Targeted Screening Strategies for Head and Neck Cancer: A Global Review of Evidence, Technologies, and Cost-Effectiveness †
Abstract
1. Introduction
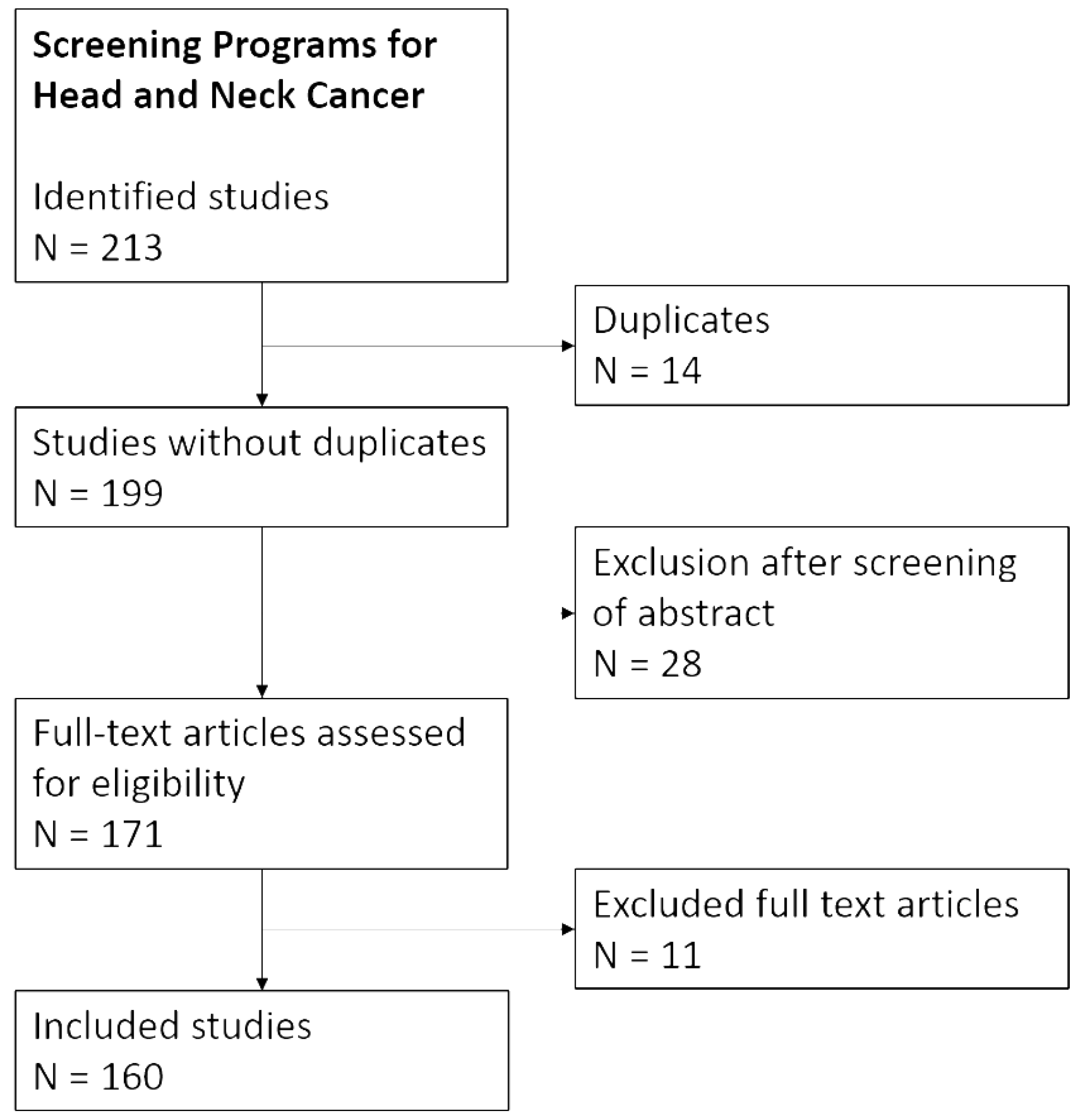
2. Search Strategy
3. Populations and Patients at High Risk of Developing HNC
| Population at Risk | Comment |
|---|---|
| Smoking | Risk is approximately 10 times higher than that of never-smokers, and 70–80% of new HNC diagnoses are associated with tobacco and alcohol use [26]. |
| Alcohol | Drinking > 3 alcoholic beverages per day was associated with a 1.5–1.7 fold increased risk in men and women [27]. Alcohol and tobacco have a synergistic effect, with the heavy consumption of both increasing HNC risk 40-fold [28]. |
| Human papillomavirus (HPV) infection | Important for oropharyngeal cancer (OPC). The global incidence of HPV positive OPC is increasing, with figures estimating that 25% of OPC cases worldwide are attributable to HPV infection, in contrast to North America, which has a higher prevalence of approximately 65% [29]. |
| Epstein-Barr virus (EBV) infection | Important for nasopharyngeal cancer (NPC). Over 90% of NPC cases, particularly those with undifferentiated types, are EBV-positive [30]. |
| Fanconi anemia | Risk is approximately 500–800 times higher than in the normal population [31]. |
| Immunodeficiency (due to solid organ transplantation or human immunodeficiency virus [HIV]) | Incidence rates are 1.5 to 4 times higher in HIV patients than in the general population [32]; it is about 1.4–1.9 times higher in solid organ transplanted patients [33]. |
| Oral potentially malignant disorder (OPMD) | Overall risk for malignant transformation in OPMDs can range from 1% to 34% [34]. |
| Former HNC | Risk of developing a second primary cancer falls within the range of 2–4% per year [23]. |
| Esophageal cancer | 5-year cumulative risk of developing second primary HNC ranges from 2.5% to 8.7% [35]. |
| Lung cancer | No numbers published! Vice versa, the risk of developing second primary lung cancer after HNC is about 6% within five years [36]. |
| Occupational exposure | Not part of this review. |
| Prior irradiation in the head and neck region | Not part of this review. |
4. Screening for Synchronous or Metachronous Second HNC
5. Screening for the Primary Tumor Site in Patients with HNC of Unknown Primary
6. Screening for Second Primary Cancer at Other Sites of the Aerodigestive Tract in Patients with Index HNC
7. Screening for Second HNC in Patients with Other Index Aerodigestive Tract Cancer
8. Screening for Early Detection of Recurrent HNC
9. Evaluated Primary HNC Screening Programs
10. Efficacy and Cost-Effectiveness Modeling of HNC Screening
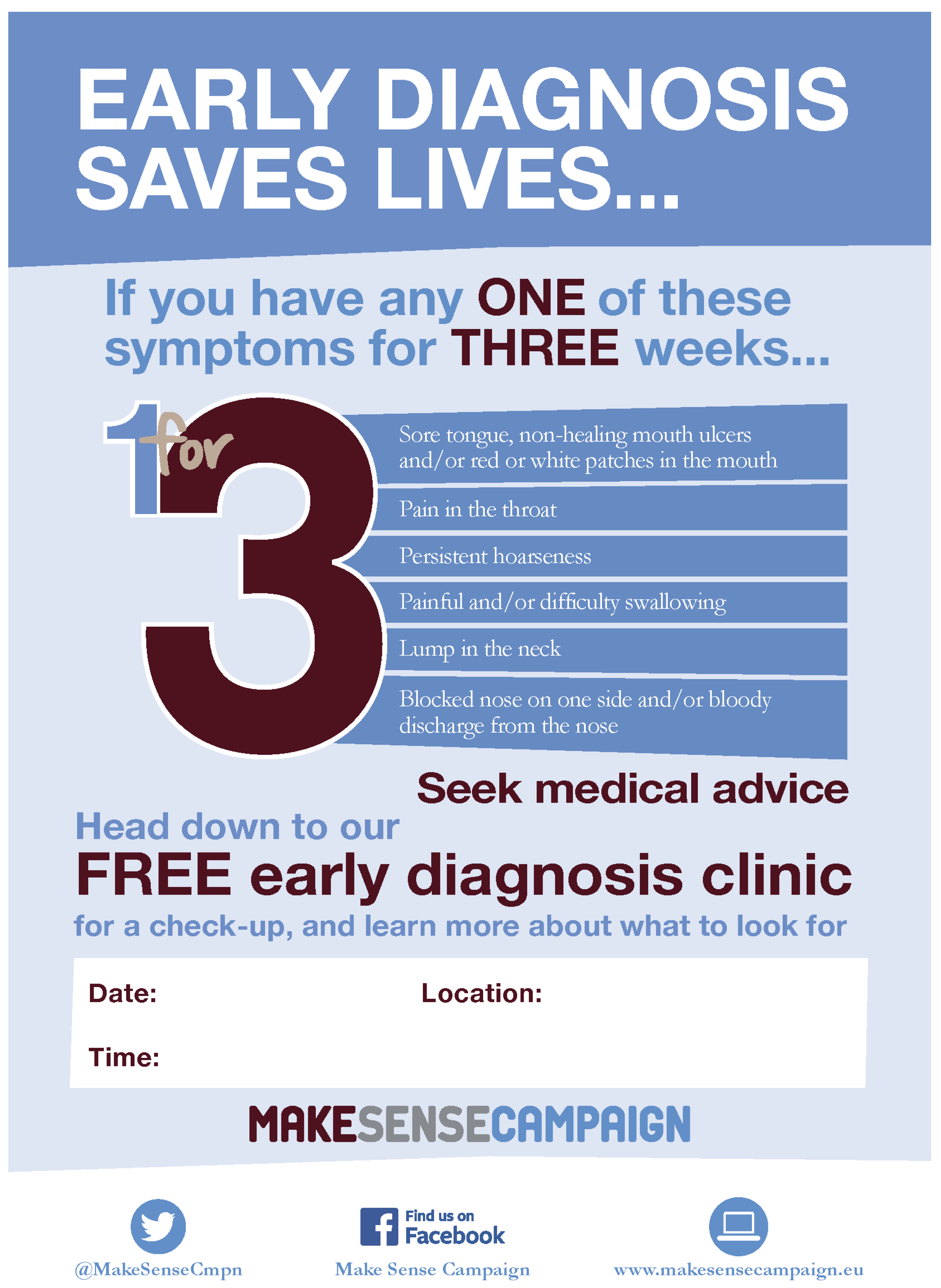
11. Awareness Campaigns
12. Liquid Biopsy Strategies
13. Innovative Imaging Technologies
14. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Gormley, M.; Creaney, G.; Schache, A.; Ingarfield, K.; Conway, D.I. Reviewing the epidemiology of head and neck cancer: Definitions, trends and risk factors. Br. Dent. J. 2022, 233, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.J.; Penfold, C.M.; Waylen, A.; Ness, A.R. The changing aetiology of head and neck squamous cell cancer: A tale of three cancers? Clin. Otolaryngol. 2018, 43, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Rumgay, H.; Nethan, S.T.; Shah, R.; Vignat, J.; Ayo-Yusuf, O.; Chaturvedi, P.; Guerra, E.N.S.; Gupta, P.C.; Gupta, R.; Liu, S.; et al. Global burden of oral cancer in 2022 attributable to smokeless tobacco and areca nut consumption: A population attributable fraction analysis. Lancet Oncol. 2024, 25, 1413–1423. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.E.; Burtness, B.; Leemans, C.R.; Lui, V.W.Y.; Bauman, J.E.; Grandis, J.R. Head and neck squamous cell carcinoma. Nat. Rev. Dis. Primers 2020, 6, 92. [Google Scholar] [CrossRef]
- Nieminen, M.; Aro, K.; Mäkitie, A.; Harlin, V.; Kainulainen, S.; Jouhi, L.; Atula, T. Challenges in diagnosing head and neck cancer in primary health care. Ann. Med. 2021, 53, 26–33. [Google Scholar] [CrossRef]
- Glen, P.; Botha, E. Early detection and prevention of head and neck cancers. Br. Dent. J. 2022, 233, 726–730. [Google Scholar] [CrossRef]
- Dittberner, A.; Friedl, B.; Wittig, A.; Buentzel, J.; Kaftan, H.; Boeger, D.; Mueller, A.H.; Schultze-Mosgau, S.; Schlattmann, P.; Ernst, T.; et al. Gender Disparities in Epidemiology, Treatment, and Outcome for Head and Neck Cancer in Germany: A Population-Based Long-Term Analysis from 1996 to 2016 of the Thuringian Cancer Registry. Cancers 2020, 12, 3418. [Google Scholar] [CrossRef]
- EHNS. EHNS: Make Sense of Head and Neck Cancer. 2025. Available online: https://makesensecampaign.eu/files/documents/Make-Sense-of-Head-and-Neck-Cancer-1for3-Leaflet.pdf (accessed on 2 May 2025).
- Hertrampf, K.; Wenz, H.J.; Koller, M.; Wiltfang, J. Comparing dentists’ and the public’s awareness about oral cancer in a community-based study in Northern Germany. J. Cranio Maxillo Facial Surg. 2012, 40, 28–32. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Döbrossy, L. Epidemiology of head and neck cancer: Magnitude of the problem. Cancer Metastasis Rev. 2005, 24, 9–17. [Google Scholar] [CrossRef]
- Chen, Y.P.; Chan, A.T.C.; Le, Q.T.; Blanchard, P.; Sun, Y.; Ma, J. Nasopharyngeal carcinoma. Lancet 2019, 394, 64–80. [Google Scholar] [CrossRef]
- Roman, B.R.; Aragones, A. Epidemiology and incidence of HPV-related cancers of the head and neck. J. Surg. Oncol. 2021, 124, 920–922. [Google Scholar] [CrossRef] [PubMed]
- Dedhia, R.C.; Grandis, J.R.; Fontes, P.A.; Johnson, J.T.; Weissfeld, J. Screening for head and neck cancer in liver transplant candidates: A review of 11 years of experience at the University of Pittsburgh. Laryngoscope 2012, 122, 539–542. [Google Scholar] [CrossRef] [PubMed]
