Minimally Invasive Surgical Approach in Granulomatosis with Polyangiitis Complicated with Intramural Descending Aorta Hematoma Followed by Aortic Wall Rupture
Abstract
1. Introduction
Objective
2. Methods
3. Case Presentation
3.1. Medical History
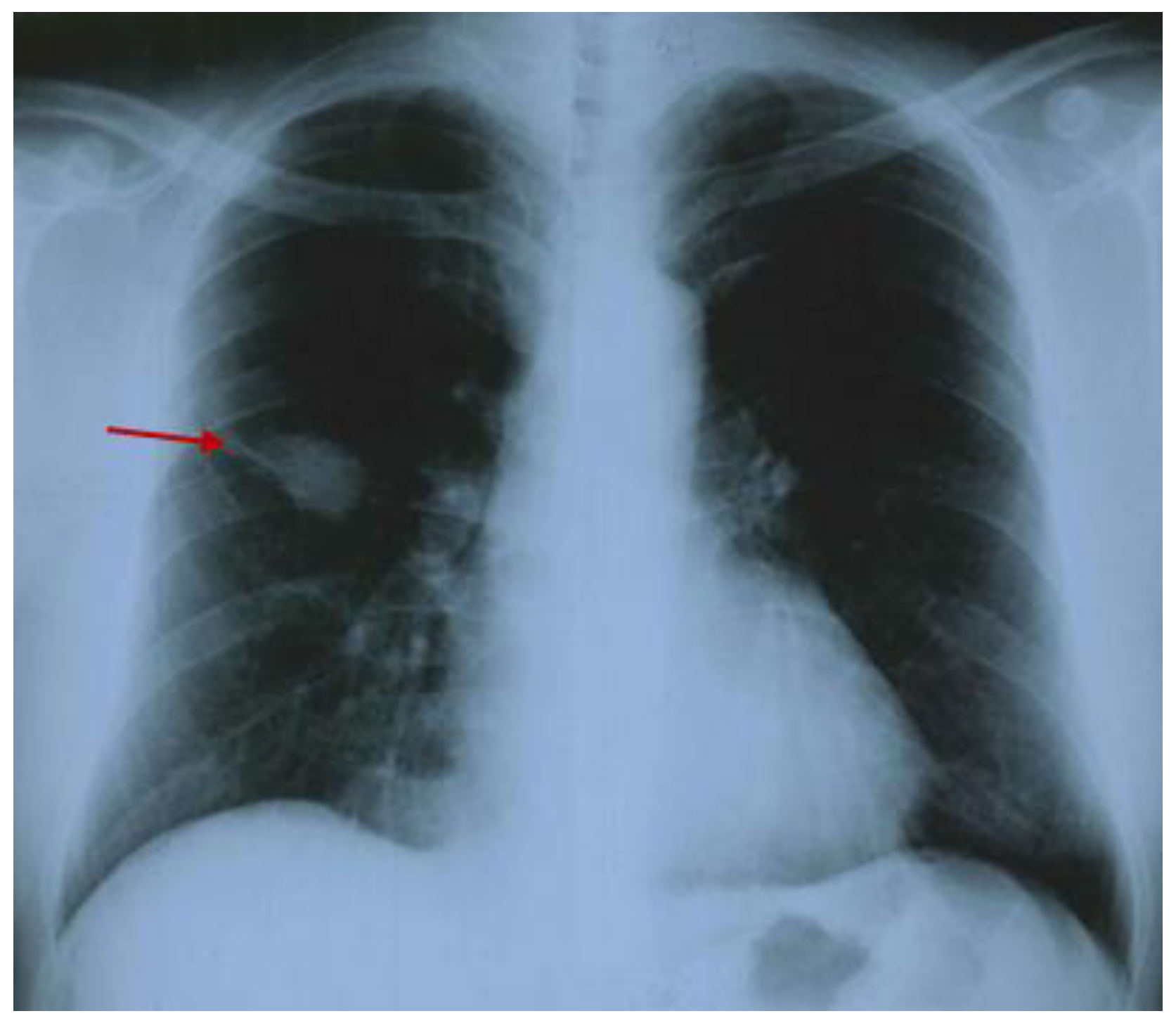
3.2. Current Hospitalization
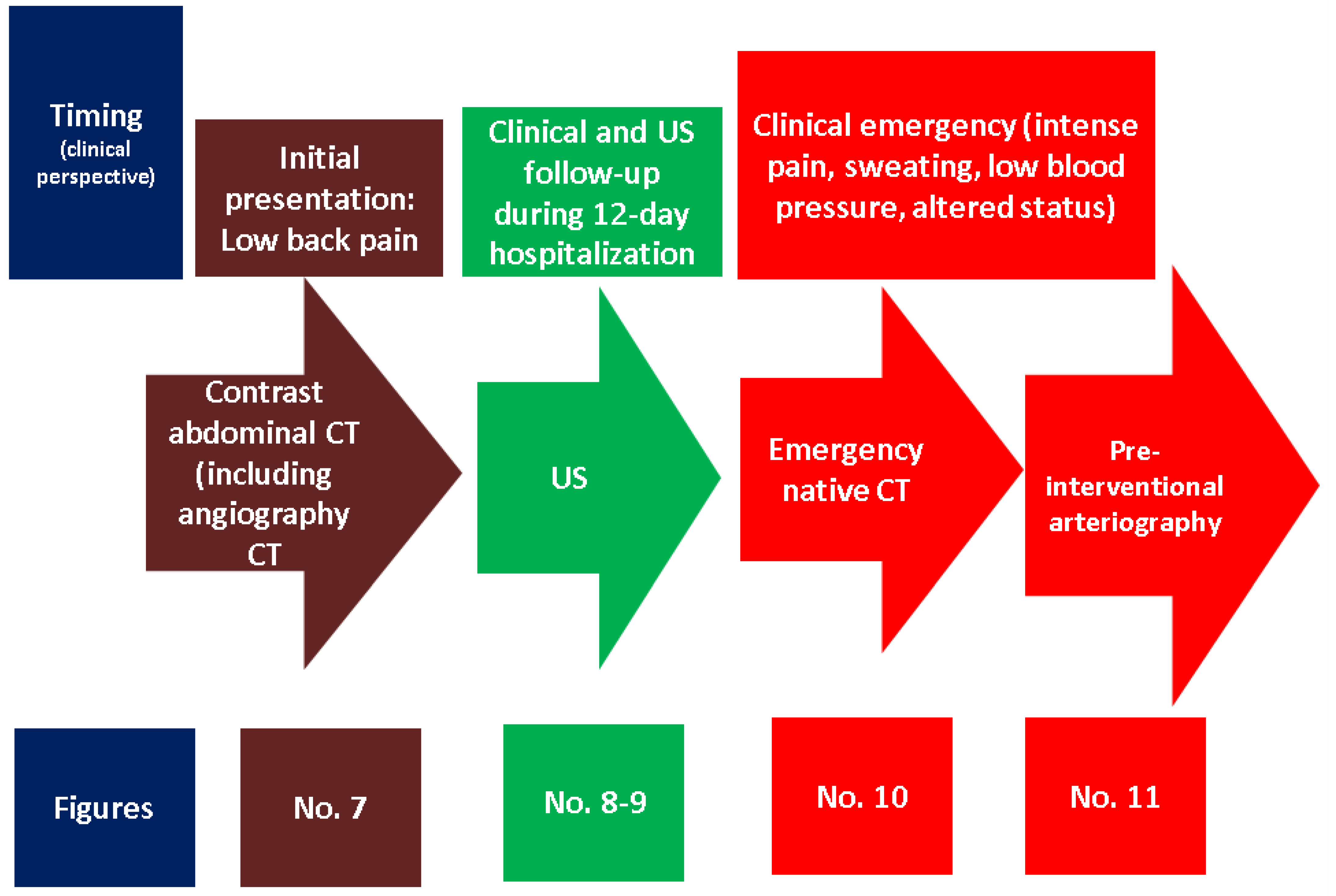
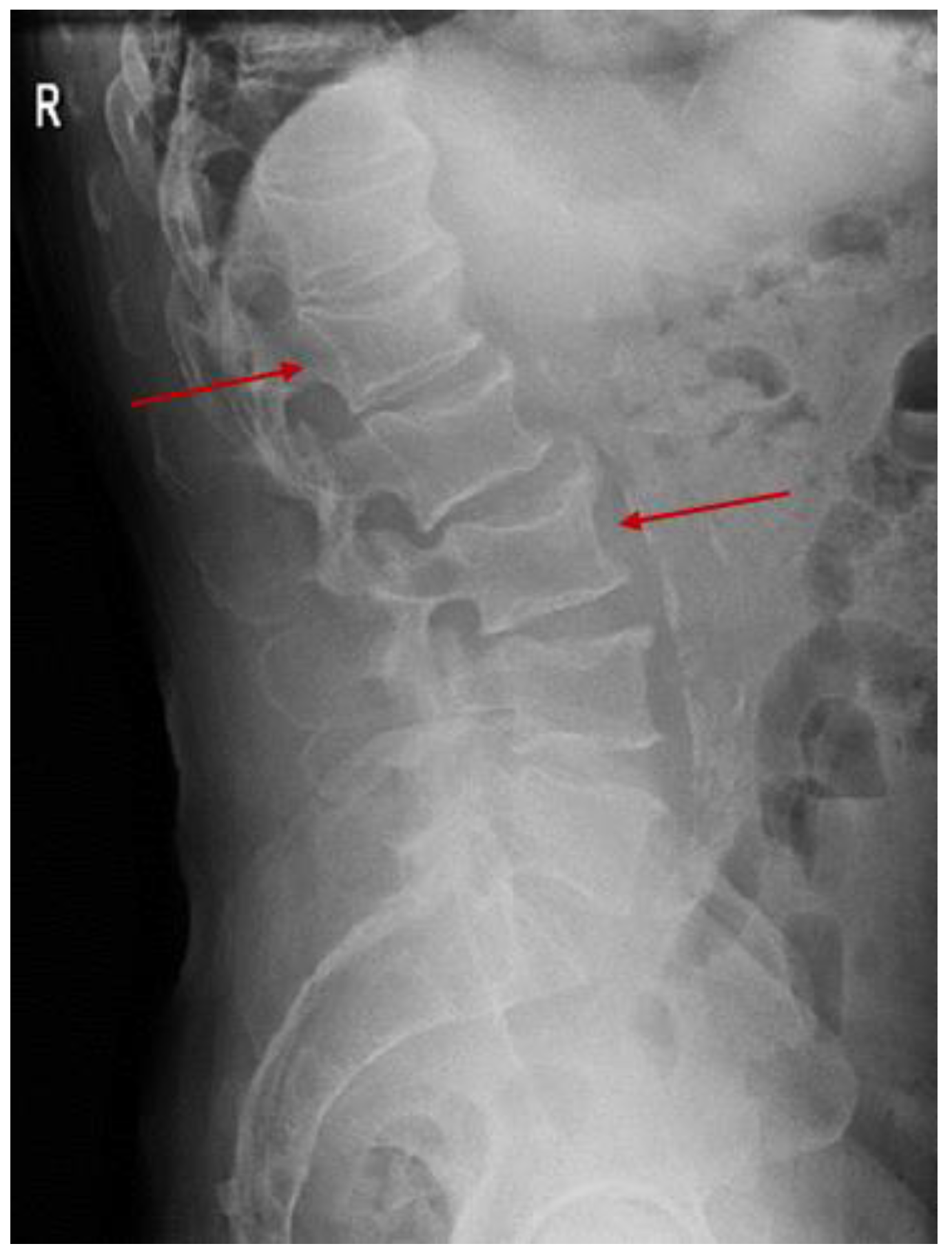
3.2.1. A Fine Index of Clinical Suspicion: Low Back Pain
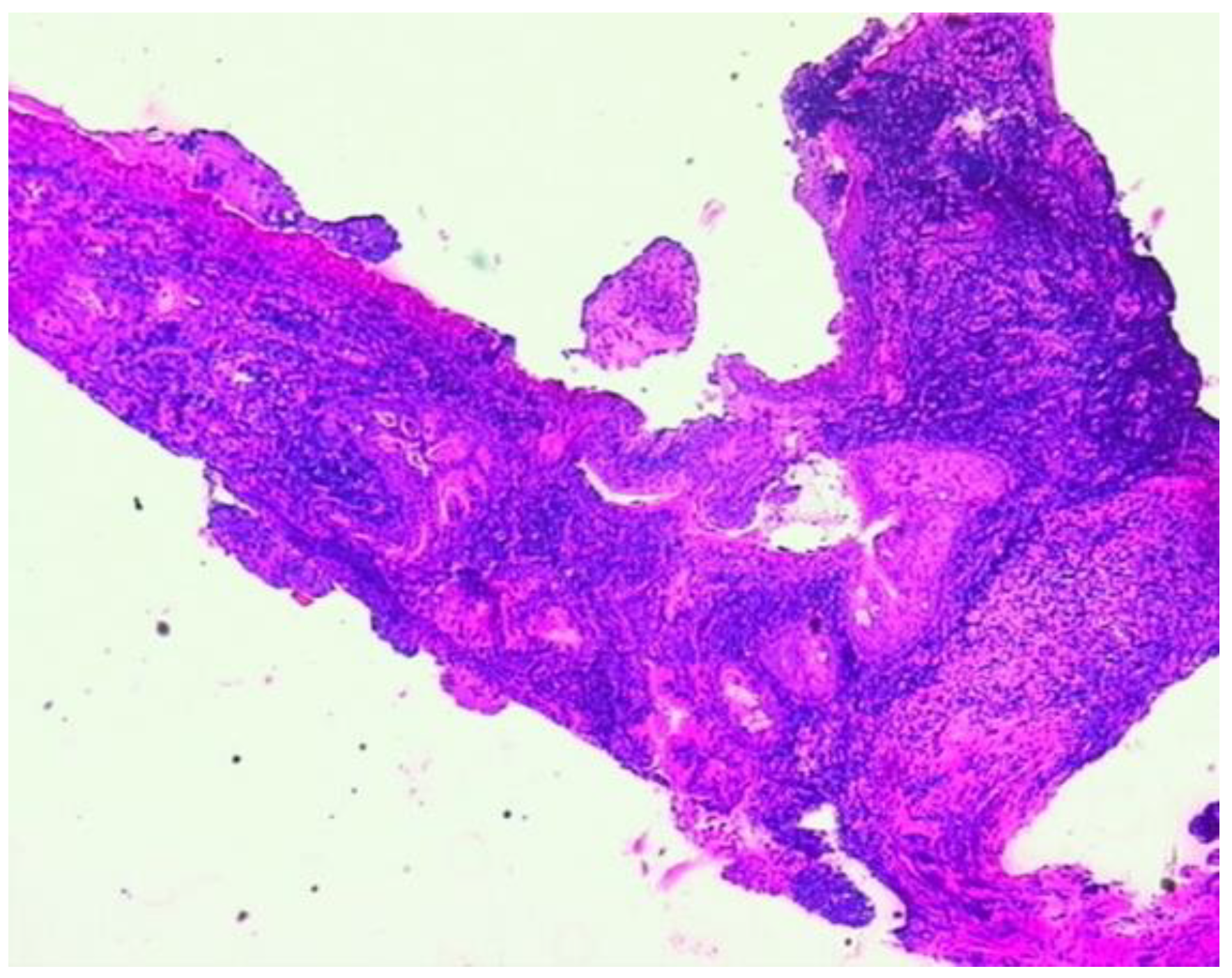
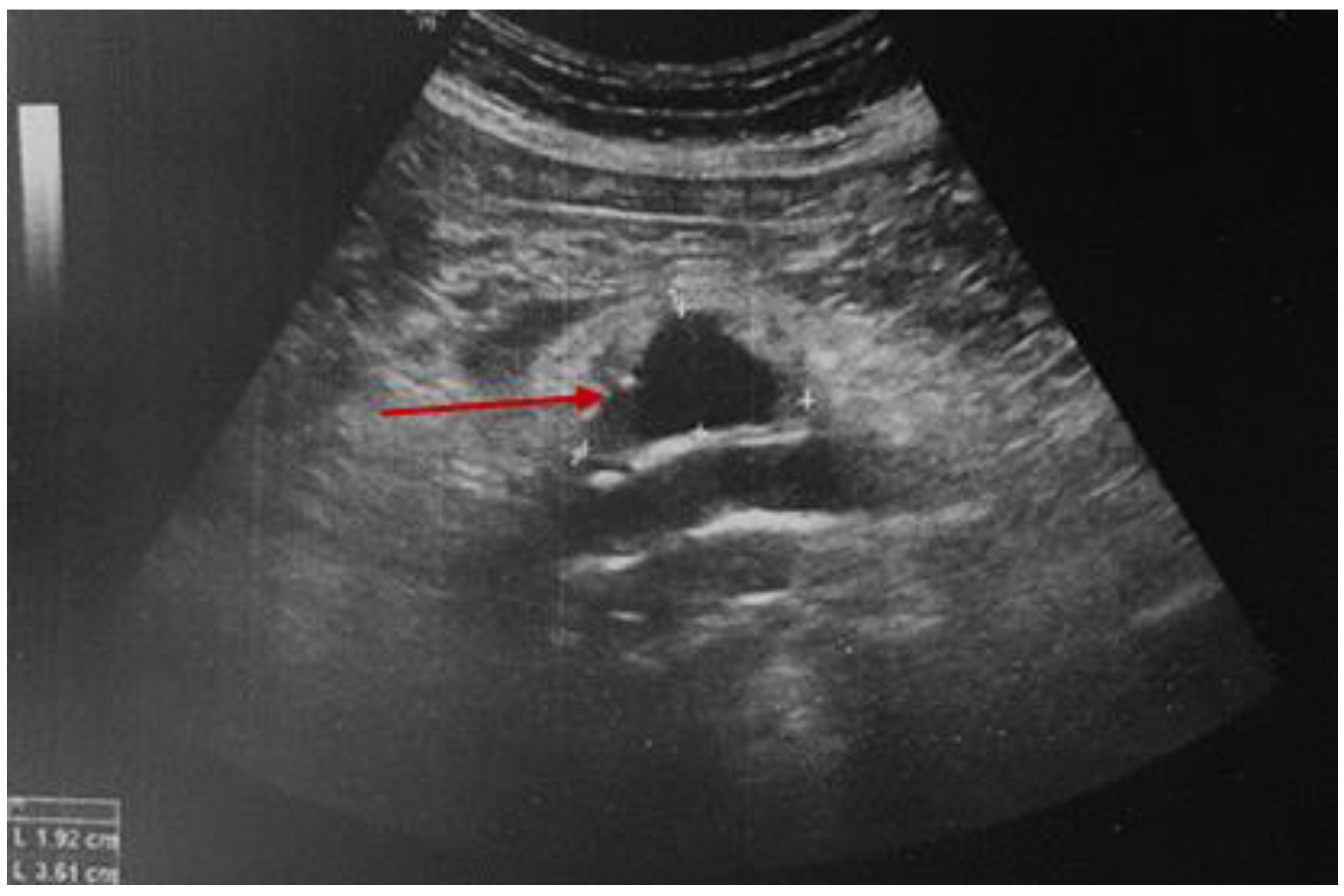
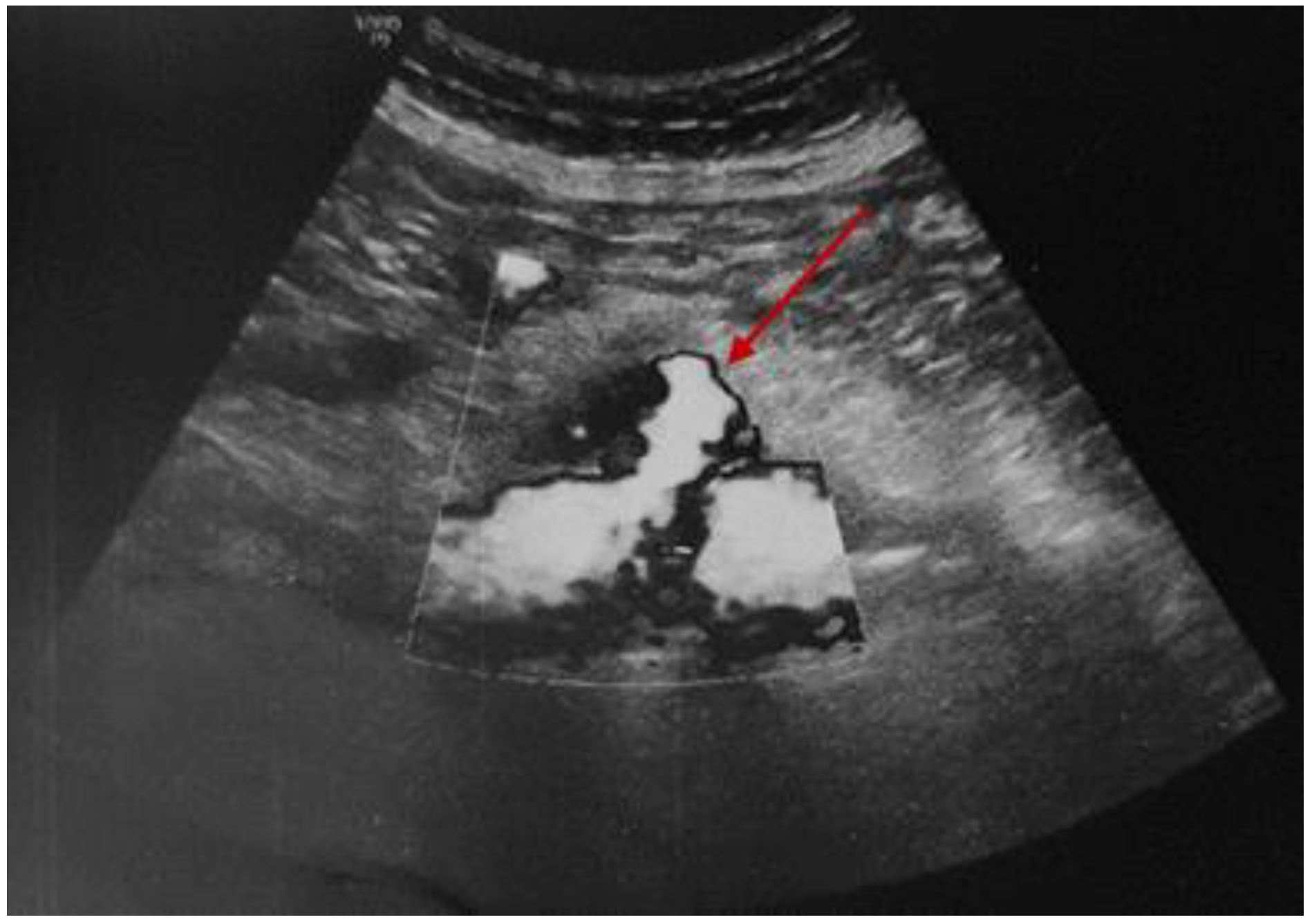
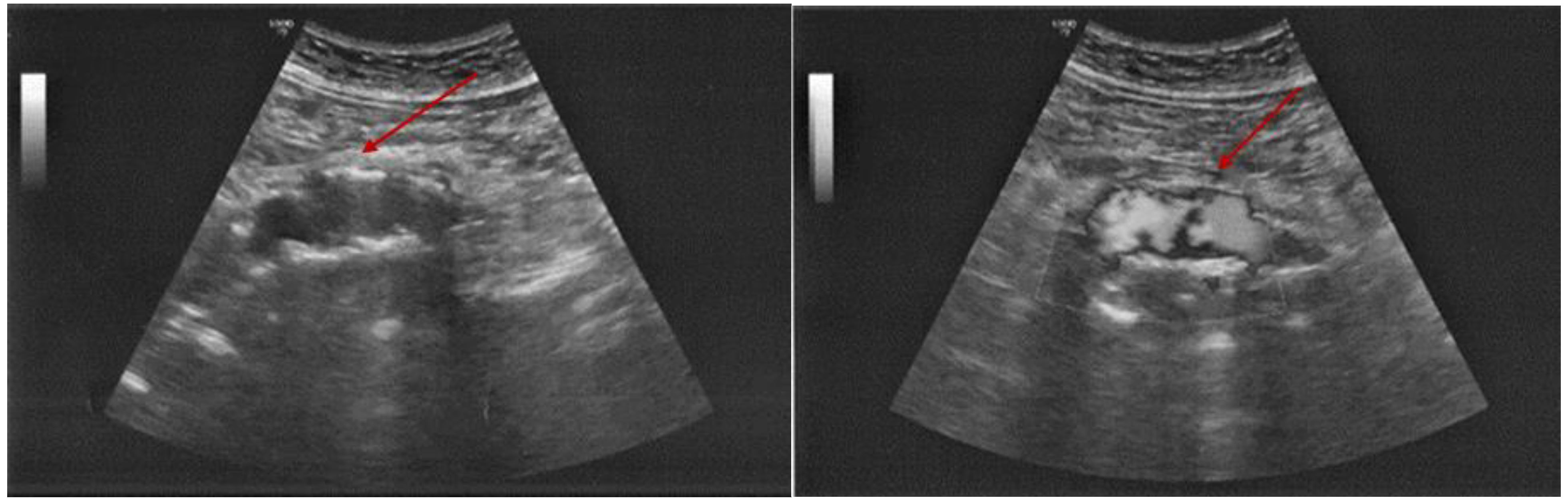
3.2.2. Additional Imaging Assessments
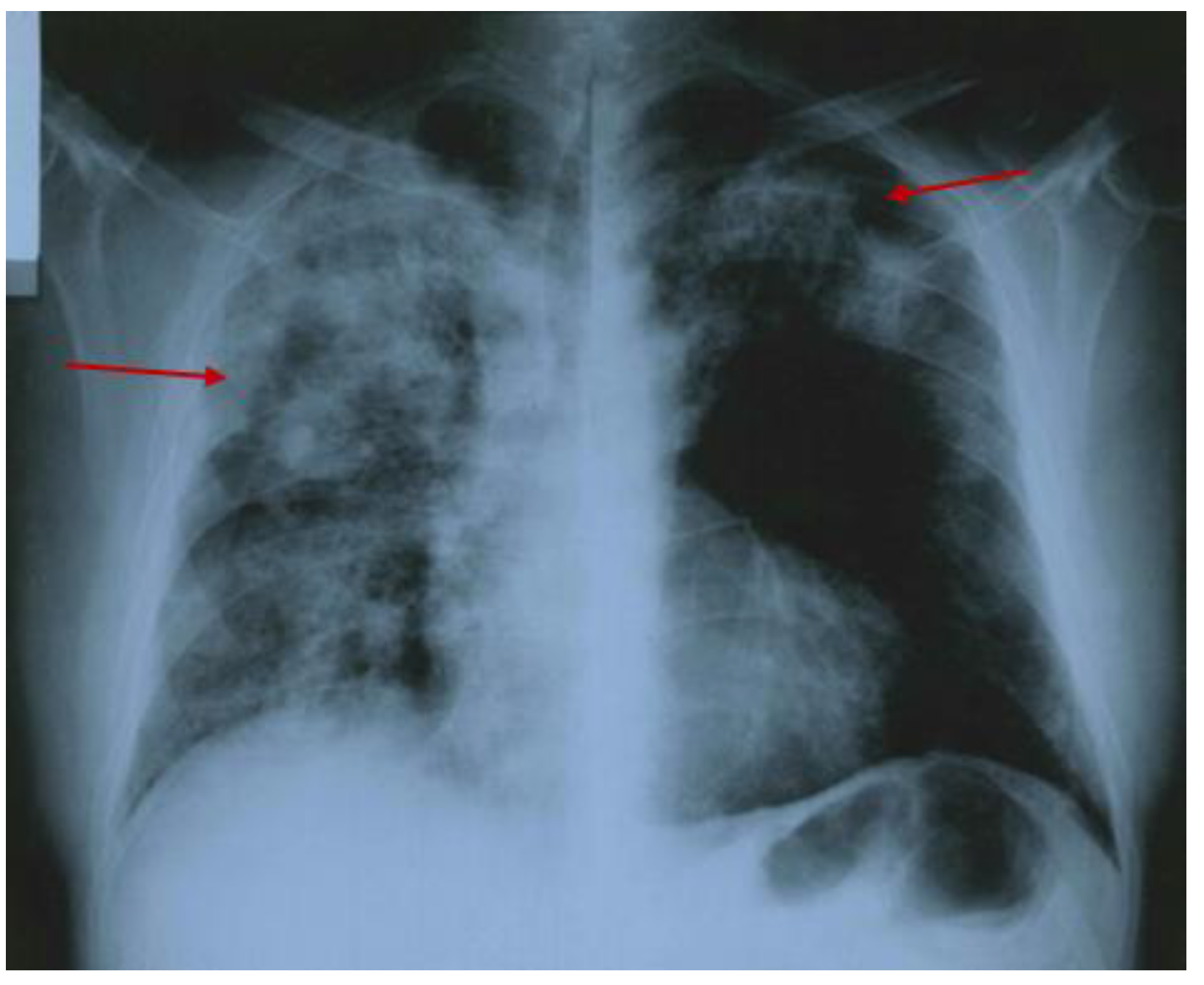
3.2.3. The Descending Aorta Rupture
3.2.4. Minimally Invasive Surgery
3.2.5. One-Month Post-Surgery Follow-Up
4. Discussion
4.1. Case-Focused Analysis
4.2. Sample-Focused Analysis
5. Conclusions
- Unusual aortic manifestations (such as intramural aortic hematoma followed by an aortic rupture) of this rare disease are difficult to recognize since the index of clinical suspicion is rather low;
- Prompt intervention may be life-saving and a multidisciplinary team is mandatory;
- Minimally invasive surgical correction of the aortic event represents optimum management in the modern era;
- This case adds to the limited series of similar reports in the literature (18 prior cases) with a mean age at diagnosis of 55.27 years, and a male–female ratio of 3.5;
- Atypical low back pain in a patient with glucocorticoid-induced osteoporosis might not always be a symptomatic vertebral fracture.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| ANCA (Normal Ranges)—UI/mL | Year of Assessment | Timing with Respect to the Disease Evolution |
|---|---|---|
| 54 (<5) | 2002 | At the moment of first diagnosis |
| 40 (<5) | 2002 | After 6 months |
| 10 (<5) | 2004 | During remission |
| 50 (<5) | 2009 | Relapse with pulmonary manifestations |
| 7.5 (<5) | 2012 | During remission |
| 6 (<5) | 2014 | During remission |
| 4 (<5) | 2016 | During remission |
| 1.2 (<5) | 2018 | During remission |
| 4 (<5) | 2020 | At the moment of macrovascular complications (aortic involvement) |
| Parameter | At the Moment of Diagnosis Value (Normal Ranges) | After 6 Months Value (Normal Ranges) |
|---|---|---|
| ESR (erythrocyte sedimentation rate) | 89 (0–20) mm/h | 26 (0–20) mm/h |
| CRP (C reactive protein) | 96 (0–5) mg/L | 2 (0–5) mg/L |
| Fibrinogen | 867 (276–471) mg/dL | 500 (276–471) mg/dL |
| Urea | 30 (17–43) mg/dL | 78 (17–43) mg/dL |
| Creatinine | 0.8 L (0.67–1.17) mg/dL | 1.89 (0.67–1.17) mg/dL |
| Proteinuria | 30 (<30) mg/24 h | 300 (<30) mg/24 h |
| Hematuria | absent | 10 (0–1) erythrocytes/high-power microscopic field |
Appendix B
References
- Younger, D.S. Overview of the Vasculitides. Neurol. Clin. 2019, 37, 171–200. [Google Scholar] [CrossRef]
- Teames, C.; Highland, J.; Cox, D.; Elstad, M.; Koening, C.; Smith, M. The Diagnosis of Granulomatosis with Polyangiitis When Serology and Biopsies are Negative. OTO Open 2024, 8, e138. [Google Scholar] [CrossRef] [PubMed]
- Lutalo, P.M.; D’Cruz, D.P. Diagnosis and classification of granulomatosis with polyangiitis (aka Wegener’s granulomatosis). J. Autoimmun. 2014, 48–49, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Geetha, D.; Jefferson, J.A. ANCA-Associated Vasculitis: Core Curriculum 2020. Am. J. Kidney Dis. 2020, 75, 124–137. [Google Scholar] [CrossRef] [PubMed]
- Panupattanapong, S.; Stwalley, D.L.; White, A.J.; Olsen, M.A.; French, A.R.; Hartman, M.E. Epidemiology and Outcomes of Granulomatosis with Polyangiitis in Pediatric and Working-Age Adult Populations In the United States: Analysis of a Large National Claims Database. Arthritis Rheumatol. 2018, 70, 2067–2076. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.; Ekbom, A.; Brandt, L.; Askling, J. Increasing incidence of Wegener’s granulomatosis in Sweden, 1975–2001. J Rheumatol. 2006, 33, 2060–2063. [Google Scholar]
