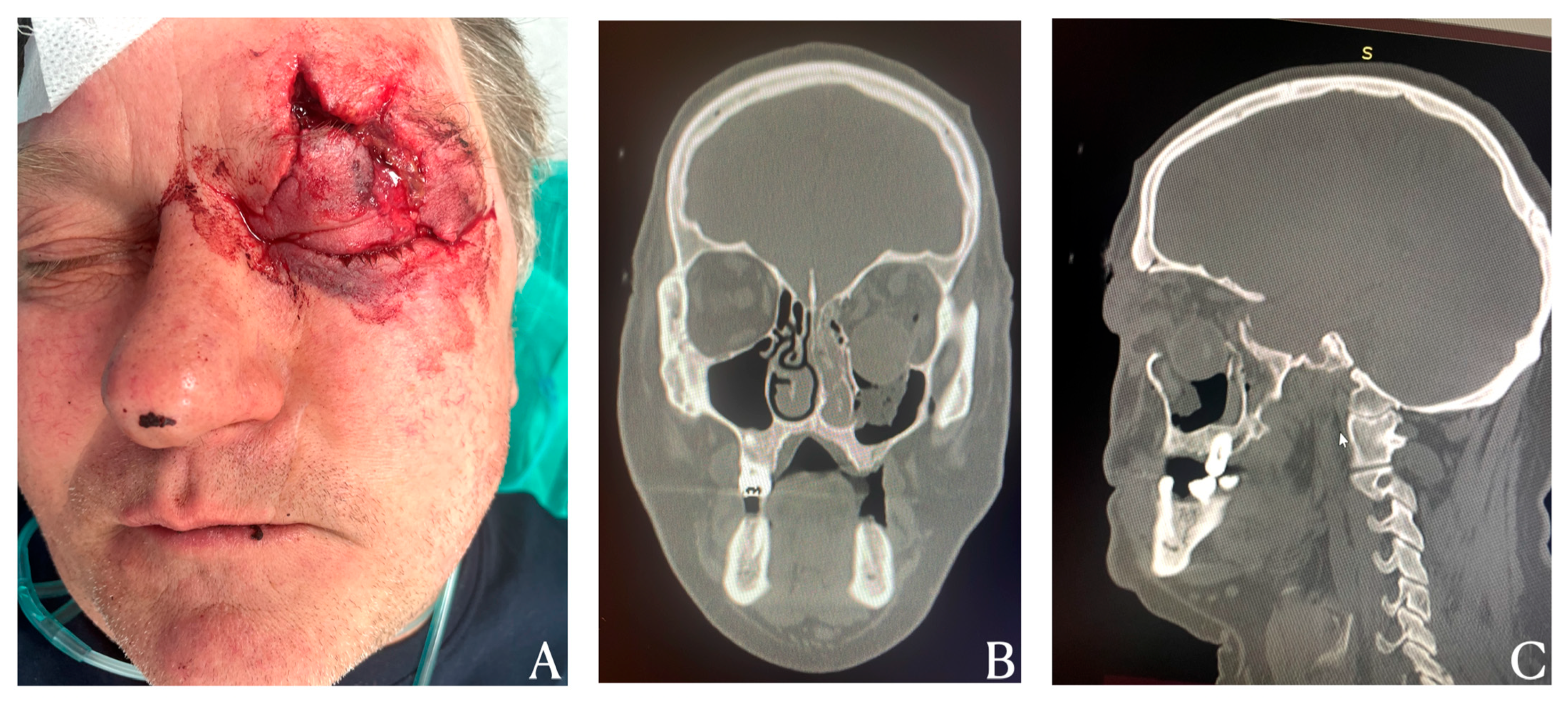
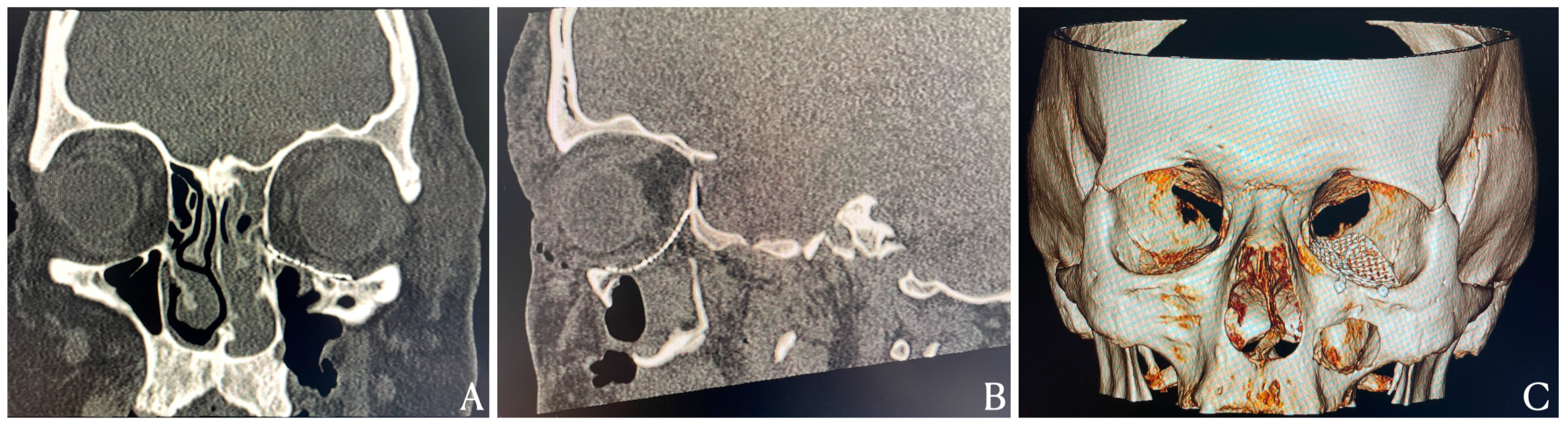
An Exceptional Case of Blow-Out Fracture with Complete Globe Dislocation into the Maxillary Sinus: Diagnostic Imaging and Surgical Reconstruction
Abstract

Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Valencia, M.R.; Miyazaki, H.; Ito, M.; Nishimura, K.; Kakizaki, H.; Takahashi, Y. Radiological findings of orbital blowout fractures: A review. Orbit 2021, 40, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Fabrega, M. Imaging of maxillofacial trauma. Oral Maxillofac. Surg. Clin. N. Am. 2023, 35, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Michalik, W.; Toppich, J.; Łuksza, A.; Bargiel, J.; Gąsiorowski, K.; Marecik, T.; Szczurowski, P.; Wyszyńska-Pawelec, G.; Gontarz, M. Exploring the correlation of epidemiological and clinical factors with facial injury severity scores in maxillofacial trauma: A comprehensive analysis. Front. Oral Health 2025, 6, 1532133. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Koryczan, P.; Zapała, J.; Gontarz, M.; Wyszyńska-Pawelec, G. Surgical treatment of enophthalmos in children and adolescents with pure orbital blowout fracture. J. Oral Sci. 2021, 63, 129–132. [Google Scholar] [CrossRef]
- Gąsiorowski, K.; Gontarz, M.; Bargiel, J.; Marecik, T.; Szczurowski, P.; Wyszyńska-Pawelec, G. Reconstructive techniques following malignant eyelid tumour excision—Our experience. J. Clin. Med. 2024, 13, 6120. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Koryczan, P.; Zapała, J.; Gontarz, M.; Wyszyńska-Pawelec, G. Comparison of the results of the treatment of enophthalmos in orbital blowout fracture in children/adolescents and adults. Dent. Med. Probl. 2021, 58, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Oliveira de Lima Junior, M.; Fontan Soares, C.; Souza Catunda, I.; de Holanda Vasconcellos, R.J. Surgical treatment of blowout fracture: A new perspective. J. Craniofac. Surg. 2023, 34, e391–e393. [Google Scholar] [CrossRef] [PubMed]