- D’souza, G.; Carey, T.E.; William, W.N.; Nguyen, M.L., Jr.; Ko, E.C.; Riddell, J.; Pai, S.I.; Gupta, V.; Walline, H.M.; Lee, J.J.; et al. Epidemiology of head and neck squamous cell cancer among HIV-infected patients. J. Acquir. Immune Defic. Syndr. 2014, 65, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Rabinovics, N.; Mizrachi, A.; Hadar, T.; Ad-El, D.; Feinmesser, R.; Guttman, D.; Shpitzer, T.; Bachar, G. Cancer of the head and neck region in solid organ transplant recipients. Head Neck 2014, 36, 181–186. [Google Scholar] [CrossRef]
- Rampinelli, V.; Gennarini, F.; Borsetto, D.; Piazza, C. Head and neck squamous cell carcinoma in HIV patients. Curr. Opin. Otolaryngol. Head Neck Surg. 2023, 31, 78–82. [Google Scholar] [CrossRef]
- Lacko, M.; Braakhuis, B.J.; Sturgis, E.M.; Boedeker, C.C.; Suárez, C.; Rinaldo, A.; Ferlito, A.; Takes, R.P. Genetic susceptibility to head and neck squamous cell carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 38–48. [Google Scholar] [CrossRef]
- Beddok, A.; Velleuer, E.; Sicre de Fontbrune, F.; Brakenhoff, R.H.; Dalle, J.H.; Dufour, C.; Faivre, S.; Genet, C.; Klijanienko, J.; Krieg, C.; et al. Strategies for early detection and detailed characterization of oral lesions and head and neck squamous cell carcinoma in Fanconi anemia patients. Cancer Lett. 2025, 617, 217529. [Google Scholar] [CrossRef]
- Warnakulasuriya, S.; Johnson, N.W.; van der Waal, I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J. Oral Pathol. Med. 2007, 36, 575–580. [Google Scholar] [CrossRef]
- Iocca, O.; Sollecito, T.P.; Alawi, F.; Weinstein, G.S.; Newman, J.G.; De Virgilio, A.; Di Maio, P.; Spriano, G.; Pardinas Lopez, S.; Shanti, R.M. Potentially malignant disorders of the oral cavity and oral dysplasia: A systematic review and meta-analysis of malignant transformation rate by subtype. Head Neck 2020, 42, 539–555. [Google Scholar] [CrossRef]
- Ng, S.P.; Pollard, C.; Kamal, M.; Ayoub, Z.; Garden, A.S.; Bahig, H.; Gunn, G.B.; Frank, S.J.; Skinner, H.D.; Phan, J.; et al. Risk of second primary malignancies in head and neck cancer patients treated with definitive radiotherapy. Npj Precis. Oncol. 2019, 3, 22. [Google Scholar] [CrossRef] [PubMed]
- Coca-Pelaz, A.; Rodrigo, J.P.; Suárez, C.; Nixon, I.J.; Mäkitie, A.; Sanabria, A.; Quer, M.; Strojan, P.; Bradford, C.R.; Kowalski, L.P.; et al. The risk of second primary tumors in head and neck cancer: A systematic review. Head Neck 2020, 42, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Dai, X.; Gakidou, E.; Lopez, A.D. Evolution of the global smoking epidemic over the past half century: Strengthening the evidence base for policy action. Tob. Control 2022, 31, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Jethwa, A.R.; Khariwala, S.S. Tobacco-related carcinogenesis in head and neck cancer. Cancer Metastasis Rev. 2017, 36, 411–423. [Google Scholar] [CrossRef]
- Freedman, N.D.; Schatzkin, A.; Leitzmann, M.F.; Hollenbeck, A.R.; Abnet, C.C. Alcohol and head and neck cancer risk in a prospective study. Br. J. Cancer 2007, 96, 1469–1474. [Google Scholar] [CrossRef]
- Barsouk, A.; Aluru, J.S.; Rawla, P.; Saginala, K.; Barsouk, A. Epidemiology, Risk Factors, and Prevention of Head and Neck Squamous Cell Carcinoma. Med. Sci. 2023, 11, 42. [Google Scholar] [CrossRef]
- Brennan, S.; Baird, A.M.; O’Regan, E.; Sheils, O. The Role of Human Papilloma Virus in Dictating Outcomes in Head and Neck Squamous Cell Carcinoma. Front. Mol. Biosci. 2021, 8, 677900. [Google Scholar] [CrossRef]
- Su, Z.Y.; Siak, P.Y.; Lwin, Y.Y.; Cheah, S.C. Epidemiology of nasopharyngeal carcinoma: Current insights and future outlook. Cancer Metastasis Rev. 2024, 43, 919–939. [Google Scholar] [CrossRef]
- Lee, R.H.; Kang, H.; Yom, S.S.; Smogorzewska, A.; Johnson, D.E.; Grandis, J.R. Treatment of Fanconi Anemia-Associated Head and Neck Cancer: Opportunities to Improve Outcomes. Clin. Cancer Res. 2021, 27, 5168–5187. [Google Scholar] [CrossRef]
- Beachler, D.C.; D’Souza, G. Oral human papillomavirus infection and head and neck cancers in HIV-infected individuals. Curr. Opin. Oncol. 2013, 25, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Mowery, A.J.; Conlin, M.J.; Clayburgh, D.R. Elevated incidence of head and neck cancer in solid organ transplant recipients. Head Neck 2019, 41, 4009–4017. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Wang, Z.; Xu, M.; Li, B.; Huang, Z.; Qin, S.; Nice, E.C.; Tang, J.; Huang, C. Oral squamous cell carcinomas: State of the field and emerging directions. Int. J. Oral Sci. 2023, 15, 44. [Google Scholar] [CrossRef] [PubMed]
- Mitani, S.; Kadowaki, S.; Oze, I.; Masuishi, T.; Narita, Y.; Bando, H.; Oonishi, S.; Hirayama, Y.; Tanaka, T.; Tajika, M.; et al. Risk of second primary malignancies after definitive treatment for esophageal cancer: A competing risk analysis. Cancer Med. 2020, 9, 394–400. [Google Scholar] [CrossRef]
- Milano, M.T.; Peterson, C.R., 3rd; Zhang, H.; Singh, D.P.; Chen, Y. Second primary lung cancer after head and neck squamous cell cancer: Population-based study of risk factors. Head Neck 2012, 34, 1782–1788. [Google Scholar] [CrossRef]
- Slaughter, D.P.; Southwick, H.W.; Smejkal, W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer 1953, 6, 963–968. [Google Scholar] [CrossRef]
- Xu, C.C.; Biron, V.L.; Puttagunta, L.; Seikaly, H. HPV status and second primary tumours in oropharyngeal squamous cell carcinoma. J. Otolaryngol. Head Neck Surg. 2013, 42, 36. [Google Scholar] [CrossRef]
- Bonilla-Velez, J.; Mroz, E.A.; Hammon, R.J.; Rocco, J.W. Impact of human papillomavirus on oropharyngeal cancer biology and response to therapy: Implications for treatment. Otolaryngol. Clin. N. Am. 2013, 46, 521–543. [Google Scholar] [CrossRef]