- Takala, J.H.; Kautiainen, H.; Malmberg, H.; Leirisalo-Repo, M. Incidence of Wegener’s granulomatosis in Finland 1981–2000. Clin Exp Rheumatol. 2008, 26 (Suppl. 49), S81–S85. [Google Scholar] [PubMed]
- Terrier, B.; Dechartres, A.; Deligny, C.; Godmer, P.; Charles, P.; Hayem, G.; Dunogué, B.; de Bandt, M.; Cohen, P.; Puéchal, X.; et al. Granulomatosis with polyangiitis according to geographic origin and ethnicity: Clinical-biological presentation and outcome in a French population. Rheumatology 2017, 56, 445–450. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Watts, R.A.; Al-Taiar, A.; Scott, D.G.; Macgregor, A.J. Prevalence and incidence of Wegener’s granulomatosis in the UK general practice research database. Arthritis Rheum. 2009, 61, 1412–1416. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, S.; Watts, R.A.; Kobayashi, S.; Suzuki, K.; Jayne, D.R.; Scott, D.G.; Hashimoto, H.; Nunoi, H. Comparison of the epidemiology of anti-neutrophil cytoplasmic antibody-associated vasculitis between Japan and the U.K. Rheumatology 2011, 50, 1916–1920. [Google Scholar] [CrossRef]
- Khan, A.R.; Chapman, P.T.; Stamp, L.K.; Wells, J.E.; O’Donnell, J.L. Wegener’s granulomatosis: Treatment and survival characteristics in a high-prevalence southern hemisphere region. Intern. Med. J. 2012, 42, e23–e26. [Google Scholar] [CrossRef] [PubMed]
- Watts, R.A.; Mooney, J.; Skinner, J.; Scott, D.G.; Macgregor, A.J. The contrasting epidemiology of granulomatosis with polyangiitis (Wegener’s) and microscopic polyangiitis. Rheumatology 2012, 51, 926–931. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, S.; Uezono, S.; Hisanaga, S.; Fukudome, K.; Kobayashi, S.; Suzuki, K.; Hashimoto, H.; Nakao, H.; Nunoi, H. Incidence of ANCA-associated primary renal vasculitis in the Miyazaki Prefecture: The first population-based, retrospective, epidemiologic survey in Japan. Clin. J. Am. Soc. Nephrol. 2006, 1, 1016–1022. [Google Scholar] [CrossRef]
- Hissaria, P.; Cai, F.Z.; Ahern, M.; Smith, M.; Gillis, D.; Roberts-Thomson, P. Wegener’s granulomatosis: Epidemiological and clinical features in a South Australian study. Intern. Med. J. 2008, 38, 776–780. [Google Scholar] [CrossRef] [PubMed]
- Ntatsaki, E.; Watts, R.A.; Scott, D.G. Epidemiology of ANCA-associated vasculitis. Rheum. Dis. Clin. North Am. 2010, 36, 447–461. [Google Scholar] [CrossRef]
- Mohammad, A.J.; Jacobsson, L.T.; Westman, K.W.; Sturfelt, G.; Segelmark, M. Incidence and survival rates in Wegener’s granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome and polyarteritis nodosa. Rheumatology 2009, 48, 1560–1565. [Google Scholar] [CrossRef] [PubMed]
- Shi, L. Anti-neutrophil cytoplasmic antibody-associated vasculitis: Prevalence, treatment, and outcomes. Rheumatol. Int. 2017, 37, 1779–1788. [Google Scholar] [CrossRef]
- Nica, S.; Sionel, R.; Maciuca, R.; Csutak, O.; Ciobica, M.L.; Nica, M.I.; Chelu, I.; Radu, I.; Toma, M. Gender-Dependent Associations Between Digit Ratio and Genetic Polymorphisms, BMI, and Reproductive Factors. Rom. J. Mil. Med. 2025, 118, 78–86. [Google Scholar] [CrossRef]
- Springer, J.M.; Kermani, T.A.; Sreih, A.; Shaw, D.G.; Young, K.; Burroughs, C.M.; Merkel, P.A. Clinical Characteristics of an Internet-Based Cohort of Patient-Reported Diagnosis of Granulomatosis with Polyangiitis and Microscopic Polyangiitis: Observational Study. J. Med. Internet Res. 2020, 22, e17231. [Google Scholar] [CrossRef]
- Naidu, G.S.R.S.N.K.; Misra, D.P.; Rathi, M.; Sharma, A. Is granulomatosis with polyangiitis in Asia different from the West? Int. J. Rheum. Dis. 2019, 22 (Suppl. 1), 90–94. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Cui, Y.; Li, Y.; Wang, C.; Zhao, H.; Han, J. Using inpatient data to estimate the prevalence of Wegener’s granulomatosis in China. Intractable Rare Dis. Res. 2016, 5, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Aydın Tufan, M.; Tekkarışmaz, N. Predictive factors of mortality in granulomatosis with polyangiitis: A single-center study. Arch. Rheumatol. 2021, 36, 435–444. [Google Scholar] [CrossRef]