- Steel, D.A.; Mortimer, T.; Bater, M.C. Severe orbital blowout fracture: Complete displacement of the globe into the maxillary sinus. BMJ Case Rep. 2023, 16, e254055. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chattopadhyay, C.; Dev, V.; Pilania, D.; Harsh, A. Reconstruction of orbital floor fractures with titanium micromesh: Our experience. J. Maxillofac. Oral Surg. 2022, 21, 369–378. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kotecha, S.; Ferro, A.; Harrison, P.; Fan, K. Orbital Reconstruction: A Systematic Review and Meta-Analysis Evaluating the Role of Patient-Specific Implants. Oral Maxillofac. Surg. 2023, 27, 213–226. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gąsiorowski, K.; Gontarz, M.; Bargiel, J.; Marecik, T.; Wyszyńska-Pawelec, G. An Exceptional Case of Blow-Out Fracture with Complete Globe Dislocation into the Maxillary Sinus: Diagnostic Imaging and Surgical Reconstruction. Diagnostics 2025, 15, 2705. https://doi.org/10.3390/diagnostics15212705
Gąsiorowski K, Gontarz M, Bargiel J, Marecik T, Wyszyńska-Pawelec G. An Exceptional Case of Blow-Out Fracture with Complete Globe Dislocation into the Maxillary Sinus: Diagnostic Imaging and Surgical Reconstruction. Diagnostics. 2025; 15(21):2705. https://doi.org/10.3390/diagnostics15212705
Chicago/Turabian StyleGąsiorowski, Krzysztof, Michał Gontarz, Jakub Bargiel, Tomasz Marecik, and Grażyna Wyszyńska-Pawelec. 2025. "An Exceptional Case of Blow-Out Fracture with Complete Globe Dislocation into the Maxillary Sinus: Diagnostic Imaging and Surgical Reconstruction" Diagnostics 15, no. 21: 2705. https://doi.org/10.3390/diagnostics15212705
APA StyleGąsiorowski, K., Gontarz, M., Bargiel, J., Marecik, T., & Wyszyńska-Pawelec, G. (2025). An Exceptional Case of Blow-Out Fracture with Complete Globe Dislocation into the Maxillary Sinus: Diagnostic Imaging and Surgical Reconstruction. Diagnostics, 15(21), 2705. https://doi.org/10.3390/diagnostics15212705







