Spinal Epidural Fat as an Imaging Biomarker of Visceral Obesity: An MRI-Based Quantitative Analysis
Abstract
1. Introduction
2. Materials and Methods
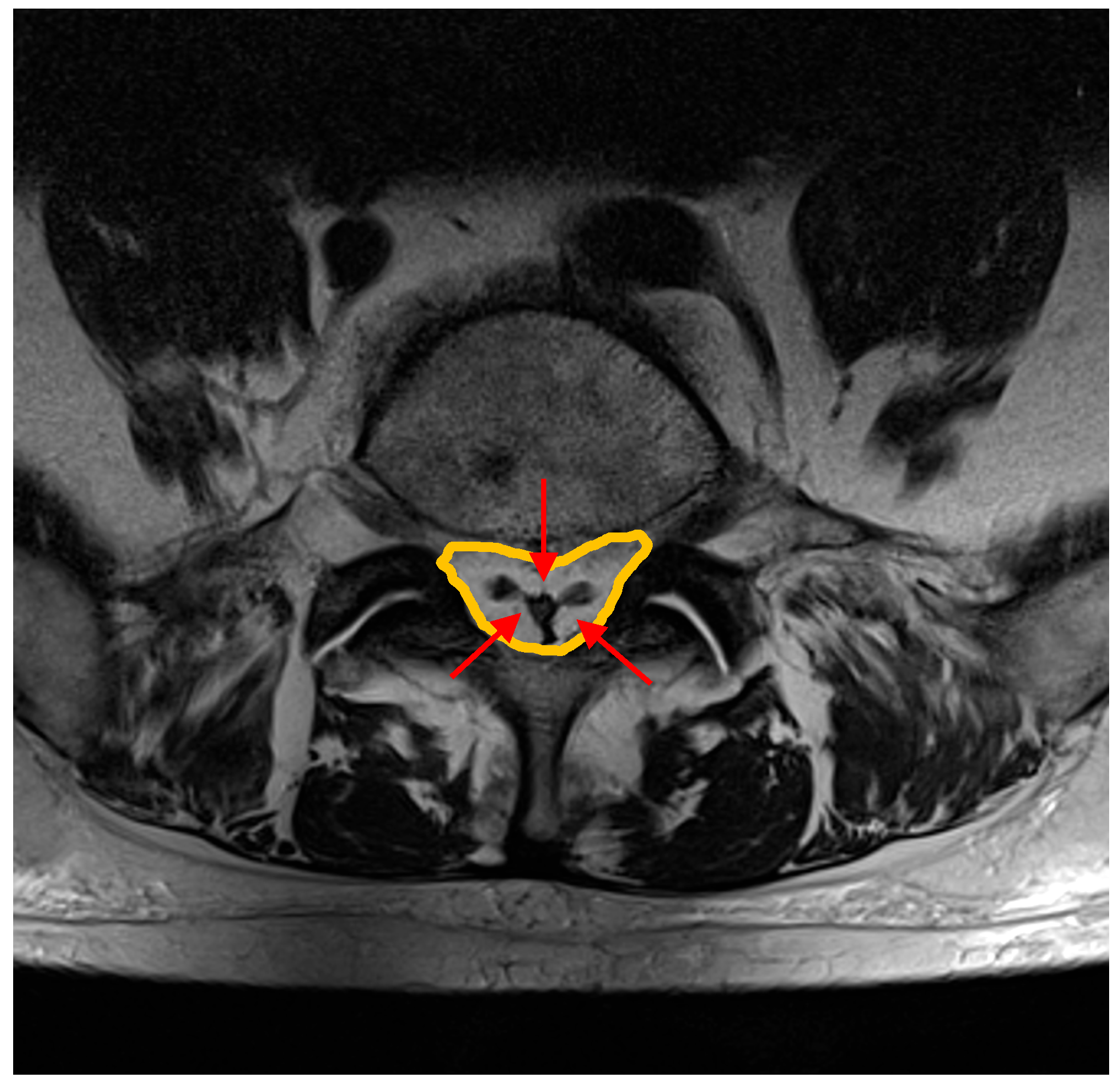
- Spinal canal antero-posterior diameter (SC), at the same level.
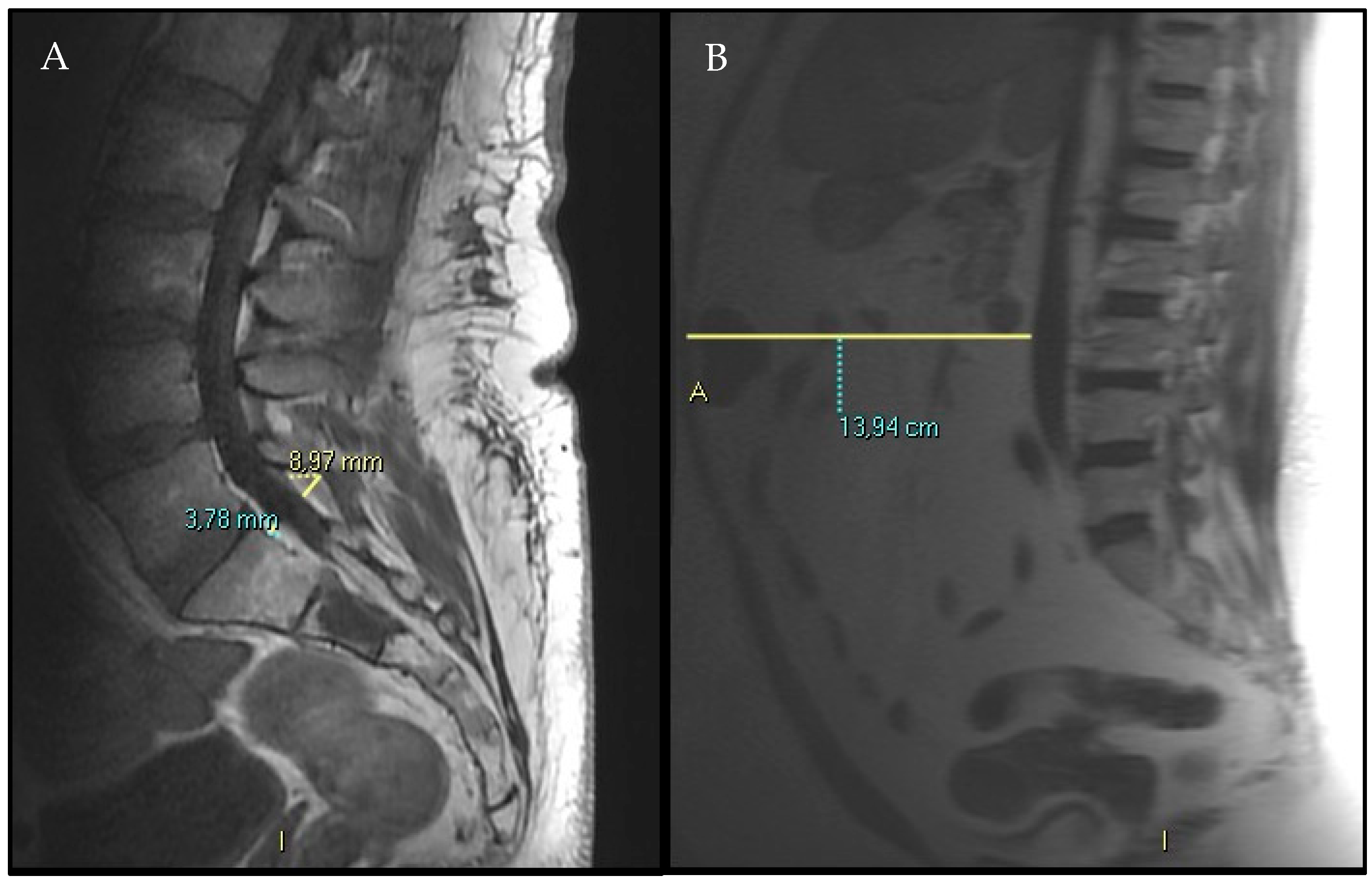
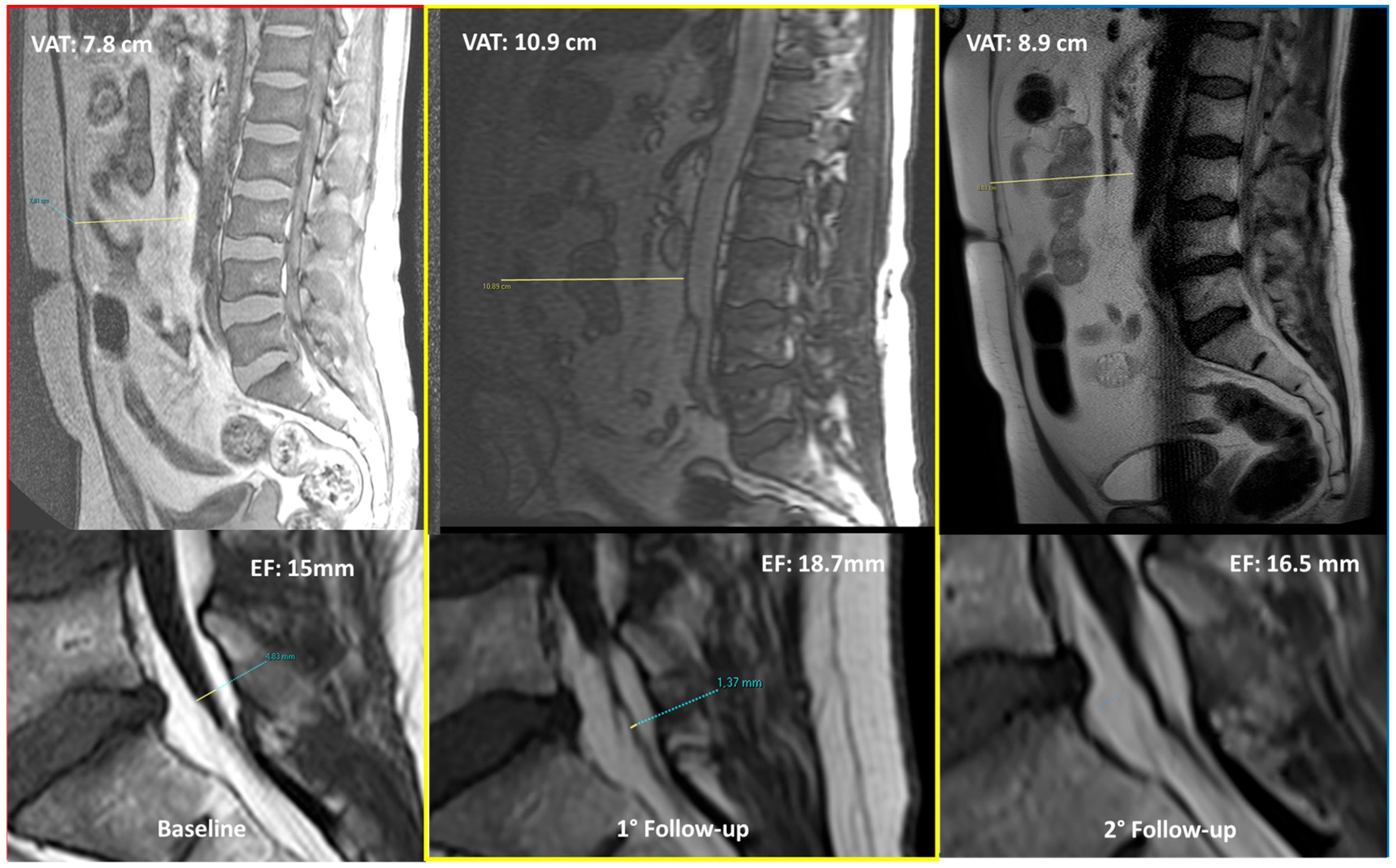
- VAT anterior–posterior max diameter at L3 level represented by the distance between the abdominal muscular fascia and the anterior wall of the abdominal aorta at the L3 vertebral level; MR-localizer sequences were used to achieve this aim (Figure 2, panel B).
- SF anterior–posterior diameter has been measured and recorded as well, whether it was comprised in the MR-localizer sequences at the same level (L3), anterior subcutaneous fat pad.