- Anghel, D.; Ciobica, L.M.; Negru, M.M.; Jurcut, C.; Otlocan, L.; Coca, A. Bone mineral density and vitamin D levels in patients with rheumatoid arthritis. Osteoporos. Int. 2017, 28, S435–S436. [Google Scholar]
- Tariq, E.; Nishanth, K.; Arshid, A.; Miqdad, M.; Cancarevic, I. Aortic Involvement in Antineutrophil Cytoplasmic Antibodies Vasculitis, a Coincidence or a Real Association? Cureus 2020, 12, e9690. [Google Scholar] [CrossRef]
- Dumitru, N.; Carsote, M.; Cocolos, A.; Petrova, E.; Olaru, M.; Dumitrache, C.; Ghemigian, A. The Link Between Bone Osteocalcin and Energy Metabolism in a Group of Postmenopausal Women. Curr. Health Sci. J. 2019, 45, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Robson, J.C.; Grayson, P.C.; Ponte, C.; Suppiah, R.; Craven, A.; Judge, A.; Khalid, S.; Hutchings, A.; Watts, R.A.; Merkel, P.A.; et al. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology classification criteria for granulomatosis with polyangiitis. Ann. Rheum Dis. 2022, 81, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Grayson, P.C.; Ponte, C.; Suppiah, R.; Robson, J.C.; Craven, A.; Judge, A.; Khalid, S.; Hutchings, A.; Luqmani, R.A.; Watts, R.A.; et al. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology Classification Criteria for Eosinophilic Granulomatosis with Polyangiitis. Ann. Rheum Dis. 2022, 81, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Suppiah, R.; Robson, J.C.; Grayson, P.C.; Ponte, C.; Craven, A.; Khalid, S.; Judge, A.; Hutchings, A.; Merkel, P.A.; Luqmani, R.A.; et al. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology Classification Criteria for Microscopic Polyangiitis. Arthritis Rheumatol. 2022, 74, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.; Makhzoum, J.P.; Pagnoux, C. Updates in ANCA-associated vasculitis. Eur. J. Rheumatol. 2022, 9, 153–166. [Google Scholar] [CrossRef]
- Konstantouli, A.M.; Lioulios, G.; Stai, S.; Moysidou, E.; Fylaktou, A.; Papagianni, A.; Stangou, M. Type of ANCA May Be Indispensable in Distinguishing Subphenotypes of Different Clinical Entities in ANCA-Associated Vasculitis. Life 2022, 12, 1467. [Google Scholar] [CrossRef] [PubMed]
- Austin, K.; Janagan, S.; Wells, M.; Crawshaw, H.; McAdoo, S.; Robson, J.C. ANCA Associated Vasculitis Subtypes: Recent Insights and Future Perspectives. J. Inflamm. Res. 2022, 15, 2567–2582. [Google Scholar] [CrossRef]
- Moretti, M.; Elefante, E.; Pisapia, L.; Di Cianni, F.; Italiano, N.; La Rocca, G.; Talarico, R.; Mosca, M.; Baldini, C.; Ferro, F. The role of tobacco smoking in anti-neutrophil cytoplasmic antibody-associated vasculitis: A systematic review. Clin. Exp. Rheumatol. 2024, 42, 1321–1332. [Google Scholar] [CrossRef] [PubMed]
- Vasiliu, O. Therapeutic management of atypical antipsychotic-related metabolic dysfunctions using GLP-1 receptor agonists: A systematic review. Exper Ther. Med. 2023, 26, 355. [Google Scholar] [CrossRef] [PubMed]
- Jiang, R.; Zhou, H.; Wen, L.; Kong, X.; Zhou, Z. COVID-19-induced granulomatosis with polyangiitis: A case report of a 16-year-old East Asian and literature review. Immun. Inflamm. Dis. 2024, 12, e70010. [Google Scholar] [CrossRef]
- Romanello, D.; Giacomelli, M.; Coccia, I.; Lido, P.; Rotunno, S. An Unusual Presentation of Granulomatosis with Polyangiitis (Wegener’s) After SARS-CoV-2 Infection. Cureus 2023, 15, e50088. [Google Scholar] [CrossRef] [PubMed]
- Doubelt, I.; Cuthbertson, D.; Carette, S.; Khalidi, N.A.; Koening, C.L.; Langford, C.; McAlear, C.A.; Moreland, L.W.; Monach, P.; Seo, P.; et al. Vitamin D status in ANCA-associated vasculitis. Rheumatol. Adv. Pract. 2023, 7, rkad021. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.O.; Oliveira, R.M.; Levy-Neto, M.; Caparbo, V.F.; Pereira, R.M.R. Serum 25-hydroxyvitamin D levels in patients with Granulomatosis with Polyangiitis: Association with respiratory infection. Clinics 2017, 72, 723–728. [Google Scholar] [CrossRef]
