Does the Position of the Mandibular Third Molar Have an Effect on the Lingual Bone Morphology? A Cone Beam Computed Tomography Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
- Age ≥ 18 years.
- Presence of mandibular third molars that were impacted.
- CBCT images including the entire mandibular body.
- Patients under 18 years of age.
- Cases with the presence of caries, bone destruction, or any other pathologies.
- Missing first or second molars in the same quadrant.
- Images with artifacts or insufficient diagnostic quality.
2.2. CBCT Image Acquisition and Analysis
2.3. Radiological Assessments and Parameters
- Impaction Classification: Each impacted third molar was classified based on Pell & Gregory’s classification (for ramus relationship and occlusal level) and Winter’s classification (for angulation).
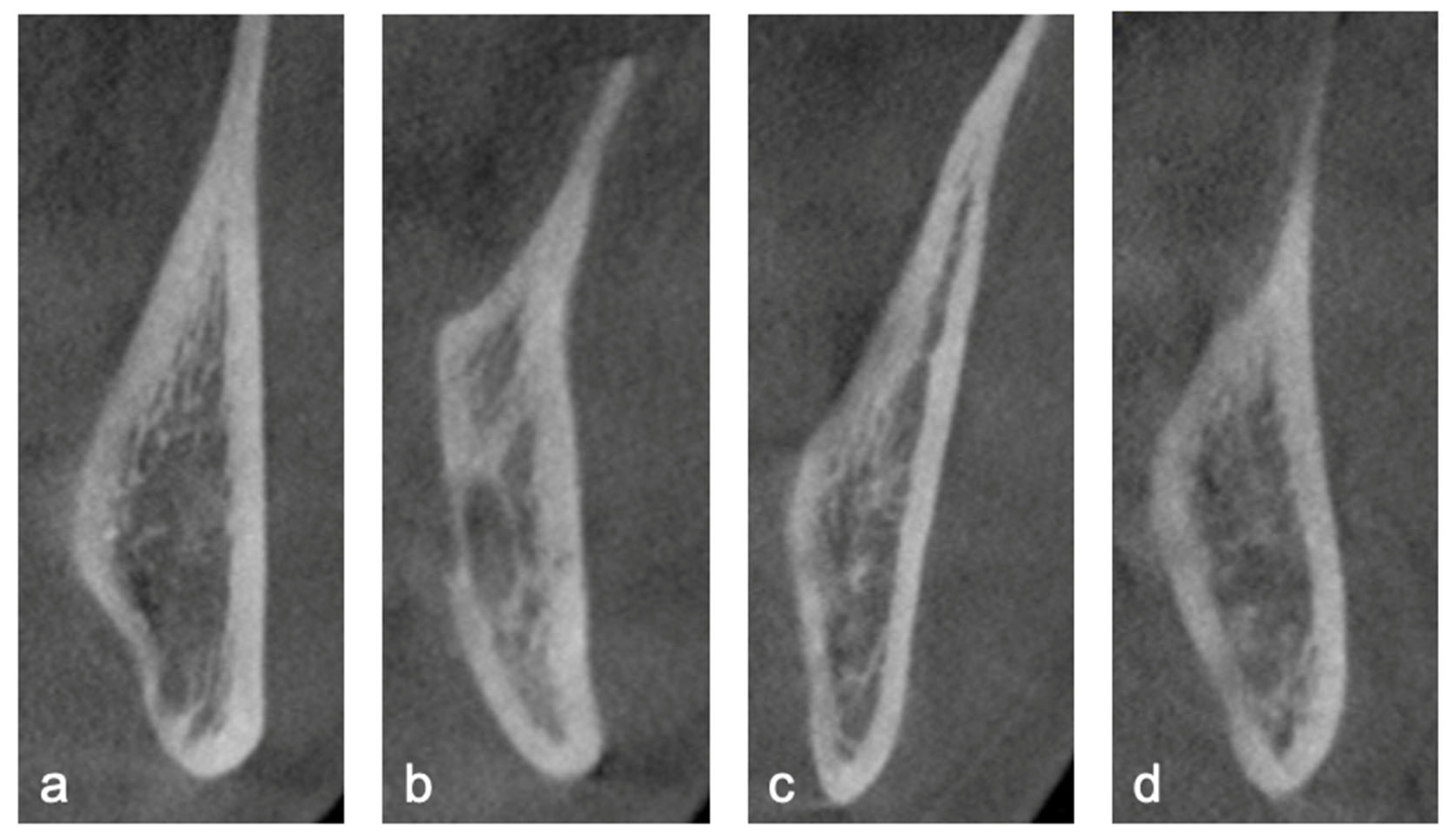
- Lingual Plate Morphology: Morphology of the lingual cortical bone at the level of the root apex was classified as undercut, parallel, slanted, or round (Figure 1).
