Incidence of Anxiety Diagnosis up to Four Years Post SARS-CoV-2 Infection in the Montefiore Medical Center in the Bronx and New York
Abstract
1. Introduction
2. Methods
2.1. Data Sources
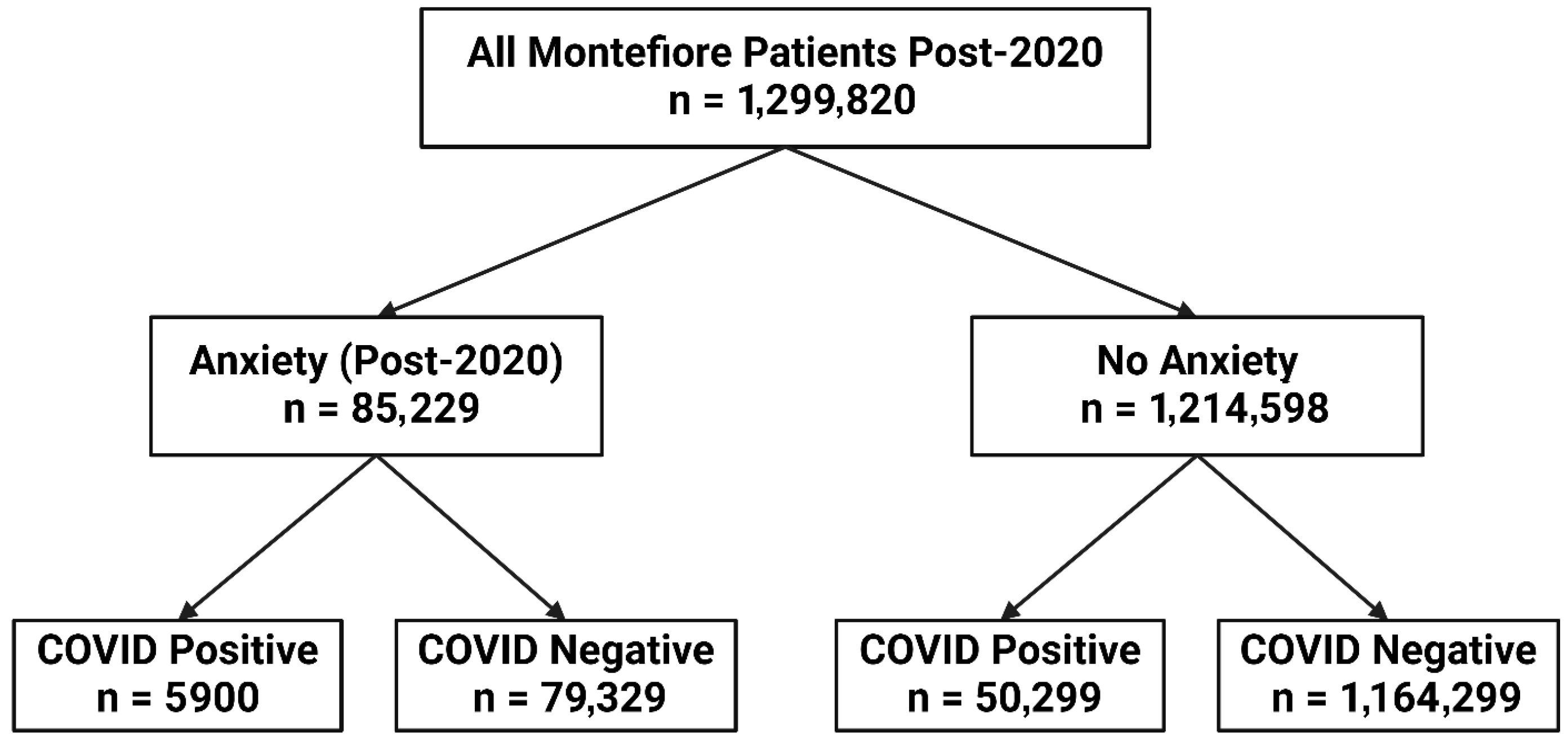
2.2. Study Population
2.3. Variables
2.4. Statistical Analysis
3. Results
3.1. Unmatched Data
3.2. Matched Data
4. Discussion
4.1. Demographic Factors
4.2. Comorbidity Factors
4.3. Matched Cohort
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Desai, A.D.; Wan, E.Y. Post-COVID-19 Condition. Annu. Rev. Med. 2023, 74, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Iosifescu, A.L.; Hoogenboom, W.S.; Buczek, A.J.; Fleysher, R.; Duong, T.Q. New-onset and persistent neurological and psychiatric sequelae of COVID-19 compared to influenza: A retrospective cohort study in a large New York City healthcare network. Int. J. Methods Psychiatr. Res. 2022, 31, e1914. [Google Scholar] [CrossRef]
- Zou, Q.; Tang, Y.; Jiang, C.; Lin, P.; Tian, J.; Sun, S. Prevalence of anxiety, depressive and insomnia symptoms among the different groups of people during COVID-19 pandemic: An overview of systematic reviews and meta-analyses. Front. Psychol. 2022, 13, 1024668. [Google Scholar] [CrossRef]
- Pashazadeh Kan, F.; Raoofi, S.; Rafiei, S.; Khani, S.; Hosseinifard, H.; Tajik, F.; Raoofi, N.; Ahmadi, S.; Aghalou, S.; Torabi, F.; et al. A systematic review of the prevalence of anxiety among the general population during the COVID-19 pandemic. J. Affect. Disord. 2021, 293, 391–398. [Google Scholar] [CrossRef]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Maunder, R.G.; Heeney, N.D.; Kiss, A.; Hunter, J.J.; Jeffs, L.P.; Ginty, L.; Johnstone, J.; Loftus, C.A.; Wiesenfeld, L.A. Psychological impact of the COVID-19 pandemic on hospital workers over time: Relationship to occupational role, living with children and elders, and modifiable factors. Gen. Hosp. Psychiatry 2021, 71, 88–94. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Zaninotto, P.; Iob, E.; Demakakos, P.; Steptoe, A. Immediate and Longer-Term Changes in the Mental Health and Well-being of Older Adults in England During the COVID-19 Pandemic. JAMA Psychiatry 2022, 79, 151–159. [Google Scholar] [CrossRef]
- Wu, Y.; Zhang, C.; Liu, H.; Duan, C.; Li, C.; Fan, J.; Li, H.; Chen, L.; Xu, H.; Li, X.; et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am. J. Obstet. Gynecol. 2020, 223, e240–e241. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Perez, I.; Zamanillo Campos, R.; Goncalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Anand, H.; Ende, V.; Singh, G.; Qureshi, I.; Duong, T.Q.; Mehler, M.F. Nervous System-Systemic Crosstalk in SARS-CoV-2/COVID-19: A Unique Dyshomeostasis Syndrome. Front. Neurosci. 2021, 15, 727060. [Google Scholar] [CrossRef] [PubMed]
