Comparison of Bilateral Versus Unilateral Transversus Abdominis Plane Block Combined with Spinal Anesthesia in Laparoscopic Appendectomy: A Retrospective Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Patient Selection
2.3. Anesthesia Protocol
2.4. Group Allocation and TAPB Technique
2.5. Postoperative Management and Outcome Measures
2.6. Statistical Analysis
3. Results
3.1. Perioperative Outcomes
3.2. Postoperative Analgesia
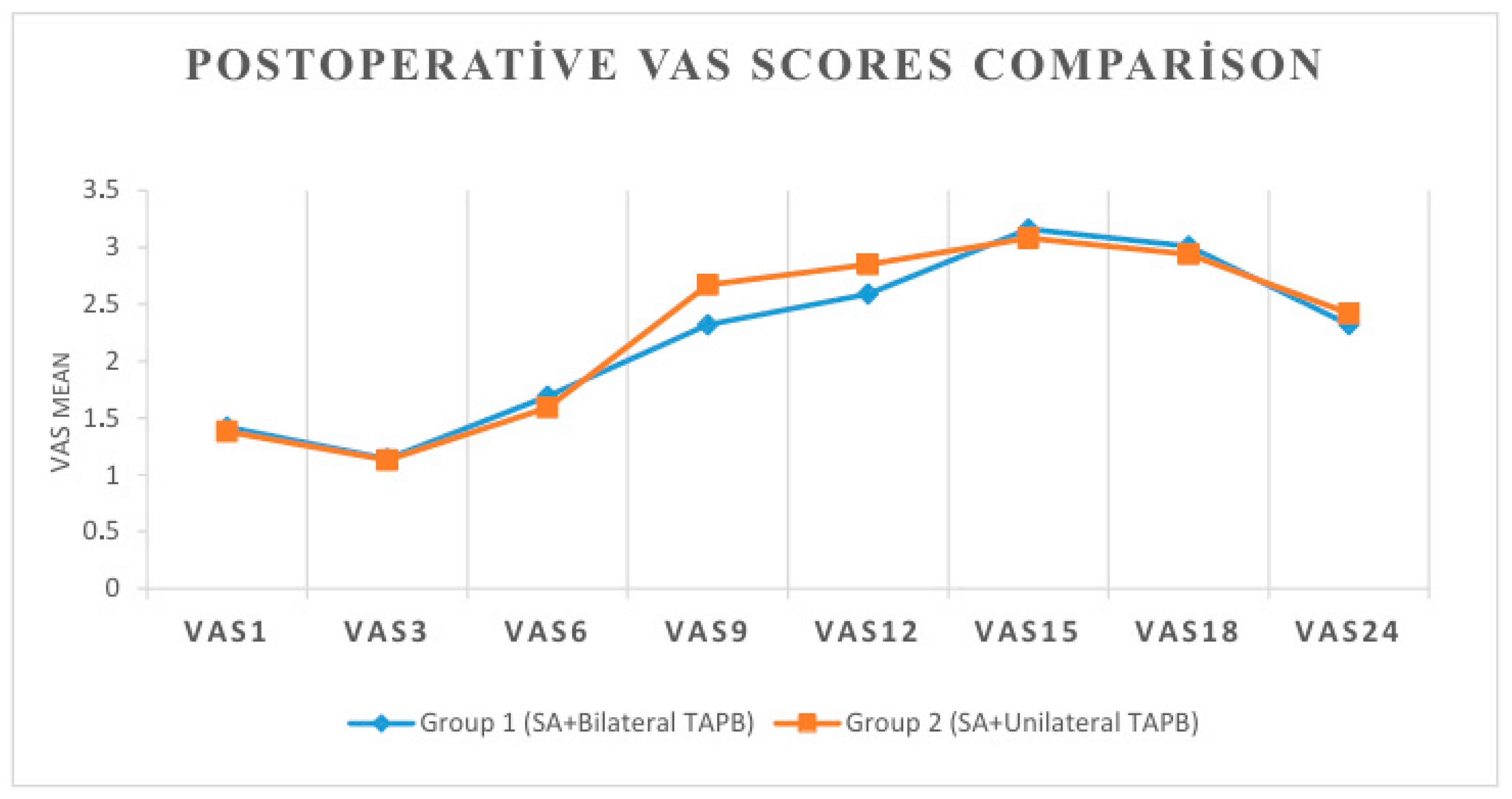
3.3. Pain Scores (VAS)
3.4. Patient Satisfaction
3.5. Shoulder Pain Subgroup Analysis
4. Discussion
Limitations
5. Conclusions
5.1. What Is Known
5.2. What Is New
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, X.; Zhang, J.; Sang, L.; Zhang, W.; Chu, Z.; Li, X.; Liu, Y. Laparoscopic versus conventional appendectomy—A meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010, 10, 129. [Google Scholar] [CrossRef]
- Ozgün, H.; Kurt, M.N.; Kurt, I.; Cevikel, M.H. Comparison of local, spinal, and general anesthesia for inguinal herniorrhaphy. Eur. J. Surg. 2002, 168, 455–459. [Google Scholar]
- Sinha, R.; Gurwara, A.K.; Gupta, S.C. Laparoscopic total extraperitoneal inguinal hernia repair under spinal anesthesia: A study of 480 patients. J. Laparoendosc. Adv. Surg. Tech. A 2008, 18, 673–677. [Google Scholar] [CrossRef] [PubMed]
- Bajwa, S.J.S.; Kulshrestha, A. Anaesthesia for laparoscopic surgery: General vs regional anesthesia. J. Minimal Access Surg. 2016, 12, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Lal, P.; Philips, P.; Saxena, K.N.; Kajla, R.K.; Chander, J.; Ramteke, V.K. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair under epidural anesthesia: A detailed evaluation. Surg. Endosc. 2007, 21, 595–601. [Google Scholar] [CrossRef]
- Hamad, M.A.; El-Khattary, O.A. Laparoscopic cholecystectomy under spinal anesthesia with nitrous oxide pneumoperitoneum: A feasibility study. Surg. Endosc. 2003, 17, 1426–1428. [Google Scholar] [CrossRef] [PubMed]
- van Zundert, A.A.J.; Stultiens, G.; Jakimowicz, J.J.; Peek, D.; van der Ham, W.G.J.M.; Korsten, H.H.M.; Wildsmith, J.A.W. Laparoscopic cholecystectomy under segmental thoracic spinal anesthesia: A feasibility study. Br. J. Anaesth. 2007, 98, 682–686. [Google Scholar] [CrossRef]
- Lee, J.H.; Huh, J.; Kim, D.K.; Gil, J.R.; Min, S.W.; Han, S.S. Laparoscopic cholecystectomy under epidural anesthesia: A clinical feasibility study. Korean J. Anesthesiol. 2010, 59, 383–388. [Google Scholar] [CrossRef]