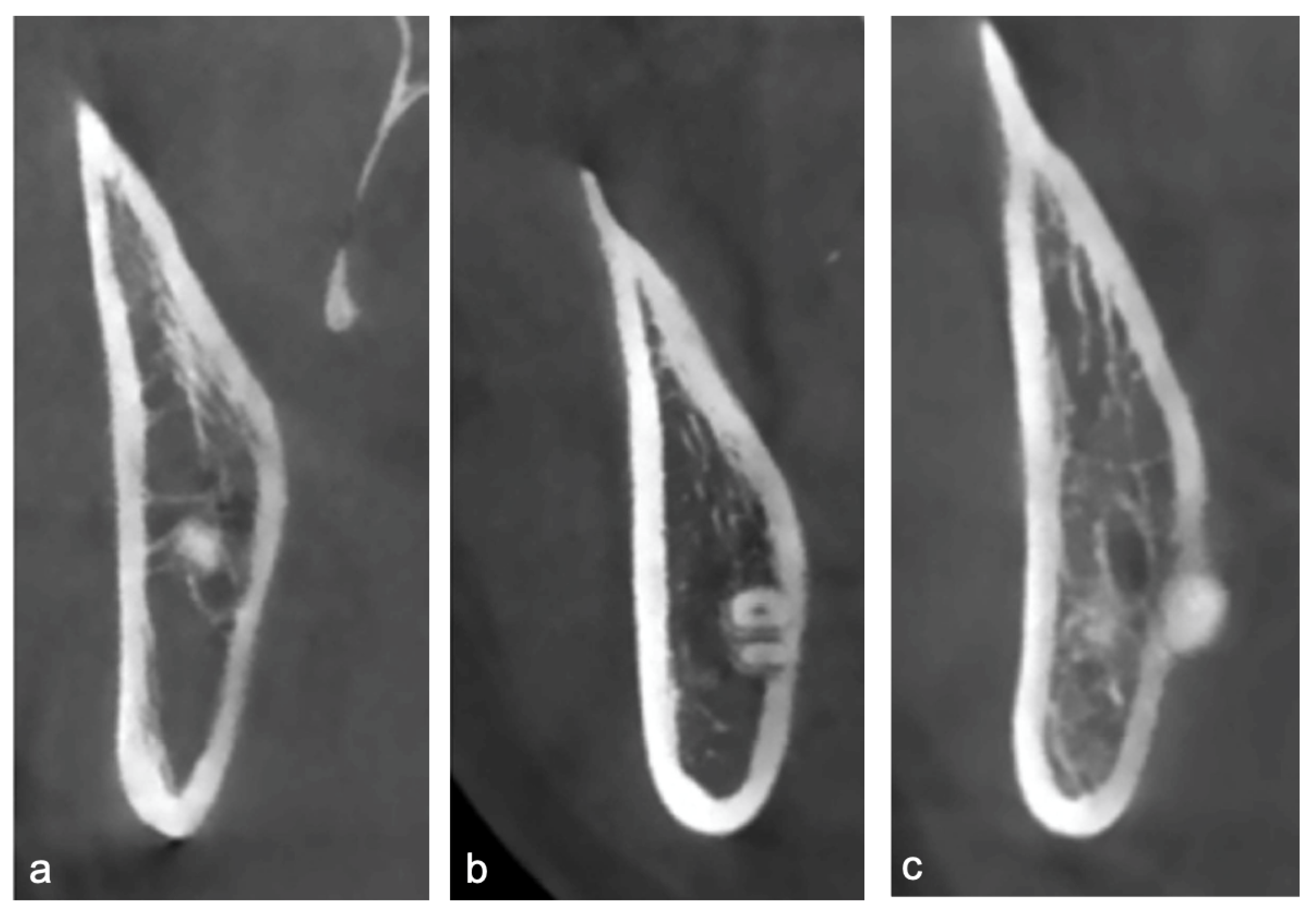
- Root Apex Position: The topographic relationship between the root apex and the lingual plate was categorized as non-contact, contact, or perforating (Figure 2). The presence or absence of lingual cortical perforation was assessed at three anatomical levels of each impacted mandibular third molar: the cementoenamel junction (CEJ), mid-root, and root apex.