- Veleri, S. Neurotropism of SARS-CoV-2 and neurological diseases of the central nervous system in COVID-19 patients. Exp. Brain Res. 2022, 240, 9–25. [Google Scholar] [CrossRef]
- Steenblock, C.; Todorov, V.; Kanczkowski, W.; Eisenhofer, G.; Schedl, A.; Wong, M.L.; Licinio, J.; Bauer, M.; Young, A.H.; Gainetdinov, R.R.; et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the neuroendocrine stress axis. Mol. Psychiatry 2020, 25, 1611–1617. [Google Scholar] [CrossRef]
- Robb, C.E.; de Jager, C.A.; Ahmadi-Abhari, S.; Giannakopoulou, P.; Udeh-Momoh, C.; McKeand, J.; Price, G.; Car, J.; Majeed, A.; Ward, H.; et al. Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK. Front. Psychiatry 2020, 11, 591120. [Google Scholar] [CrossRef]
- Dziedzic, A.; Saluk-Bijak, J.; Miller, E.; Niemcewicz, M.; Bijak, M. The Impact of SARS-CoV-2 Infection on the Development of Neurodegeneration in Multiple Sclerosis. Int. J. Mol. Sci. 2021, 22, 1804. [Google Scholar] [CrossRef]
- Yang, Y.; Cai, K.; Qi, J.; Wang, F.; Yang, R.; Wang, L.; Lyu, J.; Hu, J.; Wu, Y.; Cai, M. Exploring the moderated mediation of stress and media use: Social support’s impact on anxiety among older adults during the COVID-19 pandemic—Insights from a large-scale cross-sectional study in China. J. Affect. Disord. 2024, 367, 229–237. [Google Scholar] [CrossRef]
- Rickham, P.P. Human Experimentation. Code of Ethics of the World Medical Association. Declaration of Helsinki. Br. Med. J. 1964, 2, 177. [Google Scholar] [CrossRef]
- Changela, S.; Ashraf, S.; Lu, J.Y.; Duong, K.E.; Henry, S.; Wang, S.H.; Duong, T.Q. New-onset gastrointestinal disorders in COVID-19 patients 3.5 years post-infection in the inner-city population in the Bronx. Sci. Rep. 2024, 14, 31850. [Google Scholar] [CrossRef]
- Hadidchi, R.; Al-Ani, Y.; Piskun, H.; Pakan, R.; Duong, K.; Jamil, H.; Wang, S.; Henry, S.; Maurer, C.; Duong, T. Long-term outcomes of patients with Parkinson’s disease 3.5 years post SARS-CoV-2 infection in an inner-city population in the Bronx. Eur. J. Neurol. 2025, 32, e70013. [Google Scholar] [CrossRef] [PubMed]
- Mahesh, T.; Changela, S.; Duong, K.S.; Henry, S.; Wang, S.H.; Duong, T.Q. New-onset conjunctivitis 3.5 years post SARS-CoV-2 infection in an inner-city population in the Bronx. BMJ Open Ophthalmol. 2025, 10, e001993. [Google Scholar] [CrossRef] [PubMed]