- Ozciftci, S.; Sahiner, Y.; Sahiner, İ.T.; Akkaya, T. Is Right Unilateral Transversus Abdominis Plane (TAP) Block Successful in Postoperative Analgesia in Laparoscopic Cholecystectomy? Int. J. Clin. Pract. 2022, 6, 2668215. [Google Scholar] [CrossRef]
- Rahimzadeh, P.; Faiz, S.H.R.; Latifi-Naibin, K.; Alimian, M. A Comparison of the effect of preemptive versus postoperative use of ultrasound-guided bilateral transversus abdominis plane (TAP) block on pain relief after laparoscopic cholecystectomy. Sci. Rep. 2022, 12, 623. [Google Scholar] [CrossRef]
- Chung, C.-J.; Choi, S.-R.; Yeo, K.-H.; Park, H.-S.; Lee, S.-I.; Chin, Y.-J. Hyperbaric spinal anesthesia with 0.5% bupivacaine: A comparison of doses. Reg. Anesth. Pain Med. 2000, 25, 514–520. [Google Scholar]
- Collins, L.M.; Vaghadia, H. Regional anesthesia for laparoscopy. Anesthesiol. Clin. N. Am. 2001, 19, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Jun, G.W.; Kim, M.S.; Yang, H.J.; Sung, T.Y.; Park, D.H.; Cho, C.K.; Kwon, H.U.; Kang, P.S.; Moon, J.I. Laparoscopic appendectomy under spinal anesthesia with dexmedetomidine infusion. Korean J. Anesthesiol. 2014, 67, 246–251. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gurusamy, K.S.; Samraj, K.; Davidson, B.R. Low-pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst. Rev. 2009, CD006930. [Google Scholar] [CrossRef]
- Gerges, F.J.; Kanazi, G.E.; Jabbour-Khoury, S.I. Anesthesia for laparoscopy: A review. J. Clin. Anesth. 2006, 18, 67–78. [Google Scholar] [CrossRef]
- Spivak, H.; Nudelman, I.; Fuco, V.; Rubin, M.; Raz, P.; Peri, A.; Lelcuk, S.; Eidelman, L.A. Laparoscopic extraperitoneal inguinal hernia repair with spinal anesthesia and nitrous oxide insufflation. Surg. Endosc. 1999, 13, 1026–1029. [Google Scholar] [CrossRef]
- Sarli, L.; Costi, R.; San Sebastiano, G.; Trivelli, M.; Roncoroni, L. Prospective randomized trial of low-pressure pneumoperitoneum for reduction of shoulder-tip pain following laparoscopy. Br. J. Surg. 2000, 87, 1161–1165. [Google Scholar] [CrossRef]
- Tzovaras, G.; Fafoulakis, F.; Pratsas, K.; Georgopoulou, S.; Stamatiou, G.; Hatzitheofilou, C. Spinal vs. general anesthesia for laparoscopic cholecystectomy. Interim analysis of a controlled, randomized trial. Arch. Surg. 2008, 143, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Gurwara, A.K.; Gupta, S.C. Laparoscopic cholecystectomy under spinal anesthesia: A study of 3492 patients. J. Laparoendosc. Adv. Surg. Tech. A 2009, 19, 323–327. [Google Scholar] [CrossRef]
