Coronal CT Attenuation Measurement for Osteoporosis Screening at the Proximal Femur: A Comparative Study with the Axial Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Consideration
2.2. Study Population
2.3. Bone Mineral Density Evaluation
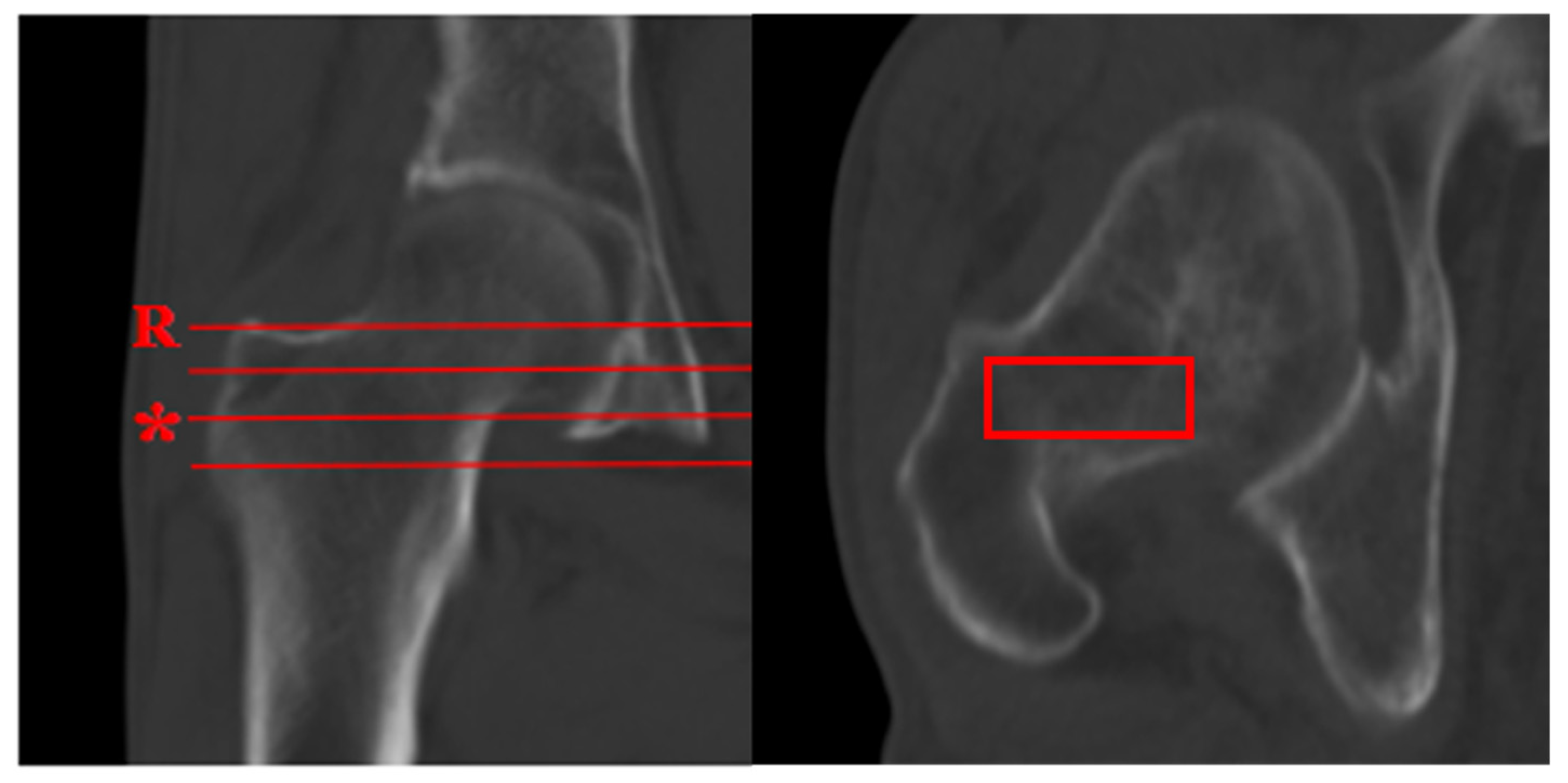