- Hadidchi, R.; Pakan, R.; Alamuri, T.; Cercizi, N.; Al-Ani, Y.; Wang, S.H.; Henry, S.; Duong, T.Q. Long COVID-19 outcomes of patients with pre-existing dementia. J. Alzheimer’s Dis. 2025, 103, 605–615. [Google Scholar] [CrossRef]
- Hadidchi, R.; Wang, S.H.; Rezko, D.; Henry, S.; Coyle, P.K.; Duong, T.Q. SARS-CoV-2 infection increases long-term multiple sclerosis disease activity and all-cause mortality in an underserved inner-city population. Mult. Scler. Relat. Disord. 2024, 86, 105613. [Google Scholar] [CrossRef]
- Pakan, R.; Hadidchi, R.; Al-Ani, Y.; Piskun, H.; Duong, K.S.; Henry, S.; Wang, S.; Maurer, C.W.; Duong, T.Q. Long-Term Outcomes of Patients with Pre-Existing Essential Tremor After SARS-CoV-2 Infection. Diagnostics 2024, 14, 2774. [Google Scholar] [CrossRef]
- Eligulashvili, A.; Darrell, M.; Miller, C.; Lee, J.; Congdon, S.; Lee, J.S.; Hsu, K.; Yee, J.; Hou, W.; Islam, M.; et al. COVID-19 Patients in the COVID-19 Recovery and Engagement (CORE) Clinics in the Bronx. Diagnostics 2022, 13, 119. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.Y.; Hou, W.; Duong, T.Q. Longitudinal prediction of hospital-acquired acute kidney injury in COVID-19: A two-center study. Infection 2022, 50, 109–119. [Google Scholar] [CrossRef]
- Lu, J.Y.; Boparai, M.S.; Shi, C.; Henninger, E.M.; Rangareddy, M.; Veeraraghavan, S.; Mirhaji, P.; Fisher, M.C.; Duong, T.Q. Long-term outcomes of COVID-19 survivors with hospital AKI: Association with time to recovery from AKI. Nephrol. Dial. Transplant. 2023, 38, 2160–2169. [Google Scholar] [CrossRef]
- Xu, A.Y.; Wang, S.H.; Duong, T.Q. Patients with prediabetes are at greater risk of developing diabetes 5 months postacute SARS-CoV-2 infection: A retrospective cohort study. BMJ Open Diabetes Res. Care 2023, 11, e003257. [Google Scholar] [CrossRef]
- Zhang, V.; Fisher, M.; Hou, W.; Zhang, L.; Duong, T.Q. Incidence of New-Onset Hypertension Post-COVID-19: Comparison With Influenza. Hypertension 2023, 80, 2135–2148. [Google Scholar] [CrossRef]
- Hripcsak, G.; Duke, J.D.; Shah, N.H.; Reich, C.G.; Huser, V.; Schuemie, M.J.; Suchard, M.A.; Park, R.W.; Wong, I.C.; Rijnbeek, P.R.; et al. Observational Health Data Sciences and Informatics (OHDSI): Opportunities for Observational Researchers. Stud. Health Technol. Inform. 2015, 216, 574–578. [Google Scholar] [PubMed]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef]
- Ambrose, A.J.H. Inequities During COVID-19. Pediatrics 2020, 146, e20201501. [Google Scholar] [CrossRef] [PubMed]
- Abrams, E.M.; Szefler, S.J. COVID-19 and the impact of social determinants of health. Lancet Respir. Med. 2020, 8, 659–661. [Google Scholar] [CrossRef] [PubMed]
