbel, P.A.; Fox, K.A.A.; Tantry, U.S.; Ten Cate, H.; Weitz, J.I. Combination Antiplatelet and Oral Anticoagulant Therapy in Patients with Coronary and Peripheral Artery Disease. Circulation 2019, 139, 2170–2185. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Majumdar, M.; Imran, R.; Yi, J. A comprehensive review on antithrombotic therapy for peripheral artery disease. Semin. Vasc. Surg. 2022, 35, 124–131. [Google Scholar] [CrossRef]
- Espinola-Klein, C.; Weisser, G.; Schmitt, V.; Schwaderlapp, M.; Munzel, T. Antithrombotic therapy in peripheral arterial disease. Front. Cardiovasc. Med. 2022, 9, 927645. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.A.; Al-Omran, M.; Creager, M.A.; Anand, S.S.; Verma, S.; Bhatt, D.L. Antithrombotic Therapy for Peripheral Artery Disease: Recent Advances. J. Am. Coll. Cardiol. 2018, 71, 2450–2467. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.-B.; Bartelink, M.-L.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.-P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. Endorsed by: The European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur. Heart J. 2018, 39, 763–816. [Google Scholar] [CrossRef]
- Abramson, B.L.; Al-Omran, M.; Anand, S.S.; Albalawi, Z.; Coutinho, T.; de Mestral, C.; Dubois, L.; Gill, H.L.; Greco, E.; Guzman, R.; et al. Canadian Cardiovascular Society 2022 Guidelines for Peripheral Arterial Disease. Can. J. Cardiol. 2022, 38, 560–587. [Google Scholar] [CrossRef]
- Frank, U.; Nikol, S.; Belch, J.; Boc, V.; Brodmann, M.; Carpentier, P.H.; Chraim, A.; Canning, C.; Dimakakos, E.; Gottsäter, A.; et al. ESVM Guideline on peripheral arterial disease. Vasa 2019, 48 (Suppl. 102), 1–79. [Google Scholar] [CrossRef]
- Gornik, H.L.; Aronow, H.D.; Goodney, P.P.; Arya, S.; Brewster, L.P.; Byrd, L.; Chandra, V.; Drachman, D.E.; Eaves, J.M.; Ehrman, J.K.; et al. 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS Guideline for the Management of Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2024, 149, e1313–e1410. [Google Scholar] [CrossRef]
- Berger, J.S.; Krantz, M.J.; Kittelson, J.M.; Hiatt, W.R. Aspirin for the Prevention of Cardiovascular Events in Patients With Peripheral Artery Disease: A Meta-analysis of Randomized Trials. JAMA 2009, 301, 1909–1919. [Google Scholar] [CrossRef] [PubMed]
- Cacoub, P.P.; Abola, M.T.B.; Baumgartner, I.; Bhatt, D.L.; Creager, M.A.; Liau, C.-S.; Goto, S.; Röther, J.; Steg, P.G.; Hirsch, A.T. Cardiovascular risk factor control and outcomes in peripheral artery disease patients in the Reduction of Atherothrombosis for Continued Health (REACH) Registry. Atherosclerosis 2009, 204, e86–e92. [Google Scholar] [CrossRef]
- Guirgis, M.; Thompson, P.; Jansen, S. Review of aspirin and clopidogrel resistance in peripheral arterial disease. J. Vasc. Surg. 2017, 66, 1576–1586. [Google Scholar] [CrossRef]
- Majumdar, M.; Waller, D.; Poyant, J.; McElroy, I.; Lella, S.; Feldman, Z.M.; Levine, E.; Kim, Y.; Nuzzolo, K.; Kirshkaln, A.; et al. Variability of antiplatelet response in patients with peripheral artery disease. J. Vasc. Surg. 2023, 77, 208–215.e3. [Google Scholar] [CrossRef]
- Kim, Y.; Patel, S.S.; McElroy, I.E.; DeCarlo, C.; Bellomo, T.R.; Majumdar, M.; Lella, S.K.; Mohebali, J.; Dua, A. A systematic review of thromboelastography utilization in vascular and endovascular surgery. J. Vasc. Surg. 2022, 75, 1107–1115. [Google Scholar] [CrossRef]
