Anterior Tooth Inclination Between Skeletal Class II and III Malocclusions After Surgical Orthodontic Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects and Materials
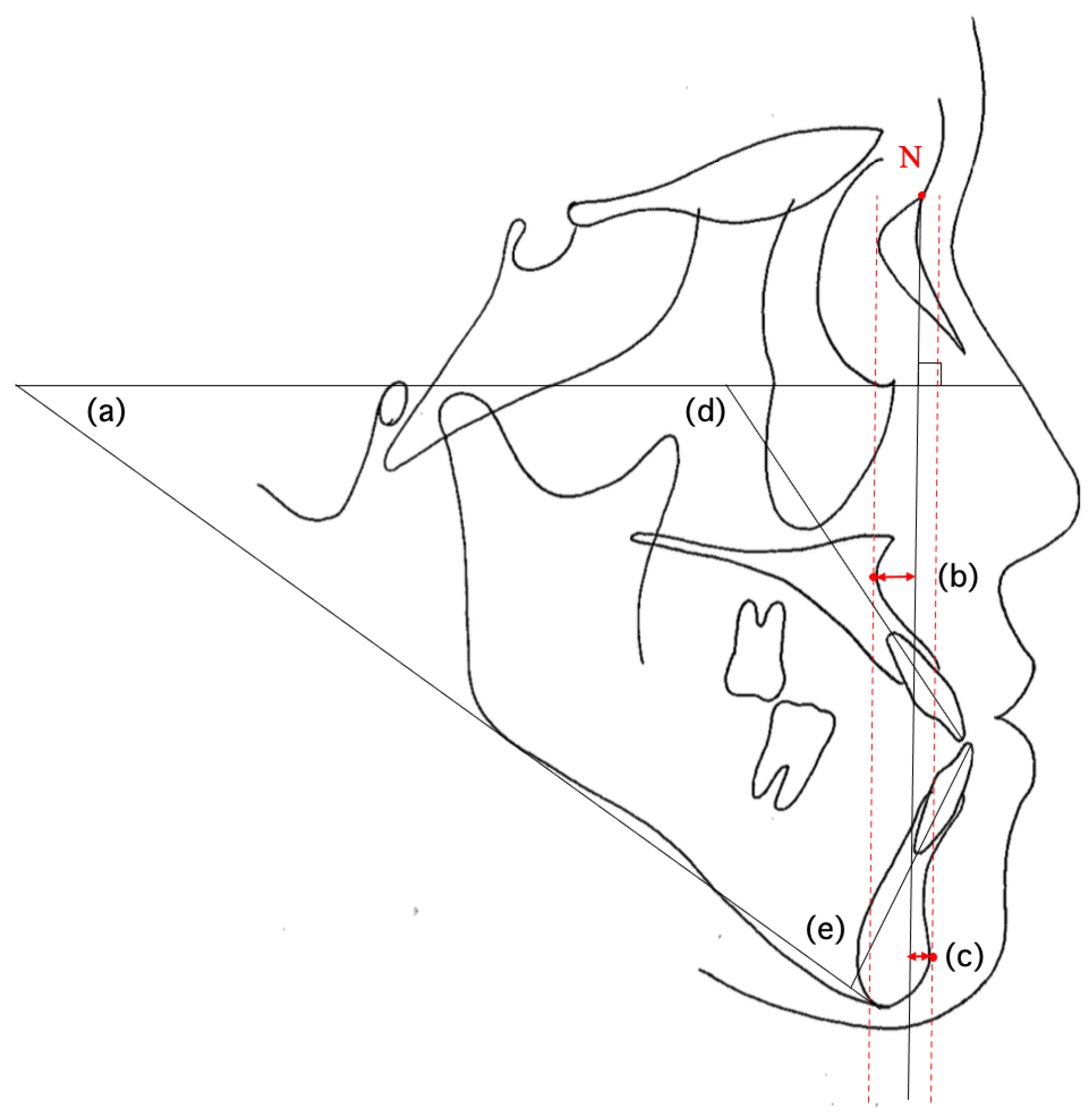
2.2. Cephalometric Landmarks and Measured Values
2.3. Statistical Processing
2.4. Clinical Application Procedure
3. Results
3.1. Comparison of Cephalometric Values Between the Three Groups
3.2. Examination of Pre-Treatment Factors Affecting the Upper and Lower Anterior Tooth Inclination Post-Treatment in Class II and Class III Groups
3.2.1. Class II Group
3.2.2. Class III Group
3.3. Results of Clinical Application
4. Discussion
4.1. Comparison of Cephalometric Analysis Items Between the Three Groups Before and After Treatment
4.2. Examination of Pre-Treatment Factors Affecting the Upper and Lower Tooth Inclination
4.3. Evaluation of the Research Hypothesis
4.4. Clinical Application
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jamilian, A.; Darnahal, A.; Perillo, L. Orthodontic Preparation for Orthognathic Surgery. In A Textbook of Advanced Oral and Maxillofacial Surgery Volume 2; Motamedi, M.H.K., Ed.; InTech: Rijeka, Croatia, 2015; ISBN 978-953-51-2035-3. [Google Scholar]
- Dayoub, N.; Al-Sabbagh, R. The Relationship between Upper Incisors Inclination and Supporting Bone Tissue/A CBCT Study. Int. Arab J. Dent. 2015, 6, 101–107. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, Y.; Lu, W.; Yang, Y.; Liu, X.; Chen, S.; Li, W.; Han, B. Lower Incisor Position in Skeletal Class III Malocclusion Patients: A Comparative Study of Orthodontic Camouflage and Orthognathic Surgery. Angle Orthod. 2024, 94, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Plaza, S.P.; Reimpell, A.; Silva, J.; Montoya, D. Relationship between Skeletal Class II and Class III Malocclusions with Vertical Skeletal Pattern. Dent. Press J. Orthod. 2019, 24, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Macari, A.T.; Hanna, A.E.; Chekie, M.E. Comparisons of Facial Soft Tissue Characteristics in Adult Patients with Various Mandibular Divergence Patterns. BMC Oral Health 2025, 25, 660. [Google Scholar] [CrossRef]
- Joss, C.U.; Thuer, U.W. Stability of Hard Tissue Profile after Mandibular Setback in Sagittal Split Osteotomies: A Longitudinal and Long-Term Follow-up Study. Eur. J. Orthod. 2008, 30, 352–358. [Google Scholar] [CrossRef]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. The Hierarchy of Stability and Predictability in Orthognathic Surgery with Rigid Fixation: An Update and Extension. Head Face Med. 2007, 3, 21. [Google Scholar] [CrossRef]
- Brandtner, C.; Hachleitner, J.; Rippel, C.; Krenkel, C.; Gaggl, A. Long-Term Skeletal and Dental Stability after Orthognathic Surgery of the Maxillo-Mandibular Complex in Class II Patients with Transverse Discrepancies. J. Cranio Maxillofac. Surg. 2015, 43, 1516–1521. [Google Scholar] [CrossRef]