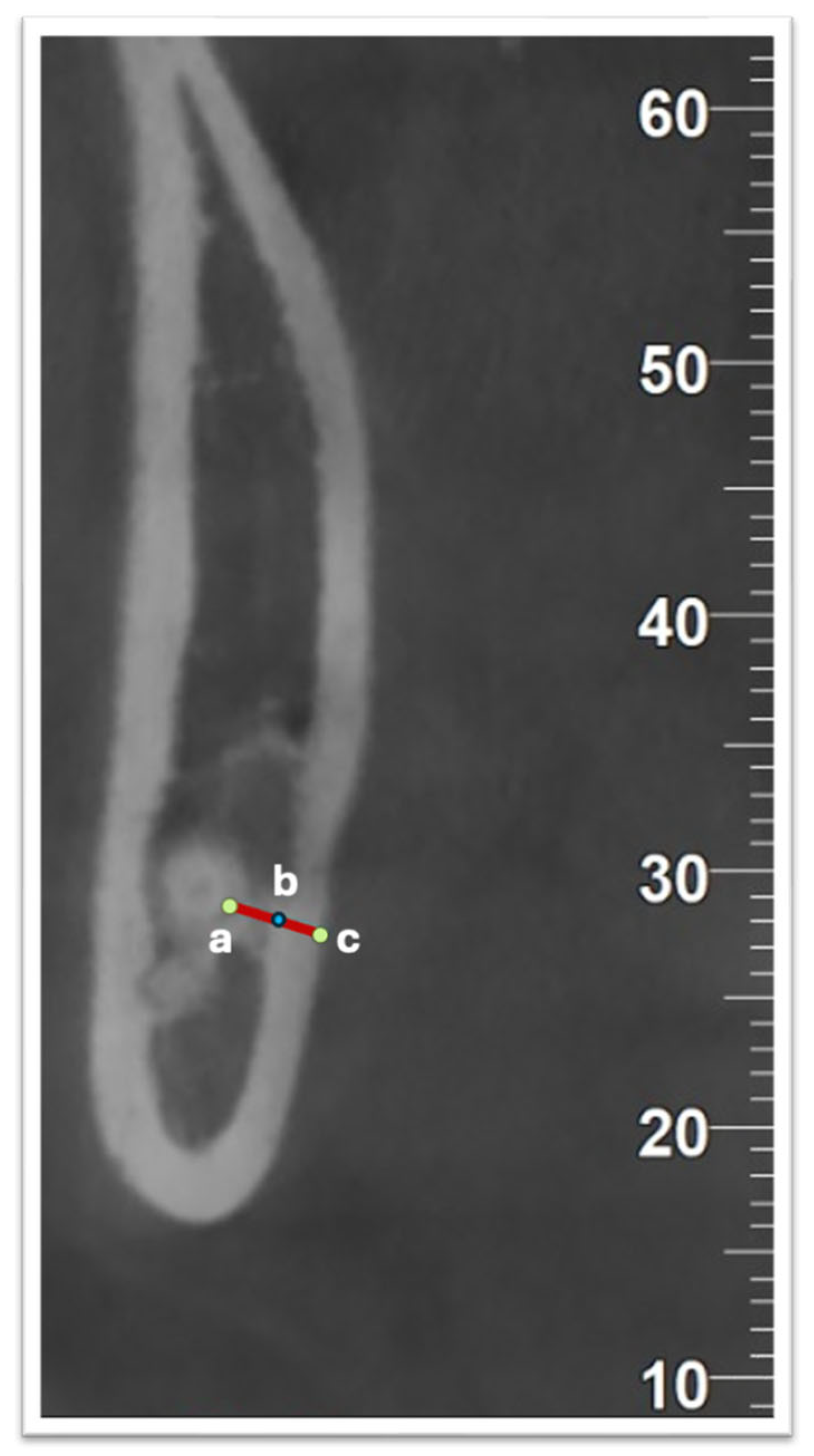
- Linear Measurements: Cortical lingual bone thickness (at the apex level) and distance from the root apex to the outer surface of the lingual plate were measured as morphometric parameters.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CBCT | Cone Beam Computed Tomography |
| DICOM | Digital Imaging and Communication in Medicine |
| CEJ | Cementoenamel Junction |
References
- Van der Linden, W.; Cleaton-Jones, P.; Lownie, M. Diseases and lesions associated with third molars. Review of 1001 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1995, 79, 142–145. [Google Scholar] [CrossRef]
- Yaseen, T.A.; Younis, H.; Aghayants, S.; Yin, M.; Cheng, B. Impact of vertical facial type on alveolar bone thickness and tooth morphology: A retrospective CBCT-based clinical study. J. Stomatol. Oral Maxillofac. Surg. 2025, 126, 102128. [Google Scholar] [CrossRef] [PubMed]
- Kose, I.; Koparal, M.; Gunes, N.; Atalay, Y.; Yaman, F.; Atilgan, S.; Kaya, G. Displaced lower third molar tooth into the submandibular space: Two case reports. J. Nat. Sci. Biol. Med. 2014, 5, 482–484. [Google Scholar] [CrossRef]
- Zhao, S.; Huang, Z.; Geng, T.; Huang, L. Intraoral management of iatrogenically displaced lower third molar roots in the sublingual space: A report of 2 cases. Int. J. Clin. Exp. Med. 2015, 8, 19591–19595. [Google Scholar]
- Bataineh, A.B. Sensory nerve impairment following mandibular third molar surgery. J. Oral Maxillofac. Surg. 2001, 59, 1012–1017. [Google Scholar] [CrossRef]
- Aznar-Arasa, L.; Figueiredo, R.; Gay-Escoda, C. Iatrogenic displacement of lower third molar roots into the sublingual space: Report of 6 cases. J. Oral Maxillofac. Surg. 2012, 70, 107–115. [Google Scholar] [CrossRef]
- Huang, C.; Zhou, C.; Xu, M.; Zou, D. Risk factors for lingual plate fracture during mandibular third molar extraction. Clin. Oral Investig. 2020, 24, 4133–4142. [Google Scholar] [CrossRef]
- Wang, D.; He, X.; Wang, Y.; Zhou, G.; Sun, C.; Yang, L.; Bai, J.; Gao, J.; Wu, Y.; Cheng, J. Topographic relationship between root apex of mesially and horizontally impacted mandibular third molar and lingual plate: Cross-sectional analysis using CBCT. Sci. Rep. 2016, 6, 39268. [Google Scholar] [CrossRef]