- Bellavance, S.; Khoury, M.; Bissada, E.; Ayad, T.; Christopoulos, A.; Tabet, J.C.; Guertin, L.; Tabet, P. Panendoscopy for Head and Neck Cancers: Detection of Synchronous Second Primary Cancers, Complications and Cost-Benefit Analysis: A Systematic Review. J. Otolaryngol. Head Neck Surg. 2025, 54, 19160216251316215. [Google Scholar] [CrossRef]
- Thomas, R.; Kelemen, N.; Molena, E.; Lester, S. Indications for oropharyngeal biopsy in head and neck squamous cell carcinoma of unknown primary: A systematic review (HNSCCUP). Clin. Otolaryngol. 2024, 49, 552–566. [Google Scholar] [CrossRef]
- Charlton, A.; Mughal, Z.; Sharin, F.; Sahota, R.B.; Mansuri, M.S.; Mair, M. Prevalence of synchronous bilateral/contralateral tonsil carcinoma: A systematic review and meta-analysis. Oral Oncol. 2025, 162, 107180. [Google Scholar] [CrossRef]
- Diaz, E.M.; Tu, J.; Diaz, E.M., Jr.; Antonoff, M.B. Lung Cancer Screening in Head and Neck Cancer Patients: An Untapped Opportunity. Ann. Thorac. Surg. 2024, 117, 305–309. [Google Scholar] [CrossRef]
- Fnais, N.; Laxague, F.; Mascarella, M.A.; Chowdhury, R.; Zhao, H.; Jatana, S.; Aljassim, A.; Roy, C.F.; Alrasheed, A.S.; Chan, D.S.; et al. Lung Cancer Surveillance for Patients with Head and Neck Cancer. JAMA Otolaryngol. Head Neck Surg. 2025, 151, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Cramer, J.D.; Grauer, J.; Sukari, A.; Nagasaka, M. Incidence of Second Primary Lung Cancer After Low-Dose Computed Tomography vs Chest Radiography Screening in Survivors of Head and Neck Cancer: A Secondary Analysis of a Randomized Clinical Trial. JAMA Otolaryngol. Head Neck Surg. 2021, 147, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Jassal, J.S.; Grauer, J.S.; Cramer, J.D. Incidence of Head and Neck Cancer With Lung Cancer Screening: Secondary Analysis of a Randomized Controlled Trial. Laryngoscope 2022, 132, 1609–1614. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, L.; Deffebach, M.; Pappas, M.; Baumann, C.; Artis, K.; Mitchell, J.P.; Zakher, B.; Fu, R.; Slatore, C.U.S. Preventive Services Task Force Evidence Syntheses, Formerly Systematic Evidence Reviews. Screening for Lung Cancer: Systematic Review to Update the US Preventive Services Task Force Recommendation; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2013. [Google Scholar]
- Piersiala, K.; Akst, L.M.; Hillel, A.T.; Best, S.R. Clinical practice patterns in laryngeal cancer and introduction of CT lung screening. Am. J. Otolaryngol. 2019, 40, 520–524. [Google Scholar] [CrossRef]
- Chung, C.S.; Liao, L.J.; Wu, C.Y.; Lo, W.C.; Hsieh, C.H.; Lee, T.H.; Liu, C.Y.; Kuo, D.Y.; Shueng, P.W. Endoscopic Screening for Second Primary Tumors of the Esophagus Among Head and Neck Cancer Patients. Front. Oncol. 2022, 12, 906125. [Google Scholar] [CrossRef]
- Chiou, T.W.; Young, C.K.; Hsu, K.H.; Liao, C.T.; Hu, Y.F.; Kang, C.J.; Huang, S.F. The incidence of esophageal second primary cancer in head and neck cancer patients. Medicine 2025, 104, e42181. [Google Scholar] [CrossRef]
- Morris, L.G.; Sikora, A.G.; Patel, S.G.; Hayes, R.B.; Ganly, I. Second primary cancers after an index head and neck cancer: Subsite-specific trends in the era of human papillomavirus-associated oropharyngeal cancer. J. Clin. Oncol. 2011, 29, 739–746. [Google Scholar] [CrossRef]
- Morais, R.; Afonso, J.; Sousa, N.; Sousa-Pinto, B.; Libânio, D.; Marinho, B.; Sacramento, M.L.; Simplício, M.; Faria-Ramos, I.; Azevedo, L.; et al. Cost-utility and clinical impact of endoscopic screening for esophageal and gastric neoplasia in patients with head and neck neoplasms. Eur. J. Gastroenterol. Hepatol. 2025, 37, 815–825. [Google Scholar] [CrossRef]
- Lee, C.T.; Chang, C.Y.; Lee, Y.C.; Tai, C.M.; Wang, W.L.; Tseng, P.H.; Hwang, J.C.; Hwang, T.Z.; Wang, C.C.; Lin, J.T. Narrow-band imaging with magnifying endoscopy for the screening of esophageal cancer in patients with primary head and neck cancers. Endoscopy 2010, 42, 613–619. [Google Scholar] [CrossRef]
- Chuang, S.C.; Hashibe, M.; Scelo, G.; Brewster, D.H.; Pukkala, E.; Friis, S.; Tracey, E.; Weiderpass, E.; Hemminki, K.; Tamaro, S.; et al. Risk of second primary cancer among esophageal cancer patients: A pooled analysis of 13 cancer registries. Cancer Epidemiol. Biomark. Prev. 2008, 17, 1543–1549. [Google Scholar] [CrossRef]
- Onochi, K.; Shiga, H.; Takahashi, S.; Watanabe, N.; Fukuda, S.; Ishioka, M.; Koizumi, S.; Matsuhasi, T.; Jin, M.; Iijima, K. Risk Factors Linking Esophageal Squamous Cell Carcinoma With Head and Neck Cancer or Gastric Cancer. J. Clin. Gastroenterol. 2019, 53, e164–e170. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Ishihara, R.; Hamada, K.; Tonai, Y.; Yamasaki, Y.; Matsuura, N.; Kanesaka, T.; Yamamoto, S.; Akasaka, T.; Hanaoka, N.; et al. Endoscopic surveillance of head and neck cancer in patients with esophageal squamous cell carcinoma. Endosc. Int. Open 2016, 4, E752–E755. [Google Scholar] [CrossRef] [PubMed]
- van de Ven, S.; Bugter, O.; Hardillo, J.A.; Bruno, M.J.; Baatenburg de Jong, R.J.; Koch, A.D. Screening for head and neck second primary tumors in patients with esophageal squamous cell cancer: A systematic review and meta-analysis. United Eur. Gastroenterol. J. 2019, 7, 1304–1311. [Google Scholar] [CrossRef] [PubMed]
- Gili, R.; Caprioli, S.; Lovino Camerino, P.; Sacco, G.; Ruelle, T.; Filippini, D.M.; Pamparino, S.; Vecchio, S.; Marchi, F.; Del Mastro, L.; et al. Clinical Evidence of Methods and Timing of Proper Follow-Up for Head and Neck Cancers. Onco 2024, 4, 275–286. [Google Scholar] [CrossRef]
