Machine Learning in Myasthenia Gravis: A Systematic Review of Prognostic Models and AI-Assisted Clinical Assessments
Abstract
1. Introduction
2. Materials and Methods
2.1. Review Protocol and Registration
2.2. Eligibility Criteria
2.3. Data Source and Search Strategy
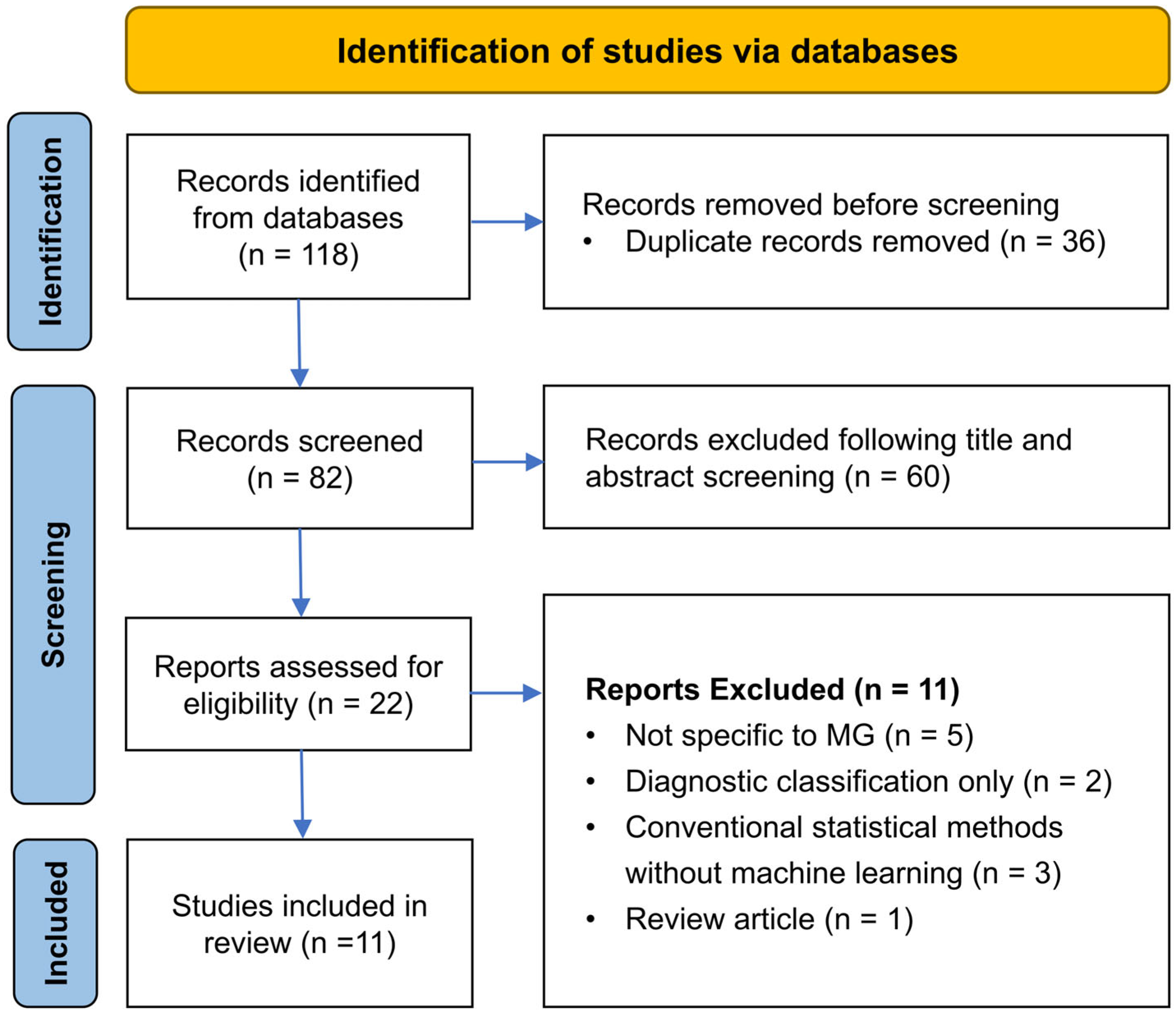
2.4. Article Selection
2.5. Data Extraction
2.6. Risk-of-Bias and Quality Assessments
2.7. Data Synthesis and Analysis
3. Results
3.1. Review Sample
3.2. Study Characteristics
3.3. Model Characteristics and Performance
3.4. Risk of Bias and Applicability
4. Discussion
4.1. Targeted Outcomes and Their Relevance to Critical Care
4.2. Balancing Transparency and Accuracy in Algorithm Design
4.3. Bridging the Gaps Between Explainability and Clinical Acceptability
4.4. The Blurred Boundary Between Prediction and Early Warning
4.5. Critical Care Applications and Implementation Challenges
4.6. Research Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AChR | Acetylcholine receptor |
| ADL | Activities of daily living |
| AUC | Area under the curve |
| AI | Artificial intelligence |
| CART | Classification and regression tree |
| ICU | Intensive care unit |
| LR | Logistic regression |
| MAPE | Mean absolute percentage error |
| MARS | Multivariate adaptive regression splines |
| MG | Myasthenia gravis |
| MG-CE | Myasthenia Gravis Core Examination |
| MGFA | Myasthenia Gravis Foundation of America |
| MLR | Multiple linear regression |
| NLP | Natural language processing |
| NLR | Neutrophil-to-lymphocyte ratio |
| PCA | Principal component analysis |
| PIS | Postintervention status |
| PLR | Platelet-to-lymphocyte ratio |
| QMG | Quantitative myasthenia gravis |
| RAE | Relative absolute error |
| SHAP | SHapley Additive exPlanations |
| SII | Systemic immune-inflammation index |
| SMAPE | Symmetric mean absolute percentage error |
| SVM | Support vector machine |
| XGBoost | eXtreme gradient boosting |
References
- Gilhus Nils, E. Myasthenia Gravis. N. Engl. J. Med. 2016, 375, 2570–2581. [Google Scholar] [CrossRef]
- Gilhus, N.E.; Verschuuren, J.J. Myasthenia Gravis: Subgroup Classification and Therapeutic Strategies. Lancet Neurol. 2015, 14, 1023–1036. [Google Scholar] [CrossRef]
- Claytor, B.; Cho, S.M.; Li, Y. Myasthenic Crisis. Muscle Nerve 2023, 68, 8–19. [Google Scholar] [CrossRef]
- Neumann, B.; Angstwurm, K.; Mergenthaler, P.; Kohler, S.; Schönenberger, S.; Bösel, J.; Neumann, U.; Vidal, A.; Huttner, H.B.; Gerner, S.T.; et al. Stetefeld. Myasthenic Crisis Demanding Mechanical Ventilation: A Multicenter Analysis of 250 Cases. Neurology 2020, 94, e299–e313. [Google Scholar] [CrossRef]
- Wang, Y.; Huan, X.; Zhu, X.; Song, J.; Yan, C.; Yang, L.; Xi, C.; Xu, Y.; Xi, J.; Zhao, C.; et al. Independent Risk Factors for in-Hospital Outcome of Myasthenic Crisis: A Prospective Cohort Study. Ther. Adv. Neurol. Disord. 2024, 17, 17562864241226745. [Google Scholar] [CrossRef] [PubMed]