- Singu, S.; Acharya, A.; Challagundla, K.; Byrareddy, S.N. Impact of Social Determinants of Health on the Emerging COVID-19 Pandemic in the United States. Front. Public. Health 2020, 8, 406. [Google Scholar] [CrossRef]
- Green, H.; Fernandez, R.; MacPhail, C. The social determinants of health and health outcomes among adults during the COVID-19 pandemic: A systematic review. Public. Health Nurs. 2021, 38, 942–952. [Google Scholar] [CrossRef]
- Acosta, A.M.; Garg, S.; Pham, H.; Whitaker, M.; Anglin, O.; O’Halloran, A.; Milucky, J.; Patel, K.; Taylor, C.; Wortham, J.; et al. Racial and Ethnic Disparities in Rates of COVID-19-Associated Hospitalization, Intensive Care Unit Admission, and In-Hospital Death in the United States From March 2020 to February 2021. JAMA Netw. Open 2021, 4, e2130479. [Google Scholar] [CrossRef]
- Correa-Agudelo, E.; Mersha, T.B.; Hernandez, A.; Branscum, A.J.; MacKinnon, N.J.; Cuadros, D.F. Identification of Vulnerable Populations and Areas at Higher Risk of COVID-19 Related Mortality in the U.S. medRxiv 2020. [Google Scholar] [CrossRef]
- Magesh, S.; John, D.; Li, W.T.; Li, Y.; Mattingly-App, A.; Jain, S.; Chang, E.Y.; Ongkeko, W.M. Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status: A Systematic-Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2134147. [Google Scholar] [CrossRef] [PubMed]
- Kanwal, A.; Delijani, K.; Sadowsky, D.J.; Zulty, M.; Tefera, E.; Weisman, D.S. The Effect of Race and Socioeconomic Status on Hospitalized Patients with COVID-19 Infection. J. Community Hosp. Intern. Med. Perspect. 2022, 12, 14–19. [Google Scholar] [CrossRef]
- Saltzman, L.Y.; Lesen, A.E.; Henry, V.; Hansel, T.C.; Bordnick, P.S. COVID-19 Mental Health Disparities. Health Secur. 2021, 19, S5–S13. [Google Scholar] [CrossRef]
- Al Maqbali, M.; Alsayed, A.; Hughes, C.; Hacker, E.; Dickens, G.L. Stress, anxiety, depression and sleep disturbance among healthcare professional during the COVID-19 pandemic: An umbrella review of 72 meta-analyses. PLoS ONE 2024, 19, e0302597. [Google Scholar] [CrossRef]
- Sun, P.; Wang, M.; Song, T.; Wu, Y.; Luo, J.; Chen, L.; Yan, L. The Psychological Impact of COVID-19 Pandemic on Health Care Workers: A Systematic Review and Meta-Analysis. Front. Psychol. 2021, 12, 626547. [Google Scholar] [CrossRef]
- Hsu, H.E.; Ashe, E.M.; Silverstein, M.; Hofman, M.; Lange, S.J.; Razzaghi, H.; Mishuris, R.G.; Davidoff, R.; Parker, E.M.; Penman-Aguilar, A.; et al. Race/Ethnicity, Underlying Medical Conditions, Homelessness, and Hospitalization Status of Adult Patients with COVID-19 at an Urban Safety-Net Medical Center—Boston, Massachusetts, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 864–869. [Google Scholar] [CrossRef]