- Bailey, L.J.; Phillips, C.; Proffit, W.R. Long-Term Outcome of Surgical Class III Correction as a Function of Age at Surgery. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 365–370. [Google Scholar] [CrossRef]
- Bailey, L.J.; Dover, A.J.; Proffit, W.R. Long-Term Soft Tissue Changes after Orthodontic and Surgical Corrections of Skeletal Class III Malocclusions. Angle Orthod. 2007, 77, 389–396. [Google Scholar] [CrossRef]
- Le, Y.; Li, F.; Wu, S.; Li, M.; Zhu, C.; Wan, Q. Influence of Differences in Mandibular Incisor Inclination on Skeletal Stability after Orthognathic Surgery in Patients with Skeletal Class III Malocclusion. J. Stomatol. Oral Maxillofac. Surg. 2024, 125, 101747. [Google Scholar] [CrossRef]
- Mahmoud, M.H.; Elfaramawi, T.I. Maxillary Stability in Patients with Skeletal Class III Malocclusion Treated by Bimaxillary Orthognathic Surgery: Comparison of Mandible-First and Maxilla-First Approaches in a Randomised Controlled Study. Br. J. Oral Maxillofac. Surg. 2022, 60, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Tejedor, N.; Martín, C.; Alarcón, J.A.; Oteo-Calatayud, M.D.; Palma-Fernández, J.C. Sexual Dimorphism in the Long-Term Stability (10 Years) of Skeletal Class III Treatment. Prog. Orthod. 2021, 22, 13. [Google Scholar] [CrossRef] [PubMed]
- Ooi, K.; Inoue, N.; Matsushita, K.; Yamaguchi, H.; Mikoya, T.; Kawashiri, S.; Tei, K. Comparison of Postoperative Stability Between BSSRO and Le Fort 1 Osteotomy with BSSRO in Skeletal Class III Malocclusion with Severe Open Bite. J. Maxillofac. Oral Surg. 2020, 19, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Chamsuparb, A.; Chen, Y.-F.; Chen, Y.-A.; Yao, C.-F.; Xi, T.; Liao, Y.-F.; Chen, Y.-R. Stability and Outcome of Surgical-Orthodontic Treatment in Patients of Class III Deformity with and without a History of Orthodontic Treatment. J. Dent. Sci. 2025, 20, 1068–1077. [Google Scholar] [CrossRef]
- Broadbent, B.H. A Foundation for Cephalometric-communication. Am. J. Orthod. 1960, 46, 691–718. [Google Scholar] [CrossRef]
- Togninalli, D.; Antonarakis, G.S.; Papadopoulou, A.K. Relationship between Craniofacial Skeletal Patterns and Anatomic Characteristics of Masticatory Muscles: A Systematic Review and Meta-Analysis. Prog. Orthod. 2024, 25, 36. [Google Scholar] [CrossRef]
- Kawai, N.; Watanabe, M.; Shibata, M.; Horiuchi, S.; Fushima, K.; Tanaka, E. Treatment Decision of Camouflage or Surgical Orthodontic Treatment for Skeletal Class III Patients Based on Analysis of Masticatory Function. J. Dent. Sci. 2022, 17, 822–830. [Google Scholar] [CrossRef]