- Schneider-Gold, C.; Hagenacker, T.; Melzer, N.; Ruck, T. Understanding the Burden of Refractory Myasthenia Gravis. Ther. Adv. Neurol. Disord. 2019, 12, 1756286419832242. [Google Scholar] [CrossRef] [PubMed]
- Tsai, N.W.; Chien, L.N.; Hung, C.; Kuo, A.; Chiu, Y.T.; Lin, H.W.; Jian, L.S.; Chou, K.P.; Yeh, J.H. Epidemiology, Patient Characteristics, and Treatment Patterns of Myasthenia Gravis in Taiwan: A Population-Based Study. Neurol. Ther. 2024, 13, 809–824. [Google Scholar] [CrossRef] [PubMed]
- Patel, U.K.; Anwar, A.; Saleem, S.; Malik, P.; Rasul, B.; Patel, K.; Yao, R.; Seshadri, A.; Yousufuddin, M.; Arumaithurai, K. Artificial Intelligence as an Emerging Technology in the Current Care of Neurological Disorders. J. Neurol. 2021, 268, 1623–1642. [Google Scholar] [CrossRef]
- Myszczynska, M.A.; Ojamies, P.N.; Lacoste, A.M.B.; Neil, D.; Saffari, A.; Mead, R.; Hautbergue, G.M.; Holbrook, J.D.; Ferraiuolo, L. Applications of Machine Learning to Diagnosis and Treatment of Neurodegenerative Diseases. Nat. Rev. Neurol. 2020, 16, 440–456. [Google Scholar] [CrossRef]
- Hong, C.T.; Bamodu, O.A.; Chiu, H.W.; Chiu, W.T.; Chan, L.; Chung, C.C. Personalized Predictions of Therapeutic Hypothermia Outcomes in Cardiac Arrest Patients with Shockable Rhythms Using Explainable Machine Learning. Diagnostics 2025, 15, 267. [Google Scholar] [CrossRef]
- Chung, C.C.; Su, E.C.Y.; Chen, J.H.; Chen, Y.T.; Kuo, C.Y. Xgboost-Based Simple Three-Item Model Accurately Predicts Outcomes of Acute Ischemic Stroke. Diagnostics 2023, 13, 842. [Google Scholar] [CrossRef] [PubMed]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Bamodu, O.A.; Chan, L.; Wu, C.H.; Yu, S.F.; Chung, C.C. Beyond Diagnosis: Leveraging Routine Blood and Urine Biomarkers to Predict Severity and Functional Outcome in Acute Ischemic Stroke. Heliyon 2024, 10, e26199. [Google Scholar] [CrossRef] [PubMed]
- Band, S.S.; Yarahmadi, A.; Hsu, C.-C.; Biyari, M.; Sookhak, M.; Ameri, R.; Dehzangi, I.; Chronopoulos, A.T.; Liang, H.-W. Application of Explainable Artificial Intelligence in Medical Health: A Systematic Review of Interpretability Methods. Inform. Med. Unlocked 2023, 40, 101286. [Google Scholar] [CrossRef]
- Chou, S.-Y.; Bamodu, O.A.; Chiu, W.-T.; Hong, C.-T.; Chan, L.; Chung, C.-C. Artificial Neural Network-Boosted Cardiac Arrest Survival Post-Resuscitation in-Hospital (Caspri) Score Accurately Predicts Outcome in Cardiac Arrest Patients Treated with Targeted Temperature Management. Sci. Rep. 2022, 12, 7254. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Erion, G.; Chen, H.; DeGrave, A.; Prutkin, J.M.; Nair, B.; Katz, R.; Himmelfarb, J.; Bansal, N.; Lee, S.-I. From Local Explanations to Global Understanding with Explainable Ai for Trees. Nat. Mach. Intell. 2020, 2, 56–67. [Google Scholar] [CrossRef]
- Chang, C.C.; Yeh, J.H.; Chiu, H.C.; Chen, Y.M.; Jhou, M.J.; Liu, T.C.; Lu, C.J. Utilization of Decision Tree Algorithms for Supporting the Prediction of Intensive Care Unit Admission of Myasthenia Gravis: A Machine Learning-Based Approach. J. Pers. Med. 2022, 12, 32. [Google Scholar] [CrossRef]