Statistical Analysis
3. Results
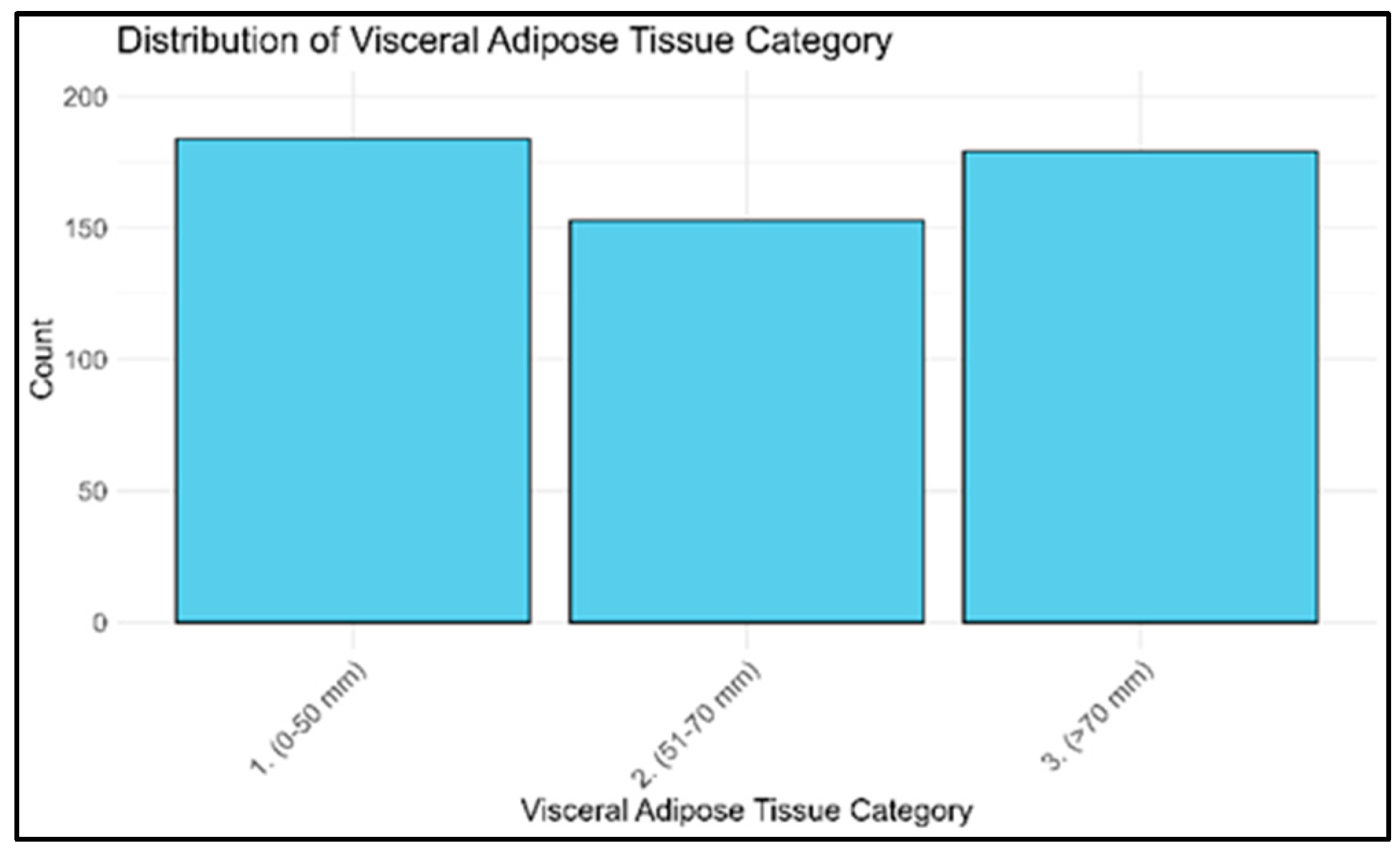
3.1. Patients’ Population and Selection
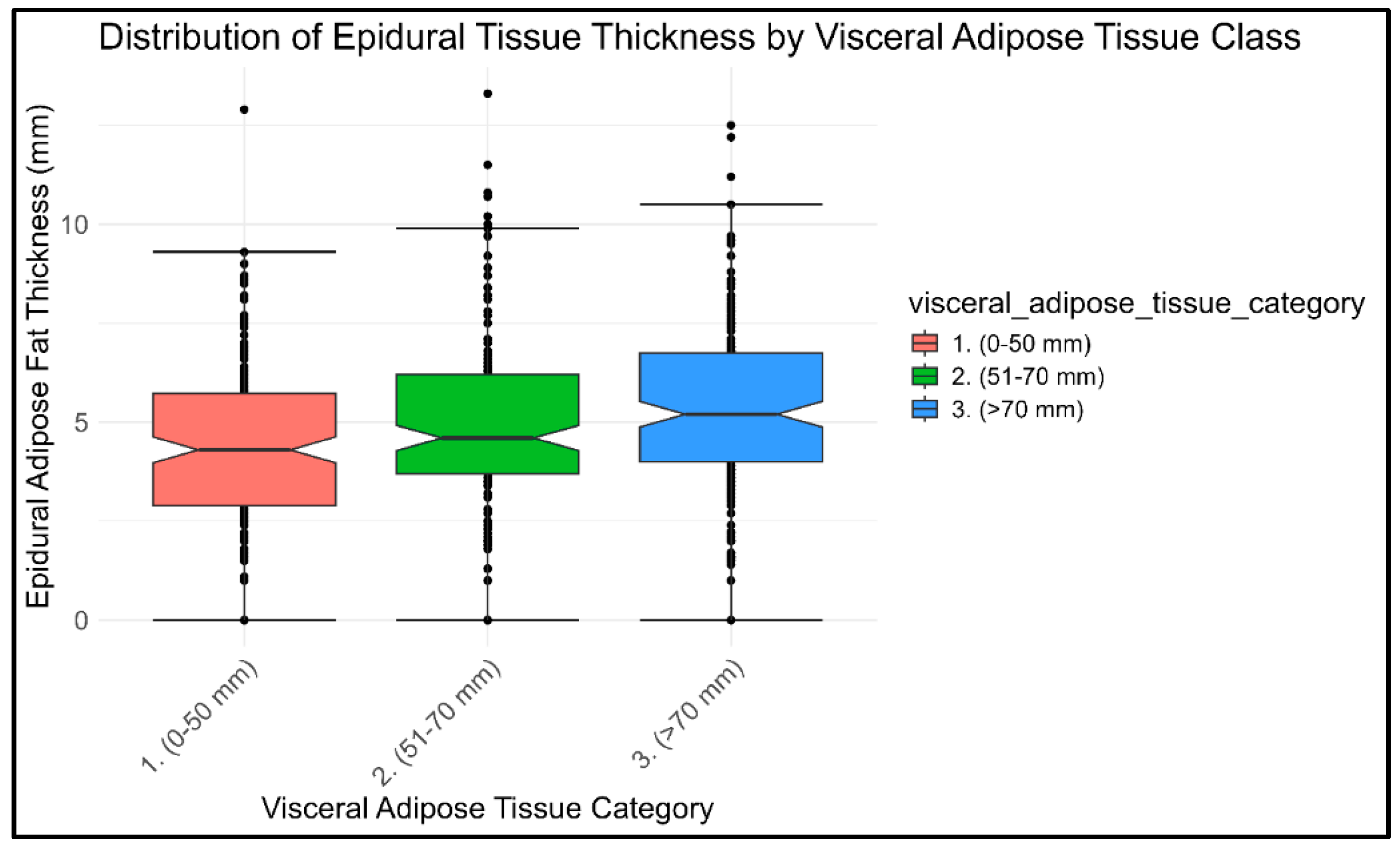
3.2. Visceral and Epidural Fat Associations
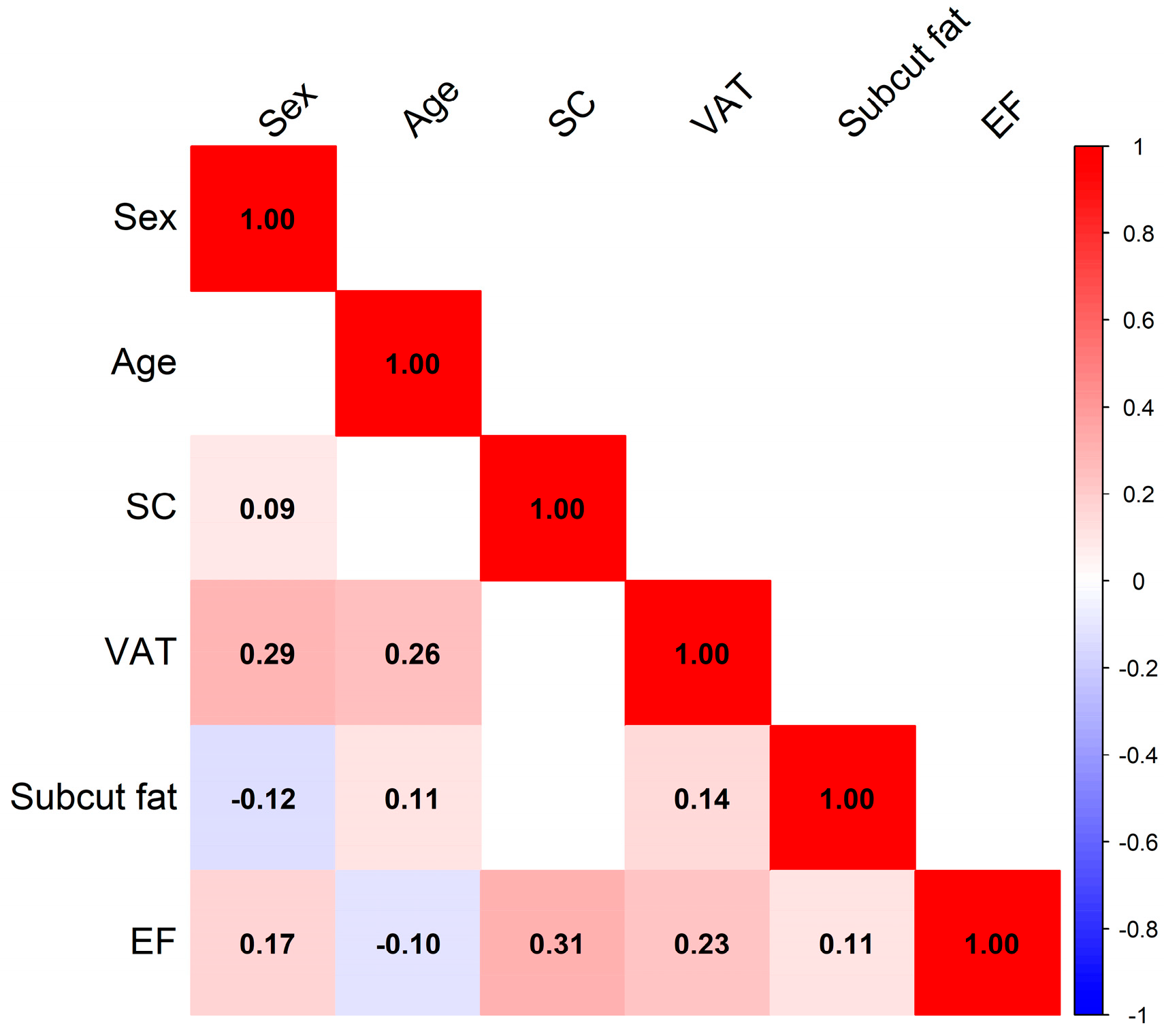
3.2.1. Correlation Analysis
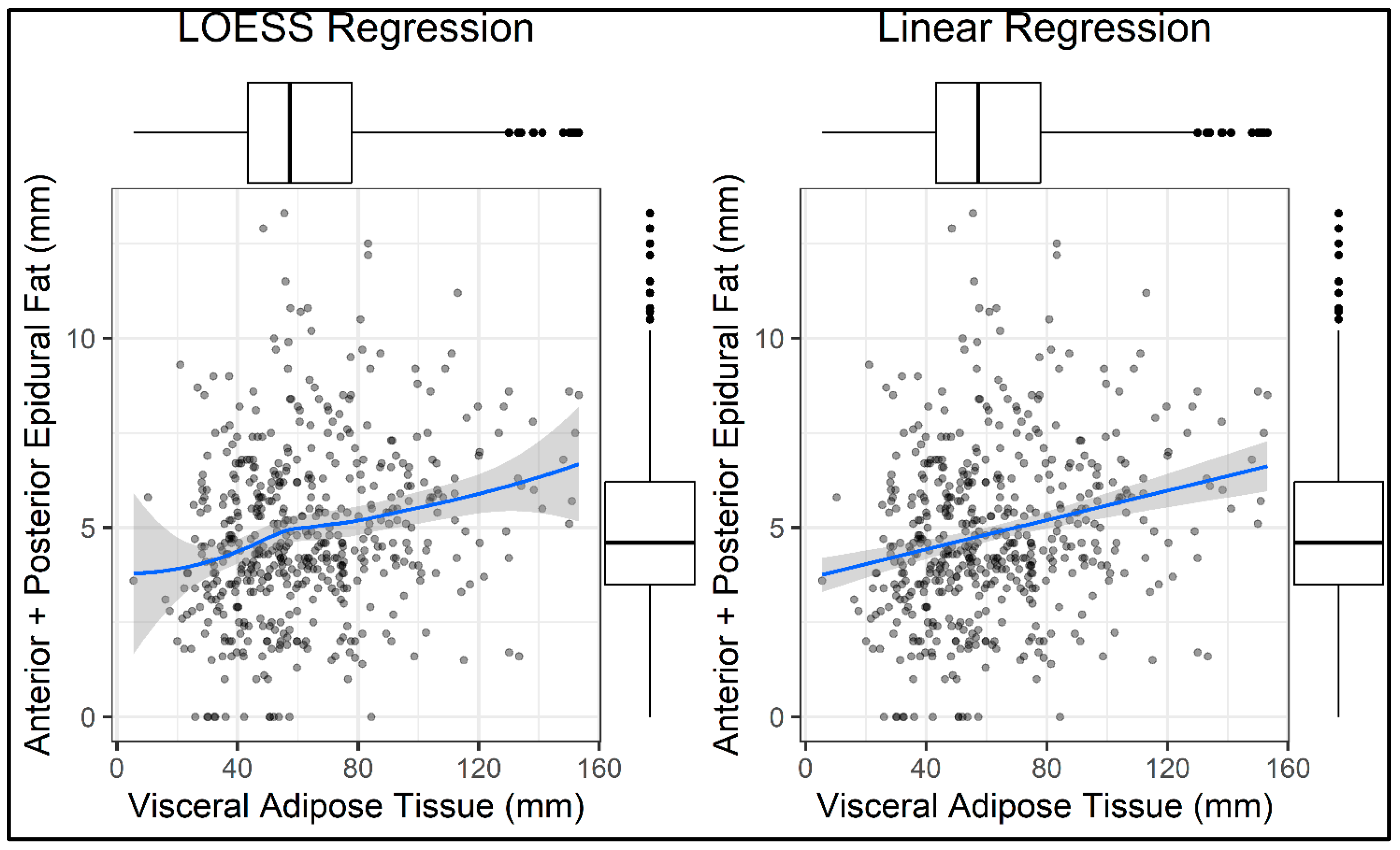
3.2.2. Linear Regression Model
3.3. Multivariate Regression Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Luo, X.; Tham, Y.C.; Giuffrè, M.; Ranisch, R.; Daher, M.; Lam, K.; Eriksen, A.V.; Hsu, C.W.; Ozaki, A.; de Moraes, F.Y.; et al. Reporting guideline for the use of Generative Artificial intelligence tools in MEdical Research: The GAMER Statement. BMJ Evid. Based Med. 2025. [Google Scholar] [CrossRef]
- Borrè, D.G.; Borrè, G.E.; Aude, F.; Palmieri, G.N. Lumbosacral epidural lipomatosis: MRI grading. Eur. Radiol. 2003, 13, 1709–1721. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, V.; Petrera, M.R.; Tedesco, G.; Pipola, V.; Ponti, F.; Spinnato, P. Could spinal epidural lipomatosis be the hallmark of metabolic syndrome on the spine? A literature review with emphasis on etiology. Diagnostics 2023, 13, 322. [Google Scholar] [CrossRef]
- Theyskens, N.C.; Paulino Pereira, N.R.; Boland, P.J.; Healey, J.H. Epidural lipomatosis: A 10-year MRI-based epidemiologic analysis. Skelet. Radiol. 2017, 46, 1743–1749. [Google Scholar]
- Theyskens, N.C.; Paulino Pereira, N.R.; Janssen, S.J.; Bono, C.M.; Schwab, J.H.; Cha, T.D. The prevalence of spinal epidural lipomatosis on magnetic resonance imaging. Spine J. 2017, 17, 969–976. [Google Scholar] [CrossRef]
- Mallard, F.; Buni, M.; Nolet, P.S.; Emary, P.; Taylor, J.A.; Moammer, G. Lumbar spinal epidural lipomatosis: A case report and review of the literature. Int. J. Surg. Case Rep. 2021, 78, 71–75. [Google Scholar] [CrossRef]
- Lee, M.; Lekias, J.; Gubbay, S.S.; Hurst, P.E. Spinal cord compression by extradural fat after renal transplantation. Med. J. Aust. 1975, 1, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Sancini, G.; Amadori, E.; Cenni, P.; Palleschi, M.; Prochowski Iamurri, A. Breast cancer leptomeningeal metastases on spinal epidural lipomatosis. Diagnostics 2024, 14, 1496. [Google Scholar] [CrossRef] [PubMed]
- Fogel, G.R.; Cunningham, P.Y., III; Esses, S.I. Spinal epidural lipomatosis: Case reports, literature review and meta-analysis. Spine J. 2005, 5, 202–211. [Google Scholar] [CrossRef]
- Choi, K.C.; Kang, B.U.; Lee, C.D.; Lee, S.H. Rapid progression of spinal epidural lipomatosis. Eur. Spine J. 2011, 21, 408–412. [Google Scholar] [CrossRef]
- Youn, M.S.; Woo, Y.H.; Shin, J.K. Rapid progression of spinal epidural lipomatosis after percutaneous endoscopic spine surgery mimicking disc herniation. Int. J. Surg. Case Rep. 2020, 73, 1–4. [Google Scholar] [CrossRef]