- Del Lhano, N.C.; Ribeiro, R.A.; Martins, C.d.C.; Assis, N.M.S.P.; Devito, K.L. Panoramic versus CBCT used to reduce inferior alveolar nerve paresthesia after third molar extractions: A systematic review and meta-analysis. Dentomaxillofac. Radiol. 2020, 49, 20190265. [Google Scholar] [CrossRef] [PubMed]
- de Baranda, B.S.; Silvestre, F.J.; Márquez-Arrico, C.F.; Silvestre-Rangil, J. Surgical difficulty and postoperative course of the third molar extraction under general anesthesia: An intervention trial. J. Stomatol. Oral Maxillofac. Surg. 2024, 125, 101663. [Google Scholar] [CrossRef]
- Huang, I.-Y.; Wu, C.-W.; Worthington, P. The Displaced lower third molar: A literature review and suggestions for management. J. Oral Maxillofac. Surg. 2007, 65, 1186–1190. [Google Scholar] [CrossRef]
- Guerrero, M.E.; Shahbazian, M.; Bekkering, G.E.; Nackaerts, O.; Jacobs, R.; Horner, K. The diagnostic efficacy of cone beam CT for impacted teeth and associated features: A systematic review. J. Oral Rehabil. 2011, 38, 208–216. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Meijer, G.J.; Soehardi, A.; Borstlap, W.A.; Mulder, J.; Bergé, S.J. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int. J. Oral Maxillofac. Surg. 2009, 38, 964–971. [Google Scholar] [CrossRef]
- Tantanapornkul, W.; Okochi, K.; Bhakdinaronk, A.; Ohbayashi, N.; Kurabayashi, T. Correlation of darkening of impacted mandibular third molar root on digital panoramic images with cone beam computed tomography findings. Dentomaxillofac. Radiol. 2009, 38, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Parhiz, S.A.; Bakhtiary, P.; Mosavat, F.; Kharazifard, M.J. Thickness of buccal and lingual alveolar bone plates according to the position of impacted mandibular third molars on cone-beam computed tomography scans. Front. Dent. 2019, 16, 279. [Google Scholar] [CrossRef] [PubMed]
- Menziletoglu, D.; Tassoker, M.; Kubilay-Isik, B.; Esen, A. The assesment of relationship between the angulation of impacted mandibular third molar teeth and the thickness of lingual bone: A prospective clinical study. Med. Oral Patol. Oral Cir. Bucal 2018, 24, e130. [Google Scholar] [CrossRef]
- Matsuda, S.; Yoshimura, H. Lingual bone thickness in the apical region of the horizontal mandibular third molar: A cross-sectional study in young Japanese. PLoS ONE 2022, 17, e0263094. [Google Scholar] [CrossRef]