- Kostakoglu, L.; Fardanesh, R.; Posner, M.; Som, P.; Rao, S.; Park, E.; Doucette, J.; Stein, E.G.; Gupta, V.; Misiukiewicz, K.; et al. Early detection of recurrent disease by FDG-PET/CT leads to management changes in patients with squamous cell cancer of the head and neck. Oncologist 2013, 18, 1108–1117. [Google Scholar] [CrossRef]
- Denaro, N.; Merlano, M.C.; Russi, E.G. Follow-up in Head and Neck Cancer: Do More Does It Mean Do Better? A Systematic Review and Our Proposal Based on Our Experience. Clin. Exp. Otorhinolaryngol. 2016, 9, 287–297. [Google Scholar] [CrossRef]
- Farsi, S.; Gardner, J.R.; King, D.; Sunde, J.; Moreno, M.; Vural, E. Head and neck cancer surveillance: The value of computed tomography and clinical exam. Am. J. Otolaryngol. 2024, 45, 104469. [Google Scholar] [CrossRef]
- Mehanna, H.; Wong, W.L.; McConkey, C.C.; Rahman, J.K.; Robinson, M.; Hartley, A.G.; Nutting, C.; Powell, N.; Al-Booz, H.; Robinson, M.; et al. PET-CT Surveillance versus Neck Dissection in Advanced Head and Neck Cancer. N. Engl. J. Med. 2016, 374, 1444–1454. [Google Scholar] [CrossRef]
- Van Hoe, S.; Hermans, R. Post-treatment surveillance imaging in head and neck cancer: A systematic review. Insights Imaging 2024, 15, 32. [Google Scholar] [CrossRef]
- Cook, G.J.R.; Alberts, I.L.; Wagner, T.; Fischer, B.M.; Nazir, M.S.; Lilburn, D. The impact of long axial field of view (LAFOV) PET on oncologic imaging. Eur. J. Radiol. 2025, 183, 111873. [Google Scholar] [CrossRef] [PubMed]
- Mei, R.; Pyka, T.; Sari, H.; Fanti, S.; Afshar-Oromieh, A.; Giger, R.; Caobelli, F.; Rominger, A.; Alberts, I. The clinical acceptability of short versus long duration acquisitions for head and neck cancer using long-axial field-of-view PET/CT: A retrospective evaluation. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 1436–1443. [Google Scholar] [CrossRef] [PubMed]
- Hall, S.F.; Owen, T.; Griffiths, R.J.; Brennan, K. Does the frequency of routine follow-up after curative treatment for head-and-neck cancer affect survival? Curr. Oncol. 2019, 26, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Brands, M.T.; Brennan, P.A.; Verbeek, A.L.M.; Merkx, M.A.W.; Geurts, S.M.E. Follow-up after curative treatment for oral squamous cell carcinoma. A critical appraisal of the guidelines and a review of the literature. Eur. J. Surg. Oncol. 2018, 44, 559–565. [Google Scholar] [CrossRef]
- Richards, M. Report of THE INDEPENDENT REVIEW OF ADULT SCREENING PROGRAMMES in England. 2019. Available online: https://www.england.nhs.uk/wp-content/uploads/2019/02/report-of-the-independent-review-of-adult-screening-programme-in-england.pdf (accessed on 17 August 2025).
- Radoï, L.; Menvielle, G.; Cyr, D.; Lapôtre-Ledoux, B.; Stücker, I.; Luce, D. Population attributable risks of oral cavity cancer to behavioral and medical risk factors in France: Results of a large population-based case-control study, the ICARE study. BMC Cancer 2015, 15, 827. [Google Scholar] [CrossRef]
- Dyba, T.; Randi, G.; Bray, F.; Martos, C.; Giusti, F.; Nicholson, N.; Gavin, A.; Flego, M.; Neamtiu, L.; Dimitrova, N.; et al. The European cancer burden in 2020: Incidence and mortality estimates for 40 countries and 25 major cancers. Eur. J. Cancer 2021, 157, 308–347. [Google Scholar] [CrossRef]
- Ligier, K.; Dejardin, O.; Launay, L.; Benoit, E.; Babin, E.; Bara, S.; Lapôtre-Ledoux, B.; Launoy, G.; Guizard, A.V. Health professionals and the early detection of head and neck cancers: A population-based study in a high incidence area. BMC Cancer 2016, 16, 456. [Google Scholar] [CrossRef]
- Moyer, V.A. Screening for oral cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2014, 160, 55–60. [Google Scholar] [CrossRef]
- Cruz, G.D.; Le Geros, R.Z.; Ostroff, J.S.; Hay, J.L.; Kenigsberg, H.; Franklin, D.M. Oral cancer knowledge, risk factors and characteristics of subjects in a large oral cancer screening program. J. Am. Dent. Assoc. 2002, 133, 1064–1071. [Google Scholar] [CrossRef]
- Gourin, C.G.; Kaboli, K.C.; Blume, E.J.; Nance, M.A.; Koch, W.M. Characteristics of participants in a free oral, head and neck cancer screening program. Laryngoscope 2009, 119, 679–682. [Google Scholar] [CrossRef]
- Kravietz, A.; Angara, P.; Le, M.; Sargi, Z. Disparities in Screening for Head and Neck Cancer: Evidence from the NHANES, 2011–2014. Otolaryngol. Head Neck Surg. 2018, 159, 683–691. [Google Scholar] [CrossRef]
- Dedhia, R.C.; Smith, K.J.; Johnson, J.T.; Roberts, M. The cost-effectiveness of community-based screening for oral cancer in high-risk males in the United States: A Markov decision analysis approach. Laryngoscope 2011, 121, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.S.; Phillips, D.R.; Sayer, J.L.; Moore, M.G. A comparison of community-based and hospital-based head and neck cancer screening campaigns: Identifying high-risk individuals and early disease. JAMA Otolaryngol. Head Neck Surg. 2013, 139, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Pothiwalla, H.; Gnanaraj, J.; Paranji, S.; Daniel, A.; Khaliq, W. Oral Cancer Risk and Screening Prevalence Among Hospitalized Women. Cureus 2024, 16, e61423. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Sykes, E.A.; Weisbrod, N.; Rival, E.; Haque, A.; Fu, R.; Eskander, A. Methods, Detection Rates, and Survival Outcomes of Screening for Head and Neck Cancers: A Systematic Review. JAMA Otolaryngol. Head Neck Surg. 2023, 149, 1047–1056. [Google Scholar] [CrossRef]
- American Cancer Society. Survival Rates for Oral Cavity and Oropharyngeal Cancer. 2023. Available online: https://www.cancer.org/cancer/types/oral-cavity-and-oropharyngeal-cancer/detection-diagnosis-staging/survival-rates.html (accessed on 23 May 2025).
- Canadian Cancer Society. Survival Statistics for Oral Cancer. 2022. Available online: https://cancer.ca/en/cancer-information/cancer-types/oral/prognosis-and-survival/survival-statistics (accessed on 23 May 2025).