- Cummings, J.R.; Allen, L.; Clennon, J.; Ji, X.; Druss, B.G. Geographic Access to Specialty Mental Health Care Across High- and Low-Income US Communities. JAMA Psychiatry 2017, 74, 476–484. [Google Scholar] [CrossRef]
- Vinkers, C.H.; Kuzminskaite, E.; Lamers, F.; Giltay, E.J.; Penninx, B. An integrated approach to understand biological stress system dysregulation across depressive and anxiety disorders. J. Affect. Disord. 2021, 283, 139–146. [Google Scholar] [CrossRef]
- Michopoulos, V.; Powers, A.; Gillespie, C.F.; Ressler, K.J.; Jovanovic, T. Inflammation in Fear- and Anxiety-Based Disorders: PTSD, GAD, and Beyond. Neuropsychopharmacology 2017, 42, 254–270. [Google Scholar] [CrossRef]
- Witteveen, A.B.; Young, S.Y.; Cuijpers, P.; Ayuso-Mateos, J.L.; Barbui, C.; Bertolini, F.; Cabello, M.; Cadorin, C.; Downes, N.; Franzoi, D.; et al. COVID-19 and common mental health symptoms in the early phase of the pandemic: An umbrella review of the evidence. PLoS Med. 2023, 20, e1004206. [Google Scholar] [CrossRef]
- Czeisler, M.E.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24-30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef]
- Liu, J.M.; Tan, B.H.; Wu, S.; Gui, Y.; Suo, J.L.; Li, Y.C. Evidence of central nervous system infection and neuroinvasive routes, as well as neurological involvement, in the lethality of SARS-CoV-2 infection. J. Med. Virol. 2021, 93, 1304–1313. [Google Scholar] [CrossRef]
- Beckman, D.; Bonillas, A.; Diniz, G.B.; Ott, S.; Roh, J.W.; Elizaldi, S.R.; Schmidt, B.A.; Sammak, R.L.; Van Rompay, K.K.A.; Iyer, S.S.; et al. SARS-CoV-2 infects neurons and induces neuroinflammation in a non-human primate model of COVID-19. Cell Rep. 2022, 41, 111573. [Google Scholar] [CrossRef]
- Saikarthik, J.; Saraswathi, I.; Alarifi, A.; Al-Atram, A.A.; Mickeymaray, S.; Paramasivam, A.; Shaikh, S.; Jeraud, M.; Alothaim, A.S. Role of neuroinflammation mediated potential alterations in adult neurogenesis as a factor for neuropsychiatric symptoms in Post-Acute COVID-19 syndrome-A narrative review. PeerJ 2022, 10, e14227. [Google Scholar] [CrossRef]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Crunfli, F.; Carregari, V.C.; Veras, F.P.; Silva, L.S.; Nogueira, M.H.; Antunes, A.; Vendramini, P.H.; Valenca, A.G.F.; Brandao-Teles, C.; Zuccoli, G.D.S.; et al. Morphological, cellular, and molecular basis of brain infection in COVID-19 patients. Proc. Natl. Acad. Sci. USA 2022, 119, e2200960119. [Google Scholar] [CrossRef]