- An, J.-S.; Jeong, W.; Sonnesen, L.; Baek, S.-H.; Ahn, S.-J. Effects of Presurgical Mandibular Incisor Decompensation on Long-Term Outcomes of Class III Surgical Orthodontic Treatment. J. Clin. Med. 2021, 10, 2870. [Google Scholar] [CrossRef]
- Quast, A.; Santander, P.; Leding, J.; Klenke, D.; Moser, N.; Schliephake, H.; Meyer-Marcotty, P. Orthodontic Incisor Decompensation in Orthognathic Therapy—Success and Efficiency in Three Dimensions. Clin. Oral. Investig. 2021, 25, 4001–4010. [Google Scholar] [CrossRef]
- Ma, H.-M.; Lyu, H.-M.; Xu, L.; Hou, J.-X.; Wang, X.-X.; Li, W.-R.; Li, X.-T. Effect of Augmented Corticotomy-Assisted Presurgical Orthodontic Treatment on Alveolar Bone Fenestration and Dehiscence in Skeletal Class III Patients. J. Dent. Sci. 2023, 18, 997–1007. [Google Scholar] [CrossRef]
- Valerio, C.S.; Cardoso, C.A.E.A.; Araújo, E.A.; Zenóbio, E.G.; Manzi, F.R. Bone Changes in the Mandibular Incisors after Orthodontic Correction of Dental Crowding without Extraction: A Cone-Beam Computed Tomographic Evaluation. Imaging Sci. Dent. 2021, 51, 155. [Google Scholar] [CrossRef]
- Kee, Y.-J.; Moon, H.-E.; Lee, K.C. Evaluation of Alveolar Bone Changes around Mandibular Incisors during Surgical Orthodontic Treatment of Patients with Mandibular Prognathism: Surgery-First Approach vs Conventional Orthognathic Surgery. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 87–94. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Wang, S.; Xiong, H. Periodontal Outcomes in Anterior Teeth Following Presurgical Orthodontic Decompensation in Patients with Skeletal Class III Malocclusion: A Single-Arm Systematic Review and Meta-Analysis. Int. J. Dent. 2024, 2024, 5020873. [Google Scholar] [CrossRef] [PubMed]
- Steiner, C.C. Cephalometrics for You and Me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Jacobson, A. Application of the “Wits” Appraisal. Am. J. Orthod. 1976, 70, 179–189. [Google Scholar] [CrossRef]
- Jacobson, A. The “Wits” Appraisal of Jaw Disharmony. Am. J. Orthod. Dentofac. Orthop. 1975, 67, 125–138. [Google Scholar] [CrossRef]
- Albayrak, E.; Sari, Ö.F.; Buyukcavus, M.H.; Findik, Y.; Yazici, T. Comparison of Soft Tissue Effects of Different Orthognathic Surgical Approaches in Class III Patients Using Photographic Analysis. Sci. Rep. 2025, 15, 15204. [Google Scholar] [CrossRef]
- Uzunçıbuk, H.; Marrapodi, M.M.; Meto, A.; Cervino, G.; Cicciù, M.; Minervini, G. Photographic Analysis of Orofacial Soft Tissue Alterations Related to Rapid Maxillary Expansion in Pediatric Patients. J. Clin. Pediatr. Dent. 2024, 48, 26. [Google Scholar] [CrossRef]
- Potts, B.; Shanker, S.; Fields, H.W.; Vig, K.W.L.; Beck, F.M. Dental and Skeletal Changes Associated with Class II Surgical-Orthodontic Treatment. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 566.e1–566.e7. [Google Scholar] [CrossRef]