- Kuo, C.-Y.; Su, E.C.-Y.; Yeh, H.-L.; Yeh, J.-H.; Chiu, H.-C.; Chung, C.-C. Predictive Modeling and Interpretative Analysis of Risks of Instability in Patients with Myasthenia Gravis Requiring Intensive Care Unit Admission. Heliyon 2024, 10, e41084. [Google Scholar] [CrossRef]
- Zhong, H.; Ruan, Z.; Yan, C.; Lv, Z.; Zheng, X.; Goh, L.-Y.; Xi, J.; Song, J.; Luo, L.; Chu, L.; et al. Short-Term Outcome Prediction for Myasthenia Gravis: An Explainable Machine Learning Model. Ther. Adv. Neurol. Disord. 2023, 16, 17562864231154976. [Google Scholar] [CrossRef]
- Chang, C.C.; Yeh, J.H.; Chiu, H.C.; Liu, T.C.; Chen, Y.M.; Jhou, M.J.; Lu, C.J. Assessing the Length of Hospital Stay for Patients with Myasthenia Gravis Based on the Data Mining Mars Approach. Front Neurol. 2023, 14, 1283214. [Google Scholar] [CrossRef]
- Xu, Y.; Li, Q.; Pan, M.; Jia, X.; Wang, W.; Guo, Q.; Luan, L. Interpretable Machine Learning Models for Predicting Short-Term Prognosis in Achr-Ab+ Generalized Myasthenia Gravis Using Clinical Features and Systemic Inflammation Index. Front. Neurol. 2024, 15, 1459555. [Google Scholar] [CrossRef]
- Bershan, S.; Meisel, A.; Mergenthaler, P. Data-Driven Explainable Machine Learning for Personalized Risk Classification of Myasthenic Crisis. Int. J. Med. Inf. 2025, 194, 105679. [Google Scholar] [CrossRef]
- Heider, D.; Stetefeld, H.; Meisel, A.; Bösel, J.; Artho, M.; Linker, R.; Angstwurm, K.; Neumann, B. Polar: Prediction of Prolonged Mechanical Ventilation in Patients with Myasthenic Crisis. J. Neurol. 2024, 271, 2875–2879. [Google Scholar] [CrossRef]
- Steyaert, S.; Lootus, M.; Sarabu, C.; Framroze, Z.; Dickinson, H.; Lewis, E.; Steels, J.C.; Rinaldo, F. A Decentralized, Prospective, Observational Study to Collect Real-World Data from Patients with Myasthenia Gravis Using Smartphones. Front. Neurol. 2023, 14, 1144183. [Google Scholar] [CrossRef] [PubMed]
- Lesport, Q.; Palmie, D.; Öztosun, G.; Kaminski, H.J.; Garbey, M. Ai-Powered Telemedicine for Automatic Scoring of Neuromuscular Examinations. Bioengineering 2024, 11, 942. [Google Scholar] [CrossRef] [PubMed]
- Garbey, M.; Lesport, Q.; Girma, H.; Öztosun, G.; Abu-Rub, M.; Guidon, A.C.; Juel, V.; Nowak, R.J.; Soliven, B.; Aban, I.; et al. Application of Digital Tools and Artificial Intelligence in the Myasthenia Gravis Core Examination. Front Neurol. 2024, 15, 1474884. [Google Scholar] [CrossRef] [PubMed]
- Garbey, M.; Lesport, Q.; Girma, H.; Öztosun, G.; Kaminski, H.J. A Quantitative Study of Factors Influencing Myasthenia Gravis Telehealth Examination Score. Muscle Nerve 2025, 72, 34–41. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The Prisma 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar]
- Wolff, R.F.; Moons, K.G.; Riley, R.D.; Whiting, P.F.; Westwood, M.; Collins, G.S.; Reitsma, J.B.; Kleijnen, J.; Mallett, S. Probast: A Tool to Assess the Risk of Bias and Applicability of Prediction Model Studies. Ann. Intern. Med. 2019, 170, 51–58. [Google Scholar] [CrossRef]