- Hartmann, J.; Murphy, M.; Dias, J.D. Viscoelastic Hemostatic Assays: Moving from the Laboratory to the Site of Care-A Review of Established and Emerging Technologies. Diagnostics 2020, 10, 118. [Google Scholar] [CrossRef]
- Kietaibl, S.; Ahmed, A.; Afshari, A.; Albaladejo, P.; Aldecoa, C.; Barauskas, G.; De Robertis, E.; Faraoni, D.; Filipescu, D.C.; Fries, D.; et al. Management of severe peri-operative bleeding: Guidelines from the European Society of Anaesthesiology and Intensive Care: Second update 2022. Eur. J. Anaesthesiol. 2023, 40, 226–304. [Google Scholar] [CrossRef] [PubMed]
- Dias, J.D.; Sauaia, A.; Achneck, H.E.; Hartmann, J.; Moore, E.E. Thromboelastography-guided therapy improves patient blood management and certain clinical outcomes in elective cardiac and liver surgery and emergency resuscitation: A systematic review and analysis. J. Thromb. Haemost. 2019, 17, 984–994. [Google Scholar] [CrossRef]
- Dias, J.D.; Levy, J.H.; Tanaka, K.A.; Zacharowski, K.; Hartmann, J. Viscoelastic haemostatic assays to guide therapy in elective surgery: An updated systematic review and meta-analysis. Anaesthesia 2025, 80, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Casselman, F.P.A.; Lance, M.D.; Ahmed, A.; Ascari, A.; Blanco-Morillo, J.; Bolliger, D.; Eid, M.; Erdoes, G.; Haumann, R.G.; Jeppsson, A.; et al. 2024 EACTS/EACTAIC Guidelines on patient blood management in adult cardiac surgery in collaboration with EBCP. Eur. J. Cardiothorac. Surg. 2024, 67, ezae352. [Google Scholar] [CrossRef]
- Raphael, J.; Mazer, C.D.; Subramani, S.; Schroeder, A.; Abdalla, M.; Ferreira, R.; Roman, P.E.; Patel, N.; Welsby, I.; Greilich, P.E.; et al. Society of Cardiovascular Anesthesiologists Clinical Practice Improvement Advisory for Management of Perioperative Bleeding and Hemostasis in Cardiac Surgery Patients. Anesth. Analg. 2019, 129, 1209–1221. [Google Scholar] [CrossRef]
- Lanigan, M.; Siers, D.; Schramski, M.; Shaffer, A.; John, R.; Knoper, R.; Huddleston, S.; Gunn-Sandell, L.; Kaizer, A.; Perry, T.E. The Adherence to an Intraoperative Blood Product Transfusion Algorithm Is Associated with Reduced Blood Product Transfusions in Cardiac Surgical Patients Undergoing Coronary Artery Bypass Grafts and Aortic and/or Valve Replacement Surgery: A Single-Center, Observational Study. J. Cardiothorac. Vasc. Anesth. 2024, 38, 1135–1143. [Google Scholar] [CrossRef]
- Hartmann, J.; Curzen, N. Modified Thromboelastography for Peri-interventional Assessment of Platelet Function in Cardiology Patients: A Narrative Review. Semin. Thromb. Hemost. 2023, 49, 192–200. [Google Scholar] [CrossRef]
- Dias, J.D.; Lopez-Espina, C.G.; Bliden, K.; Gurbel, P.; Hartmann, J.; Achneck, H.E. TEG®6s system measures the contributions of both platelet count and platelet function to clot formation at the site-of-care. Platelets 2020, 31, 932–938. [Google Scholar] [CrossRef] [PubMed]
- Dias, J.D.; Pottgiesser, T.; Hartmann, J.; Duerschmied, D.; Bode, C.; Achneck, H.E. Comparison of three common whole blood platelet function tests for in vitro P2Y12 induced platelet inhibition. J. Thromb. Thrombolysis 2020, 50, 135–143. [Google Scholar] [CrossRef]
- Tantry, U.S.; Hartmann, J.; Neal, M.D.; Schöechl, H.; Bliden, K.P.; Agarwal, S.; Mason, D.; Dias, J.D.; Mahla, E.; Gurbel, P.A. The role of viscoelastic testing in assessing peri-interventional platelet function and coagulation. Platelets 2022, 33, 520–530. [Google Scholar] [CrossRef]