- Runowska, M.; Majewski, D.; Majewska, K.; Puszczewicz, M. Vitamin D supply in patients with rheumatic diseases in Poland—A pilot study. Reumatologia 2021, 59, 146–152. [Google Scholar] [CrossRef]
- Vasiliu, O. Impact of SGLT2 inhibitors on metabolic status in patients with psychiatric disorders undergoing treatment with second-generation antipsychotics (Review). Exp. Ther. Med. 2023, 25, 125. [Google Scholar] [CrossRef]
- Charn, G.; Sturman, J.; Ozbek, L.; Henderson, S.; Burns, A.; Hamour, S.; Pepper, R.; McClelland, L.; Chanouzas, D.; Gane, S.; et al. Cocaine-induced granulomatosis with polyangiitis: An under-recognised condition. Clin. Med. 2023, 23 (Suppl. 6), 23. [Google Scholar] [CrossRef]
- Gill, C.; Sturman, J.; Ozbek, L.; Henderson, S.R.; Burns, A.; Hamour, S.; Pepper, R.J.; McClelland, L.; Chanouzas, D.; Gane, S.; et al. Cocaine-induced granulomatosis with polyangiitis-an under-recognized condition. Rheumatol. Adv. Pract. 2023, 7, rkad027. [Google Scholar] [CrossRef] [PubMed]
- Bantis, K.; Stangou, M.; Kalpakidis, S.; Hatziadamou, M.; Daikidou, D.V.; Lioulios, G.; Mitsoglou, Z.; Chatzidrosou, H.; Nikolaidou, C.; Fylaktou, A.; et al. Systemic complement activation in anti-neutrophil cytoplasmic antibody-associated vasculitis and necrotizing glomerulonephritis. Nephrology 2021, 26, 30–37. [Google Scholar] [CrossRef]
- Berti, A.; Warner, R.; Johnson, K.; Cornec, D.; Schroeder, D.; Kabat, B.; Langford, C.A.; Hoffman, G.S.; Fervenza, F.C.; Kallenberg, C.G.M.; et al. Brief Report: Circulating Cytokine Profiles and Antineutrophil Cytoplasmic Antibody Specificity in Patients with Antineutrophil Cytoplasmic Antibody-Associated Vasculitis. Arthritis Rheumatol. 2018, 70, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Potentas-Policewicz, M.; Fijolek, J. Granulomatosis with polyangiitis: Clinical characteristics and updates in diagnosis. Front. Med. 2024, 11, 1369233. [Google Scholar] [CrossRef]
- Roper, T.; Salama, A.D. ANCA-Associated Vasculitis: Practical Issues in Management. Indian J. Nephrol. 2024, 34, 6–23. [Google Scholar] [CrossRef] [PubMed]
- Tzanninis, I.; Elserwey, A.; Mason, A.; Rawlins, J. A rare case report of granulomatosis with polyangiitis presenting with thrombus of the ascending aorta. Clin. Med. 2022, 22 (Suppl. 4), 42–43. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Padilla, J.; Carrascosa, T. Periaortic Mass Simulating Aortic Graft Infection as a Rare Presentation of Granulomatosis with Polyangiitis. J. Clin. Rheumatol. 2021, 27, e24–e25. [Google Scholar] [CrossRef] [PubMed]
- Hesford, J.; Medford, A.R.; Gunawardena, H. Lessons of the month: ANCA-associated vasculitis-granulomatosis with polyangiitis: ’the great mimic’. Clin. Med. 2021, 21, e231–e233. [Google Scholar] [CrossRef]
- Pineda Bernal, L.; Bitencourt, N.; Batra, K.; Solow, E.B. Successful use of rituximab in granulomatosis with polyangiitis with aortic inflammation. Clin. Exp. Rheumatol. 2019, 37 (Suppl. 117), 144–147. [Google Scholar]
- Pan, L.; Yan, J.H.; Gao, F.Q.; Li, H.; Han, S.S.; Cao, G.H.; Lv, C.J.; Wang, X.Z. Case report of a 28-year-old man with aortic dissection and pulmonary shadow due to granulomatosis with polyangiitis. BMC Pulm. Med. 2019, 19, 122. [Google Scholar] [CrossRef]
- Parperis, K.; Abdulqader, Y. Aortitis and pachymeningitis: An unusual combination in granulomatosis with polyangiitis (myeloperoxidase-associated vasculitis). BMJ Case Rep. 2019, 12, e226795. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.K.; Kim, J.B. Granulomatosis with Polyangiitis Involving the Ascending Aorta. Ann. Thorac. Surg. 2018, 106, e11–e13. [Google Scholar] [CrossRef] [PubMed]