- Liu, Z.; Zhu, Y.; Yuan, Y.; Yang, L.; Wang, K.; Wang, M.; Yang, X.; Wu, X.; Tian, X.; Zhang, R.; et al. 3d Densenet Deep Learning Based Preoperative Computed Tomography for Detecting Myasthenia Gravis in Patients with Thymoma. Front. Oncol. 2021, 11, 631964. [Google Scholar] [CrossRef]
- Ozkan, E.; Orhan, K.; Soydal, C.; Kahya, Y.; Tunc, S.S.; Celik, O.; Sak, S.D.; Cangir, A.K. Combined Clinical and Specific Positron Emission Tomography/Computed Tomography-Based Radiomic Features and Machine-Learning Model in Prediction of Thymoma Risk Groups. Nucl. Med. Commun. 2022, 43, 529–539. [Google Scholar] [CrossRef]
- Liu, W.; Wang, W.; Guo, R.; Zhang, H.; Guo, M. Deep Learning for Risk Stratification of Thymoma Pathological Subtypes Based on Preoperative Ct Images. BMC Cancer 2024, 24, 651. [Google Scholar] [CrossRef] [PubMed]
- Abgrall, G.; Holder, A.L.; Chelly Dagdia, Z.; Zeitouni, K.; Monnet, X. Should Ai Models Be Explainable to Clinicians? Crit. Care 2024, 28, 301. [Google Scholar] [CrossRef]
- Gonzalez, F.A.; Santonocito, C.; Lamas, T.; Costa, P.; Vieira, S.M.; Ferreira, H.A.; Sanfilippo, F. Is Artificial Intelligence Prepared for the 24-H Shifts in the Icu? Anaesth. Crit. Care Pain Med. 2024, 43, 101431. [Google Scholar] [CrossRef] [PubMed]
- Shamsutdinova, D.; Stamate, D.; Stahl, D. Balancing Accuracy and Interpretability: An R Package Assessing Complex Relationships Beyond the Cox Model and Applications to Clinical Prediction. Int. J. Med. Inform. 2025, 194, 105700. [Google Scholar] [CrossRef] [PubMed]
- Cutillo, C.M.; Sharma, K.R.; Foschini, L.; Kundu, S.; Mackintosh, M.; Mandl, K.D. Machine Intelligence in Healthcare-Perspectives on Trustworthiness, Explainability, Usability, and Transparency. npj Digit. Med. 2020, 3, 47. [Google Scholar] [CrossRef]
- Alshekhlee, A.; Miles, J.D.; Katirji, B.; Preston, D.C.; Kaminski, H.J. Incidence and Mortality Rates of Myasthenia Gravis and Myasthenic Crisis in Us Hospitals. Neurology 2009, 72, 1548–1554. [Google Scholar] [CrossRef]
- Kalita, J.; Kohat, A.K.; Misra, U.K. Predictors of Outcome of Myasthenic Crisis. Neurol. Sci. 2014, 35, 1109–1114. [Google Scholar] [CrossRef]
- Liu, F.; Wang, Q.; Chen, X. Myasthenic Crisis Treated in a Chinese Neurological Intensive Care Unit: Clinical Features, Mortality, Outcomes, and Predictors of Survival. BMC Neurol. 2019, 19, 172. [Google Scholar] [CrossRef]
- Nelke, C.; Stascheit, F.; Eckert, C.; Pawlitzki, M.; Schroeter, C.B.; Huntemann, N.; Mergenthaler, P.; Arat, E.; Öztürk, M.; Foell, D.; et al. Independent Risk Factors for Myasthenic Crisis and Disease Exacerbation in a Retrospective Cohort of Myasthenia Gravis Patients. J. Neuroinflammation 2022, 19, 89. [Google Scholar] [CrossRef]
- Rajkomar, A.; Oren, E.; Chen, K.; Dai, A.M.; Hajaj, N.; Hardt, M.; Liu, P.J.; Liu, X.; Marcus, J.; Sun, M.; et al. Scalable and Accurate Deep Learning with Electronic Health Records. npj Digit. Med. 2018, 1, 18. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Rao, S.; Solares, J.R.A.; Hassaine, A.; Ramakrishnan, R.; Canoy, D.; Zhu, Y.; Rahimi, K.; Salimi-Khorshidi, G. Behrt: Transformer for Electronic Health Records. Sci. Rep. 2020, 10, 7155. [Google Scholar] [CrossRef] [PubMed]