- Pereira-Stabile, C.L.; Ochs, M.W.; De Moraes, M.; Moreira, R.W.F. Preoperative Incisor Inclination in Patients with Class III Dentofacial Deformities Treated with Orthognathic Surgery. Br. J. Oral Maxillofac. Surg. 2012, 50, 533–536. [Google Scholar] [CrossRef]
- McNeill, R.W.; West, R.A. Severe Mandibular Retrognathism: Orthodontic versus Surgical Orthodontic Treatment. Am. J. Orthod. 1977, 72, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Yamada, C.; Kitai, N.; Kakimoto, N.; Murakami, S.; Furukawa, S.; Takada, K. Spatial Relationships between the Mandibular Central Incisor and Associated Alveolar Bone in Adults with Mandibular Prognathism. Angle Orthod. 2007, 77, 766–772. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Park, J.U.; Kook, Y.-A. Alveolar Bone Loss around Incisors in Surgical Skeletal Class III Patients. Angle Orthod. 2009, 79, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Li, W.; Xu, L.; Hou, J.; Wang, X.; Ding, S.; Lv, H.; Li, X. Morphometric Evaluation of the Alveolar Bone around Central Incisors during Surgical Orthodontic Treatment of High-angle Skeletal Class III Malocclusion. Orthod. Craniofacial Res. 2021, 24, 87–95. [Google Scholar] [CrossRef]
- Li, M.; Liu, Z.; Yang, X.; Zhu, M.; Ni, J. A Preliminary Investigation into the Impact of Soft Tissue Augmentation-Based Periodontal Phenotype Modification Therapy for Patients Exhibiting Class III Decompensation. BMC Oral Health 2024, 24, 880. [Google Scholar] [CrossRef]
- Chen, Y.; Zhao, B. Comparison and Analysis of Alveolar Bone Structure Characteristics in Skeletal Class II and Class III Malocclusion in the Mandibular Incisor Region. Medicine 2024, 103, e40184. [Google Scholar] [CrossRef]
- Ciavarella, D.; Tepedino, M.; Gallo, C.; Montaruli, G.; Zhurakivska, K.; Coppola, L.; Troiano, G.; Chimenti, C.; Laurenziello, M. Post-Orthodontic Position of Lower Incisors and Gingival Recession: A Retrospective Study. J. Clin. Exp. Dent. 2017, 9, e1425. [Google Scholar] [CrossRef]
- Lee, K.-M.; Kim, Y.-I.; Park, S.-B.; Son, W.-S. Alveolar Bone Loss around Lower Incisors during Surgical Orthodontic Treatment in Mandibular Prognathism. Angle Orthod. 2012, 82, 637–644. [Google Scholar] [CrossRef]
- Joss-Vassalli, I.; Grebenstein, C.; Topouzelis, N.; Sculean, A.; Katsaros, C. Orthodontic Therapy and Gingival Recession: A Systematic Review: Orthodontic Therapy and Gingival Recession. Orthod. Craniofacial Res. 2010, 13, 127–141. [Google Scholar] [CrossRef]
- Hou, L.; He, Y.; Yi, B.; Wang, X.; Liu, X.; Zhang, Y.; Li, Z. Evaluation of Soft Tissue Prediction Accuracy for Orthognathic Surgery with Skeletal Class III Malocclusion Using Maxillofacial Regional Aesthetic Units. Clin. Oral Investig. 2022, 27, 173–182. [Google Scholar] [CrossRef]