- Mohan, P.; Richardson, A.; Potter, J.D.; Coope, P.; Paterson, M. Opportunistic Screening of Oral Potentially Malignant Disorders: A Public Health Need for India. JCO Glob. Oncol. 2020, 6, 688–696. [Google Scholar] [CrossRef]
- Sankaranarayanan, R.; Ramadas, K.; Thomas, G.; Muwonge, R.; Thara, S.; Mathew, B.; Rajan, B. Effect of screening on oral cancer mortality in Kerala, India: A cluster-randomised controlled trial. Lancet 2005, 365, 1927–1933. [Google Scholar] [CrossRef]
- Cairns, J.; Spellman, J.; Kanatas, A. Attendance at a one-off screening clinic for head and neck cancer during Cancer Awareness Week. Br. J. Oral Maxillofac. Surg. 2020, 58, e1–e2. [Google Scholar] [CrossRef]
- World Health Organization. Comprehensive Assessment of Evidence on Oral Cancer Prevention Released. 2023. Available online: https://www.who.int/news/item/29-11-2023-comprehensive-assessment-of-evidence-on-oral-cancer-prevention-released-29-november-2023 (accessed on 23 May 2025).
- Bouvard, V.; Nethan, S.T.; Singh, D.; Warnakulasuriya, S.; Mehrotra, R.; Chaturvedi, A.K.; Chen, T.H.; Ayo-Yusuf, O.A.; Gupta, P.C.; Kerr, A.R.; et al. IARC Perspective on Oral Cancer Prevention. N. Engl. J. Med. 2022, 387, 1999–2005. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization International Agency for Research on Cancer. Oral cancer prevention. In IARC Handbook of Cancer Prevention; World Health Organization: Lyon, France, 2023. [Google Scholar]
- Brill, J.V. Screening for cancer: The economic, medical, and psychosocial issues. Am. J. Manag. Care 2020, 26 (Suppl. S14), S300–S306. [Google Scholar] [CrossRef] [PubMed]
- Ratushnyak, S.; Hoogendoorn, M.; van Baal, P.H.M. Cost-Effectiveness of Cancer Screening: Health and Costs in Life Years Gained. Am. J. Prev. Med. 2019, 57, 792–799. [Google Scholar] [CrossRef] [PubMed]
- Speight, P.M.; Palmer, S.; Moles, D.R.; Downer, M.C.; Smith, D.H.; Henriksson, M.; Augustovski, F. The cost-effectiveness of screening for oral cancer in primary care. Health Technol. Assess. 2006, 10, 1–144. [Google Scholar] [CrossRef]
- Chan, K.C.A.; Woo, J.K.S.; King, A.; Zee, B.C.Y.; Lam, W.K.J.; Chan, S.L.; Chu, S.W.I.; Mak, C.; Tse, I.O.L.; Leung, S.Y.M.; et al. Analysis of Plasma Epstein-Barr Virus DNA to Screen for Nasopharyngeal Cancer. N. Engl. J. Med. 2017, 377, 513–522. [Google Scholar] [CrossRef]
- Chan, K.C.A.; Lam, W.K.J.; King, A.; Lin, V.S.; Lee, P.P.H.; Zee, B.C.Y.; Chan, S.L.; Tse, I.O.L.; Tsang, A.F.C.; Li, M.Z.J.; et al. Plasma Epstein-Barr Virus DNA and Risk of Future Nasopharyngeal Cancer. NEJM Evid. 2023, 2, EVIDoa2200309. [Google Scholar] [CrossRef]
- Coghill, A.E.; Hsu, W.L.; Pfeiffer, R.M.; Juwana, H.; Yu, K.J.; Lou, P.J.; Wang, C.P.; Chen, J.Y.; Chen, C.J.; Middeldorp, J.M.; et al. Epstein-Barr virus serology as a potential screening marker for nasopharyngeal carcinoma among high-risk individuals from multiplex families in Taiwan. Cancer Epidemiol. Biomark. Prev. 2014, 23, 1213–1219. [Google Scholar] [CrossRef]
- Yang, S.; Wu, S.; Zhou, J.; Chen, X.Y. Screening for nasopharyngeal cancer. Cochrane Database Syst. Rev. 2015, 2015, Cd008423. [Google Scholar] [CrossRef]
- Rui, M.; Wang, Y.; You, J.H.S. Health Economic Evaluations of Circulating Tumor DNA Testing for Cancer Screening: Systematic Review. Cancer Med. 2025, 14, e70641. [Google Scholar] [CrossRef]
- Chow, J.C.H.; Lee, A.W.M.; Wong, C.H.L.; Ng, W.T.; Liu, Z.; Tay, J.K.; Loh, K.S.; Pace-Asciak, P.; Cohen, O.; Corry, J.; et al. Epstein-Barr virus directed screening for nasopharyngeal carcinoma in individuals with positive family history: A systematic review. Oral Oncol. 2022, 133, 106031. [Google Scholar] [CrossRef]
- Dwivedi, P.; Lohiya, A.; Bahuguna, P.; Singh, A.; Sulaiman, D.; Singh, M.K.; Rajsekar, K.; Rizwan, S.A. Cost-effectiveness of population-based screening for oral cancer in India: An economic modelling study. Lancet Reg. Health Southeast Asia 2023, 16, 100224. [Google Scholar] [CrossRef]
- Warnakulasuriya, S.; Kerr, A.R. Oral Cancer Screening: Past, Present, and Future. J. Dent. Res. 2021, 100, 1313–1320. [Google Scholar] [CrossRef]
- Shruti, T.; Khanna, D.; Khan, A.; Dandpat, A.; Tiwari, M.; Singh, A.G.; Mishra, A.; Shetty, A.; Birur, P.; Chaturvedi, P. Status and Determinants of Early Detection of Oral Premalignant and Malignant Lesions in India. Cancer Control 2023, 30, 10732748231159556. [Google Scholar] [CrossRef] [PubMed]
- Khanna, D.; Mishra, A.; Birur, P.; Shruti, T.; Gurushanth, K.; Mukhia, N.; Pathak, R.; Gurmeet Singh, A.; Shetty, A.; Pradhan, S.; et al. A prospective study on diagnostic accuracy of technology-enabled early detection of oral cancer and epidemiology of tobacco and other substances use in rural India. Cancer 2025, 131, e35702. [Google Scholar] [CrossRef] [PubMed]
- Kumdee, C.; Kulpeng, W.; Teerawattananon, Y. Cost-utility analysis of the screening program for early oral cancer detection in Thailand. PLoS ONE 2018, 13, e0207442. [Google Scholar] [CrossRef] [PubMed]
- European Head & Neck Society. Make Sense Campaign. 2025. Available online: https://makesensecampaign.eu/en/ (accessed on 23 May 2025).