- Halvorsen, S.; Mehilli, J.; Cassese, S.; Hall, T.S.; Abdelhamid, M.; Barbato, E.; De Hert, S.; de Laval, I.; Geisler, T.; Hinterbuchner, L.; et al. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur. Heart J. 2022, 43, 3826–3924. [Google Scholar] [CrossRef]
- Gurbel, P.A.; Bliden, K.P.; Navickas, I.A.; Mahla, E.; Dichiara, J.; Suarez, T.A.; Antonino, M.J.; Tantry, U.S.; Cohen, E. Adenosine diphosphate-induced platelet-fibrin clot strength: A new thrombelastographic indicator of long-term poststenting ischemic events. Am. Heart J. 2010, 160, 346–354. [Google Scholar] [CrossRef]
- Jeong, Y.H.; Bliden, K.P.; Shuldiner, A.R.; Tantry, U.S.; Gurbel, P.A. Thrombin-induced platelet-fibrin clot strength: Relation to high on-clopidogrel platelet reactivity, genotype, and post-percutaneous coronary intervention outcomes. Thromb. Haemost. 2014, 111, 713–724. [Google Scholar] [CrossRef] [PubMed]
- Kwon, O.; Ahn, J.-H.; Koh, J.-S.; Park, Y.; Hwang, S.J.; Tantry, U.S.; A Gurbel, P.; Hwang, J.-Y.; Jeong, Y.-H. Platelet-fibrin clot strength and platelet reactivity predicting cardiovascular events after percutaneous coronary interventions. Eur. Heart J. 2024, 45, 2217–2231. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.-F.; Han, Y.-L.; Zhang, J.-H.; Wang, J.; Zhang, Y.; Xu, B.; Gao, Z.; Qiao, S.-B.; Chen, J.; Wu, Y.; et al. Comparing of light transmittance aggregometry and modified thrombelastograph in predicting clinical outcomes in Chinese patients undergoing coronary stenting with clopidogrel. Chin. Med. J. 2015, 128, 774–779. [Google Scholar] [CrossRef]
- Gurbel, P.A.; Bliden, K.P.; Guyer, K.; Cho, P.W.; Zaman, K.A.; Kreutz, R.P.; Bassi, A.K.; Tantry, U.S. Platelet reactivity in patients and recurrent events post-stenting: Results of the PREPARE POST-STENTING Study. J. Am. Coll. Cardiol. 2005, 46, 1820–1826. [Google Scholar] [CrossRef]
- Majumdar ML, S.; Waller, D.; Feldman, Z.M.; Sumpio, B.J.; Kim, Y.; Decarlo, C.S.; Cardenas, J.C.; Hall, R.P.; Nuzzolo, K.; Kirshkaln, A.; et al. Usage of Thromboelastography With Platelet Mapping Assay to Predict Graft Thrombosis in Lower Extremity Revascularization. J. Vasc. Surg. 2022, 75, E53–E54. [Google Scholar] [CrossRef]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Bonaca, M.P.; Bauersachs, R.M.; Anand, S.S.; Debus, E.S.; Nehler, M.R.; Patel, M.R.; Fanelli, F.; Capell, W.H.; Diao, L.; Jaeger, N.; et al. Rivaroxaban in Peripheral Artery Disease after Revascularization. New Engl. J. Med. 2020, 382, 1994–2004. [Google Scholar] [CrossRef]
- Eikelboom, J.W.; Connolly, S.J.; Bosch, J.; Dagenais, G.R.; Hart, R.G.; Shestakovska, O.; Diaz, R.; Alings, M.; Lonn, E.M.; Anand, S.S.; et al. Rivaroxaban with or without Aspirin in Stable Cardiovascular Disease. New Engl. J. Med. 2017, 377, 1319–1330. [Google Scholar] [CrossRef]
- Tang, Y.-D.; Wang, W.; Yang, M.; Zhang, K.; Chen, J.; Qiao, S.; Yan, H.; Wu, Y.; Huang, X.; Xu, B.; et al. Randomized Comparisons of Double-Dose Clopidogrel or Adjunctive Cilostazol Versus Standard Dual Antiplatelet in Patients with High Posttreatment Platelet Reactivity: Results of the CREATIVE Trial. Circulation 2018, 137, 2231–2245. [Google Scholar] [CrossRef]