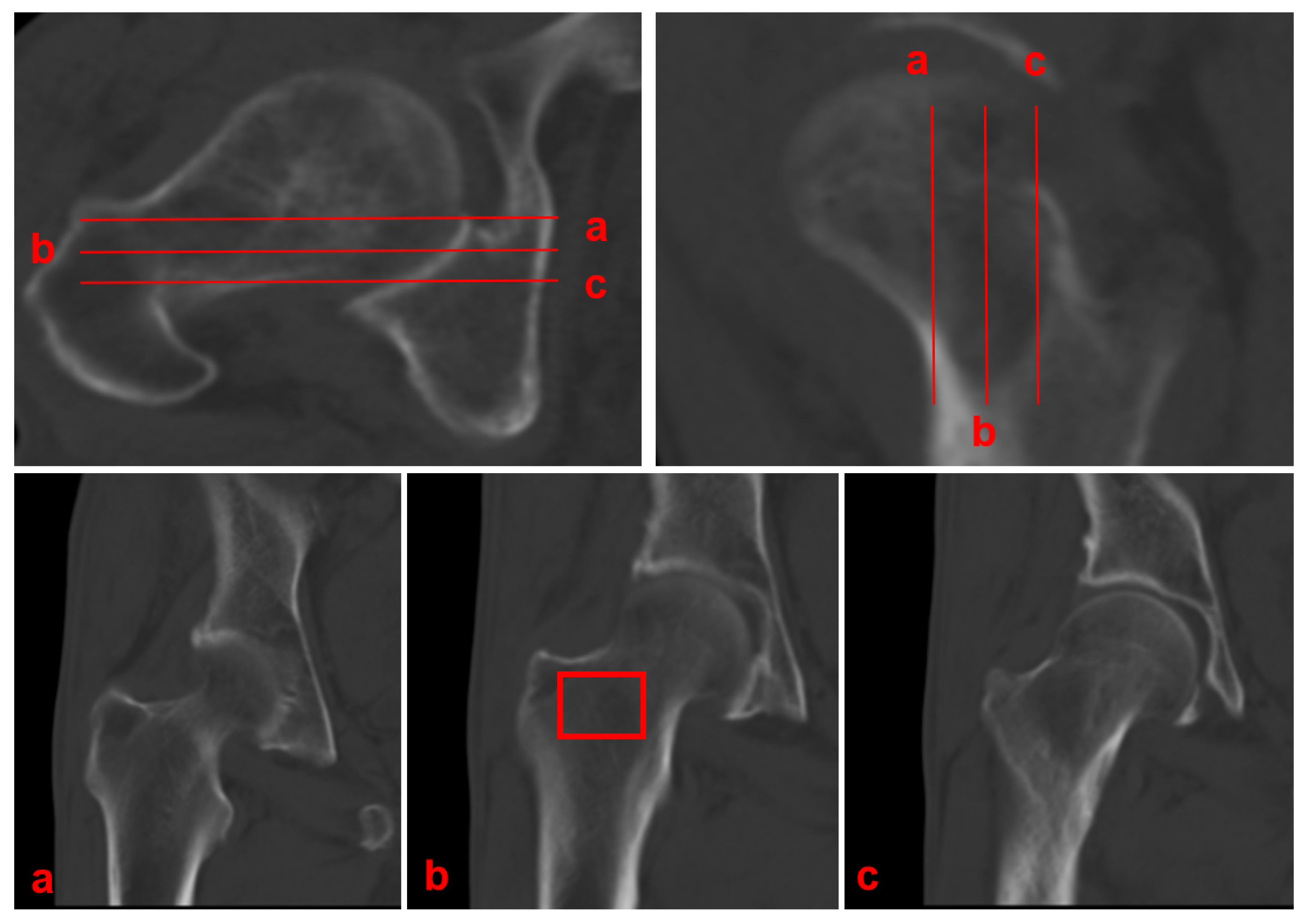
2.4. CT Attenuation Measurement
- Planar selection: Identify the coronal slice demonstrating the maximal cross-sectional area of intertrochanteric cancellous bone, which typically coincides with the central mechanical axis of the proximal femur.
