Point-of-Care Ultrasound Within One Hour Associated with ED Flow and Resource Use in Non-Traumatic Abdominal Pain: A Retrospective Observational Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Setting and Population
2.3. Variables
2.4. Outcome Measures
2.5. Data Analyses
3. Results
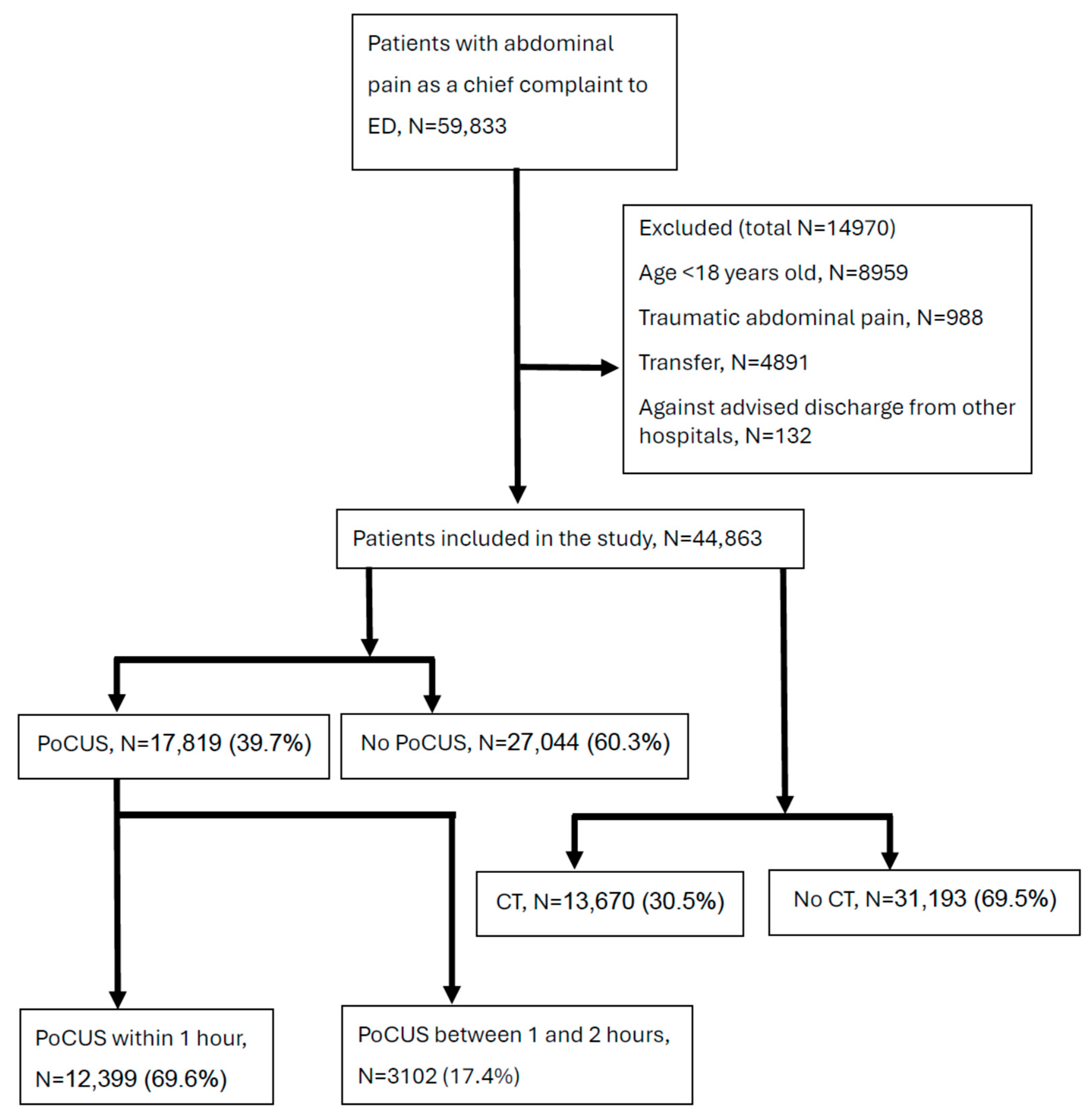
3.1. Population Distribution
3.2. Baseline Demographics
3.3. Impact of PoCUS Timing on ED LOS and Costs
3.4. Quality of Care with POCUS
4. Discussion
4.1. PoCUS Utilization Patterns
4.2. The Association of PoCUS with ED Patient Flow and Resource Utilization
4.3. Quality of Care and Patient Safety
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Kocher, K.E.; Meurer, W.J.; Fazel, R.; Scott, P.A.; Krumholz, H.M.; Nallamothu, B.K. National trends in use of computed tomography in the emergency department. Ann. Emerg. Med. 2011, 58, 452–462.e453. [Google Scholar] [CrossRef]
- Karcioglu, O.; Yenocak, S.; Hosseinzadeh, M.; Sezgin, S.B. Abdominal Pain: Essential Diagnosis and Management in Acute Medicine; Bentham Science Publishers: Singapore, 2022. [Google Scholar]
- Brachet-Contul, R.; Cinti, L.; Nardi, M.J.; Condurro, S.; Millo, P.; Marrelli, D. Non-specific Abdominal Pain. In Emergency Laparoscopic Surgery in the Elderly and Frail Patient; Springer: Berlin/Heidelberg, Germany, 2021; pp. 121–127. [Google Scholar]
- Mazzei, M.A.; Guerrini, S.; Cioffi Squitieri, N.; Cagini, L.; Macarini, L.; Coppolino, F.; Giganti, M.; Volterrani, L. The role of US examination in the management of acute abdomen. Crit. Ultrasound J. 2013, 5, S6. [Google Scholar] [CrossRef] [PubMed]
- Marincek, B. Nontraumatic abdominal emergencies: Acute abdominal pain: Diagnostic strategies. Eur. Radiol. 2002, 12, 2136–2150. [Google Scholar] [CrossRef] [PubMed]
- Gans, S.L.; Pols, M.A.; Stoker, J.; Boermeester, M.A.; Group, E.S. Guideline for the diagnostic pathway in patients with acute abdominal pain. Dig. Surg. 2015, 32, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Mills, A.M.; Baumann, B.M.; Chen, E.H.; Zhang, K.-Y.; Glaspey, L.J.; Hollander, J.E.; Pines, J.M. The Impact of Crowding on Time until Abdominal CT Interpretation in Emergency Department Patients with Acute Abdominal Pain. Postgrad. Med. 2010, 122, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.T. Counter-Point: Are we really ordering too many CT scans? West. J. Emerg. Med. 2008, 9, 120. [Google Scholar] [PubMed]