- Tiwari, S.; Chauhan, A.; Chatterjee, P.; Alam, M.T. Laparoscopic cholecystectomy under spinal anesthesia: A prospective, randomized study. J. Minimal Access Surg. 2013, 9, 65–71. [Google Scholar]
- Goyal, S.; Goyal, S.; Singla, S. Laparoscopic Cholecystectomy Under Spinal Anesthesia with Low-Pressure Pneumoperitoneum—Prospective Study of 150 Cases. Arch. Clin. Exp. Surg. 2012, 1, 224–228. [Google Scholar] [CrossRef]
- Mukhtar, K.; Singh, S. Transversus abdominis plane block for laparoscopic surgery. Br. J. Anaesth. 2009, 102, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Baeriswyl, M.; Zeiter, F.; Piubellini, D.; Kirkham, K.R.; Albrecht, E. The analgesic efficacy of transverse abdominis plane block versus epidural analgesia: A systematic review with meta-analysis. Medicine 2018, 97, e11261. [Google Scholar] [CrossRef] [PubMed]
- Turkstani, A.; Ibraheim, O.; Khairy, G.; Alseif, A.; Khalil, N. Spinal versus general anesthesia for laparoscopic cholecystectomy: A cost-effectiveness and side effects study. Anaesth. Pain Intensive Care 2009, 13, 9–14. [Google Scholar]
- Ellakany, M. Comparative study between general and thoracic spinal anesthesia for laparoscopic cholecystectomy. Egypt. J. Anaesth. 2013, 29, 375–381. [Google Scholar] [CrossRef]
- Mehta, P.J.; Chavda, H.R.; Wadhwana, A.P.; Porecha, M.M. Comparative analysis of spinal versus general anesthesia for laparoscopic cholecystectomy: A controlled, prospective, randomized trial. Anesth. Essays Res. 2010, 4, 91–95. [Google Scholar]
- Kalaivani, V.; Pujari, V.S.; Sreevathsa, M.R.; Hiremath, B.V.; Bevinaguddaiah, Y. Laparoscopic Cholecystectomy Under Spinal Anaesthesia vs. General Anaesthesia: A Prospective Randomised Study. J. Clin. Diagn. Res. 2014, 8, NC01–NC04. [Google Scholar] [CrossRef]
- Erdem, V.M.; Donmez, T.; Uzman, S.; Ferahman, S.; Hatipoglu, E.; Sunamak, O. Spinal/epidural block as an alternative to general anesthesia for laparoscopic appendectomy: A prospective randomized clinical study. Videosurg. Other Miniinvasive Tech. 2018, 13, 148–156. [Google Scholar] [CrossRef]
| Variable | Group 1 (SA + Bilateral TAPB) | Group 2 (SA + Unilateral TAPB) | p-Value | |
|---|---|---|---|---|
| Gender n (%) | Male | 67 (60.9) | 63 (57.3) | 0.583 * |
| Female | 43 (39.1) | 47 (42.7) | ||
| Age mean (95% CI) | 37.2 (34.3–40) | 33.8 (31.4–36.2) | 0.224 † | |
| Height means cm (95% CI) | 168.5 (166.8–170.3) | 169 (167.4–170.6) | 0.797 † | |
| Weight means kg (95% CI) | 79.9 (76.9–83) | 80 (76.9–83.2) | 0.467 † | |
| BMI mean (95% CI) | 28.3 (27.1–29.4) | 28.2 (27–29.4) | 0.367 † | |