- De Lira, A.D.L.S.; De Moura, W.L.; De Barros Vieira, J.M.; Nojima, M.G.; Nojima, L.I. Surgical Prediction of Skeletal and Soft Tissue Changes in Class III Treatment. J. Oral Maxillofac. Surg. 2012, 70, e290–e297. [Google Scholar] [CrossRef] [PubMed]
- Ter Horst, R.; Van Weert, H.; Loonen, T.; Bergé, S.; Vinayahalingam, S.; Baan, F.; Maal, T.; De Jong, G.; Xi, T. Three-Dimensional Virtual Planning in Mandibular Advancement Surgery: Soft Tissue Prediction Based on Deep Learning. J. Cranio Maxillofac. Surg. 2021, 49, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.Y.; Han, M.D.; Tsay, T.P.; Kusnoto, B. Accuracy of Patient-Specific Soft-Tissue Prediction Algorithms for Maxillomandibular Surgery in Class III Patients. Contemp. Clin. Dent. 2022, 13, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, D.; Yamauchi, K.; Yazaki, M.; Saito, S.; Suzuki, H.; Nogami, S.; Takahashi, T. A Comparison of Postoperative, Three-Dimensional Soft Tissue Changes in Patients with Skeletal Class III Malocclusions Treated via Orthodontics-First and Surgery-First Approaches. J. Cranio Maxillofac. Surg. 2021, 49, 898–904. [Google Scholar] [CrossRef]
- Sahm, C.; Kirschneck, C.; Proff, P.; Paddenberg-Schubert, E. Predictors of Changes in Incisor Inclination during Orthodontic Levelling and Alignment with Fixed Appliances: A Retrospective Cross-Sectional Study. Head Face Med. 2025, 21, 41. [Google Scholar] [CrossRef]

| Inclusion Criteria | |||
|---|---|---|---|
| Parameter | Class II | Class III | Class I |
| ANB angle | ANB ≥ 5° | ANB ≤ −1° | 0° < ANB < 5° |
| Wits appraisal | Wits ≥ +2 mm | Wits ≤ −6 mm | −6 < Wits < 2 mm |
| SNA angle | SNA ≥ 80° | SNA ≤ 84° | 80° < SNA < 84° |
| SNB angle | SNB ≤ 76° | SNB ≥ 86° | 76° < SNB < 86° |
| Molar relationship | Angle Class II | Angle Class III | Angle Class I molar relationship or mild deviations |
| Parameter | Exclusion Criteria |
|---|---|
| Congenital anomalies | Cleft lip and palate |
| Anterior open bite | Overbite ≤ −2 mm |
| Facial asymmetry | Menton deviation > 3 mm |
| Missing or prosthetic anterior teeth | Patients with one or more missing or prosthetic anterior teeth |
| Multiple missing teeth | Patients with three or more missing permanent teeth (excluding third molars) |
| History of genioplasty | History of genioplasty |
| Surgery-first protocol | Cases treated with surgery-first approach |
| Class II Group (ANB ≥ 5°) n = 40 | Class III Group (Wits ≤ −6 mm) n = 41 | Class I Group (0° < ANB < 5°) n = 41 | |
|---|---|---|---|
| Sex | |||
| Male | 10 | 17 | 12 |
| Female | 30 | 24 | 29 |
| Age (y) | |||
| Mean | 29.7 ± 8.4 | 29.6 ± 7.5 | 20.5 ± 8.0 |
| Range | 15.0–49.0 | 18.6–51.8 | 11.0–58.5 |
| Ext or Non Ext | |||
| Ext | 20 | 21 | 28 |
| Non Ext | 20 | 20 | 13 |
| Orthognathic surgery | |||