- Spampinato, M.D.; Luppi, F.; Cristofaro, E.; Benedetto, M.; Cianci, A.; Bachechi, T.; Ghirardi, C.; Perna, B.; Guarino, M.; Passaro, A.; et al. Diagnostic accuracy of Point of Care UltraSound (POCUS) in clinical practice: A retrospective, emergency department based study. J. Clin. Ultrasound 2024, 52, 255–264. [Google Scholar] [CrossRef]
- Diaz-Gomez, J.L.; Mayo, P.H.; Koenig, S.J. Point-of-care ultrasonography. N. Engl. J. Med. 2021, 385, 1593–1602. [Google Scholar] [CrossRef]
- Wu, X.; Li, K.; Kou, S.; Wu, X.; Zhang, Z. The accuracy of point-of-care ultrasound in the detection of gallbladder disease: A meta-analysis. Acad. Radiol. 2024, 31, 1336–1343. [Google Scholar] [CrossRef]
- Lee, W.; Goh, S.; Lee, B.; Juan, S.; Asinas-Tan, M.; Lim, B. Renal point-of-care ultrasound performed by ED staff with limited training and 30-day outcomes in patients with renal colic. Can. J. Emerg. Med. 2024, 26, 198–203. [Google Scholar] [CrossRef]
- Van Oyen, A.; Tamirian, R.; Tay, E. 30 Point-of-Care Ultrasound by Emergency Physicians for the Diagnosis of Ectopic Pregnancies: How Good Are We? Ann. Emerg. Med. 2024, 84, S14. [Google Scholar] [CrossRef]
- Recker, F.; Weber, E.; Strizek, B.; Gembruch, U.; Westerway, S.C.; Dietrich, C.F. Point-of-care ultrasound in obstetrics and gynecology. Arch. Gynecol. Obstet. 2021, 303, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.-H.; Chen, J.-Y.; Ling, D.-A.; Lee, A.-F.; Ko, Y.-C.; Lien, W.-C.; Huang, C.-H. Earlier point-of-care ultrasound, shorter length of stay in patients with acute flank pain. Scand. J. Trauma Resusc. Emerg. Med. 2022, 30, 29. [Google Scholar] [CrossRef] [PubMed]
- Barton, M.F.; Barton, K.M.; Goldsmith, A.J.; Gottlieb, M.; Harris, C.; Chottiner, M.; Barton, B.L.; Selame, L.; Baugh, C.W.; Duggan, N.M. POCUS-first in acute diverticulitis: Quantifying cost savings, length-of-stay reduction. Am. J. Emerg. Med. 2025, 88, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Brower, C.H.; Baugh, C.W.; Shokoohi, H.; Liteplo, A.S.; Duggan, N.; Havens, J.; Askari, R.; Rehani, M.M.; Kapur, T.; Goldsmith, A.J. Point-of-care ultrasound-first for the evaluation of small bowel obstruction: National cost savings, length of stay reduction, and preventable radiation exposure. Acad. Emerg. Med. 2022, 29, 824–834. [Google Scholar] [CrossRef]
- Lau, H.T.; Liu, W.; Lam, V.; Pang, T. Early routine (erCT) versus selective computed tomography (sCT) for acute abdominal pain: A systematic review and meta-analysis of randomised trials. Int. J. Surg. 2022, 101, 106622. [Google Scholar] [CrossRef]