- Rasmi, Y.; Shokati, A.; Hatamkhani, S.; Farnamian, Y.; Naderi, R.; Jalali, L. Assessment of the relationship between the dopaminergic pathway and severe acute respiratory syndrome coronavirus 2 infection, with related neuropathological features, and potential therapeutic approaches in COVID-19 infection. Rev. Med. Virol. 2024, 34, e2506. [Google Scholar] [CrossRef]
- Hufner, K.; Vedova, S.; Tymoszuk, P.; Nelles, P.; Bruckner, T.; Deisenhammer, E.A.; Egeter, J.; Galffy, M.; Giesinger, J.M.; Lehmann, J.; et al. The effect of inflammation, SARS-CoV-2 infection, age and mental health on serotonin, and kynurenine and catecholamine pathway metabolites. Psychoneuroendocrinology 2023, 156, 106334. [Google Scholar] [CrossRef]
- Imai, M.; Kawakami, F.; Uematsu, T.; Matsumoto, T.; Kawashima, R.; Kurosaki, Y.; Tamaki, S.; Maehana, S.; Ichikawa, T.; Hanaki, H.; et al. SARS-CoV-2 propagation to the TPH2-positive neurons in the ventral tegmental area induces cell death via GSK3beta-dependent accumulation of phosphorylated tau. PLoS ONE 2024, 19, e0312834. [Google Scholar] [CrossRef]
- Blum, K.; Cadet, J.L.; Baron, D.; Badgaiyan, R.D.; Brewer, R.; Modestino, E.J.; Gold, M.S. Putative COVID- 19 Induction of Reward Deficiency Syndrome (RDS) and Associated Behavioral Addictions with Potential Concomitant Dopamine Depletion: Is COVID-19 Social Distancing a Double Edged Sword? Subst. Use Misuse 2020, 55, 2438–2442. [Google Scholar] [CrossRef]
- Fancourt, D.; Steptoe, A.; Bu, F. Psychological consequences of long COVID: Comparing trajectories of depressive and anxiety symptoms before and after contracting SARS-CoV-2 between matched long- and short-COVID groups. Br. J. Psychiatry 2023, 222, 74–81. [Google Scholar] [CrossRef]
- Saltzman, L.Y.; Longo, M.; Hansel, T.C. Long-COVID stress symptoms: Mental health, anxiety, depression, or posttraumatic stress. Psychol. Trauma. 2024, 16, 1169–1178. [Google Scholar] [CrossRef]
- Xin, M.; Luo, S.; She, R.; Yu, Y.; Li, L.; Wang, S.; Ma, L.; Tao, F.; Zhang, J.; Zhao, J.; et al. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am. Psychol. 2020, 75, 607–617. [Google Scholar] [CrossRef]
- Fernandez, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef]
- Sauer, M.C.; Barlow, P.B.; Comellas, A.P.; Garg, A. Anxiety and depression symptoms among patients with long COVID: A retrospective cohort study. Eur. Arch. Psychiatry Clin. Neurosci. 2024, 274, 1879–1886. [Google Scholar] [CrossRef]
- Clift, A.K.; Ranger, T.A.; Patone, M.; Coupland, C.A.C.; Hatch, R.; Thomas, K.; Hippisley-Cox, J.; Watkinson, P. Neuropsychiatric Ramifications of Severe COVID-19 and Other Severe Acute Respiratory Infections. JAMA Psychiatry 2022, 79, 690–698. [Google Scholar] [CrossRef]