- Cayla, G.; Cuisset, T.; Silvain, J.; Leclercq, F.; Manzo-Silberman, S.; Saint-Etienne, C.; Delarche, N.; Bellemain-Appaix, A.; Range, G.; El Mahmoud, R.; et al. Platelet function monitoring to adjust antiplatelet therapy in elderly patients stented for an acute coronary syndrome (ANTARCTIC): An open-label, blinded-endpoint, randomised controlled superiority trial. Lancet 2016, 388, 2015–2022. [Google Scholar] [CrossRef] [PubMed]
- Elmahdy, M.F.; Antoniucci, D. ARCTIC: Additional proof against antiplatelet adjusted therapy. Glob. Cardiol. Sci. Pract. 2013, 2013, 130–132. [Google Scholar] [CrossRef]
- Price, M.J.; Angiolillo, D.J.; Teirstein, P.S.; Lillie, E.; Manoukian, S.V.; Berger, P.B.; Tanguay, J.-F.; Cannon, C.P.; Topol, E.J. Platelet reactivity and cardiovascular outcomes after percutaneous coronary intervention: A time-dependent analysis of the Gauging Responsiveness with a VerifyNow P2Y12 assay: Impact on Thrombosis and Safety (GRAVITAS) trial. Circulation 2011, 124, 1132–1137. [Google Scholar] [CrossRef]
- Majumdar, M.; Lella, S.; Hall, R.P.; Sumetsky, N.; Waller, H.D.; McElroy, I.; Sumpio, B.; Feldman, Z.M.; Kim, Y.; DeCarlo, C.; et al. Utilization of Thromboelastography with Platelet Mapping to Predict Infection and Poor Wound Healing in Postoperative Vascular Patients. Ann. Vasc. Surg. 2022, 87, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, M.; McElroy, I.; Waller, H.D.; Lella, S.; Hall, R.P.; Kirshkaln, A.; Feldman, Z.; Kim, Y.; DeCarlo, C.; Dua, A. Identifying Sex Dimorphism in Peripheral Artery Disease with Platelet Mapping. Ann. Vasc. Surg. 2023, 88, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, S.P.S.; Hall, R.P.; Morrow, K.; Patel, S.; Lee, I.; Hagos, F.; Zacharias, N.; Machlus, K.; Dua, A. The impact of sex on platelet responses to aspirin in patients with peripheral artery disease. Am. J. Hematol. 2024, 99 (Suppl. 1), S6–S12. [Google Scholar] [CrossRef] [PubMed]
- Suarez, S.; Agrawal, A.; Patel, S.B.; Grobman, B.B.; Ghandour, S.; Morena, L.; Rodriguez, A.; Machlus, K.; Roy, T.; Eagleton, M.; et al. The Impact of Sex on Antiplatelet and Anticoagulant Thromboprophylaxis in Patients with Peripheral Artery Disease Post-revascularization. Ann. Surg. 2024, 280, 463–472. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dua, A.; Cieri, I.; Rodriguez, A.; Patel, S.; Barberi, D.; Dias, J.D.; Hartmann, J. Thromboelastography to Support Clinical Decision Making in Patients with Peripheral Artery Disease. Diagnostics 2025, 15, 3113. https://doi.org/10.3390/diagnostics15243113
Dua A, Cieri I, Rodriguez A, Patel S, Barberi D, Dias JD, Hartmann J. Thromboelastography to Support Clinical Decision Making in Patients with Peripheral Artery Disease. Diagnostics. 2025; 15(24):3113. https://doi.org/10.3390/diagnostics15243113
Chicago/Turabian StyleDua, Anahita, Isabella Cieri, Adriana Rodriguez, Shiv Patel, Dawn Barberi, Joao D. Dias, and Jan Hartmann. 2025. "Thromboelastography to Support Clinical Decision Making in Patients with Peripheral Artery Disease" Diagnostics 15, no. 24: 3113. https://doi.org/10.3390/diagnostics15243113
APA StyleDua, A., Cieri, I., Rodriguez, A., Patel, S., Barberi, D., Dias, J. D., & Hartmann, J. (2025). Thromboelastography to Support Clinical Decision Making in Patients with Peripheral Artery Disease. Diagnostics, 15(24), 3113. https://doi.org/10.3390/diagnostics15243113