- Juvonen, P.; Lehtimäki, T.; Eskelinen, M.; Ilves, I.; Vanninen, R.; Miettinen, P.; Paajanen, H. The need for surgery in acute abdominal pain: A randomized study of abdominal computed tomography. Vivo 2014, 28, 305–309. [Google Scholar]
- Andersen, C.A.; Holden, S.; Vela, J.; Rathleff, M.S.; Jensen, M.B. Point-of-care ultrasound in general practice: A systematic review. Ann. Fam. Med. 2019, 17, 61–69. [Google Scholar] [CrossRef]
- Di Serafino, M.; Iacobellis, F.; Schillirò, M.L.; D’auria, D.; Verde, F.; Grimaldi, D.; Dell’Aversano Orabona, G.; Caruso, M.; Sabatino, V.; Rinaldo, C. Common and uncommon errors in emergency ultrasound. Diagnostics 2022, 12, 631. [Google Scholar] [CrossRef]
- Huang, C.-T.; Wang, L.-W.; Lin, S.-Y.; Chen, T.-Y.; Ho, Y.-J.; Wang, P.-H.; Liu, K.-L.; Wu, Y.-M.; Wang, H.-P.; Lien, W.-C. Impact of a POCUS-first versus CT-first approach on emergency department length of stay and time to surgical consultation in patients with acute cholecystitis: A retrospective study. Scand. J. Trauma Resusc. Emerg. Med. 2025, 33, 28. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Graham, K.L.; Auerbach, A.D.; Schnipper, J.L.; Flanders, S.A.; Kim, C.S.; Robinson, E.J.; Ruhnke, G.W.; Thomas, L.R.; Kripalani, S.; Vasilevskis, E.E. Preventability of early versus late hospital readmissions in a national cohort of general medicine patients. Ann. Intern. Med. 2018, 168, 766–774. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.-J.; Yen, Z.-S.; Tsai, J.C.-H.; Chen, L.C.; Lin, S.J.; Sang, Y.Y.; Chen, J.-C.; Group, T.N.W. Validation of the Taiwan triage and acuity scale: A new computerised five-level triage system. Emerg. Med. J. 2011, 28, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Alfoti, B.O.O.; Alfoti, F.O.O.; Alothman, S.T.H.; Al-Dhafiri, T.M.A.; Al-Harbi, N.H.M.; Al-Khalidi, A.M.; Alzahrany, N.D.B.; Abutalib, F.M.; Almojam, S.A.; Al-Hayani, S.A. Utilization of Point-of-Care Ultrasound (POCUS) in Emergency and Critical Care: Role of Nursing for Enhancing Diagnostic Accuracy and Efficiency-Systematic Review. Egypt. J. Chem. 2024, 67, 705–716. [Google Scholar] [CrossRef]
- Manasievska, M. Combined Approach with Point-of-Care Ultrasound in Emergency Medicine: Methodological Aspects and Clinical Impact. 2021. Available online: https://iris.unito.it/bitstream/2318/2017275/2/Thesis_M.pdf (accessed on 19 June 2025).