- ROI placement: Position a rectangular ROI to fully encompass this cancellous bone area.
- Cortical exclusion: Carefully adjust the ROI to exclude the cortical bone boundaries.
- Data recording: Record the mean CT attenuation value (in Hounsfield Units) provided by the imaging software.
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnston, C.B.; Dagar, M. Osteoporosis in Older Adults. Med. Clin. N. Am. 2020, 104, 873–884. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Huang, X.; Tang, K.; Wu, J.; Zhou, J.; Bai, H.; Zhou, L.; Shan, S.; Luo, Z.; Cao, J.; et al. Prevalence of osteoporosis and associated factors among Chinese adults: A systematic review and modelling study. J. Glob. Health 2025, 15, 04009. [Google Scholar] [CrossRef]
- Cosman, F.; Langdahl, B.; Leder, B.Z. Treatment Sequence for Osteoporosis. Endocr. Pract. 2024, 30, 490–496. [Google Scholar] [CrossRef]
- Arceo-Mendoza, R.M.; Camacho, P.M. Postmenopausal Osteoporosis: Latest Guidelines. Endocrinol. Metab. Clin. N. Am. 2021, 50, 167–178. [Google Scholar] [CrossRef]
- Slart, R.; Punda, M.; Ali, D.S.; Bazzocchi, A.; Bock, O.; Camacho, P.; Carey, J.J.; Colquhoun, A.; Compston, J.; Engelke, K.; et al. Updated practice guideline for dual-energy X-ray absorptiometry (DXA). Eur. J. Nucl. Med. Mol. Imaging 2025, 52, 539–563. [Google Scholar] [CrossRef]
- Cheng, X.; Wang, L.; Blake, G.M.; Guglielmi, G. Update on Quantitative Computed Tomography. Semin. Musculoskelet. Radiol. 2024, 28, 557–559. [Google Scholar] [CrossRef]
