Agreement and Clinical Utility of the Easytone Transpalpebral Tonometer Compared with Goldmann Applanation, Tono-Pen, and Icare in Healthy Eyes
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Device-Specific Procedures
2.3. Statistical Analysis
3. Results
3.1. Inter-Observer Agreement
3.2. Comparison of Mean IOP Values
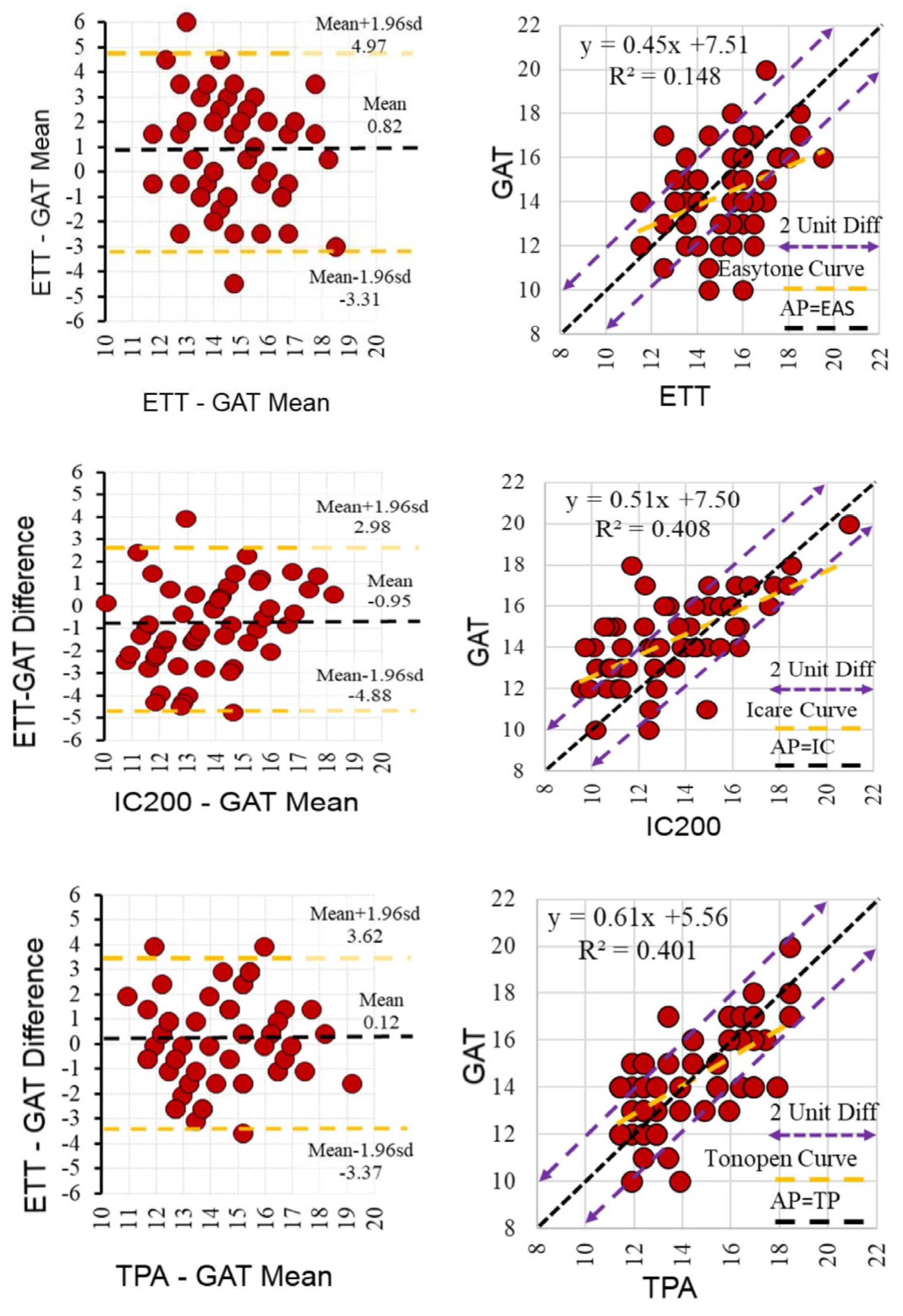
3.3. Agreement Analysis Between Devices
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Comparison | p-Value |
|---|---|
| ETT vs. IC200 | <0.001 |
| ETT vs. TPA | 0.040 |
| ETT vs. GAT | 0.001 |
| IC200 vs. TPA | 0.001 |
| IC200 vs. GAT | 0.001 |
| TPA vs. GAT | 0.765 |
References
- Ertel, M.K.; Seibold, L.K.; Patnaik, J.L.; Kahook, M.Y. Comparison of intraocular pressure readings with Perkins, Tonopen, iCare 200, and iCare Home to manometry in cadaveric eyes. Int. J. Ophthalmol. 2022, 15, 2022–2027. [Google Scholar] [CrossRef]
- EIomdina, N.; Kushnarevich, N.Y. Possibilities of monitoring intraocular pressure in children using EASYTON transpalpebral tonometer. Int. Ophthalmol. 2022, 42, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Broman, A.T.; Congdon, N.G.; Bandeen-Roche, K.; Quigley, H.A. Influence of corneal structure, corneal responsiveness, and other ocular parameters on tonometric measurement of intraocular pressure. J. Glaucoma 2007, 16, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Resua, C.; Gonzalez-Meijome, J.M.; Gilino, J.; Yebra-Pimentel, E. Accuracy of the new ICare rebound tonometer vs. other portable tonometers in healthy eyes. Optom. Vis. Sci. 2006, 83, 102–107. [Google Scholar] [CrossRef]
- Lamparter, J.; Hoffmann, E.M. Messung des Augeninnendrucks (Tonometrie) mit unterschiedlichen Verfahren. [Measuring intraocular pressure by different methods]. Ophthalmologe 2009, 106, 676–682. [Google Scholar] [CrossRef]
- Yildiz, M.B.; Kose, A.O.; Celik, G.; Kizilay, O.; Imamoglu, S.; Yildiz, E. Agreement among Goldmann Applanation Tonometer, Easyton Transpalpebral Tonometer, Tonopen, and Icare in Patients with Keratoconus. Beyoglu Eye J. 2023, 8, 170–176. [Google Scholar] [CrossRef]
- Jerrome, S.; Joseph, S.; Niranjana, B.; Vidya, S.; Kumaragurupari, T.; Balagiri, S.; Senthilkumar, V.A.; Krishnadas, S.R. Evaluation of the agreement and reliability of Transpalpebral Tonometers compared with Goldmann Applanation Tonometer-A systematic Review and Meta-Analysis Protocol. Indian. J. Ophthalmol. 2023, 71, 2225–2229. [Google Scholar] [CrossRef]
- Kim, Y.W.; Park, K.H. Exogenous influences on intraocular pressure. Br. J. Ophthalmol. 2019, 103, 1209–1216. [Google Scholar] [CrossRef]
- Galgauskas, S.; Strupaite, R.; Strelkauskaite, E.; Asoklis, R. Comparison of intraocular pressure measurements with different contact tonometers in young healthy persons. Int. J. Ophthalmol. 2016, 9, 76–80. [Google Scholar] [CrossRef]