- Collaborators, C.-M.D. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Cozen, A.E.; Carton, T.; Hamad, R.; Kornak, J.; Faulkner Modrow, M.; Peyser, N.D.; Park, S.; Orozco, J.H.; Brandner, M.; O’Brien, E.C.; et al. Factors associated with anxiety during the first two years of the COVID-19 pandemic in the United States: An analysis of the COVID-19 Citizen Science study. PLoS ONE 2024, 19, e0297922. [Google Scholar] [CrossRef]
- Benke, C.; Autenrieth, L.K.; Asselmann, E.; Pane-Farre, C.A. Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020, 293, 113462. [Google Scholar] [CrossRef]
| Anxiety (n = 85,229) | No Anxiety (n = 1,214,598) | p Value | |
|---|---|---|---|
| COVID-19 | 5900 (6.92%) | 50,299 (4.14%) | <0.0001 |
| Age, mean ± SD (Years Old) | 43.44 ± 21.43 | 38.23 ± 24.28 | 0.87 |
| Female, n (%) | 58,983 (69.21%) | 661,944 (54.50%) | <0.0001 |
| Race/Ethnicity | |||
| White | 14,182 (16.64%) | 160,737 (13.23%) | <0.0001 |
| Asian | 2231 (2.62%) | 34,892 (2.87%) | 0.00002 |
| Black | 22,251 (26.11%) | 303,792 (25.01%) | <0.0001 |
| Other | 46,552 (54.62%) | 703,707 (57.94%) | <0.0001 |
| Hispanic | 39,724 (46.61%) | 397,156 (32.70%) | <0.0001 |
| Pre-Existing Comorbidities | |||
| Hypertension | 26,570 (31.17%) | 185,297 (15.26%) | <0.0001 |
| Chronic Kidney Disease | 6779 (7.95%) | 42,958 (3.54%) | <0.0001 |
| Diabetes | 13,544 (15.89%) | 95,315 (7.85%) | <0.0001 |
| Cardiovascular Diseases | 4682 (5.49%) | 29,803 (2.45%) | <0.0001 |
| COPD | 3166 (3.71%) | 11,715 (0.96%) | <0.0001 |
| Asthma | 16,601 (19.48%) | 81,834 (6.74%) | <0.0001 |
| Obesity | 21,049 (24.70%) | 108,852 (8.96%) | <0.0001 |
| Pre-Existing Anxiety | 28,523 (33.47%) | 35,647 (2.93%) | <0.0001 |
| Variable | Crude OR | 95% CI | Adjusted OR | 95% CI |
|---|---|---|---|---|
| COVID-19 | 4.56 * | (4.44, 4.69) | 2.13 * | (2.06, 2.20) |
| Age (Years Old) | 1.01 * | (1.008, 1.009) | 1.00 | (1.00, 1.002) |
| Female vs. Male | 1.89 * | (1.85, 1.89) | 1.54 * | (1.52, 1.56) |
| Black vs. White | 1.06 * | (1.04, 1.08) | 1.38 * | (1.35, 1.41) |
| Asian vs. White | 0.91 * | (0.87, 0.95) | 1.48 * | (1.41, 1.55) |
| Other vs. White | 1.00 | (0.60, 1.67) | 1.01 | (0.57, 1.78) |
| Hispanic vs. Non-Hispanic | 1.80 * | (1.77, 1.82) | 1.79 * | (1.76, 1.83) |
| Hypertension | 2.52 * | (2.48, 2.56) | 1.25 * | (1.22, 1.28) |
| Chronic Kidney Disease | 2.36 * | (2.30, 2.42) | 1.05 * | (1.01, 1.09) |
| Diabetes | 2.22 * | (2.18, 2.26) | 0.97 * | (0.94, 0.99) |
| Obesity | 3.33 * | (3.28, 3.39) | 1.58 * | (1.54, 1.61) |