- Momin, M.A.; Matsumoto, K.; Ejima, K.; Asaumi, R.; Kawai, T.; Arai, Y.; Honda, K.; Yosue, T. Correlation of mandibular impacted tooth and bone morphology determined by cone beam computed topography on a premise of third molar operation. Surg. Radiol. Anat. 2012, 35, 311–318. [Google Scholar] [CrossRef]
- Mallik, A.; Vidya, K.C.; Waran, A.; Rout, S.K. Measurement of lingual cortical plate thickness and lingual position of lower third molar roots using cone beam computed tomography. J. Int. Soc. Prev. Community Dent. 2017, 7, 8–12. [Google Scholar] [CrossRef]
- Emes, Y.; Öncu, B.; Aybar, B.; Al-Badri, N.; Işsever, H.; Atalay, B.; Yalçın, S. Measurement of the lingual position of the lower third molar roots using cone-beam computed tomography. J. Oral Maxillofac. Surg. 2015, 73, 13–17. [Google Scholar] [CrossRef]
- Tolstunov, L.; Brickeen, M.; Kamanin, V.; Susarla, S.M.; Selvi, F. Is Mandibular Third Molar’s Angulation Associated with the Lingual Bone Thickness? Br. J. Oral Maxillofac. Surg. 2016, 54, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Halder, M.; Chhaparwal, Y.; Patil, V.; Smriti, K.; Chhaparwal, S.; Pentapati, K.C. Quantitative and qualitative correlation of mandibular lingual bone with risk factors for third molar using cone beam computed tomography. Clin. Cosmet. Investig. Dent. 2023, 15, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Jamet, E.; Imai, T.; Kubota, S.; Nishimoto, A.; Katsura-Fuchihata, S.; Uzawa, N. Risk factors for impacted lower third molar root perforation through the undercut-shaped lingual plate: Preoperative insights from panoramic radiography. Odontology 2024, 112, 562–569. [Google Scholar] [CrossRef]
- Ge, J.; Zheng, J.-W.; Yang, C.; Qian, W.-T. Variations in the buccal-lingual alveolar bone thickness of impacted mandibular third molar: Our classification and treatment perspectives. Sci. Rep. 2016, 6, 16375. [Google Scholar] [CrossRef] [PubMed]
| n (%) | ||
|---|---|---|
| Side | Right | 65 (54.2%) 55 (45.8%) |
| Left | ||
| Gender | Male | 34 (47.9%) 27 (52.1%) |
| Female | ||
| Pell & Gregory’s Classification/ Ramus Relationship | A | 45 (37.5%) 52 (43.3%) 23 (19.2%) |
| B | ||
| C | ||
| Pell & Gregory’s Classification/ Impaction Depth | I | 46 (38.3%) 38 (31.7%) 36 (30.0%) |
| II | ||
| III | ||