- Lin, C.W.; Wang, J.J.; Lai, C.H.; Chen, C.Y.; Lai, I.C. Assessing Agreement and Variability Among Alternative Devices for Intraocular Pressure Measurement: A Comparative Study. Clin. Ophthalmol. 2023, 17, 3453–3461. [Google Scholar] [CrossRef]
- Sharma, H.; Nainiwal, S.K.; Sarraf, A.; Porwal, R.; Sharma, V. Intraocular pressure measurement techniques: Current concepts and a review. Indian J. Clin. Exp. Ophthalmol. 2020, 6, 315–323. [Google Scholar] [CrossRef]
- Montolío-Marzo, E.; Morales-Fernández, L.; Saenz-Frances San Baldomero, F.; García-Saenz, S.; García-Feijoo, J.; Piñero, D.P.; Martínez-de-la-Casa, J.M. Easyton(R) transpalpebral versus Perkins applanation tonometry in different populations. Int. Ophthalmol. 2023, 43, 3491–3497. [Google Scholar] [CrossRef]
- del Buey Sayas, M.Á.; Pascual, P.C.; Rodriguez, N.L.; Monzon, S.M.; Ascaso, J.; Sancho, E.L. Possibilities of monitoring intraocular pressure using easyton transpalpebral tonometer. Acta Ophthalmol. 2022, 100, S275. [Google Scholar] [CrossRef]
- Sandner, D.; Böhm, A.; Kostov, S.; Pillunat, L. Measurement of the intraocular pressure with the “transpalpebral tonometer” TGDc-01 in comparison with applanation tonometry. Graefe’s Arch. Clin. Exp. Ophthalmol. 2005, 243, 563–569. [Google Scholar] [CrossRef]
- Bradfield, Y.S.; Kaminski, B.M.; Repka, M.X.; Melia, M.; Pediatric Eye Disease Investigator Group. Comparison of Tono-Pen and Goldmann applanation tonometers for measurement of intraocular pressure in healthy children. J. AAPOS 2012, 16, 242–248. [Google Scholar] [CrossRef] [PubMed]
- AlHarkan, D.H.; Al-Shamlan, F.T.; Edward, D.P.; Khan, A.O. A Comparison of Rebound to Indentation Tonometry in Supine Sedated Children with Glaucoma. Middle East Afr. J. Ophthalmol. 2016, 23, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Onochie, C.; Okoye, O.; Ogunro, A.; Aribaba, T.; Hassan, K.; Onakoya, A. Comparisons of the Tono-Pen(R) and Goldmann Applanation Tonometer in the Measurement of Intraocular Pressure of Primary Open Angle Glaucoma Patients in a Hospital Population in Southwest Nigeria. Med. Princ. Pract. 2016, 25, 566–571. [Google Scholar] [CrossRef]
- Deuter, C.M.; Schlote, T.; Hahn, G.A.; Bende, T.; Derse, M. Messung des Augeninnendrucks mit dem Tono-Pen im Vergleich zum Applanationstonometer nach Goldmann-eine klinische Studie an 100 Augen [Measurement of intraocular pressure using the Tono-Pen in comparison with Goldmann applanation tonometry-a clinical study in 100 eyes]. Klin. Monbl Augenheilkd. 2002, 219, 138–142. [Google Scholar] [CrossRef]