- Li, Q.; Hu, B.; Yang, H.; Yang, X.; Wang, L.; Song, Y. MRI-based pedicle bone quality score: Correlation to quantitative computed tomography bone mineral density and its role in quantitative assessment of osteoporosis. Spine J. 2024, 24, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Ye, K.; Xing, Y.; Zou, D.; Zhou, F.; Zhang, Z.; Du, G.; Tian, Y. Positive correlation between the proximal femur Hounsfield units from routine CT and DXA results. J. Orthop. Res. 2023, 41, 2648–2656. [Google Scholar] [CrossRef]
- Lee, S.J.; Binkley, N.; Lubner, M.G.; Bruce, R.J.; Ziemlewicz, T.J.; Pickhardt, P.J. Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos. Int. 2016, 27, 1131–1136. [Google Scholar] [CrossRef]
- Wang, L.; Diacinti, D.; Diacinti, D.; Minisola, S.; Yajun, L. The Diagnosis of Osteoporosis, Including Opportunistic Computed Tomography: A Narrative Review. Gerontology 2025, 71, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Paderno, A.; Ataide Gomes, E.J.; Gilberg, L.; Maerkisch, L.; Teodorescu, B.; Koç, A.M.; Meyer, M. Artificial intelligence-enhanced opportunistic screening of osteoporosis in CT scan: A scoping Review. Osteoporos. Int. 2024, 35, 1681–1692. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.W.; Kim, J.H.; Yoon, S.H.; Lee, J.H.; Lee, C.H.; Shin, C.S.; Park, Y.S. Vertebral bone attenuation on low-dose chest CT: Quantitative volumetric analysis for bone fragility assessment. Osteoporos. Int. 2017, 28, 329–338. [Google Scholar] [CrossRef]
- Jain, R.K.; Lee, E.; Mathai, C.; Dako, F.; Gogineni, P.; Weiner, M.G.; Vokes, T. Using opportunistic screening with abdominal CT to identify osteoporosis and osteopenia in patients with diabetes. Osteoporos. Int. 2020, 31, 2189–2196. [Google Scholar] [CrossRef]
- Pinto, E.M.; Neves, J.R.; Teixeira, A.; Frada, R.; Atilano, P.; Oliveira, F.; Veigas, T.; Miranda, A. Efficacy of Hounsfield Units Measured by Lumbar Computer Tomography on Bone Density Assessment: A Systematic Review. Spine 2022, 47, 702–710. [Google Scholar] [CrossRef]