| SSRO | 20 | 21 | |
| Le Fort I + SSRO | 20 | 20 |
| Parameter | Definition |
|---|---|
| FMA | The angle formed between the Frankfort horizontal plane and the mandibular plane |
| Mc PtA | The distance between the nasion perpendicular line and point A, measured perpendicular to the nasion perpendicular line |
| Mc Pog | The distance between the pogonion and the nasion perpendicular line measured perpendicular to the nasion perpendicular line |
| U1 to FH | The angle between the long axis of the upper central incisor (U1) and the Frankfort horizontal plane |
| L1 to MP | The angle between the long axis of the lower central incisor (L1) and the mandibular plane |
| Class I | Class II | Class III | Cl.I–Cl.II | Cl.I–Cl.III | Cl.II–Cl.III | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | Mean | S.D. | ||||
| ANB (°) | 2.5 | 1.5 | 8.6 | 2.5 | −3.0 | 2.9 | ** | ** | ** |
| Mc PtA (mm) | −1.1 | 2.7 | −0.9 | 5.3 | −0.9 | 3.5 | N.S. | N.S. | N.S. |
| Mc Pog (mm) | −5.8 | 5.4 | −20.2 | 12.2 | 8.1 | 7.4 | ** | ** | ** |
| Wits (mm) | −1.6 | 3.4 | 5.7 | 6.7 | −14.1 | 5.7 | ** | ** | ** |
| FMA (°) | 30.8 | 5.8 | 37.9 | 8.5 | 28.3 | 7.2 | ** | N.S. | ** |
| U1 to FH (°) | 116.9 | 8.4 | 112.1 | 9.4 | 119.5 | 6.4 | * | N.S. | ** |
| L1 to MP (°) | 95.5 | 7.5 | 98.1 | 8.6 | 82.9 | 8.8 | N.S. | ** | ** |
| Overjet (mm) | 3.2 | 2.7 | 7.4 | 2.7 | −2.1 | 2.7 | ** | ** | ** |
| Overbite (mm) | 1.1 | 1.9 | 0.1 | 4.0 | 0.3 | 2.0 | N.S. | N.S. | N.S. |
| E-line upper (mm) | −0.2 | 2.6 | 3.7 | 2.8 | −3.7 | 2.6 | ** | ** | ** |
| E-line lower (mm) | 1.5 | 3.1 | 4.7 | 3.3 | −0.2 | 3.4 | ** | * | ** |
| Class I | Class II | Class III | Cl.I–Cl.II | Cl.I–Cl.III | Cl.II–Cl.III | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | Mean | S.D. | ||||
| ANB (°) | 2.4 | 1.5 | 6.3 | 2.5 | 0 | 2.2 | ** | ** | ** |
| Mc PtA (mm) | −1.4 | 2.9 | −1.3 | 5.8 | −0.3 | 2.8 | N.S. | N.S. | N.S. |
| Mc Pog (mm) | −6.1 | 5.4 | −14.8 | 10.9 | 0.6 | 7.4 | ** | ** | ** |
| Wits (mm) | −1.5 | 3.2 | 2.0 | 4.2 | −6.2 | 3.5 | ** | ** | ** |
| FMA (°) | 30.7 | 5.6 | 36.5 | 8.7 | 29.3 | 6.6 | ** | N.S. | ** |
| U1 to FH (°) | 111.1 | 7.9 | 106.8 | 6.9 | 120.4 | 7.2 | * | ** | ** |
| L1 to MP (°) | 92.4 | 7.8 | 95.8 | 6.8 | 84.9 | 7.3 | N.S. | ** | ** |
| Overjet (mm) | 2.7 | 0.9 | 2.8 | 0.9 | 3.1 | 0.8 | N.S. | N.S. | N.S. |
| Overbite (mm) | 1.9 | 0.8 | 2.1 | 1.7 | 1.3 | 0.8 | N.S. | N.S. | * |
| E-line upper (mm) | −1.0 | 2.4 | 1.0 | 2.8 | −2.4 | 2.1 | ** | * | ** |
| E-line lower (mm) | 0.2 | 2.1 | 1.7 | 2.9 | −1.0 | 2.9 | * | N.S. | ** |
| Regression Coefficient | Standardized Regression Coefficient | Significance (p) | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Constant | 117.143 | 0.000 ** | 112.623 | 121.663 | |
| Mc Pog (pre) | 0.453 | 0.726 | 0.000 ** | 0.240 | 0.665 |