| Winter’s Classification/Angulation | Mesioangular | 33 (27.5%) 67 (55.8%) 19 (15.8%) 1 (0.8%) |
| Vertical | ||
| Horizontal | ||
| Buccolingual | ||
| Lingual Bone Morphology | Undercut | 35 (29.2%) 34 (28.3%) 36 (30.0%) 15 (12.5%) |
| Parallel | ||
| Slanted | ||
| Round | ||
| Apex Position | Contact | 43 (35.8%) 41 (34.2%) 36 (30.0%) |
| Non-contact | ||
| Perforating | ||
| Perforation at CEJ | Yes | 11 (9.2%) 109 (90.8%) |
| No | ||
| Perforation at Mid-root | Yes | 30 (25.0%) 90 (75.0%) |
| No | ||
| Perforation at Apex | Yes | 35 (29.2%) 85 (70.8%) |
| No |
| Available Space (Concerning Ascending Mandibular Ramus) | |||||
|---|---|---|---|---|---|
| Class I (n = 45) | Class II (n = 52) | Class III (n = 23) | |||
| n (%) | n (%) | n (%) | p | ||
| Lingual Bone Morphology | Undercut | 19 (42.2%) | 11 (21.2%) | 5 (21.7%) | 0.020 * |
| Parallel | 5 (11.1%) | 18 (34.6%) | 11 (47.8%) | ||
| Slanted | 14 (31.1%) | 18 (34.6%) | 4 (17.4%) | ||
| Round | 7 (15.6%) | 5 (9.6%) | 3 (13%) | ||
| Apex Position | Contact | 22 (48.9%) | 13 (25%) | 8 (34.8%) | 0.055 |
| Non-contact | 14 (31.1%) | 17 (32.7%) | 10 (43.5%) | ||
| Perforating | 9 (20%) | 22 (42.3%) | 5 (21.7%) | ||
| Perforation at CEJ | Yes | 2 (4.4%) | 4 (%7.7) | 5 (%21.7) | 0.058 |
| No | 43 (95.6%) | 48 (%92.3) | 18 (%78.3) | ||
| Perforation at Mid-root | Yes | 8 (17.8%) | 17 (32.7%) | 5 (21.7%) | 0.221 |
| No | 37 (82.2%) | 35 (67.3%) | 18 (78.3%) | ||
| Perforation at Apex | Yes | 7 (15.6%) | 22 (42.3%) | 6 (26.1%) | 0.014 * |
| No | 38 (84.4%) | 30 (57.7%) | 17 (73.9%) | ||
| Depth (Concerning the Occlusal Plane) | |||||
|---|---|---|---|---|---|
| Level A (n = 46) | Level B (n = 38) | Level C (n = 36) | |||
| n (%) | n (%) | n (%) | p | ||
| Lingual Bone Morphology | Undercut | 18 (39.1%) | 10 (%26.3) | 7 (%19.4) | 0.008 * |
| Parallel | 4 (8.7%) | 13 (%34.2) | 17 (%47.2) | ||
| Slanted | 17 (37%) | 9 (%23.7) | 10 (%27.8) | ||
| Round | 7 (15.2%) | 6 (%15.8) | 2 (%5.6) | ||
| Apex Position | Contact | 23 (50%) | 12 (%31.6) | 8 (%22.2) | 0.110 |
| Non-contact | 12 (26.1%) | 13 (%34.2) | 16 (%44.4) | ||
| Perforating | 11 (23.9%) | 13 (%34.2) | 12 (%33.3) | ||
| Perforation at CEJ | Yes | 0 (0%) | 1 (2.6%) | 10 (27.8%) | 0.001 * |
| No | 46 (100%) | 37 (97.4%) | 26 (72.2%) | ||
| Perforation at Mid-root | Yes | 11 (23.9%) | 10 (26.3%) | 9 (25%) | 0.968 |