- Vazquez, L.; Ellis, A.; Saint-Genez, D.; Patino, J.; Nogues, M. Epidural lipomatosis after renal transplantation—Complete recovery without surgery. Transplantation 1988, 46, 773–774. [Google Scholar] [CrossRef]
- Stern, J.D.; Quint, D.J.; Sweasey, T.A.; Hoff, J.T. Spinal epidural lipomatosis: Two new idiopathic cases and a review of the literature. J. Spinal Disord. 1994, 7, 343–349. [Google Scholar] [CrossRef]
- Tobler, W.D.; Weil, S. Epidural lipomatosis and renal transplantation. Surg. Neurol. 1988, 29, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Cersósimo, M.G.; Lasala, B.; Folgar, S.; Micheli, F. Epidural lipomatosis secondary to indinavir in an HIV-positive patient. Clin. Neuropharmacol. 2002, 25, 51–54. [Google Scholar] [CrossRef]
- Schurmann, D.; Rademaker, J.; Trottenberg, T.; Bergmann, F.; Wesselmann, H.; Suttorp, N. Spinal epidural lipomatosis: A manifestation of HAART-associated lipodystrophy. AIDS 2005, 19, 2052–2054. [Google Scholar] [CrossRef]
- López-González, A.; Giner, M.R. Idiopathic spinal epidural lipomatosis: Urgent decompression in an atypical case. Eur. Spine J. 2008, 17, 225–227. [Google Scholar] [CrossRef]
- Billings, F.; Hoyt, M. Epidural lipomatosis causing new debilitating back pain in a patient with human immunodeficiency virus on highly active antiretroviral therapy. Int. J. Obstet. Anesth. 2012, 21, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Spinnato, P.; Lotrecchiano, L.; Ponti, F. “Y” sign in spinal epidural lipomatosis. Jt. Bone Spine 2021, 88, 105056. [Google Scholar] [CrossRef] [PubMed]
- Robertson, S.C.; Traynelis, V.C.; Follett, K.A.; Menezes, A.H. Idiopathic spinal epidural lipomatosis. Neurosurgery 1997, 41, 68–74. [Google Scholar] [CrossRef]
- Papastefan, S.T.; Bhimani, A.D.; Denyer, S.; Khan, S.R.; Esfahani, D.R.; Nikas, D.C.; Mehta, A.I. Management of idiopathic spinal epidural lipomatosis: A case report and review of the literature. Childs Nerv. Syst. 2018, 34, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Ferlic, P.W.; Mannion, A.F.; Jeszenszky, D.; Porchet, F.; Fekete, T.F.; Kleinstück, F.; Haschtmann, D. Patient-reported outcome of surgical treatment for lumbar spinal epidural lipomatosis. Spine J. 2016, 16, 1333–1341. [Google Scholar] [CrossRef] [PubMed]
- Greenish, D.; Watura, K.; Harding, I. Spinal epidural lipomatosis following bilateral spinal decompression surgery. BMJ Case Rep. 2019, 12, e226985. [Google Scholar] [CrossRef]
- Praver, M.; Kennedy, B.C.; Ellis, J.A.; D’Amico, R.; Mandigo, C.E. Severity of presentation is associated with time to recovery in spinal epidural lipomatosis. J. Clin. Neurosci. 2015, 22, 1244–1249. [Google Scholar] [CrossRef]
- Al-Khawaja, D.; Seex, K.; Eslick, G.D. Spinal epidural lipomatosis—A brief review. J. Clin. Neurosci. 2008, 15, 1323–1326. [Google Scholar] [CrossRef] [PubMed]
- Morishita, S.; Arai, Y.; Yoshii, T.; Sakai, K.; Hirai, T.; Okawa, A. Lumbar epidural lipomatosis is associated with visceral fat and metabolic disorders. Eur. Spine J. 2018, 27, 487–493. [Google Scholar] [CrossRef]