- Ruiter, A.M.; Verschuuren, J.J.G.M.; Tannemaat, M.R. Fatigue in Patients with Myasthenia Gravis. A Systematic Review of the Literature. Neuromuscul. Disord. 2020, 30, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Marbin, D.; Piper, S.K.; Lehnerer, S.; Harms, U.; Meisel, A. Mental Health in Myasthenia Gravis Patients and Its Impact on Caregiver Burden. Sci. Rep. 2022, 12, 19275. [Google Scholar] [CrossRef]
- Gelinas, D.; Parvin-Nejad, S.; Phillips, G.; Cole, C.; Hughes, T.; Silvestri, N.; Govindarajan, R.; Jefferson, M.; Campbell, J.; Burnett, H. The Humanistic Burden of Myasthenia Gravis: A Systematic Literature Review. J. Neurol. Sci. 2022, 437, 120268. [Google Scholar] [CrossRef]
- Severcan, F.; Ozyurt, I.; Dogan, A.; Severcan, M.; Gurbanov, R.; Kucukcankurt, F.; Elibol, B.; Tiftikcioglu, I.; Gursoy, E.; Yangin, M.N.; et al. Decoding Myasthenia Gravis: Advanced Diagnosis with Infrared Spectroscopy and Machine learning. Sci. Rep. 2024, 14, 19316. [Google Scholar] [CrossRef]
- Ruiter, A.M.; Wang, Z.; Yin, Z.; Naber, W.C.; Simons, J.; Blom, J.T.; van Gemert, J.C.; Verschuuren, J.J.G.M.; Tannemaat, M.R. Assessing Facial Weakness in Myasthenia Gravis with Facial Recognition Software and Deep Learning. Ann. Clin. Transl. Neurol. 2023, 10, 1314–1325. [Google Scholar] [CrossRef]
- Zhou, G.; Wang, S.; Lin, L.; Lu, K.; Lin, Z.; Zhang, Z.; Zhang, Y.; Cheng, D.; Szeto, K.; Peng, R.; et al. Screening for Immune-Related Biomarkers Associated with Myasthenia Gravis and Dilated Cardiomyopathy Based on Bioinformatics Analysis and Machine Learning. Heliyon 2024, 10, e28446. [Google Scholar] [CrossRef]
- Liu, H.; Liu, G.; Guo, R.; Li, S.; Chang, T. Identification of Potential Key Genes for the Comorbidity of Myasthenia Gravis with Thymoma by Integrated Bioinformatics Analysis and Machine Learning. Bioinform. Biol. Insights 2024, 18, 11779322241281652. [Google Scholar] [CrossRef]
- Sha, Q.; Zhang, Z.; Li, H.; Xu, Y.; Wang, J.; Du, A. Serum Metabolomic Profile of Myasthenia Gravis and Potential Values as Biomarkers in Disease Monitoring. Clin. Chim. Acta 2024, 562, 119873. [Google Scholar] [CrossRef]
- Chang, C.C.; Liu, T.C.; Lu, C.J.; Chiu, H.C.; Lin, W.N. Explainable Machine Learning Model for Identifying Key Gut Microbes Metabolites Biomarkers Associated with Myasthenia Gravis. Comput. Struct. Biotechnol. J. 2024, 23, 1572–1583. [Google Scholar] [CrossRef]
- Zhdanava, M.; Pesa, J.; Boonmak, P.; Schwartzbein, S.; Cai, Q.; Pilon, D.; Choudhry, Z.; Lafeuille, M.-H.; Lefebvre, P.; Souayah, N. Predictors of High Healthcare Cost among Patients with Generalized Myasthenia Gravis: A Combined Machine Learning and Regression Approach from a Us Payer Perspective. Appl. Health Econ. Health Policy 2024, 22, 735–747. [Google Scholar] [CrossRef]