- Boling, B.; Solis, A. Point-of-care ultrasonography in the critical care setting: Abdominal POCUS. AACN Adv. Crit. Care 2023, 34, 216–227. [Google Scholar] [CrossRef]
- Di Saverio, S.; Birindelli, A.; Kelly, M.D.; Catena, F.; Weber, D.G.; Sartelli, M.; Sugrue, M.; De Moya, M.; Gomes, C.A.; Bhangu, A. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J. Emerg. Surg. 2016, 11, 34. [Google Scholar]
- Reinoso-Párraga, P.P.; González-Montalvo, J.I.; Menéndez-Colino, R.; Perkisas, S.; Rivera-Deras, I.; Garmendia-Prieto, B.; Arain, S.J.; Tung-Chen, Y.; Vilches-Moraga, A. Usefulness of point of care ultrasound in older adults: A multicentre study across different geriatric care settings in Spain and the United Kingdom. Age Ageing 2024, 53, afae165. [Google Scholar] [CrossRef] [PubMed]
- Cortellaro, F.; Perani, C.; Guarnieri, L.; Ferrari, L.; Cazzaniga, M.; Maconi, G.; Wu, M.A.; Aseni, P. Point-of-care ultrasound in the diagnosis of acute abdominal pain. In Operative Techniques and Recent Advances in Acute Care and Emergency Surgery; Springer: Berlin/Heidelberg, Germany, 2019; pp. 383–401. [Google Scholar]
- Andersen, C.A.; Brodersen, J.B.; Graumann, O.; Davidsen, A.S.; Jensen, M.B. Factors affecting point-of-care ultrasound implementation in general practice: A survey in Danish primary care clinics. BMJ Open 2023, 13, e077702. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Abu-Zidan, F.M. Point-of-care ultrasound for the acute abdomen in the primary health care. Turk. J. Emerg. Med. 2020, 20, 1–11. [Google Scholar]
- Smith, C.J.; Barron, K.; Shope, R.J.; Beam, E.; Piro, K. Motivations, barriers, and professional engagement: A multisite qualitative study of internal medicine faculty’s experiences learning and teaching point-of-care ultrasound. BMC Med. Educ. 2022, 22, 171. [Google Scholar] [CrossRef]
- Beals, T.; Naraghi, L.; Grossestreuer, A.; Schafer, J.; Balk, D.; Hoffmann, B. Point of care ultrasound is associated with decreased ED length of stay for symptomatic early pregnancy. Am. J. Emerg. Med. 2019, 37, 1165–1168. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, A.J.; Shokoohi, H.; Loesche, M.; Patel, R.C.; Kimberly, H.; Liteplo, A. Point-of-care Ultrasound in Morbidity and Mortality Cases in Emergency Medicine: Who Benefits the Most? West J. Emerg. Med. 2020, 21, 172–178. [Google Scholar] [CrossRef]
- Blanco, P.; Volpicelli, G. Common pitfalls in point-of-care ultrasound: A practical guide for emergency and critical care physicians. Crit. Ultrasound J. 2016, 8, 15. [Google Scholar] [CrossRef]