- Muñoz, A.; Barkovich, J.A.; Mateos, F.; Simón, R. Symptomatic epidural lipomatosis of the spinal cord in a child: MR demonstration of spinal cord injury. Pediatr. Radiol. 2002, 32, 865–868. [Google Scholar] [CrossRef]
- Spinnato, P.; Ponti, F.; De Pasqua, S. MRI Diagnosis of Obesity-Related Spinal Epidural Lipomatosis. Can. J. Neurol. Sci. 2020, 47, 124–125. [Google Scholar] [CrossRef]
- Shimada, Y.; Ishikawa, Y.; Miyakoshi, N.; Suzuki, T.; Hongo, M.; Kasukawa, Y.; Okada, K.; Itoi, E. Decompression of idiopathic lumbar epidural lipomatosis: Diagnostic magnetic resonance imaging evaluation and review of the literature. J. Neurosurg. Spine 2006, 4, 24–30. [Google Scholar]
- Sugaya, H.; Tanaka, T.; Ogawa, T.; Mishima, H. Spinal epidural lipomatosis in lumbar magnetic resonance imaging scans. Orthopedics 2014, 37, e362–e366. [Google Scholar] [CrossRef]
- Spinnato, P.; D’Agostino, V.; Fiorenzo, D.; Barakat, M.; Vara, G.; Ponti, F.; Filonzi, G.; Crombé, A.; Tetta, C.; Miceli, M. Underreporting of spinal epidural lipomatosis: A retrospective analysis of lumbosacral MRI examinations from different radiological settings. Diagn. Interv. Imaging 2022, 103, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Bodelier, A.; Groeneveld, W.; Van Der Linden, A.; Haak, H. Symptomatic epidural lipomatosis in ectopic Cushing’s syndrome. Eur. J. Endocrinol. 2004, 151, 765–769. [Google Scholar] [CrossRef] [PubMed]
- Mukhtar, N.; Alzahrani, A.S. Spinal epidural lipomatosis: A rare and frequently unrecognized complication of Cushing syndrome. Endocrine 2022, 76, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Benamou, P.H.; Hilliquin, P.; Chemla, N.; Chevrot, A.; Cormier, C.; Menkès, C.J. Epidural lipomatosis not induced by corticosteroid therapy. Three cases including one in a patient with primary Cushing’s disease. Rev. Rhum. Engl. Ed. 1996, 63, 207–212. [Google Scholar]
- Koch, C.A.; Doppman, J.L.; Watson, J.C.; Patronas, N.J.; Nieman, L.K. Spinal epidural lipomatosis in a patient with the ectopic corticotropin syndrome. N. Engl. J. Med. 1999, 341, 1399–1400. [Google Scholar] [CrossRef]
- Bhatia, K.; Frydenberg, E.; Steel, T.; Ow-Yang, M.; Ho, K.; Grainger, E. Spinal epidural lipomatosis due to a bronchial ACTH-secreting carcinoid tumour. J. Clin. Neurosci. 2010, 17, 1461–1462. [Google Scholar] [CrossRef]
- Ahmad, S.; Best, T.; Lansdown, A.; Hayhurst, C.; Smeeton, F.; Davies, S.; Rees, A. Spinal epidural lipomatosis: A rare association of Cushing’s disease. Endocrinol. Diabetes Metab. Case Rep. 2020, 2020, 20-0111. [Google Scholar] [CrossRef]
- Al-Omari, A.A.; Obeidat, N.; Alnemer, A.F.; Dalou, A.A. Is there a relationship between lumbosacral epidural spinal injections and lumbosacral epidural lipomatosis? A retrospective study. Neurochirurgie 2025, 71, 101636. [Google Scholar] [CrossRef]