- González Revilla, E.M.; Fernandez, A.A.; Ramirez, M.T.; Pardo, S.C.; Moragues, M.A. Retroperitoneal fibrosis with periaortitis: A case report of an unusual form of presentation of granulomatosis with polyangiitis. Respir. Med. Case Rep. 2016, 19, 121–124. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ozaki, T.; Maeshima, K.; Kiyonaga, Y.; Torigoe, M.; Imada, C.; Hamasaki, H.; Haranaka, M.; Ishii, K.; Shibata, H. Large-vessel involvement in granulomatosis with polyangiitis successfully treated with rituximab: A case report and literature review. Mod. Rheumatol. 2017, 27, 699–704. [Google Scholar] [CrossRef]
- Ohta, N.; Waki, T.; Fukase, S.; Suzuki, Y.; Kurakami, K.; Aoyagi, M.; Kakehata, S. Aortic aneurysm rupture as a rare complication of granulomatosis with polyangiitis: A case report. J. Med. Case Rep. 2013, 7, 202. [Google Scholar] [CrossRef] [PubMed]
- Amos, L.A.; Roberts, M.A.; Blair, S.; McMahon, L.P. cANCA-associated aortitis. Clin. Kidney J. 2012, 5, 47–49. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shmagel, A.; Kokebie, R.; Meyer, C. Granulomatosis with polyangiitis (Wegener’s) presenting as a periaortic mass. J. Clin. Rheumatol. 2011, 17, 442–443. [Google Scholar] [CrossRef] [PubMed]
- Unlü, C.; Willems, M.; Ten Berge, I.J.; Legemate, D.A. Aortitis with aneurysm formation as a rare complication of Wegener’s granulomatosis. J. Vasc. Surg. 2011, 54, 1485–1487. [Google Scholar] [CrossRef] [PubMed]
- Minnee, R.C.; van den Berk, G.E.; Groeneveld, J.O.; van Dijk, J.; Turkcan, K.; Visser, M.J.; Vahl, A.C. Aortic aneurysm and orchitis due to Wegener’s granulomatosis. Ann. Vasc. Surg. 2009, 23, e15–e19. [Google Scholar] [CrossRef]
- Carels, T.; Verbeken, E.; Blockmans, D. p-ANCA-associated periaortitis with histological proof of Wegener’s granulomatosis: Case report. Clin. Rheumatol. 2005, 24, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Schildhaus, H.U.; Von Netzer, B.; Dombrowski, F.; Pfeifer, U. Atypical manifestation of a cytoplasmic antineutrophil cytoplasmic antibody (PR3-ANCA)-associated vasculitis with involvement of aortic intima and parietal endocardium. Hum. Pathol. 2002, 33, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Blockmans, D.; Baeyens, H.; Van Loon, R.; Lauwers, G.; Bobbaers, H. Periaortitis and aortic dissection due to Wegener’s granulomatosis. Clin. Rheumatol. 2000, 19, 161–164. [Google Scholar] [CrossRef] [PubMed]
- Fink, A.M.; Miles, K.A.; Wraight, E.P. Indium-111 labelled leucocyte uptake in aortitis. Clin. Radiol. 1994, 49, 863–866. [Google Scholar] [CrossRef]
- Nistor, C.E.; Găvan, C.S.; Ciritel, A.A.; Nemes, A.F.; Ciuche, A. The Association of Minimally Invasive Surgical Approaches and Mortality in Patients with Malignant Pleuropericarditis—A 10 Year Retrospective Observational Study. Medicina 2022, 58, 718. [Google Scholar] [CrossRef]
- Carsote, M.; Valea, A.; Dumitru, N.; Terzea, D.; Petrova, E.; Albu, S.; Buruiana, A.; Ghemigian, A. Metastases in daily endocrine practice. Arch. Balk. Med. Union 2016, 51, 476–480. [Google Scholar]
- Mitrică, M.; Lorusso, L.; Badea, A.A.; Sîrbu, C.A.; Pleșa, A.; Stănescu, A.A.; Pleșa, F.C.; Sîrbu, O.M.; Munteanu, A.E. The Hidden Heart: Exploring Cardiac Damage Post-Stroke: A Narrative Review. Medicina 2024, 60, 1699. [Google Scholar] [CrossRef] [PubMed]
- Adam, R.; Munteanu, A.; Mititelu, R.; Onciul, S.; Deleanu, D.; Iliescu, V.A.; Popescu, B.A.; Jurcut, R. Severe Aortic Stenosis and ATTRwt Amyloidosis - Beware in the Aging: A Case Report and Review of the Literature. Clin. Interv. Aging 2020, 15, 1863–1872. [Google Scholar] [CrossRef]
- Schäfer, V.S.; Petzinna, S.M.; Schmidt, W.A. News on the imaging of large vessel vasculitis. Z. Rheumatol. 2024, 83, 800–811. [Google Scholar] [CrossRef] [PubMed]
- Anghel, A.; Stanciu, S.; Ciobica, M.L.; Stoicescu, D.; Muresan, M.M. Contrast-enhanced ultrasound-clinical applications. Rom. J. Mil. Med. 2011, 114, 25–30. [Google Scholar]
- Stanciu, S.; Enciu, C.; Raduta, I.; Stoicescu, D.; Anghel, A.; Anghel, D.; Olan, B.; Ciobica, L. The role of contrast-enhanced ultrasound in risk assessment of carotid atheroma. Rom. J. Mil. Med. 2016, 119, 9–11. [Google Scholar] [CrossRef]