| ASA n (%) | ASA I | 53 (48.2) | 59 (53.6) | 0.717 |
| ASA II | 42 (38.2) | 38 (34.5) | ||
| ASA III | 15 (13.6) | 13 (11.8) | ||
| Comorbidities n (%) | None | 77 (70.0) | 83 (75.5) | 0.364 |
| Present | 33 (30.0) | 27 (24.5) | ||
| Smoking n (%) | Non-smoker | 75 (68.2) | 78 (70.9) | 0.66 |
| Smoker | 35 (31.8) | 32 (29.1) |
| Variable | Group 1 (SA + Bilateral TAPB) | Group 2 (SA + Unilateral TAPB) | p-Value | |
|---|---|---|---|---|
| (a) | ||||
| Right Shoulder Pain n (%) | None | 46 (41.8) | 49 (44.5) | 0.683 * |
| Present | 64 (58.2) | 61 (55.5) | ||
| Hypotension n (%) | None | 98 (89.1) | 101 (91.8) | 0.491 * |
| Present | 12 (10.9) | 9 (8.2) | ||
| Nausea/Vomiting n (%) | None | 107 (97.3) | 108 (98.2) | 1.000 * |
| Present | 3 (2.7) | 2 (1.8) | ||
| Deep sedation during surgery n (%) | Not Required | 84 (76.4) | 82 (74.5) | 0.754 * |
| Required | 26 (23.6) | 28 (25.5) | ||
| Operation Time (minute) | 34.3 ± 8.7 | 32.9 ± 8.5 | 0.229 † | |
| Satisfaction mean (95% CI min-maks) | 1.92 (1.86–1.97) | 1.85 (1.78–1.92) | 0.084 † | |
| Postoperative Analgesia Needed n (%) | None | 15 (13.6) | 4 (3.6) | 0.008 * |
| Present | 95 (86.4) | 106 (96.4) | ||
| Time to First Analgesic (hours) mean (95% CI min-maks) | 13.7 (12.9–14.6) | 12.1 (11.4–12.8) | 0.001 † | |
| Analgesic Doses in First 24 h mean (95% CI min-maks) | 1.24 (1.14–1.34) | 1.32 (1.22–1.42) | 0.010 † | |
| (b) | ||||
| Satisfaction Level n (%) | Slightly Satisfied | 1 (0.9) | 0 (0.0) | 0.07 |
| Neutral | 7 (6.4) | 15 (13.6) | ||
| Satisfied | 41(37.3) | 48 (43.6) | ||
| Very Satisfied/Excellent | 61 (55.5) | 47 (42.7) | ||
| Time | Group 1 (SA + Bilateral TAPB) | Group 2 (SA + Unilateral TAPB) | p-Value * |
|---|---|---|---|
| VAS1 mean (95% CI min-maks) | 1.42 (1.26–1.58) | 1.38 (1.24–1.52) | 0.902 |
| VAS3 mean (95% CI min-maks) | 1.14 (1.06–1.21) | 1.13 (1.06–1.21) | 0.981 |
| VAS6 mean (95% CI min-maks) | 1.69 (1.48–1.91) | 1.59 (1.40–1.78) | 0.941 |
| VAS9 mean (95% CI min-maks) | 2.32 (2.06–2.57) | 2.67 (2.42–2.92) | 0.003 |
| VAS12 mean (95% CI min-maks) | 2.59 (2.34–2.84) | 2.85 (2.58–3.12) | 0.039 |
| VAS15 mean (95% CI min-maks) | 3.16 (2.90–3.41) | 3.08 (2.84–3.31) | 0.481 |
| VAS18 mean (95% CI min-maks) | 3.01 (2.76–3.27) | 2.94 (2.70–3.18) | 0.905 |
| VAS24 mean (95% CI min-maks) | 2.32 (2.17–2.46) | 2.42 (2.29–2.56) | 0.172 |
| Variable | Right Shoulder Pain | p-Value | ||
|---|---|---|---|---|
| None | Present | |||