- Caruba, T.; Brunie, V.; Bousseau, V.; Guillemain, R.; Prognon, P.; Bégué, D.; Sabatier, B. Substitution of corticosteroid with everolimus after lung transplantation: A pediatric case report. Pharm. World Sci. 2010, 32, 347–349. [Google Scholar] [CrossRef]
- Möller, J.; Girschick, H.; Hahn, G.; Pessler, F. Steroid-induced spinal epidural lipomatosis in pediatric patients. Z Rheumatol. 2010, 69, 447–449. [Google Scholar] [CrossRef]
- Jaimes, R., III; Rocco, A.G. Multiple epidural steroid injections and body mass index linked with the occurrence of epidural lipomatosis: A case series. BMC Anesthesiol. 2014, 14, 70. [Google Scholar] [CrossRef]
- Zentner, J.; Buchbender, K.; Vahlensieck, M. Spinal epidural lipomatosis is a complication of prolonged corticosteroid therapy. J. Neurosurg. Sci. 1995, 39, 81–85. [Google Scholar]
- Pinsker, M.O.; Kinzel, D.; Lumenta, C.B. Epidural thoracic lipomatosis induced by long-term steroid treatment case illustration. Acta Neurochir. 1998, 140, 991–992. [Google Scholar] [CrossRef]
- Kotilainen, E.; Hohenthal, U.; Karhu, J.; Kotilainen, P. Spinal epidural lipomatosis caused by corticosteroid treatment in ulcerative colitis. Eur. J. Intern. Med. 2006, 17, 138–140. [Google Scholar] [CrossRef]
- Koch, C.A.; Doppman, J.L.; Patronas, N.J.; Nieman, L.K.; Chrousos, G.P. Do glucocorticoids cause spinal epidural lipomatosis? When endocrinology and spinal surgery meet. Trends Endocrinol. Metab. 2000, 11, 86–90. [Google Scholar] [CrossRef]
- Fessler, R.G.; Johnson, D.L.; Brown, F.D.; Erickson, R.K.; Reid, S.A.; Kranzler, L. Epidural lipomatosis in steroid-treated patients. Spine 1992, 17, 183–188. [Google Scholar] [CrossRef]
- McCullen, G.M.; Spurling, G.R.; Webster, J.S. Epidural lipomatosis complicating lumbar steroid injections. J. Spinal Disord. 1999, 12, 526–529. [Google Scholar] [CrossRef] [PubMed]
- Roy-Camille, R.; Mazel, C.; Husson, J.L.; Saillant, G. Symptomatic spinal epidural lipomatosis induced by long-term steroid treatment. Review of the literature and report of two additional cases. Spine 1991, 16, 1365–1371. [Google Scholar] [CrossRef]
- Sandberg, D.I.; Lavyne, M.H. Symptomatic spinal epidural lipomatosis after local epidural corticosteroid injections: Case report. Neurosurgery 1999, 45, 162–165. [Google Scholar] [PubMed]
- Vince, G.H.; Brucker, C.; Langmann, P.; Herbold, C.; Solymosi, L.; Roosen, K. Epidural spinal lipomatosis with acute onset of paraplegia in an HIV-positive patient treated with corticosteroids and protease inhibitor: Case report. Spine 2005, 30, E524–E527. [Google Scholar] [CrossRef] [PubMed]
- Ebright, J.R.; Stellini, M.A.; Tselis, A.C. Spinal epidural lipomatosis in a human immunodeficiency virus-positive patient receiving steroids and protease inhibitor therapy. Clin. Infect. Dis. 2001, 32, e90–e91. [Google Scholar] [CrossRef]