- Hosal, S.; Golusiński, W.; René Leemans, C.; Dietz, A.; Licitria, L.; Simon, C.; Gomes, A.V.; Verdonck-de Leeuw, I. European Cancer Summit 2022 submission for Prevention, Early Detection and Screening NetworkThe value of awareness campaigns in the head and neck cancer setting: An evaluation of the European Head and Neck Society’s Make Sense campaign. J. Cancer Policy 2023, 35. [Google Scholar] [CrossRef]
- Baumann, E.; Koller, M.; Wenz, H.J.; Wiltfang, J.; Hertrampf, K. Oral cancer awareness campaign in Northern Germany: Successful steps to raise awareness for early detection. J. Cancer Res. Clin. Oncol. 2023, 149, 8779–8789. [Google Scholar] [CrossRef]
- Hertrampf, K.; Pritzkuleit, R.; Baumann, E.; Wiltfang, J.; Wenz, H.J.; Waldmann, A. Oral cancer awareness campaign in Northern Germany: First positive trends in incidence and tumour stages. J. Cancer Res. Clin. Oncol. 2020, 146, 2489–2496. [Google Scholar] [CrossRef]
- She, Y.; Nong, X.; Zhang, M.; Wang, M. Epstein-Barr virus infection and oral squamous cell carcinoma risk: A meta-analysis. PLoS ONE 2017, 12, e0186860. [Google Scholar] [CrossRef]
- Tay, J.K.; Siow, C.H.; Goh, H.L.; Lim, C.M.; Hsu, P.P.; Chan, S.H.; Loh, K.S. A comparison of EBV serology and serum cell-free DNA as screening tools for nasopharyngeal cancer: Results of the Singapore NPC screening cohort. Int. J. Cancer 2020, 146, 2923–2931. [Google Scholar] [CrossRef]
- Lo, Y.M.; Chan, L.Y.; Chan, A.T.; Leung, S.F.; Lo, K.W.; Zhang, J.; Lee, J.C.; Hjelm, N.M.; Johnson, P.J.; Huang, D.P. Quantitative and temporal correlation between circulating cell-free Epstein-Barr virus DNA and tumor recurrence in nasopharyngeal carcinoma. Cancer Res. 1999, 59, 5452–5455. [Google Scholar] [PubMed]
- Wang, W.Y.; Twu, C.W.; Lin, W.Y.; Jiang, R.S.; Liang, K.L.; Chen, K.W.; Wu, C.T.; Shih, Y.T.; Lin, J.C. Plasma Epstein-Barr virus DNA screening followed by 18F-fluoro-2-deoxy-D-glucose positron emission tomography in detecting posttreatment failures of nasopharyngeal carcinoma. Cancer 2011, 117, 4452–4459. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.P.; Huang, X.D.; Lv, J.W.; Wen, D.W.; Zhou, G.Q.; Lin, L.; Kou, J.; Wu, C.F.; Chen, Y.; Zheng, Z.Q.; et al. Prognostic potential of liquid biopsy tracking in the posttreatment surveillance of patients with nonmetastatic nasopharyngeal carcinoma. Cancer 2020, 126, 2163–2173. [Google Scholar] [CrossRef] [PubMed]
- Zhou, G.Q.; Lv, J.W.; Tang, L.L.; Mao, Y.P.; Guo, R.; Ma, J.; Sun, Y. Evaluation of the National Comprehensive Cancer Network and European Society for Medical Oncology Nasopharyngeal Carcinoma Surveillance Guidelines. Front. Oncol. 2020, 10, 119. [Google Scholar] [CrossRef]
- Bossi, P.; Chan, A.T.; Licitra, L.; Trama, A.; Orlandi, E.; Hui, E.P.; Halamkova, J.; Mattheis, S.; Baujat, B.; Hardillo, J.; et al. Nasopharyngeal carcinoma: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up(dagger). Ann. Oncol. 2021, 32, 452–465. [Google Scholar] [CrossRef]
- Yuan, Y.; Ye, F.; Wu, J.H.; Fu, X.Y.; Huang, Z.X.; Zhang, T. Early screening of nasopharyngeal carcinoma. Head Neck 2023, 45, 2700–2709. [Google Scholar] [CrossRef]
- Faden, D.L. Liquid biopsy for the diagnosis of HPV-associated head and neck cancer. Cancer Cytopathol. 2022, 130, 12–15. [Google Scholar] [CrossRef]
- Kentnowski, M.; Cortez, A.J.; Mazurek, A.M.; Mrochem-Kwarciak, J.; Hebda, A.; Kacorzyk, U.; Drosik-Rutowicz, K.; Chmielik, E.; Paul, P.; Gajda, K.; et al. Determinants of the level of circulating-tumor HPV16 DNA in patients with HPV-associated oropharyngeal cancer at the time of diagnosis. Sci. Rep. 2023, 13, 21226. [Google Scholar] [CrossRef]
- Aye, L.; Bryan, M.E.; Das, D.; Hirayama, S.; Al-Inaya, Y.; Mendel, J.; Naegele, S.; Fisch, A.S.; Faquin, W.C.; Sadow, P.; et al. Multi-feature next-generation liquid biopsy for diagnosis and prognosis in HPV-associated head and neck cancer. J. Clin. Oncol. 2024, 42 (Suppl. S16), 6064. [Google Scholar] [CrossRef]
- Das, D.; Hirayama, S.; Aye, L.; Bryan, M.E.; Naegele, S.; Zhao, B.; Efthymiou, V.; Mendel, J.; Fisch, A.S.; Kröller, L.; et al. Blood-based screening for HPV-associated cancers. medRxiv 2024. [Google Scholar] [CrossRef]
- Ma, D.M.; Price, K.; Moore, E.J.; Patel, S.H.; Hinni, M.L.; Fruth, B.; Foster, N.R.; Van Abel, K.; Yin, L.X.; Neben-Wittich, M.A.; et al. MC1675, a Phase III Evaluation of De-Escalated Adjuvant Radiation Therapy (DART) vs. Standard Adjuvant Treatment for Human Papillomavirus Associated Oropharyngeal Squamous Cell Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 1324. [Google Scholar] [CrossRef]
- Routman, D.M.; Van Abel, K.M.; Price, K.A.; Moore, E.J.; Patel, S.H.; Hinni, M.L.; Fruth, B.; Foster, N.R.; Yin, L.X.; Neben-Wittich, M.; et al. ctDNA and Recurrence Risk for Adjuvant De-Escalation in HPV-Positive Oropharyngeal Carcinoma: A Secondary Analysis of the DART Phase 3 Randomized Clinical Trial. JAMA Otolaryngol. Head Neck Surg. 2025, 151, 665. [Google Scholar] [CrossRef]
- Hirayama, S.; Al-Inaya, Y.; Aye, L.; Bryan, M.; Das, D.; Mendel, J.; Naegele, S.; Faquin, W.; Sadow, P.; Fisch, A.; et al. Prospective validation of ctHPVDNA for detection of minimal residual disease and prediction of recurrence in patients with HPV-associated head and neck cancer treated with surgery. J. Clin. Oncol. 2024, 42, 6010. [Google Scholar] [CrossRef]
- Bryan, M.E.; Aye, L.; Das, D.; Hirayama, S.; Al-Inaya, Y.; Mendel, J.; Naegele, S.; Efthymiou, V.; Alzumaili, B.; Faquin, W.C.; et al. Direct Comparison of Alternative Blood-Based Approaches for Early Detection and Diagnosis of HPV-Associated Head and Neck Cancers. Clin. Cancer Res. 2025, 31, Of1–Of11. [Google Scholar] [CrossRef]
- Sim, E.S.; Rhoades, J.; Xiong, K.; Walsh, L.; Crnjac, A.; Blewett, T.; Al-Inaya, Y.; Mendel, J.; Ruiz-Torres, D.A.; Efthymiou, V.; et al. Early Postoperative Minimal Residual Disease Detection with MAESTRO Is Associated with Recurrence and Worse Survival in Patients with Head and Neck Cancer. Clin. Cancer Res. 2025, 31, Of1–Of9. [Google Scholar] [CrossRef]
- Diez-Fraile, A.; De Ceulaer, J.; Derpoorter, C.; Spaas, C.; De Backer, T.; Lamoral, P.; Abeloos, J.; Lammens, T. Tracking the Molecular Fingerprint of Head and Neck Cancer for Recurrence Detection in Liquid Biopsies. Int. J. Mol. Sci. 2022, 23, 2403. [Google Scholar] [CrossRef]
- Mohammadi, N.; Rosenberg, A.J.; Izumchenko, E.G.; Pearson, A.T.; Skandari, M.R. Computationally optimized ctDNA surveillance for recurrence detection in HPV-positive head and neck squamous cell carcinoma. medRxiv 2025. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Network. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015, 517, 576–582. [Google Scholar] [CrossRef]
- Flach, S.; Kumbrink, J.; Walz, C.; Hess, J.; Drexler, G.; Belka, C.; Canis, M.; Jung, A.; Baumeister, P. Analysis of genetic variants of frequently mutated genes in human papillomavirus-negative primary head and neck squamous cell carcinoma, resection margins, local recurrences and corresponding circulating cell-free DNA. J. Oral Pathol. Med. 2022, 51, 738–746. [Google Scholar] [CrossRef]
- Honoré, N.; van Marcke, C.; Galot, R.; Helaers, R.; Ambroise, J.; van Maanen, A.; Mendola, A.; Dahou, H.; Marbaix, E.; Van Eeckhout, P.; et al. Tumor-agnostic plasma assay for circulating tumor DNA detects minimal residual disease and predicts outcome in locally advanced squamous cell carcinoma of the head and neck. Ann. Oncol. 2023, 34, 1175–1186. [Google Scholar] [CrossRef]
- Lennon, A.M.; Buchanan, A.H.; Kinde, I.; Warren, A.; Honushefsky, A.; Cohain, A.T.; Ledbetter, D.H.; Sanfilippo, F.; Sheridan, K.; Rosica, D.; et al. Feasibility of blood testing combined with PET-CT to screen for cancer and guide intervention. Science 2020, 369, eabb9601. [Google Scholar] [CrossRef]
- Cohen, J.D.; Li, L.; Wang, Y.; Thoburn, C.; Afsari, B.; Danilova, L.; Douville, C.; Javed, A.A.; Wong, F.; Mattox, A.; et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 2018, 359, 926–930. [Google Scholar] [CrossRef]