| Regression Coefficient | Standardized Regression Coefficient | Significance (p) | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Constant | 19.413 | 0.305 | −19.219 | 58.046 | |
| L1-MP (pre) | 0.804 | 0.708 | 0.000 ** | 0.406 | 1.201 |
| Regression Coefficient | Standardized Regression Coefficient | Significance (p) | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Constant | 60.030 | 0.017 * | 12.385 | 107.675 | |
| U1-FH (pre) | 0.472 | 0.445 | 0.030 * | 0.050 | 0.895 |
| Mc Pog (pre) | 0.658 | 0.404 | 0.047 * | 0.010 | 1.306 |
| Regression Coefficient | Standardized Regression Coefficient | Significance (p) | 95%Confidence Interval | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Constant | 8.467 | 0.656 | −30.888 | 47.821 | |
| L1-MP (pre) | 0.787 | 0.679 | 0.001 ** | 0.360 | 1.214 |
| FMA (pre) | 0.405 | 0.420 | 0.028 * | 0.050 | 0.761 |
| Case 1 | Case 2 | |||||
|---|---|---|---|---|---|---|
| Measured Value | Predicted Value | Residual | Measured Value | Predicted Value | Residual | |
| U1 to FH | 104.0 | 107.2 | −3.2 | 108.0 | 106.7 | 1.3 |
| L1 to MP | 95.0 | 94.2 | 0.8 | 100.2 | 100.5 | −0.3 |
| Case 3 | Case 4 | |||||
|---|---|---|---|---|---|---|
| Measured Value | Predicted Value | Residual | Measured Value | Predicted Value | Residual | |
| U1 to FH | 121.0 | 120.0 | 1.0 | 121.6 | 119.8 | 1.8 |
| L1 to MP | 84.6 | 85.9 | −1.3 | 85.1 | 84.6 | 0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomaru, H.; Tachiki, C.; Nakamura, Y.; Ariizumi, D.; Matsunaga, S.; Sugahara, K.; Watanabe, A.; Katakura, A.; Nishii, Y. Anterior Tooth Inclination Between Skeletal Class II and III Malocclusions After Surgical Orthodontic Treatment. Diagnostics 2025, 15, 1553. https://doi.org/10.3390/diagnostics15121553
Tomaru H, Tachiki C, Nakamura Y, Ariizumi D, Matsunaga S, Sugahara K, Watanabe A, Katakura A, Nishii Y. Anterior Tooth Inclination Between Skeletal Class II and III Malocclusions After Surgical Orthodontic Treatment. Diagnostics. 2025; 15(12):1553. https://doi.org/10.3390/diagnostics15121553
Chicago/Turabian StyleTomaru, Hiromi, Chie Tachiki, Yu Nakamura, Dai Ariizumi, Satoru Matsunaga, Keisuke Sugahara, Akira Watanabe, Akira Katakura, and Yasushi Nishii. 2025. "Anterior Tooth Inclination Between Skeletal Class II and III Malocclusions After Surgical Orthodontic Treatment" Diagnostics 15, no. 12: 1553. https://doi.org/10.3390/diagnostics15121553
APA StyleTomaru, H., Tachiki, C., Nakamura, Y., Ariizumi, D., Matsunaga, S., Sugahara, K., Watanabe, A., Katakura, A., & Nishii, Y. (2025). Anterior Tooth Inclination Between Skeletal Class II and III Malocclusions After Surgical Orthodontic Treatment. Diagnostics, 15(12), 1553. https://doi.org/10.3390/diagnostics15121553