- Nuñez, S.; Hexdall, A.; Aguirre-Jaime, A. Unscheduled returns to the emergency department: An outcome of medical errors? Qual. Saf. Health Care 2006, 15, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Sauvin, G.; Freund, Y.; Saïdi, K.; Riou, B.; Hausfater, P. Correction: Unscheduled return visits to the emergency department: Consequences for triage. Acad. Emerg. Med. 2013, 20, E3–E9. [Google Scholar] [CrossRef]
- Verelst, S.; Pierloot, S.; Desruelles, D.; Gillet, J.-B.; Bergs, J. Short-term Unscheduled Return Visits of Adult Patients to the Emergency Department. J. Emerg. Med. 2014, 47, 131–139. [Google Scholar] [CrossRef]
- Pham, J.C.; Kirsch, T.D.; Hill, P.M.; DeRuggerio, K.; Hoffmann, B. Seventy-two-hour returns may not be a good indicator of safety in the emergency department: A national study. Acad. Emerg. Med. 2011, 18, 390–397. [Google Scholar] [CrossRef]
- Sabbatini, A.K.; Kocher, K.E.; Basu, A.; Hsia, R.Y. In-Hospital Outcomes and Costs Among Patients Hospitalized During a Return Visit to the Emergency Department. JAMA 2016, 315, 663–671. [Google Scholar] [CrossRef]
- Tsai, C.-L.; Ling, D.-A.; Lu, T.-C.; Lin, J.C.-C.; Huang, C.-H.; Fang, C.-C. Inpatient outcomes following a return visit to the emergency department: A nationwide cohort study. West. J. Emerg. Med. 2021, 22, 1124. [Google Scholar] [CrossRef]
- Chen, R.-F.; Cheng, K.-C.; Lin, Y.-Y.; Chang, I.-C.; Tsai, C.-H. Predicting unscheduled emergency department return visits among older adults: Population-based retrospective study. JMIR Med. Inform. 2021, 9, e22491. [Google Scholar] [CrossRef]
- Rising, K.L.; Padrez, K.A.; O’Brien, M.; Hollander, J.E.; Carr, B.G.; Shea, J.A. Return visits to the emergency department: The patient perspective. Ann. Emerg. Med. 2015, 65, 377–386.e3. [Google Scholar] [CrossRef] [PubMed]
- Brau, F.; Papin, M.; Batard, E.; Abet, E.; Frampas, E.; Le Thuaut, A.; Montassier, E.; Le Bastard, Q.; Le Conte, P. Impact of emergency physician performed ultrasound in the evaluation of adult patients with acute abdominal pain: A prospective randomized bicentric trial. Scand. J. Trauma Resusc. Emerg. Med. 2024, 32, 15. [Google Scholar] [CrossRef] [PubMed]
- Boendermaker, A.E.; Coolsma, C.W.; Emous, M.; Ter Avest, E. Efficacy of scheduled return visits for emergency department patients with non-specific abdominal pain. Emerg. Med. J. 2018, 35, 499–506. [Google Scholar] [CrossRef] [PubMed]
| PoCUS, N = 17,819 | No PoCUS, N = 27,044 | p | |
|---|---|---|---|
| Age | 42.91 ± 17.80 | 45.42 ± 19.56 | <0.001 |
| Sex | <0.001 | ||
| Male | 6497 (36.46) | 10,905 (40.32) | |