- Bosch, P.; Bond, M.; Dejaco, C.; Ponte, C.; Mackie, S.L.; Falzon, L.; Schmidt, W.A.; Ramiro, S. Imaging in diagnosis, monitoring and outcome prediction of large vessel vasculitis: A systematic literature review and meta-analysis informing the 2023 update of the EULAR recommendations. RMD Open 2023, 9, e003379. [Google Scholar] [CrossRef] [PubMed]
- Carubbi, F.; Bosch, P.; Machado, P.M.; Scirè, C.A.; Alunno, A.; Proft, F.; Baraliakos, X.; Dejaco, C. Current Practice of Imaging-Guided Interventional Procedures in Rheumatic and Musculoskeletal Diseases: Results of a Multinational Multidisciplinary Survey. Front. Med. 2021, 8, 779975. [Google Scholar] [CrossRef] [PubMed]
- Bosch, P.; Carubbi, F.; Scirè, C.A.; Baraliakos, X.; Falzon, L.; Dejaco, C.; Machado, P.M. Value of imaging to guide interventional procedures in rheumatic and musculoskeletal diseases: A systematic literature review informing EULAR points to consider. RMD Open 2021, 7, e001864. [Google Scholar] [CrossRef] [PubMed]
- Elsayed, N.; Perez, S.; Straus, S.L.; Unkart, J.; Malas, M. Outcomes of Thoracic and Complex Endovascular Aortic Repair in Patients with Renal Insufficiency. Ann. Vasc. Surg. 2024, 109, 83–90. [Google Scholar] [CrossRef]
- Wu, C.C.; Chou, A.H.; Lin, Y.S.; Wu, V.C.; Chang, S.H.; Chu, P.H.; Cheng, Y.T.; Ko, P.J.; Liu, K.S.; Chen, S.W. Late outcomes of endovascular aortic stent graft therapy in patients with chronic kidney disease. Medicine 2020, 99, e22157. [Google Scholar] [CrossRef] [PubMed]
- Alimy, A.R.; Anastasilakis, A.D.; Carey, J.J.; D’Oronzo, S.; Naciu, A.M.; Paccou, J.; Yavropoulou, M.P.; Lems, W.F.; Rolvien, T. Conservative Treatments in the Management of Acute Painful Vertebral Compression Fractures: A Systematic Review and Network Meta-Analysis. JAMA Netw. Open 2024, 7, e2432041. [Google Scholar] [CrossRef] [PubMed]
- Checa-Betegón, P.; Luque-Pérez, R.; Oñate-Martínez-Olascoaga, D.; Pérez-González, J.L.; Domínguez-Esteban, I. Osteoporotic vertebral fractures: Natural history and impact. Rev. Esp. Cir. Ortop. Traumatol. 2024, 68, 587–596. [Google Scholar] [CrossRef]
- Al Taha, K.; Lauper, N.; Bauer, D.E.; Tsoupras, A.; Tessitore, E.; Biver, E.; Dominguez, D.E. Multidisciplinary and Coordinated Management of Osteoporotic Vertebral Compression Fractures: Current State of the Art. J. Clin. Med. 2024, 13, 930. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.D.; Kim, E.H.; Lee, J.C.; Choi, S.W.; Kim, H.S.; Cha, J.S.; Shin, B.J. Management of Osteoporotic Vertebral Fracture: Review Update 2022. Asian Spine J. 2022, 16, 934–946. [Google Scholar] [CrossRef]
- Jang, H.D.; Kim, E.H.; Lee, J.C.; Choi, S.W.; Kim, K.; Shin, B.J. Current Concepts in the Management of Osteoporotic Vertebral Fractures: A Narrative Review. Asian Spine J. 2020, 14, 898–909. [Google Scholar] [CrossRef] [PubMed]
- Benditz, A.; Jerosch, J. Osteoporotic vertebral fractures-From diagnosis to treatment. Z. Rheumatol. 2023, 82, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Floyd, L.; Morris, A.D.; Woywodt, A.; Dhaygude, A. Cardiovascular disease and ANCA-associated vasculitis: Are we missing a beat? Clin. Kidney J. 2022, 15, 618–623. [Google Scholar] [CrossRef]
- Houben, E.; Penne, E.L.; Voskuyl, A.E.; van der Heijden, J.W.; Otten, R.H.J.; Boers, M.; Hoekstra, T. Cardiovascular events in anti-neutrophil cytoplasmic antibody-associated vasculitis: A meta-analysis of observational studies. Rheumatology 2018, 57, 555–562. [Google Scholar] [CrossRef]
- Massicotte-Azarniouch, D.; Petrcich, W.; Walsh, M.; Canney, M.; Hundemer, G.L.; Milman, N.; Hladunewich, M.A.; Fairhead, T.; Sood, M.M. Association of anti-neutrophil cytoplasmic antibody-associated vasculitis and cardiovascular events: A population-based cohort study. Clin. Kidney J. 2021, 15, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Clifford, A.H.; Cohen Tervaert, J.W. Cardiovascular events and the role of accelerated atherosclerosis in systemic vasculitis. Atherosclerosis 2021, 325, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.L.; Liang, Q.H.; Huang, B.T.; Ding, N.; Li, B.W.; Hao, J. The plasma level of mCRP is linked to cardiovascular disease in antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Res. Ther. 2020, 22, 228. [Google Scholar] [CrossRef]