| Author (Year) [Ref.] | Study Design | Region/Center Type | Sample Size | Prediction Target | No. of Input Features | Representative Features | Best-Performing Model (Comparators) | Validation Strategy | Performance | Interpretability Method | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chang et al. (2022) [17] | Retrospective | Taiwan/Single-center | 228 | ICU admission | 20 | MGFA, thymoma, azathioprine, disease duration, sex, onset age | Decision Tree C5.0 (CART, C4.5, LR) | Cross-validation (10-fold) | AUC 0.814 | Decision rules | ICU admission rules via decision tree |
| Kuo et al. (2024) [18] | Retrospective | Taiwan/Single-center | 314 | ICU admission | 14 | MGFA, thymectomy, disease duration, age | XGBoost (LR, SVM, random forest) | Cross-validation, calibration (10-fold) | AUC 0.894 | SHAP | Calibration plot, Brier score |
| Zhong et al. (2023) [19] | Retrospective | China/Multicenter | 890 | PIS at 6-month | 25 | QMG: left arm outstretch, corticosteroid, QMG: ptosis, antibody | Random Forest | External validation (independent cohort) | AUC 0.84 (improved), 0.74 (unchanged), 0.79 (worse) | SHAP | Online prediction tool |
| Chang et al. (2023) [20] | Retrospective | Taiwan/Single-center | 196 | Length of hospital stay | 18 | Disease duration, age, MGFA, daily prednisolone dose | MARS (Lasso MLR, CART, random forest) | Cross-validation (10-fold) | MAPE: 0.524, SMAPE: 0.409, RAE: 1.133 | Variable thresholds | Continuous outcome |
| Xu et al. (2024) [21] | Retrospective | China/Multicenter | 202 | PIS at 6-month | 8 | SII, NLR, disease duration, PLR, QMG score | XGBoost (LR, SVM, random forest) | External validation (independent cohort) | AUC 0.944 (internal) AUC 0.908 (external) | SHAP | AChR-Ab+ subgroup |
| Steyaert et al. (2023) [24] | Prospective observational | USA/Decentralized virtual study (multi-state) | 82 | Symptom exacerbation subtype clustering | 40 (18 static, 22 longitudinal) | Daily step count, MG-ADL symptom scores, medication group, time since diagnosis | K-means clustering | Cluster selection via elbow method | N/A (unsupervised; not benchmarked against outcomes) | Cluster profiling via random forest; PCA visualization | Smartphone-based digital phenotyping |
| Bershan et al. (2025) [22] | Pseudo-prospective | Germany/Single-center | 51 | Myasthenic crisis | 79 | Creatinine trend, lymphocyte variability, hospitalization trajectory | Random forest (Lasso regression) | Repeated holdout (100 runs) | AUC 0.765 | Feature stability, contribution maps | Open-source code |
| Heider et al. (2024) [23] | Retrospective | Germany/Multicenter | 195 | Prolonged mechanical ventilation (>15 days) | 9 (after Ensemble Feature Selection) | Age, comorbidities, late-onset MG, MGFA IVb, delirium, pneumonia, CPR | Logistic regression (no comparator) | 10 × 10-fold cross-validation | AUC 0.78 | Ensemble Feature Selection | Web-based prediction tool (POLAR) |