- Zhu, Y.; Triphuridet, N.; Yip, R.; Becker, B.J.; Wang, Y.; Yankelevitz, D.F.; Henschke, C.I. Opportunistic CT screening of osteoporosis on thoracic and lumbar spine: A meta-analysis. Clin. Imaging 2021, 80, 382–390. [Google Scholar] [CrossRef]
- Abbouchie, H.; Raju, N.; Lamanna, A.; Chiang, C.; Kutaiba, N. Screening for osteoporosis using L1 vertebral density on abdominal CT in an Australian population. Clin. Radiol. 2022, 77, e540–e548. [Google Scholar] [CrossRef] [PubMed]
- Christensen, D.L.; Nappo, K.E.; Wolfe, J.A.; Wade, S.M.; Brooks, D.I.; Potter, B.K.; Forsberg, J.A.; Tintle, S.M. Proximal Femur Hounsfield Units on CT Colonoscopy Correlate With Dual-energy X-ray Absorptiometry. Clin. Orthop. Relat. Res. 2019, 477, 850–860. [Google Scholar] [CrossRef]
- Uemura, K.; Otake, Y.; Takao, M.; Makino, H.; Soufi, M.; Iwasa, M.; Sugano, N.; Sato, Y. Development of an open-source measurement system to assess the areal bone mineral density of the proximal femur from clinical CT images. Arch. Osteoporos. 2022, 17, 17. [Google Scholar] [CrossRef]
- Andresen, J.R.; Schröder, G.; Haider, T.; Schober, H.C.; Andresen, R. Osteoporosis Assessment Using Bone Density Measurement in Hounsfield Units in the Femoral Native CT Cross-Section: A Comparison with Computed Tomography X-Ray Absorptiometry of the Hip. Diagnostics 2025, 15, 1014. [Google Scholar] [CrossRef]
- Park, S.Y.; Ha, H.I.; Lee, S.M.; Lee, I.J.; Lim, H.K. Comparison of diagnostic accuracy of 2D and 3D measurements to determine opportunistic screening of osteoporosis using the proximal femur on abdomen-pelvic CT. PLoS ONE 2022, 17, e0262025. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Adachi, J.D.; Cooper, C.; Clark, P.; Cummings, S.R.; Diaz-Curiel, M.; Harvey, N.; Hiligsmann, M.; Papaioannou, A.; Pierroz, D.D.; et al. Standardising the descriptive epidemiology of osteoporosis: Recommendations from the Epidemiology and Quality of Life Working Group of IOF. Osteoporos. Int. 2013, 24, 2763–2764. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; McCloskey, E.V.; Johansson, H.; Oden, A.; Melton, L.J., 3rd; Khaltaev, N. A reference standard for the description of osteoporosis. Bone 2008, 42, 467–475. [Google Scholar] [CrossRef]
- Engelke, K.; Chaudry, O.; Bartenschlager, S. Opportunistic Screening Techniques for Analysis of CT Scans. Curr. Osteoporos. Rep. 2023, 21, 65–76. [Google Scholar] [CrossRef]
- Chen, B.; Zou, S.P.; Wang, Y.H.; Zhou, Y.; Chen, W.Z.; Wang, A.G.; Si, W.T. [Regional CT value in prediction of proximal femoral fracture]. Zhongguo Gu Shang 2023, 36, 1142–1146. [Google Scholar] [CrossRef]
- Mousavi, S.Z.; Moshfeghinia, R.; Molavi Vardanjani, H.; Sasani, M.R. Opportunistic screening of osteoporosis by CT scan compared to DXA: A systematic review and meta-analysis. Clin. Imaging 2025, 118, 110372. [Google Scholar] [CrossRef] [PubMed]
- Emir, S.N.; Soydan, A.K.; Bulut, S.S.D. Diagnostic accuracy of axial and sagittal CT measurements for osteoporosis: A multi-vertebra evaluation. J. Clin. Densitom. 2025, 28, 101596. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Tang, M.L.; Wu, X.P.; Yuan, L.Q.; Dai, R.C.; Zhang, H.; Sheng, Z.F.; Peng, Y.Q.; Luo, X.H.; Wu, X.Y.; et al. Gender differences in a reference database of age-related femoral neck geometric parameters for Chinese population and their association with femoral neck fractures. Bone 2016, 93, 64–70. [Google Scholar] [CrossRef]