- Wong, S.Q.; Dawson, S.J. Combining liquid biopsies and PET-CT for early cancer detection. Nat. Med. 2020, 26, 1010–1011. [Google Scholar] [CrossRef] [PubMed]
- Bola, S.; Cutts, A.; Vavoulis, D.; Shrivastava, M.; Bhuva, S.; Schuh, A.; Shah, K.; Winter, S.C.; Taylor, J.C. Circulating tumour DNA to augment PET-CT in determining clinical outcome after head and neck cancer treatment. Eur. J. Cancer 2025, 227, 115626. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.S.; Bonan, P.R.; Ferreira, V.Y.; de Lucena Pereira, L.; Correia, R.J.; da Silva Teixeira, H.B.; Pereira, D.C.; Bonan, P. Development of a mobile application for oral cancer screening. Technol. Health Care 2017, 25, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Birur, N.P.; Gurushanth, K.; Patrick, S.; Sunny, S.P.; Raghavan, S.A.; Gurudath, S.; Hegde, U.; Tiwari, V.; Jain, V.; Imran, M.; et al. Role of community health worker in a mobile health program for early detection of oral cancer. Indian J. Cancer 2019, 56, 107–113. [Google Scholar] [CrossRef]
- Vinayagamoorthy, K.; Acharya, S.; Kumar, M.; Pentapati, K.C.; Acharya, S. Efficacy of a remote screening model for oral potentially malignant disorders using a free messaging application: A diagnostic test for accuracy study. Aust. J. Rural Health 2019, 27, 170–176. [Google Scholar] [CrossRef]
- Birur, N.P.; Song, B.; Sunny, S.P.; Keerthi, G.; Mendonca, P.; Mukhia, N.; Li, S.; Patrick, S.; Shubha, G.; Subhashini, A.R.; et al. Field validation of deep learning based Point-of-Care device for early detection of oral malignant and potentially malignant disorders. Sci. Rep. 2022, 12, 14283. [Google Scholar] [CrossRef]
- Pierfelice, T.V.; D’Amico, E.; Cinquini, C.; Iezzi, G.; D’Arcangelo, C.; D’Ercole, S.; Petrini, M. The Diagnostic Potential of Non-Invasive Tools for Oral Cancer and Precancer: A Systematic Review. Diagnostics 2024, 14, 2033. [Google Scholar] [CrossRef]
- Lau, J.; Guru, O.; Warnakulasuriya, S.; Balasubramaniam, R.; Frydrych, A.; Kujan, O. Adjunctive aids for the detection of oral squamous cell carcinoma and oral potentially malignant disorders: A systematic review of systematic reviews. Jpn. Dent. Sci. Rev. 2024, 60, 53–72. [Google Scholar] [CrossRef]
- Lingen, M.W.; Tampi, M.P.; Urquhart, O.; Abt, E.; Agrawal, N.; Chaturvedi, A.K.; Cohen, E.; D’Souza, G.; Gurenlian, J.; Kalmar, J.R.; et al. Adjuncts for the evaluation of potentially malignant disorders in the oral cavity: Diagnostic test accuracy systematic review and meta-analysis-a report of the American Dental Association. J. Am. Dent. Assoc. 2017, 148, 797–813.e52. [Google Scholar] [CrossRef] [PubMed]
- Walsh, T.; Macey, R.; Kerr, A.R.; Lingen, M.W.; Ogden, G.R.; Warnakulasuriya, S. Diagnostic tests for oral cancer and potentially malignant disorders in patients presenting with clinically evident lesions. Cochrane Database Syst. Rev. 2021, 7, Cd010276. [Google Scholar] [CrossRef] [PubMed]
- Maraki, D.; Becker, J.; Boecking, A. Cytologic and DNA-cytometric very early diagnosis of oral cancer. J. Oral Pathol. Med. 2004, 33, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.M.; Zhou, T.J.; Wang, R.; Shan, J.; Wu, Y.N.; Song, X.L.; Gu, N.; Fan, Y. Brush biopsy with DNA-image cytometry: A useful and noninvasive method for monitoring malignant transformation of potentially malignant oral disorders. Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 3291–3295. [Google Scholar] [CrossRef]
- Ng, S.P.; Mann, I.S.; Zed, C.; Doudkine, A.; Matisic, J. The use of quantitative cytology in identifying high-risk oral lesions in community practice. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, 358–364. [Google Scholar] [CrossRef]
- Piazza, C.; Francesca, D.B.; Peretti, G.; Nicolai, P. ‘Biologic endoscopy’: Optimization of upper aerodigestive tract cancer evaluation. Curr. Opin. Otolaryngol. Head Neck Surg. 2011, 19, 67–76. [Google Scholar] [CrossRef]
- Green, B.; Cobb, A.R.; Brennan, P.A.; Hopper, C. Optical diagnostic techniques for use in lesions of the head and neck: Review of the latest developments. Br. J. Oral Maxillofac. Surg. 2014, 52, 675–680. [Google Scholar] [CrossRef]
- Sweeny, L.; Dean, N.R.; Magnuson, J.S.; Carroll, W.R.; Clemons, L.; Rosenthal, E.L. Assessment of tissue autofluorescence and reflectance for oral cavity cancer screening. Otolaryngol. Head Neck Surg. 2011, 145, 956–960. [Google Scholar] [CrossRef]
- Walsh, T.; Warnakulasuriya, S.; Lingen, M.W.; Kerr, A.R.; Ogden, G.R.; Glenny, A.M.; Macey, R. Clinical assessment for the detection of oral cavity cancer and potentially malignant disorders in apparently healthy adults. Cochrane Database Syst. Rev. 2021, 12, Cd010173. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, Y.; Pan, D.; Zhang, Z.; Jiang, L.; Feng, X.; Jiang, Y.; Luo, X.; Chen, Q. Accuracy of narrow band imaging for detecting the malignant transformation of oral potentially malignant disorders: A systematic review and meta-analysis. Front. Surg. 2022, 9, 1068256. [Google Scholar] [CrossRef]
- Piazza, C.; Cocco, D.; Del Bon, F.; Mangili, S.; Nicolai, P.; Majorana, A.; Bolzoni Villaret, A.; Peretti, G. Narrow band imaging and high definition television in evaluation of oral and oropharyngeal squamous cell cancer: A prospective study. Oral Oncol. 2010, 46, 307–310. [Google Scholar] [CrossRef]
- Yang, S.W.; Lee, Y.S.; Chang, L.C.; Chien, H.P.; Chen, T.A. Light sources used in evaluating oral leukoplakia: Broadband white light versus narrowband imaging. Int. J. Oral Maxillofac. Surg. 2013, 42, 693–701. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, T.; Liu, D.; Qiu, X.; Hou, F.; Wang, J.; Luo, X.; Dan, H.; Zhou, Y.; Zeng, X.; et al. New IPCL Classification Using NBI for Early Detection of OPMDs Malignant Transformation. Oral Dis. 2025, 31, 1198–1205. [Google Scholar] [CrossRef]
- Azam, M.A.; Sampieri, C.; Ioppi, A.; Benzi, P.; Giordano, G.G.; De Vecchi, M.; Campagnari, V.; Li, S.; Guastini, L.; Paderno, A.; et al. Videomics of the Upper Aero-Digestive Tract Cancer: Deep Learning Applied to White Light and Narrow Band Imaging for Automatic Segmentation of Endoscopic Images. Front. Oncol. 2022, 12, 900451. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kim, S.W.; Hwang, S.H. Efficacy of optical coherence tomography in the diagnosing of oral cancerous lesion: Systematic review and meta-analysis. Head Neck 2023, 45, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Nagi, R.; Bibra, A.; Rakesh, N.; Patil, D.J.; Vyas, T. Artificial intelligence-integrated optical coherence tomography for screening and early detection of oral cancer. Gen. Dent. 2024, 72, 46–52. [Google Scholar] [PubMed]
- Carta, F.; Sionis, S.; Cocco, D.; Gerosa, C.; Ferreli, C.; Puxeddu, R. Enhanced contact endoscopy for the assessment of the neoangiogenetic changes in precancerous and cancerous lesions of the oral cavity and oropharynx. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 1895–1903. [Google Scholar] [CrossRef]
- Klančnik, M.; Glunčić, I.; Cikojević, D. The role of contact endoscopy in screening for premalignant laryngeal lesions: A study of 141 patients. Ear Nose Throat J. 2014, 93, 177–180. [Google Scholar] [CrossRef]
- Esmaeili, N.; Sharaf, E.; Gomes Ataide, E.J.; Illanes, A.; Boese, A.; Davaris, N.; Arens, C.; Navab, N.; Friebe, M. Deep Convolution Neural Network for Laryngeal Cancer Classification on Contact Endoscopy-Narrow Band Imaging. Sensors 2021, 21, 8157. [Google Scholar] [CrossRef]
- Farah, C.S.; Janik, M.; Woo, S.B.; Grew, J.; Slim, Z.; Fox, S.A. Dynamic real-time optical microscopy of oral mucosal lesions using confocal laser endomicroscopy. J. Oral Pathol. Med. 2023, 52, 539–547. [Google Scholar] [CrossRef]
- Ramani, R.S.; Tan, I.; Bussau, L.; O’Reilly, L.A.; Silke, J.; Angel, C.; Celentano, A.; Whitehead, L.; McCullough, M.; Yap, T. Convolutional neural networks for accurate real-time diagnosis of oral epithelial dysplasia and oral squamous cell carcinoma using high-resolution in vivo confocal microscopy. Sci. Rep. 2025, 15, 2555. [Google Scholar] [CrossRef] [PubMed]