| No | 35 (76.1%) | 28 (73.7%) | 27 (75%) | ||
| Perforation at Apex | Yes | 11 (23.9%) | 13 (34.2%) | 11 (30.6%) | 0.572 |
| No | 35 (76.1%) | 25 (65.8%) | 25 (69.4%) | ||
| Angulation | |||||
|---|---|---|---|---|---|
| Mesioangular (n = 33) | Vertical (n = 67) | Horizontal (n = 19) | |||
| n (%) | n (%) | n (%) | p | ||
| Lingual Bone Morphology | Undercut | 8 (24.2%) | 24 (%35.8) | 3 (%15.8) | 0.001 * |
| Parallel | 15 (45.5%) | 7 (%10.4) | 11 (%57.9) | ||
| Slanted | 9 (27.3%) | 24 (%35.8) | 3 (%15.8) | ||
| Round | 1 (3%) | 12 (%17.9) | 2 (%10.5) | ||
| Apex Position | Contact | 7 (21.2%) | 31 (46.3%) | 5 (26.3%) | 0.127 |
| Non-contact | 13 (39.4%) | 19 (28.4%) | 8 (42.1%) | ||
| Perforating | 13 (39.4%) | 17 (25.4%) | 6 (31.6%) | ||
| Perforation at CEJ | Yes | 2 (6.1%) | 1 (1.5%) | 7 (36.8%) | 0.001 * |
| No | 31 (93.9%) | 66 (98.5%) | 12 (63.2%) | ||
| Perforation at Mid-root | Yes | 13 (39.4%) | 14 (20.9%) | 3 (15.8%) | 0.079 |
| No | 20 (60.6%) | 53 (79.1%) | 16 (84.2%) | ||
| Perforation at Apex | Yes | 14 (42.4%) | 17 (25.4%) | 4 (21.1%) | 0.145 |
| No | 19 (57.6%) | 50 (74.6%) | 15 (78.9%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yüceer-Çetiner, E.; Sakarya, Ö.; Vural, A.; Kazan, D. Does the Position of the Mandibular Third Molar Have an Effect on the Lingual Bone Morphology? A Cone Beam Computed Tomography Evaluation. Diagnostics 2025, 15, 2401. https://doi.org/10.3390/diagnostics15182401
Yüceer-Çetiner E, Sakarya Ö, Vural A, Kazan D. Does the Position of the Mandibular Third Molar Have an Effect on the Lingual Bone Morphology? A Cone Beam Computed Tomography Evaluation. Diagnostics. 2025; 15(18):2401. https://doi.org/10.3390/diagnostics15182401
Chicago/Turabian StyleYüceer-Çetiner, Ezgi, Özgür Sakarya, Attila Vural, and Dilara Kazan. 2025. "Does the Position of the Mandibular Third Molar Have an Effect on the Lingual Bone Morphology? A Cone Beam Computed Tomography Evaluation" Diagnostics 15, no. 18: 2401. https://doi.org/10.3390/diagnostics15182401
APA StyleYüceer-Çetiner, E., Sakarya, Ö., Vural, A., & Kazan, D. (2025). Does the Position of the Mandibular Third Molar Have an Effect on the Lingual Bone Morphology? A Cone Beam Computed Tomography Evaluation. Diagnostics, 15(18), 2401. https://doi.org/10.3390/diagnostics15182401