- Zarzour, F.; Aftabi, S.; Leslie, W.D. Effects of femoral neck width and hip axis length on incident hip fracture risk: A registry-based cohort study. J. Bone Miner. Res. 2025, 40, 332–338. [Google Scholar] [CrossRef]
- Zhu, X.; Mei, J.; Ni, M.; Jia, G.; Liu, S.; Dai, Y.; Zhang, Y. General anatomy and image reconstruction analysis of the proximal femoral trabecular structures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2019, 33, 1254–1259. [Google Scholar] [CrossRef]
- Ding, K.; Zhu, Y.; Li, J.; Yuwen, P.; Yang, W.; Zhang, Y.; Wang, H.; Ren, C.; Chen, W.; Zhang, Q.; et al. Age-related Changes with the Trabecular Bone of Ward’s Triangle and Neck-shaft Angle in the Proximal Femur: A Radiographic Study. Orthop. Surg. 2023, 15, 3279–3287. [Google Scholar] [CrossRef]
- Uemura, K.; Otake, Y.; Takashima, K.; Hamada, H.; Imagama, T.; Takao, M.; Sakai, T.; Sato, Y.; Okada, S.; Sugano, N. Development and validation of an open-source tool for opportunistic screening of osteoporosis from hip CT images. Bone Jt. Res. 2023, 12, 590–597. [Google Scholar] [CrossRef] [PubMed]

| Measurement | ICC | 95% CI | p * |
|---|---|---|---|
| Axial attenuation | 0.843 | 0.810–0.871 | <0.001 |
| Coronal attenuation | 0.862 | 0.833–0.887 | <0.001 |
| Patient Information | Overall (n = 708) | Normal BMD (a) (n = 14) | Osteopenia (b) (n = 108) | Osteoporosis (c) (n = 592) | p * | pa−b | pa−c | pb−c |
|---|---|---|---|---|---|---|---|---|
| Gender (M/F) | 164/543 | 2/12 | 26/75 | 136/456 | 0.605 | 0.342 | 0.447 | 0.543 |
| Interval time (days) | 20 (3, 83) | 35 (1, 83) | 38 (6, 93) | 19 (3, 78) | 0.146 | 0.458 | 0.998 | 0.050 |
| Age (years) | 64.24 ± 11.29 | 51.75 ± 11.82 | 59.60 ± 11.75 | 65.62 ± 10.98 | 0.007 | 0.204 | 0.017 | 0.027 |