- Vegting, Y.; Penne, E.L.; Hilhorst, M.L.; Hoekstra, T.; Bemelman, F.J.; Vogt, L.; Voskuyl, A.E.; Pagnoux, C.; Houben, E. Traditional and disease-related cardiovascular risk factors in ANCA-associated vasculitis: A prospective, two-centre cohort study. Jt. Bone Spine 2023, 90, 105540. [Google Scholar] [CrossRef]
- Granel, J.; Korkmaz, B.; Nouar, D.; Weiss, S.A.I.; Jenne, D.E.; Lemoine, R.; Hoarau, C. Pathogenicity of Proteinase 3-Anti-Neutrophil Cytoplasmic Antibody in Granulomatosis with Polyangiitis: Implications as Biomarker and Future Therapies. Front. Immunol. 2021, 12, 571933. [Google Scholar] [CrossRef] [PubMed]
- Sayer, M.; Gavin, C.; Matthew, T.; Neeraj, D. Cardiovascular Disease in Anti-neutrophil Cytoplasm Antibody-Associated Vasculitis. Curr. Rheumatol. Rep. 2024, 26, 12–23. [Google Scholar] [CrossRef]






| First Author Year of Publication Reference Number | Patient’ Age (Years) Sex | Features of the Aortic Involvement Associated Symptoms/Signs | Granulomatosis with Polyangiitis | Outcome of the Aortic Lesion | ||
|---|---|---|---|---|---|---|
| Disease-Related Involvement | ANCA Profile | Treatment | ||||
| Tzanninis 2022 [46] | 58 M | Ascending aorta: aortitis and thrombus Chest pain, vomiting, and hemoptysis | Migratory arthritis Episcleritis | PR3-ANCA (74 UI/mL) | PT: UFH, W, GC, and CYC | Complete resolution of ascending aorta thrombus lesion |
| Rodriguez- Padilla 2021 [47] | 74 M | Thoracic aorta: irregular peri-aortic mass surrounding the aortic graft Fever, epistaxis, cough, hemoptysis, and weight loss | Aorto-aortic bypass | cANCA (>1/20) PR3-ANCA (33 UI/mL) | PT: GC and MTX | Dimensional reduction of peri-aortic mass |
| Hesford 2021 [48] | 61 F | Aortic arch: infiltrative wall process Thoracic back pain, progressive dyspnea, dry cough, and night sweats | Pulmonary infiltrates Chronic nasal congestion Hilar lymphadenopathy | PR3-ANCA (60–90 UI/mL) | PT: GC, CYC, and RTX | Clinical, serological, and radiological remission |
| Bernal 2019 [49] | 34 M | Ascending aorta: circumferential wall thickening Facial swelling, nasal congestion, epistaxis, and progressive vision and weight loss | ENT Necrotizing scleritis Pan-uveitis | cANCA (>1/4) PR3-ANCA (>8 UI/mL) | PT: GC, RTX, and MTX | Significant decrease in the wall thickening around the ascending aorta + improvement in vision from the left eye, but no change from the right |
| Pan 2019 [50] | 28 M | Thoracic aorta: dissection and aortic hematoma Aortitis Chest pain | Scleritis Conjunctivitis Arthritis | PR3-ANCA (180 UI/mL) MPO-ANCA (10 UI/mL) | PT: GC and CYC | Stable condition upon surgery: ascending aorta and arch replacement |
| Parperis 2019 [51] | 71 F | Ascending aorta + aortic arch: thickening of the aortic wall Headache | Left eye blindness | pANCA (159 UI/mL) | PT: GC and MTX | Clinical and serological regression |
| Kim 2018 [52] | 58 M | Ascending aorta: eccentric thickening of the aortic wall Mid-sternal pain, fever, and cough | Pulmonary infiltrates Hilar lymphadenopathy Scleral keratitis Pituitary adenoma resection | cANCA positive | PT: GC | Dimensional reduction in peri-aortic mass and pulmonary nodule |
| Revilla 2016 [53] | 74 M | Abdominal aorta: soft tissue mass around the infrarenal aorta Back pain | Pulmonary infiltrates Pleural effusion Aorto-bifemoral bypass | cANCA (>1/20) PR3-ANCA (38 UI/mL) | PT: GC and MTX | Dimensional reduction in peri-aortic mass and pulmonary infiltrates |
| Ozaki 2015 [54] | 60 F | Aortic arch + abdominal aorta: wall thickening Fever, epistaxis, and nasal obstruction | ENT Pulmonary infiltrates with cavities Skin ulcers | PR3-ANCA (153 UI/mL) | PT: GC, CYC, RTX, and AZA | Clinical, serological, and radiological remission |