- Bugter, O.; Hardillo, J.A.; Baatenburg de Jong, R.J.; Amelink, A.; Robinson, D.J. Optical pre-screening for laryngeal cancer using reflectance spectroscopy of the buccal mucosa. Biomed. Opt. Express 2018, 9, 4665–4678. [Google Scholar] [CrossRef] [PubMed]
- Bailey, M.J.; Verma, N.; Fradkin, L.; Lam, S.; MacAulay, C.; Poh, C.; Markey, M.K.; Sokolov, K. Detection of precancerous lesions in the oral cavity using oblique polarized reflectance spectroscopy: A clinical feasibility study. J. Biomed. Opt. 2017, 22, 65002. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Lang, Z.Q.; Guo, L.; Walker, D.C.; Matella, M.; Wang, M.; Murdoch, C. Deep learning-based electrical impedance spectroscopy analysis for malignant and potentially malignant oral disorder detection. Sci. Rep. 2025, 15, 19458. [Google Scholar] [CrossRef]
- Sharwani, A.; Jerjes, W.; Salih, V.; Swinson, B.; Bigio, I.J.; El-Maaytah, M.; Hopper, C. Assessment of oral premalignancy using elastic scattering spectroscopy. Oral Oncol. 2006, 42, 343–349. [Google Scholar] [CrossRef]
- Hanna, K.; Asiedu, A.L.; Theurer, T.; Muirhead, D.; Speirs, V.; Oweis, Y.; Abu-Eid, R. Advances in Raman spectroscopy for characterising oral cancer and oral potentially malignant disorders. Expert Rev. Mol. Med. 2024, 26, e25. [Google Scholar] [CrossRef]
- Lin, Y.C.; Watanabe, A.; Chen, W.C.; Lee, K.F.; Lee, I.L.; Wang, W.H. Narrowband imaging for early detection of malignant tumors and radiation effect after treatment of head and neck cancer. Arch. Otolaryngol. Head Neck Surg. 2010, 136, 234–239. [Google Scholar] [CrossRef]
- Inoue, H. Endoscopic diagnosis of tissue atypism (EA) in the pharyngeal and esophageal squamous epithelium; IPCL pattern classification and ECA classification. Kyobu Geka 2007, 60 (Suppl. S8), 768–775. [Google Scholar]
- Krishna, H.; Majumder, S.K.; Chaturvedi, P.; Sidramesh, M.; Gupta, P.K. In vivo Raman spectroscopy for detection of oral neoplasia: A pilot clinical study. J. Biophotonics 2014, 7, 690–702. [Google Scholar] [CrossRef]
- Matthies, L.; Gebrekidan, M.T.; Tegtmeyer, J.F.; Oetter, N.; Rohde, M.; Vollkommer, T.; Smeets, R.; Wilczak, W.; Stelzle, F.; Gosau, M.; et al. Optical diagnosis of oral cavity lesions by label-free Raman spectroscopy. Biomed. Opt. Express 2021, 12, 836–851. [Google Scholar] [CrossRef]
- Maryam, S.; Benazza, A.; Fahy, E.; Sekar, S.K.V.; Dinish, U.S.; Olivo, M.; Riordain, R.N.; Andersson-Engels, S.; Humbert, G.; Komolibus, K.; et al. Liquid saliva analysis using optofluidic photonic crystal fiber for detection of oral potentially malignant disorders. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2025, 332, 125788. [Google Scholar] [CrossRef]
- Chen, P.H.; Lee, H.Y.; Chen, Y.F.; Yeh, Y.C.; Chang, K.W.; Hou, M.C.; Kuo, W.C. Detection of Oral Dysplastic and Early Cancerous Lesions by Polarization-Sensitive Optical Coherence Tomography. Cancers 2020, 12, 2376. [Google Scholar] [CrossRef]
- Sidransky, D. The oral cavity as a molecular mirror of lung carcinogenesis. Cancer Prev. Res. 2008, 1, 12–14. [Google Scholar] [CrossRef]
- Bugter, O.; van Brummelen, S.E.; van der Leest, K.H.; Aerts, J.; Maat, A.; Baatenburg de Jong, R.J.; Amelink, A.; Robinson, D.J. Towards the Optical Detection of Field Cancerization in the Buccal Mucosa of Patients with Lung Cancer. Transl. Oncol. 2019, 12, 1533–1538. [Google Scholar] [CrossRef]
| Strategy Type | Method | Use Case/Notes |
|---|---|---|
| Opportunistic | Oral visual/tactile exam | Dentist and physician visits |
| Invitational | Letter-based outreach | Rarely implemented; mainly by otolaryngology departments used |
| Community-based | Trained health workers conduct screenings | With health workers mainly studying in India |
| Hospital-based campaigns | Drop-in screenings | Like in the European Make Sense Campaign |
| Self-examination | Mouth self-exam | Not yet widely validated |
| Technique | Comment |
|---|---|
| Oral cancer screening with smartphone images from the field to specialists | Sensitivity of 82–94%; specificity of 72–100% [101,133,134,135,136] |
| Vital staining | With toluidine blue or Lugol’s iodine: pooled sensitivity of 86% and specificity of 68% [137,138] |
| Cytology | As exfoliative biopsy or brush biopsy cytology; pooled sensitivity of 90–92% and specificity of 94% [139,140] |
| DNA cytometry | Mainly to detect aneuploidy; pooled sensitivity of 76% and specificity of 98% [141,142,143] |
| Imaging Technique | Comment |
|---|---|
| Tissue autofluorescence | Sensitivity of 81% but very low specificity of 50%, cannot be recommended [146,147] |
| Tissue reflectance | Via direct illumination with low-wavelength light; pooled sensitivity of 94% but very low specificity of 19–69%; hence, it cannot be recommended [139,147] |
| Narrow-band imaging (NBI) | Tool for identifying malignant transformation of oral potentially malignant disorders and oral cancer; intra-epithelial papillary capillary loop (IPCL) classification II or above is recommended to undergo biopsy; pooled sensitivity of 87–96% and specificity of 83–98%. Medical devices available [148,149,150,151,152] |
| Optical coherence tomography (OCT) | Also, a tool for the detection of oral cancer; pooled sensitivity of about 91% and specificity also of 91% [153]; implementation of machine learning algorithms might help to improve the accuracy [154] |
| Contact endoscopy | Analyzed for use in the oral cavity, pharynx, and larynx. Can reach a sensitivity and specificity of >95%. Needs experience in the interpretation of the vascular structure [155,156,157,158]. Contact endoscopy. Medical devices available |
| Confocal endomicroscopy | Confocal laser endomicroscopy combined with the contrast agents acriflavine or fluorescein and machine learning. Accuracy in two studies was sensitivity 81–86.8%, specificity 92–95%. Medical devices available [158,159] |
| Reflectance spectroscopy | This was used to field cancerization in the oral cavity in patients with laryngeal cancer [160], but not for screening for oral cancer; as polarized reflectance spectroscopy with a sensitivity 74–80%, specificity 80–93% [161]; might be used in the future also for screening when improved by the use of deep learning analysis [162] |
| Elastic scattering spectroscopy | Just used in a few studies; sensitivity of 72% and a specificity of 75% [163] |
| Raman spectroscopy, including surface-enhanced Raman spectroscopy (SERS) and shifted-excitation Raman difference spectroscopy (SERDS) | When coupled with deep learning, both sensitivity and specificity can reach values > 95% [164] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guntinas-Lichius, O.; Bücking, C.; Ng, S.P.; López, F.; Rodrigo, J.P.; Rao, K.N.; Pelaz, A.C.; Kowalski, L.P.; Piazza, C.; Rinaldo, A.; et al. Targeted Screening Strategies for Head and Neck Cancer: A Global Review of Evidence, Technologies, and Cost-Effectiveness. Diagnostics 2025, 15, 2095. https://doi.org/10.3390/diagnostics15162095
Guntinas-Lichius O, Bücking C, Ng SP, López F, Rodrigo JP, Rao KN, Pelaz AC, Kowalski LP, Piazza C, Rinaldo A, et al. Targeted Screening Strategies for Head and Neck Cancer: A Global Review of Evidence, Technologies, and Cost-Effectiveness. Diagnostics. 2025; 15(16):2095. https://doi.org/10.3390/diagnostics15162095
Chicago/Turabian StyleGuntinas-Lichius, Orlando, Claudio Bücking, Sweet Ping Ng, Fernando López, Juan Pablo Rodrigo, Karthik N. Rao, Andrés Coca Pelaz, Luiz P. Kowalski, Cesare Piazza, Alessandra Rinaldo, and et al. 2025. "Targeted Screening Strategies for Head and Neck Cancer: A Global Review of Evidence, Technologies, and Cost-Effectiveness" Diagnostics 15, no. 16: 2095. https://doi.org/10.3390/diagnostics15162095
APA StyleGuntinas-Lichius, O., Bücking, C., Ng, S. P., López, F., Rodrigo, J. P., Rao, K. N., Pelaz, A. C., Kowalski, L. P., Piazza, C., Rinaldo, A., & Ferlito, A. (2025). Targeted Screening Strategies for Head and Neck Cancer: A Global Review of Evidence, Technologies, and Cost-Effectiveness. Diagnostics, 15(16), 2095. https://doi.org/10.3390/diagnostics15162095