- Ceska, B.M.; Ferrova, K.; Filous, A.; Oskorypova, K.; Lezatkova, P.; Sedlackova, P. Srovnavaci studie meren nitroocniho tlaku aplanacni tonometrii, bezkontaktni tonometrii a TonoPenem [Comparative study of intraocular pressure measurements by Goldmann applanation tonometer, noncontact tonometer and TonoPen]. Cesk Slov. Oftalmol. 2012, 68, 43–46. Available online: https://www.ncbi.nlm.nih.gov/pubmed/22679697 (accessed on 1 February 2012).
- Kim, N.R.; Kim, C.Y.; Kim, H.; Seong, G.J.; Lee, E.S. Comparison of goldmann applanation tonometer, noncontact tonometer, and TonoPen XL for intraocular pressure measurement in different types of glaucomatous, ocular hypertensive, and normal eyes. Curr. Eye Res. 2011, 36, 295–300. [Google Scholar] [CrossRef]
- Feng, C.S.; Jin, K.W.; Yi, K.; Choi, D.G. Comparison of Intraocular Pressure Measurements Obtained by Rebound, Noncontact, and Goldmann Applanation Tonometry in Children. Am. J. Ophthalmol. 2015, 160, 937–943.e1. [Google Scholar] [CrossRef]
- Sachdeva, R.; Iordanous, Y.; Lin, T. Comparison of intraocular pressure measured by iCare tonometers and Goldmann applanation tonometer. Can. J. Ophthalmol. 2023, 58, 426–432. [Google Scholar] [CrossRef]
- Barkana, Y.; Gutfreund, S. Measurement of the difference in intraocular pressure between the sitting and lying body positions in healthy subjects: Direct comparison of the Icare Pro with the Goldmann applanation tonometer, Pneumatonometer and Tonopen XL. Clin. Exp. Ophthalmol. 2014, 42, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.E.; Yoo, C.; Kim, Y.Y. Comparison of Three Different Tonometers in Eyes with Angle Closure. Optom. Vis. Sci. 2019, 96, 124–129. [Google Scholar] [CrossRef]
- Schweier, C.; Hanson, J.V.; Funk, J.; Toteberg-Harms, M. Repeatability of intraocular pressure measurements with Icare PRO rebound, Tono-Pen AVIA, and Goldmann tonometers in sitting and reclining positions. BMC Ophthalmol. 2013, 13, 44. [Google Scholar] [CrossRef]
| Feature | ETT (Easytone Transpalpebral) | IC200 (Icare 200) | TPA (Tonopen AVIA) | GAT (Goldmann Applanation) |
|---|---|---|---|---|
| Measurement method | Transpalpebral | Rebound | Applanation | Applanation (Gold standard) |
| Direct corneal contact | No | Yes | Yes | Yes |
| Need for an anesthetic | No | No | Yes | Yes |
| Need for fluorescein | No | No | No | Yes |
| Portable | Yes | Yes | Yes | No |
| Patient position | Head tilted back, parallel to the floor | Sitting or supine | Sitting or supine | Sitting at the slit lamp |
| Measurement time | Short (1–2 s) | Short (1–2 s) | Moderate (needs anesthesia) | Longer (requires slit-lamp setup) |
| Repeatability | Moderate (affected by eyelid tone) | High | High | Very high |
| Ease of use in children | High | High | Moderate | Low |