| Ohta 2013 [55] | 38 M | Thoracic aorta: dissection and rupture of aortic aneurysm Chest and back pain and loss of consciousness | ENT Glomerulonephritis | cANCA (x128) | PT: GC | Clinical and radiological remission upon surgery (J-graft insertion) |
| Amos 2012 [56] | 64 M | Aortic arch + abdominal aorta: circumferential wall thickening Fever, malaise, dysuria, hematuria, and intermittent chest pain | Glomerulonephritis Diffuse alveolar hemorrhage | PR3-ANCA (55 UI/mL) | PT: GC, CYC, and MTX Plasma exchanges Hemodialysis | Slow regression of clinical manifestations |
| Shmagel 2011 [57] | 68 F | Abdominal aorta: aneurysm and soft tissue mass around the infrarenal aorta Low abdominal pain | ENT Respiratory failure | cANCA (>1/20) PR3-ANCA (>100 UI/mL) | PT: GC, CYC, and MTX | Dimensional reduction of peri-aortic mass |
| Unlü 2011 [58] | 43 M | Abdominal aorta: aneurysm and soft tissue mass around the infrarenal aorta Abdominal pain and generalized malaise | ENT nasopharyngeal ulceration Glomerulonephritis | NA | PT: GC | Clinical and radiological remission (Surgery: aorto-bi-iliac Dacron graft) |
| Minnee 2009 [59] | 51 M | Abdominal aorta: aneurysm of the distal part of the aorta Low back pain and weakness of the upper and lower extremities with sensory loss | Testis The peripheral nerve system Skin | PR3-ANCA (>530 kU/L) | PT: GC, CYC, and Iloprost | Clinical remission |
| Carels 2004 [60] | 63 M | Abdominal aorta: aneurysm of the distal part of the aorta Low back pain and paresthesia in the lower limbs | Lungs Bowel Polyneuropathy in the lower limbs | pANCA—positive | PT: GC | Clinical and serological remission (Surgery: aorto-bi-iliac Dacron graft) |
| Schildhaus 2002 [61] | 63 M | Thoracic aorta: inflammatory lesions Weight loss, dyspnea, peripheral edema, and arthralgias | Skin | cANCA (1:320) PR3-ANCA (>100 U/mL) | Conservative treatment | Death: circulatory collapse |
| Blockmans 2000 [62] | 42 M | Abdominal aorta: peri-aortitis and intramural dissection Abdominal pain | ENT Lungs Arthralgia Muscle weakness Paranesthesia | cANCA (1/1280) PR3-ANCA (55 UI/mL) | PT: GC and CYC | Slow recovery upon surgery: aorto-iliac graft + re-implantation of inferior mesenteric artery |
| Fink 1994 [63] | 45 M | Abdominal aorta: wall thickening around the aorta, extending to the right iliac artery Intermittent right abdominal pain, malaise | ENT Lungs | cANCA positive | PT: GC, CYC | Good |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciobica, M.-L.; Botezatu, A.-S.; Galajda, Z.; Carsote, M.; Nistor, C.; Sandulescu, B.-A. Minimally Invasive Surgical Approach in Granulomatosis with Polyangiitis Complicated with Intramural Descending Aorta Hematoma Followed by Aortic Wall Rupture. Diagnostics 2025, 15, 144. https://doi.org/10.3390/diagnostics15020144
Ciobica M-L, Botezatu A-S, Galajda Z, Carsote M, Nistor C, Sandulescu B-A. Minimally Invasive Surgical Approach in Granulomatosis with Polyangiitis Complicated with Intramural Descending Aorta Hematoma Followed by Aortic Wall Rupture. Diagnostics. 2025; 15(2):144. https://doi.org/10.3390/diagnostics15020144
Chicago/Turabian StyleCiobica, Mihai-Lucian, Alexandru-Sebastian Botezatu, Zoltan Galajda, Mara Carsote, Claudiu Nistor, and Bianca-Andreea Sandulescu. 2025. "Minimally Invasive Surgical Approach in Granulomatosis with Polyangiitis Complicated with Intramural Descending Aorta Hematoma Followed by Aortic Wall Rupture" Diagnostics 15, no. 2: 144. https://doi.org/10.3390/diagnostics15020144
APA StyleCiobica, M.-L., Botezatu, A.-S., Galajda, Z., Carsote, M., Nistor, C., & Sandulescu, B.-A. (2025). Minimally Invasive Surgical Approach in Granulomatosis with Polyangiitis Complicated with Intramural Descending Aorta Hematoma Followed by Aortic Wall Rupture. Diagnostics, 15(2), 144. https://doi.org/10.3390/diagnostics15020144