| Pre-Existing Anxiety | 16.64 * | (16.35, 16.94) | 11.26 * | (11.05, 11.47) |
| Cardiovascular Diseases | 2.31 * | (2.24, 2.39) | 0.89 * | (0.83, 0.96) |
| COPD | 3.97 * | (3.81, 4.13) | 1.1 * | (1.05, 1.16) |
| Asthma | 3.35 * | (3.29, 3.41) | 1.56 * | (1.53, 1.60) |
| Anxiety (n = 85,229) | No Anxiety (n = 170,458) | p Value | |
|---|---|---|---|
| COVID-19 | 5900 (6.92%) | 7843 (4.60%) | <0.0001 |
| Age, mean ± SD (Years Old) | 43.44 ± 21.43 | 43.29 ± 21.88 | 0.99 |
| Female, n (%) | 58,983 (69.21%) | 117,865 (69.15%) | 0.99 |
| Race/Ethnicity | |||
| White | 14,182 (16.64%) | 28,364 (16.64%) | 1.00 |
| Asian | 2231 (2.62%) | 4462 (2.62%) | 1.00 |
| Black | 22,251 (26.11%) | 44,502 (26.11%) | 1.00 |
| Other | 46,552 (54.62%) | 91,269 (53.54%) | 1.00 |
| Hispanic | 39,724 (46.61%) | 64,113 (37.61%) | 0.99 |
| Pre-Existing Comorbidities | |||
| Hypertension | 26,570 (31.17%) | 30,793 (18.06%) | <0.0001 |
| Chronic Kidney Disease | 6779 (7.95%) | 6709 (3.94%) | 0.89 |
| Diabetes | 13,544 (15.89%) | 15,603 (9.15%) | <0.0001 |
| Cardiovascular Diseases | 4682 (5.49%) | 4673 (2.74%) | <0.0001 |
| COPD | 3166 (3.71%) | 1916 (1.12%) | <0.0001 |
| Asthma | 16,601 (19.48%) | 12,323 (7.23%) | <0.0001 |
| Obesity | 21,049 (24.70%) | 18,536 (10.87%) | <0.0001 |
| Pre-Existing Anxiety | 28,523 (33.47%) | 6295 (3.69%) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Changela, S.; Hadidchi, R.; Wu, S.; Ali, E.; Liu, A.; Peng, T.; Duong, T.Q. Incidence of Anxiety Diagnosis up to Four Years Post SARS-CoV-2 Infection in the Montefiore Medical Center in the Bronx and New York. Diagnostics 2025, 15, 2605. https://doi.org/10.3390/diagnostics15202605
Changela S, Hadidchi R, Wu S, Ali E, Liu A, Peng T, Duong TQ. Incidence of Anxiety Diagnosis up to Four Years Post SARS-CoV-2 Infection in the Montefiore Medical Center in the Bronx and New York. Diagnostics. 2025; 15(20):2605. https://doi.org/10.3390/diagnostics15202605
Chicago/Turabian StyleChangela, Sagar, Roham Hadidchi, Sophia Wu, Ekram Ali, Alex Liu, Thomas Peng, and Tim Q. Duong. 2025. "Incidence of Anxiety Diagnosis up to Four Years Post SARS-CoV-2 Infection in the Montefiore Medical Center in the Bronx and New York" Diagnostics 15, no. 20: 2605. https://doi.org/10.3390/diagnostics15202605
APA StyleChangela, S., Hadidchi, R., Wu, S., Ali, E., Liu, A., Peng, T., & Duong, T. Q. (2025). Incidence of Anxiety Diagnosis up to Four Years Post SARS-CoV-2 Infection in the Montefiore Medical Center in the Bronx and New York. Diagnostics, 15(20), 2605. https://doi.org/10.3390/diagnostics15202605