| Female | 11,322 (63.54) | 16,139 (59.68) | |
| BMI | 24.11 ± 24.98 | 24.16 ± 37.70 | 0.855 |
| Triage | <0.001 | ||
| 1 | 104 (0.58) | 340 (1.26) | |
| 2 | 1684 (9.45) | 3555 (13.15) | |
| 3 | 15,750 (88.39) | 22,464 (83.06) | |
| 4 | 279 (1.57) | 634 (2.34) | |
| 5 | 2 (0.01) | 51 (0.19) | |
| Heart rate | 87.43 ± 17.29 | 91.55 ± 18.37 | |
| Systolic blood pressure | 130.2 ± 23.93 | 128.3 ± 23.46 | |
| Diastolic blood pressure | 80.67 ± 14.61 | 79.39 ± 14.43 | |
| Body temperature | 36.64 ± 0.68 | 36.73 ± 0.88 | |
| Respiratory rate | 19.47 ± 1.56 | 19.58 ± 1.60 | |
| CT | 5086 (28.54) | 8584 (31.74) | <0.001 |
| Discharged with OPD | 13,791 (77.39) | 18,456 (68.24) | <0.001 |
| Admission to ward | 2406 (13.50) | 5324 (19.69) | <0.001 |
| Admission to ICU | 69 (0.39) | 168 (0.62) | <0.001 |
| Expire in ED | 1 (0.01) | 20 (0.07) | 0.001 |
| ED LOS | 5.11 ± 7.12 | 6.24 ± 9.52 | <0.001 |
| Hospital LOS | 7.55 ± 10.90 | 9.40 ± 12.88 | <0.001 |
| Whole Population, N = 44,863 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No PoCUS | PoCUS | p | No PoCUS | PoCUS Within 1 h | p | No PoCUS | PoCUS Between 1 and 2 h | p | |
| OPD, N = 32,247 | 18,456 | 13,791 | 18,456 | 9743 | 18,456 | 2403 | |||
| LOS in ED (h) | 3.80 ± 5.77 | 3.74 ± 4.60 | 0.282 | 3.80 ± 5.77 | 3.33 ± 3.92 | <0.001 | 3.80 ± 5.77 | 3.82 ± 4.38 | 0.849 |
| Costs in ED (NT$) | 4367.9 ± 4216.2 | 4918.9 ± 3931.7 | <0.001 | 4367.9 ± 4216.2 | 4657.2 ± 3738.8 | <0.001 | 4367.9 ± 4216.2 | 5157.2 ± 4240.9 | <0.001 |
| Admission to ward (no ICU), N = 7730 | 5324 | 2406 | 5324 | 1542 | 5324 | 437 | |||
| LOS in ED (h) | 16.13 ± 14.56 | 14.78 ± 13.03 | <0.001 | 16.13 ± 14.56 | 13.28 ± 11.76 | <0.001 | 16.13 ± 14.56 | 16.26 ± 13.75 | 0.857 |
| Costs in ED (NT$) | 13,221.1 ± 9812.8 | 13,064.6 ± 9515.9 | 0.512 | 1322.1 ± 9812.8 | 12,820.6 ± 9169.8 | 0.137 | 13,221.1 ± 9812.8 | 13,571.4 ± 10,002.0 | 0.473 |
| Admission to ICU, N = 237 | 168 | 69 | 168 | 43 | 168 | 15 | |||
| LOS in ED (h) | 12.94 ± 13.26 | 16.40 ± 16.01 | 0.087 | 12.94 ± 13.26 | 13.32 ± 14.03 | 0.869 | 12.94 ± 13.26 | 15.59 ± 15.64 | 0.466 |
| Costs in ED (NT$) | 33,873.2 ± 36,233.5 | 33,246.1 ± 30,747.5 | 0.899 | 33,873.2 ± 36,233.5 | 26,144.8 ± 19,990.3 | 0.064 | 33,873.2 ± 36,233.5 | 32,197.0 ± 30,001.0 | 0.862 |
| Without CT, N = 31,193 | |||||||||
| No POCUS | POCUS | p | No POCUS | POCUS within 1 h | p | No POCUS | POCUS above 1 h | p | |
| OPD, N = 26,008 | 14,857 | 11,151 | 14,857 | 7865 | 14,857 | 1987 | |||
| LOS in ED (h) | 3.16 ± 5.27 | 3.12 ± 4.09 | 0.577 | 3.16 ± 5.27 | 2.79 ± 3.43 | <0.001 | 3.16 ± 5.27 | 3.14 ± 3.65 | 0.901 |