| Intraoperative Deep Sedation n (%) | Not Required | 95 (100) | 71 (56.8) | <0.001 * |
| Required | 0 (0.0) | 54 (43.2) | ||
| VAS1 mean (95% CI min-max) | 1 (1–1) | 1.70 (1.53–1.86) | <0.001 † | |
| VAS3 mean (95% CI min-max) | 1 (1–1) | 1.23 (1.15–1.32) | <0.001 † | |
| VAS6 mean (95% CI min-max) | 1.40 (1.25–1.54) | 1.83 (1.61–2.05) | 0.048 † | |
| VAS9 mean (95% CI min-max) | 2.36 (2.12–2.60) | 2.61 (2.36–2.86) | 0.233 † | |
| VAS12 mean (95% CI min-max) | 2.69 (2.39–2.98) | 2.76 (2.52–2.99) | 0.489 † | |
| VAS15 mean (95% CI min-max) | 3.01 (2.75–3.28) | 3.19 (2.96–3.42) | 0.270 † | |
| VAS18 mean (95% CI min-max) | 2.98 (2.69–3.26) | 2.97 (2.76–3.19) | 0.719 † | |
| VAS24 mean (95% CI min-max) | 2.41 (2.27–2.54) | 2.35 (2.21–2.49) | 0.393 † | |
| Satisfaction mean (95% CI min-max) | 1.92 (1.86–1.98) | 1.85 (1.79–1.92) | 0.143 † | |
| Postoperative Analgesia n (%) | 86 (90.5) | 115 (92.0) | 0.700 * | |
| Time to First Analgesic (95% CI min-max) | 13.23 (12.5–13.97) | 12.61 (11.82–13.4) | 0.366 † | |
| Analgesic Doses in First 24 Hours (95% CI min-max) | 1.27 (1.17–1.37) | 1.30 (1.2–1.39) | 0.655 † | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Şengel, A.; Büyükfırat, E.; Seçilmiş, S.; Altay, N.; Atlas, A.; Karahan, M.A. Comparison of Bilateral Versus Unilateral Transversus Abdominis Plane Block Combined with Spinal Anesthesia in Laparoscopic Appendectomy: A Retrospective Observational Study. Diagnostics 2025, 15, 2122. https://doi.org/10.3390/diagnostics15172122
Şengel A, Büyükfırat E, Seçilmiş S, Altay N, Atlas A, Karahan MA. Comparison of Bilateral Versus Unilateral Transversus Abdominis Plane Block Combined with Spinal Anesthesia in Laparoscopic Appendectomy: A Retrospective Observational Study. Diagnostics. 2025; 15(17):2122. https://doi.org/10.3390/diagnostics15172122
Chicago/Turabian StyleŞengel, Abdulhakim, Evren Büyükfırat, Selçuk Seçilmiş, Nuray Altay, Ahmet Atlas, and Mahmut Alp Karahan. 2025. "Comparison of Bilateral Versus Unilateral Transversus Abdominis Plane Block Combined with Spinal Anesthesia in Laparoscopic Appendectomy: A Retrospective Observational Study" Diagnostics 15, no. 17: 2122. https://doi.org/10.3390/diagnostics15172122
APA StyleŞengel, A., Büyükfırat, E., Seçilmiş, S., Altay, N., Atlas, A., & Karahan, M. A. (2025). Comparison of Bilateral Versus Unilateral Transversus Abdominis Plane Block Combined with Spinal Anesthesia in Laparoscopic Appendectomy: A Retrospective Observational Study. Diagnostics, 15(17), 2122. https://doi.org/10.3390/diagnostics15172122