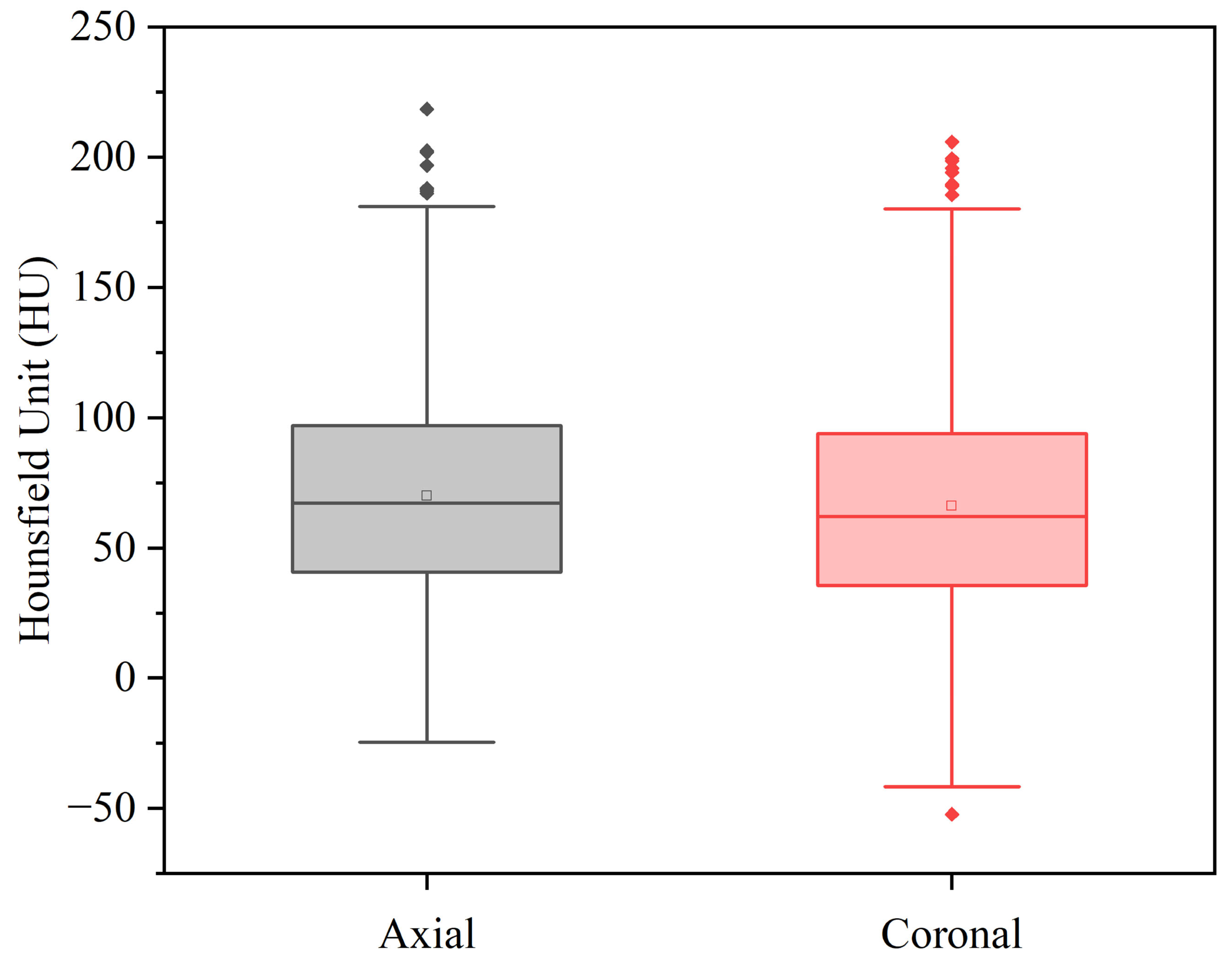
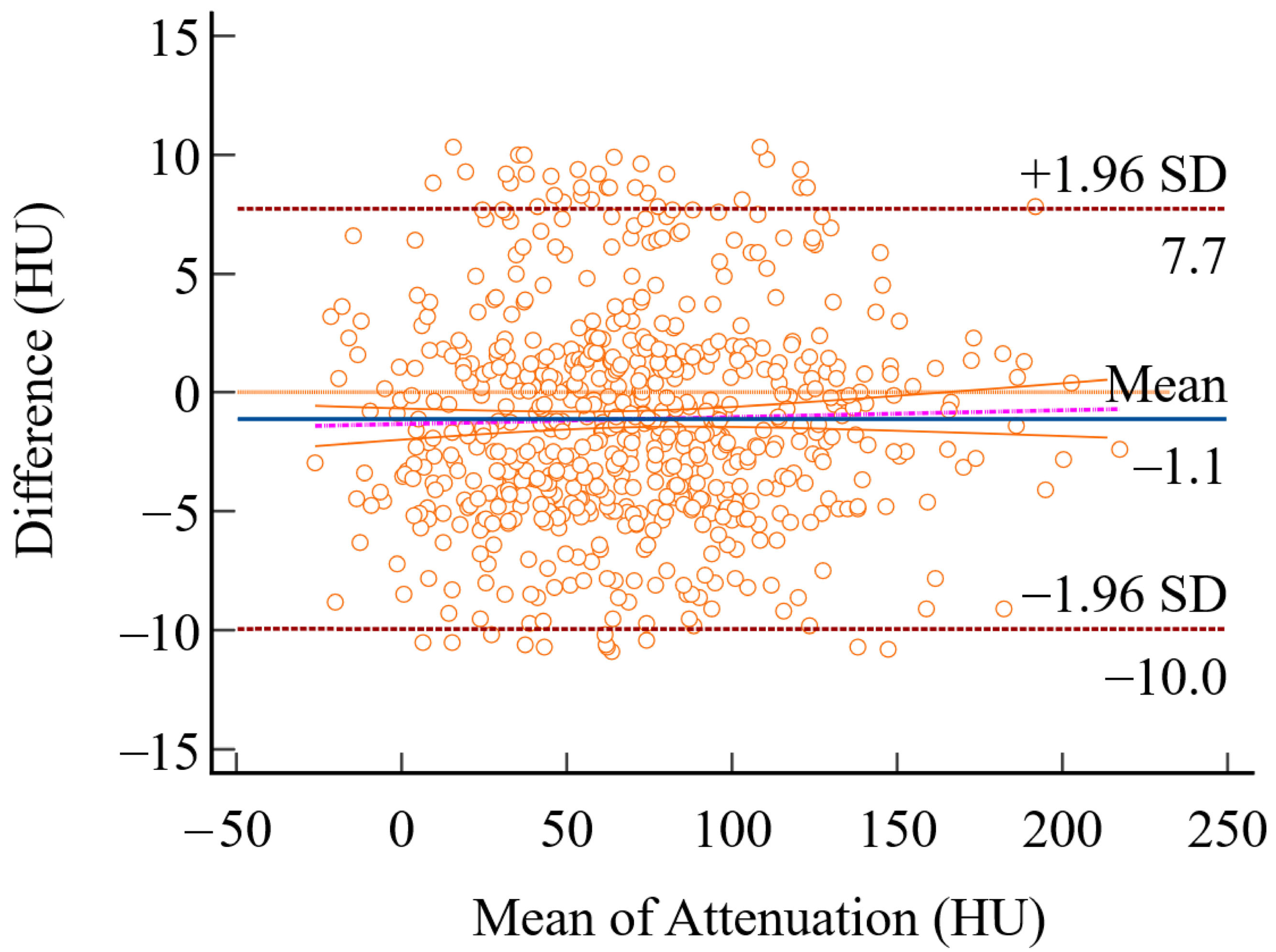
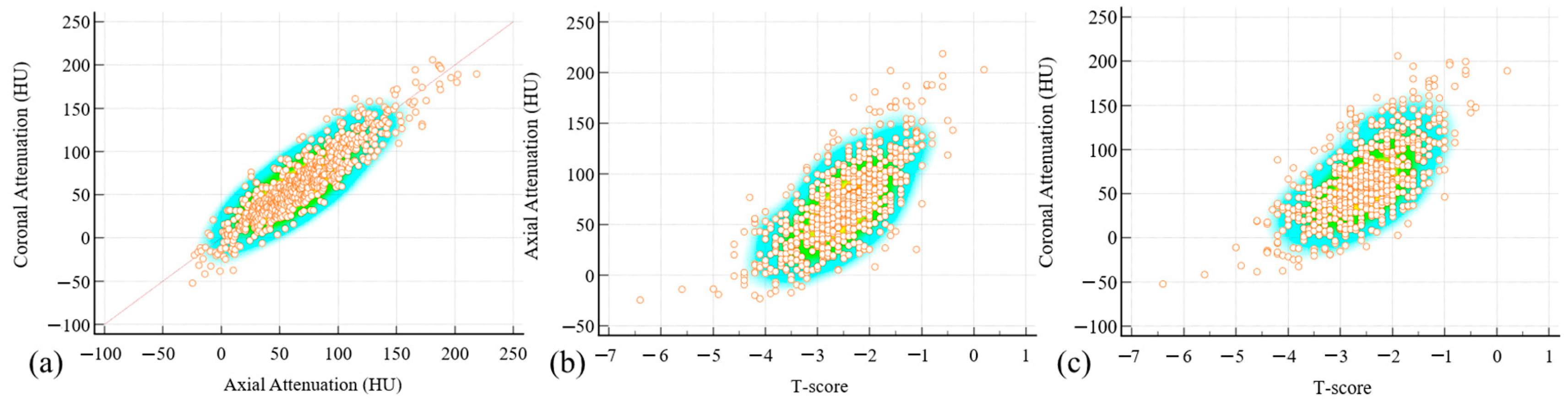
| Axial attenuation (HU) | 70.67 ± 42.30 | 170.02 ± 30.81 | 99.73 ± 36.94 | 63.37 ± 38.13 | <0.001 | <0.001 | <0.001 | <0.001 |
| Coronal attenuation (HU) | 66.13 ± 44.83 | 167.78 ± 44.69 | 96.26 ± 38.30 | 60.88 ± 43.80 | <0.001 | <0.001 | <0.001 | <0.001 |
| Femoral neck T-score | −2.52 ± 0.83 | −0.55 ± 0.30 | −1.81 ± 0.44 | −2.68 ± 0.76 | <0.001 | <0.001 | <0.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ye, K.; Qi, J.; Fan, J.; Luo, Y.; Dong, Y.; Hu, Y.; Chen, Z.; Tian, Y. Coronal CT Attenuation Measurement for Osteoporosis Screening at the Proximal Femur: A Comparative Study with the Axial Approach. Diagnostics 2025, 15, 2794. https://doi.org/10.3390/diagnostics15212794
Ye K, Qi J, Fan J, Luo Y, Dong Y, Hu Y, Chen Z, Tian Y. Coronal CT Attenuation Measurement for Osteoporosis Screening at the Proximal Femur: A Comparative Study with the Axial Approach. Diagnostics. 2025; 15(21):2794. https://doi.org/10.3390/diagnostics15212794
Chicago/Turabian StyleYe, Kaifeng, Junbo Qi, Jixing Fan, Yutian Luo, Yanlei Dong, Yuanyu Hu, Zhuo Chen, and Yun Tian. 2025. "Coronal CT Attenuation Measurement for Osteoporosis Screening at the Proximal Femur: A Comparative Study with the Axial Approach" Diagnostics 15, no. 21: 2794. https://doi.org/10.3390/diagnostics15212794
APA StyleYe, K., Qi, J., Fan, J., Luo, Y., Dong, Y., Hu, Y., Chen, Z., & Tian, Y. (2025). Coronal CT Attenuation Measurement for Osteoporosis Screening at the Proximal Femur: A Comparative Study with the Axial Approach. Diagnostics, 15(21), 2794. https://doi.org/10.3390/diagnostics15212794