| Costs in ED (NT$) | 2906.6 ± 2864.2 | 3576.8 ± 2675.2 | <0.001 | 2906.6 ± 2864.2 | 3320.9 ± 2431.2 | <0.001 | 2906.6 ± 2864.2 | 3899.5 ± 3034.0 | <0.001 |
| Admission to ward (no ICU), N = 2179 | 1546 | 633 | 1546 | 357 | 1546 | 119 | |||
| LOS in ED (h) | 14.66 ± 14.66 | 12.91 ± 12.11 | 0.004 | 14.66 ± 14.66 | 10.52 ± 10.26 | <0.001 | 14.66 ± 14.66 | 14.89 ± 13.09 | 0.866 |
| Costs in ED (NT$) | 8303.4 ± 7860.9 | 7092.4 ± 6242.9 | <0.001 | 8303.4 ± 7860.9 | 6469.9 ± 5682.0 | <0.001 | 8303.4 ± 7860.9 | 7397.9 ± 7184.8 | 0.223 |
| Admission to ICU, N = 41 | 33 | 8 | 33 | 5 | 33 | 1 | |||
| LOS in ED (h) | 7.84 ± 10.10 | 12.09 ± 10.96 | 0.299 | 7.84 ± 10.10 | 6.90 ± 5.39 | 0.841 | 7.84 ± 10.10 | 25.00 ± 0.00 | - |
| Costs in ED (NT$) | 30,935.5 ± 37,952.3 | 30,410.1 ± 57,536.8 | 0.974 | 30,935.5 ± 37,952.3 | 8796.6 ± 4089.2 | 0.002 | 30,935.5 ± 37,952.3 | 3977.0 ± 0.00 | - |
| With CT, N = 13,670 | |||||||||
| No POCUS | POCUS | p | No POCUS | POCUS within 1 h | p | No POCUS | POCUS above 1 h | p | |
| OPD, N = 6239 | 3599 | 2640 | 3599 | 1878 | 3599 | 416 | |||
| LOS in ED (h) | 6.48 ± 6.85 | 6.35 ± 5.62 | 0.425 | 6.48 ± 6.85 | 5.62 ± 4.89 | <0.001 | 6.48 ± 6.85 | 7.06 ± 5.87 | 0.060 |
| Costs in ED (NT$) | 10,400.3 ± 3476.8 | 10,587.9 ± 3282.9 | 0.029 | 10,400.3 ± 3476.8 | 10,253.4 ± 2995.3 | 0.103 | 10,400.3 ± 3476.8 | 11,164.4 ± 4037.2 | <0.001 |
| Admission to ward (no ICU), N = 5551 | 3778 | 1773 | 3778 | 1185 | 3778 | 318 | |||
| LOS in ED (h) | 16.73 ± 14.48 | 15.44 ± 13.28 | 0.001 | 16.73 ± 14.48 | 14.11 ± 12.05 | <0.001 | 16.73 ± 14.48 | 16.77 ± 13.97 | 0.962 |
| Costs in ED (NT$) | 15,233.5 ± 9822.4 | 15,196.9 ± 9576.5 | 0.896 | 15,233.5 ± 9822.4 | 14,733.8 ± 9160.1 | 0.107 | 15,233.5 ± 9822.4 | 15,881.6 ± 9935.7 | 0.259 |
| Admission to ICU, N = 196 | 135 | 61 | 135 | 38 | 135 | 14 | |||
| LOS in ED (h) | 14.19 ± 13.67 | 16.96 ± 16.54 | 0.219 | 14.19 ± 13.67 | 14.16 ± 14.63 | 0.992 | 14.19 ± 13.67 | 14.91 ± 16.01 | 0.852 |
| Costs in ED (NT$) | 34,591.3 ± 35,910.6 | 33,618.0 ± 26,153.8 | 0.831 | 34,591.3 ± 35,910.6 | 28,427.4 ± 20,144.1 | 0.173 | 34,591.3 ± 35,910.6 | 34,212.7 ± 30,060.9 | 0.969 |
| Admission After Index Visit, N = 7967 | PoCUS Within 1 h Alone at Index Visit and Admitted After an Unscheduled Return Visit, N = 110 | p-Value | |
|---|---|---|---|
| LOS in ED 1st (h) | 15.66 ± 14.12 | 3.25 ± 3.02 | <0.001 |
| LOS in ED 2nd (h) | N/A | 13.05 ± 11.48 | - |
| Total LOS in ED | 15.66 ± 14.12 | 16.30 ± 11.83 | 0.571 |
| ED 1st cost (NT$) | 13,782.8 ± 11,808.3 | 3166.6 ± 1560.2 | <0.001 |