| Lesport et al. (2024) [25] | Algorithm development | USA/Single center | 51 | MG-CE scoring automation via AI | Not reported | Eye/body motion, NLP-based vocalization features | AI-based pipeline (no comparator) | Not reported | No formal metric reported | None | Proposed telemedicine scoring enhancement |
| Garbey et al. (2024) [26] | Prospective observational | USA/Single center | 51 MG, 15 controls | AI-assisted MG-CE quantification | Not reported | Lid and eye position, arm movement, breath count, vocalization/NLP | Custom AI pipeline (Computer Vision + NLP) | Repeated video recordings on separate days | No formal metric reported | None | Cheek puff limited; lighting and camera angle issues |
| Garbey et al. (2025) [27] | Prospective observational | USA/Single center | 51 | Reproducibility and variability in MG-CE and MG-ADL | Not reported | Eye motion, speech, examiner instruction | AI-based analysis pipeline (no comparator) | Inter-rater comparison | Up to 25% scoring variation | None | Variability attributed to instruction and technical limitations |
| Study (First Author, Year [Ref.]) | Participants | Predictors | Outcome | Analysis | Overall Risk of Bias | Applicability Concerns |
|---|---|---|---|---|---|---|
| Chang, 2022 [17] | High | High | Low | High | High | High |
| Kuo, 2024 [18] | High | Low | Low | High | High | High |
| Zhong, 2023 [19] | Low | Low | Low | Low | Low | Low |
| Chang, 2023 [20] | High | High | High | High | High | High |
| Xu, 2024 [21] | Low | Low | Low | Low | Low | Low |
| Steyaert, 2023 [24] | High | High | Not Applicable | High | High | High |
| Bershan, 2025 [22] | High | High | Low | High | High | High |
| Heider, 2024 [23] | Low | Low | Low | Low | Low | Low |
| Lesport, 2024 [25] | High | High | Not Applicable | High | High | High |
| Garbey, 2024 [26] | High | High | Not Applicable | High | High | High |
| Garbey, 2025 [27] | High | High | Not Applicable | High | High | High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chung, C.-C.; Wu, I.-C.; Bamodu, O.A.; Hong, C.-T.; Chiu, H.-C. Machine Learning in Myasthenia Gravis: A Systematic Review of Prognostic Models and AI-Assisted Clinical Assessments. Diagnostics 2025, 15, 2044. https://doi.org/10.3390/diagnostics15162044
Chung C-C, Wu I-C, Bamodu OA, Hong C-T, Chiu H-C. Machine Learning in Myasthenia Gravis: A Systematic Review of Prognostic Models and AI-Assisted Clinical Assessments. Diagnostics. 2025; 15(16):2044. https://doi.org/10.3390/diagnostics15162044
Chicago/Turabian StyleChung, Chen-Chih, I-Chieh Wu, Oluwaseun Adebayo Bamodu, Chien-Tai Hong, and Hou-Chang Chiu. 2025. "Machine Learning in Myasthenia Gravis: A Systematic Review of Prognostic Models and AI-Assisted Clinical Assessments" Diagnostics 15, no. 16: 2044. https://doi.org/10.3390/diagnostics15162044
APA StyleChung, C.-C., Wu, I.-C., Bamodu, O. A., Hong, C.-T., & Chiu, H.-C. (2025). Machine Learning in Myasthenia Gravis: A Systematic Review of Prognostic Models and AI-Assisted Clinical Assessments. Diagnostics, 15(16), 2044. https://doi.org/10.3390/diagnostics15162044