- Zhang, B.; Yuan, H.; Hu, L.; Saad, M. Obesity is a risk factor for epidural lipomatosis. A meta-analysis. J. Orthop. Surg. 2021, 29, 23094990211027391. [Google Scholar]
- Noh, E. An unusual complication of morbid obesity: Epidural lipomatosis. Am. J. Emerg. Med. 2015, 33, 742.e3–742.e4. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, B.; Puvanesarajah, V.; An, H.S.; Novicoff, W.M.; Jain, A.; Shen, F.H.; Hassanzadeh, H. Lumbosacral Epidural Lipomatosis: A Retrospective Matched Case-Control Database Study. World Neurosurg. 2016, 96, 209–214. [Google Scholar] [CrossRef]
- Fassett, D.R.; Schmidt, M.H. Spinal epidural lipomatosis: A review of its causes and recommendations for treatment. Neurosurg. Focus 2004, 16, E11. [Google Scholar] [CrossRef]
- Kumar, K.; Nath, R.K.; Nair, C.P.V.; Tchang, S.P. Symptomatic epidural lipomatosis secondary to obesity. Case report. J. Neurosurg. 1996, 85, 348–350. [Google Scholar] [CrossRef]
- Yki-Järvinen, H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014, 2, 901–910. [Google Scholar] [CrossRef]
- Abe, T.; Miyazaki, M.; Ishihara, T.; Kanezaki, S.; Notani, N.; Kataoka, M.; Tsumura, H. Spinal epidural lipomatosis is associated with liver fat deposition and dysfunction. Clin. Neurol. Neurosurg. 2019, 185, 105480. [Google Scholar] [CrossRef]
- Spinnato, P.; Barakat, M.; Lotrecchiano, L.; Giusti, D.; Filonzi, G.; Spinellim, D.; Pipola, V.; Moio, A.; Tetta, C.; Ponti, F. MRI Features and Clinical Significance of Spinal Epidural Lipomatosis: All You Should Know. Curr. Med. Imaging 2022, 18, 208–215. [Google Scholar] [CrossRef]
- Spinnato, P.; Petrera, M.R.; Parmeggiani, A.; Manzetti, M.; Ruffilli, A.; Faldini, C.; D’aGostino, V.; Di Carlo, M.; Cumani, M.P.; Crombé, A.; et al. A new comprehensive MRI classification and grading system for lumbosacral central and lateral stenosis: Clinical application and comparison with previous systems. Radiol. Med. 2024, 129, 93–106. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Zimmet, P.; Shaw, J. The metabolic syndrome--a new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Ginsberg, H.N. Insulin resistance and cardiovascular disease. J. Clin. Investig. 2000, 106, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Reaven, G.; Abbasi, F.; McLaughlin, T. Obesity, insulin resistance, and cardiovascular disease. Recent Prog. Horm. Res. 2004, 59, 207–223. [Google Scholar] [CrossRef]
- Saltiel, A.R.; Olefsky, J.M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Investig. 2017, 127, 1–4. [Google Scholar] [CrossRef]
- Lumeng, C.N.; Saltiel, A.R. Inflammatory links between obesity and metabolic disease. J. Clin. Investig. 2011, 121, 2111–2117. [Google Scholar] [CrossRef]
- Rigsby, R.K.; Barnes, S.; Sabaté, J.; Oyoyo, U.; Chowdhury, S.; Peters, E.M. Correlation of spinal epidural fat volume with body mass index: A longitudinal study. Clin. Imaging 2023, 98, 61–66. [Google Scholar] [CrossRef]