| Advantages | No corneal contact, portable, no anesthesia | Portable, no anesthesia, reproducible | Portable, less affected by CCT | Gold standard, high accuracy |
| Disadvantages | Affected by eyelid/scleral tone, not usable with lid pathologies | Affected by corneal biomechanics | Requires anesthesia, contact-based | Needs slit lamp, anesthesia, fluorescein, and risk of infection |
| Parameter | Min–Max | Median | Mean ± SD | n (%) |
|---|---|---|---|---|
| Age (years) | 20–54 | 36.5 | 35.3 ± 7.9 | |
| Gender | ||||
| Female Male Central corneal thickness (µm) | 440–598 | 546.5 | 542.2 ± 33.3 | 29 (50.0) 29 (50.0) |
| Axial length (mm) | 21.8–26.1 | 23.4 | 23.5 ± 0.9 | |
| Spherical equivalent (D) | –2.50–+2.50 | –0.50 | –0.38 ± 0.82 | |
| Mean IOP (mmHg) | ||||
| ETT IC200 TPA GAT | 15.5 13.0 14.4 14.0 | 15.2 ± 1.7 13.4 ± 2.6 14.5 ± 2.1 14.3 ± 2.0 |
| Tonometer | Observer 1 (Mean ± SD, mmHg) | Observer 2 (Mean ± SD, mmHg) | p-Value (Wilcoxon) | ICC | 95% CI |
|---|---|---|---|---|---|
| ETT | 15.1 ± 2.0 | 15.2 ± 1.8 | 0.873 | 0.805 | 0.670–0.884 |
| IC200 | 13.3 ± 2.7 | 13.4 ± 2.7 | 0.468 | 0.910 | 0.848–0.947 |
| TPA | 14.5 ± 2.1 | 14.4 ± 2.4 | 0.329 | 0.879 | 0.795–0.928 |
| GAT | 14.3 ± 2.0 | 14.3 ± 2.0 | 1.000 | 1.000 | 1.000–1.000 |
| Comparison | ICC (95% CI) | Bias (mmHg) | 95% Limits of Agreement (mmHg) |
|---|---|---|---|
| ETT vs. GAT | 0.551 (0.242–0.734) | +0.9 | –3.5 to +5.2 |
| ETT vs. IC200 | 0.440 (0.054–0.669) | +1.8 | –2.4 to +2.3 |
| ETT vs. TPA | 0.455 | +0.7 | –3.7 to +7.3 |
| GAT vs. IC200 | 0.768 (0.607–0.862) | +1.0 | –3.2 to +5.1 |
| GAT vs. TPA | 0.772 (0.620–0.867) | –0.1 | –3.9 to +3.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kizilay, O.; Karaca, S.; Celik, G.; Yilmaz, O.F. Agreement and Clinical Utility of the Easytone Transpalpebral Tonometer Compared with Goldmann Applanation, Tono-Pen, and Icare in Healthy Eyes. Diagnostics 2025, 15, 2766. https://doi.org/10.3390/diagnostics15212766
Kizilay O, Karaca S, Celik G, Yilmaz OF. Agreement and Clinical Utility of the Easytone Transpalpebral Tonometer Compared with Goldmann Applanation, Tono-Pen, and Icare in Healthy Eyes. Diagnostics. 2025; 15(21):2766. https://doi.org/10.3390/diagnostics15212766
Chicago/Turabian StyleKizilay, Osman, Serap Karaca, Gokhan Celik, and Omer Faruk Yilmaz. 2025. "Agreement and Clinical Utility of the Easytone Transpalpebral Tonometer Compared with Goldmann Applanation, Tono-Pen, and Icare in Healthy Eyes" Diagnostics 15, no. 21: 2766. https://doi.org/10.3390/diagnostics15212766
APA StyleKizilay, O., Karaca, S., Celik, G., & Yilmaz, O. F. (2025). Agreement and Clinical Utility of the Easytone Transpalpebral Tonometer Compared with Goldmann Applanation, Tono-Pen, and Icare in Healthy Eyes. Diagnostics, 15(21), 2766. https://doi.org/10.3390/diagnostics15212766