| ED 2nd cost (NT$) | N/A | 10,889.3 ± 8212.6 | - |
| Admission cost (NT$) | 100,911 ± 261,456 | 51,195.6 ± 43,312.5 | <0.001 |
| Total cost | 114,618 ± 263,743 | 65,251.5 ± 45,280.1 | <0.001 |
| Hospital LOS (day) | 8.91 ± 12.45 | 5.89 ± 5.36 | <0.001 |
| ICU | 237 (2.97) | 2 (1.82) | 0.773 |
| ICU LOS (day) | 7.67 ± 10.34 | 2.00 ± 0.00 | <0.001 |
| Expired | 0(0.00) | 0 (0.00) | - |
| Expired after admission | 306 (3.84) | 1 (0.91) | 0.131 |
| Outcome Measures, Point Estimate (95% CI) | Admission After Index Visit N = 7967 | PoCUS Within 1 h Alone at Index Visit and Admitted After an Unscheduled Return Visit, N = 110 | p-Value |
|---|---|---|---|
| LOS in 1st ED (h) | Ref. | −11.59 (−14.20 to −8.98) | <0.001 |
| Total ED LOS (h) | Ref. | 1.47 (−1.15 to 4.09) | 0.271 |
| 1st ED costs (NT$) | Ref. | −9436.1 (−11,542.9 to −7329.3) | <0.001 |
| Total ED costs (NT$) | Ref. | 1458.6 (−655.6 to 3572.8) | 0.176 |
| Total cost (including admission costs) (NT$) | Ref. | −32,807.8 (−81,456.9 to 15,841.3) | 0.186 |
| ICU, OR | Ref. | 0.88 (0.21 to 3.68) | 0.855 |
| Expired, OR | Ref. | - | - |
| Expired after admission, OR | Ref. | 0.37 (0.05 to 2.72) | 0.331 |
| Hospital LOS (day) | Ref. | −1.77 (−4.03 to 0.50) | 0.127 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, S.-Y.; Huang, F.-W.; Lien, W.-C.; Chiu, T.-F.; Wong, T.-C.; Lin, W.-J.; Wu, S.-H. Point-of-Care Ultrasound Within One Hour Associated with ED Flow and Resource Use in Non-Traumatic Abdominal Pain: A Retrospective Observational Study. Diagnostics 2025, 15, 1580. https://doi.org/10.3390/diagnostics15131580
Hung S-Y, Huang F-W, Lien W-C, Chiu T-F, Wong T-C, Lin W-J, Wu S-H. Point-of-Care Ultrasound Within One Hour Associated with ED Flow and Resource Use in Non-Traumatic Abdominal Pain: A Retrospective Observational Study. Diagnostics. 2025; 15(13):1580. https://doi.org/10.3390/diagnostics15131580
Chicago/Turabian StyleHung, Sheng-Yao, Fen-Wei Huang, Wan-Ching Lien, Te-Fa Chiu, Tse-Chyuan Wong, Wei-Jun Lin, and Shih-Hao Wu. 2025. "Point-of-Care Ultrasound Within One Hour Associated with ED Flow and Resource Use in Non-Traumatic Abdominal Pain: A Retrospective Observational Study" Diagnostics 15, no. 13: 1580. https://doi.org/10.3390/diagnostics15131580
APA StyleHung, S.-Y., Huang, F.-W., Lien, W.-C., Chiu, T.-F., Wong, T.-C., Lin, W.-J., & Wu, S.-H. (2025). Point-of-Care Ultrasound Within One Hour Associated with ED Flow and Resource Use in Non-Traumatic Abdominal Pain: A Retrospective Observational Study. Diagnostics, 15(13), 1580. https://doi.org/10.3390/diagnostics15131580