- Ishihara, S.; Fujita, N.; Azuma, K.; Michikawa, T.; Yagi, M.; Tsuji, T.; Takayama, M.; Matsumoto, H.; Nakamura, M.; Matsumoto, M.; et al. Spinal epidural lipomatosis is a previously unrecognized manifestation of metabolic syndrome. Spine J. 2019, 19, 493–500. [Google Scholar] [CrossRef]

| Min. | 1st Qu. | Median | Mean | 3rd Qu. | Max. |
|---|---|---|---|---|---|
| 5.50 | 43.10 | 56.80 | 62.10 | 77.12 | 153.20 |
| VAT Group Comparison | Mean Difference in EF Thickness (mm) | 95% Confidence Interval | p-Value |
|---|---|---|---|
| 0–50 mm vs. 51–70 mm | 0.58 | 0.01–1.16 | 0.04 * |
| 0–50 mm vs. >70 mm | 1.02 | 0.47–1.58 | 0.00005 *** |
| 51–70 mm vs. >70 mm | 0.44 | −0.14–1.02 | 0.18 |
| Variable | Estimate (mm) | Std. Error | p-Value |
|---|---|---|---|
| Intercept | 3.65 | 0.25 | <2 × 10−16 *** |
| VAT | 0.02 | 0.004 | 7.75 × 10−7 *** |
| Variable | Estimate | Std. Error | p-Value | Adjusted R2 |
|---|---|---|---|---|
| Age | −0.013 | 0.006 | 0.006 *** | 0.008 |
| Sex | 0.81 | 0.20 | 8.02 × 10−5 *** | 0.03 |
| Subcutaneous Adipose Tissue (mm) | 0.026 | 0.01 | 0.01 * | 0.011 |
| Spinal Canal Diameter (mm) | 0.175 | 0.024 | 0.02 * | 0.09 |
| Variable | Estimate | Std. Error | p-Value | Tolerance |
|---|---|---|---|---|
| (Intercept) | 1.68 | 0.56 | 0.003 ** | – |
| Age | −0.02 | 0.01 | 2.94 × 10−5 *** | 0.95 |
| Sex | 0.30 | 0.21 | 0.15 | 0.87 |
| Spinal Canal Diameter (mm) | 0.17 | 0.02 | 9.59 × 10−12 *** | 0.96 |
| Visceral Adipose Tissue (mm) | 0.02 | 0.004 | 7.75 × 10−6 *** | 0.87 |
| Subcutaneous Adipose Tissue (mm) | 0.01 | 0.01 | 0.16 | 0.94 |
| canal × VAT interaction | −0.12 | 0.10 | 0.23 | 0.97 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marrone, N.; Bilancia, G.; Romeo, D.; D’Agostino, V.; Ponti, F.; Salamanna, F.; Crombé, A.; Spinnato, P. Spinal Epidural Fat as an Imaging Biomarker of Visceral Obesity: An MRI-Based Quantitative Analysis. Diagnostics 2025, 15, 2490. https://doi.org/10.3390/diagnostics15192490
Marrone N, Bilancia G, Romeo D, D’Agostino V, Ponti F, Salamanna F, Crombé A, Spinnato P. Spinal Epidural Fat as an Imaging Biomarker of Visceral Obesity: An MRI-Based Quantitative Analysis. Diagnostics. 2025; 15(19):2490. https://doi.org/10.3390/diagnostics15192490
Chicago/Turabian StyleMarrone, Nicola, Gabriele Bilancia, Domenico Romeo, Valerio D’Agostino, Federico Ponti, Francesca Salamanna, Amandine Crombé, and Paolo Spinnato. 2025. "Spinal Epidural Fat as an Imaging Biomarker of Visceral Obesity: An MRI-Based Quantitative Analysis" Diagnostics 15, no. 19: 2490. https://doi.org/10.3390/diagnostics15192490
APA StyleMarrone, N., Bilancia, G., Romeo, D., D’Agostino, V., Ponti, F., Salamanna, F., Crombé, A., & Spinnato, P. (2025). Spinal Epidural Fat as an Imaging Biomarker of Visceral Obesity: An MRI-Based Quantitative Analysis. Diagnostics, 15(19), 2490. https://doi.org/10.3390/diagnostics15192490







