One-Year Follow-Up of Non-Healing Socket in Hodgkin’s Lymphoma Patient: Case Report and Literature Review on Management Strategies
Abstract
1. Introduction
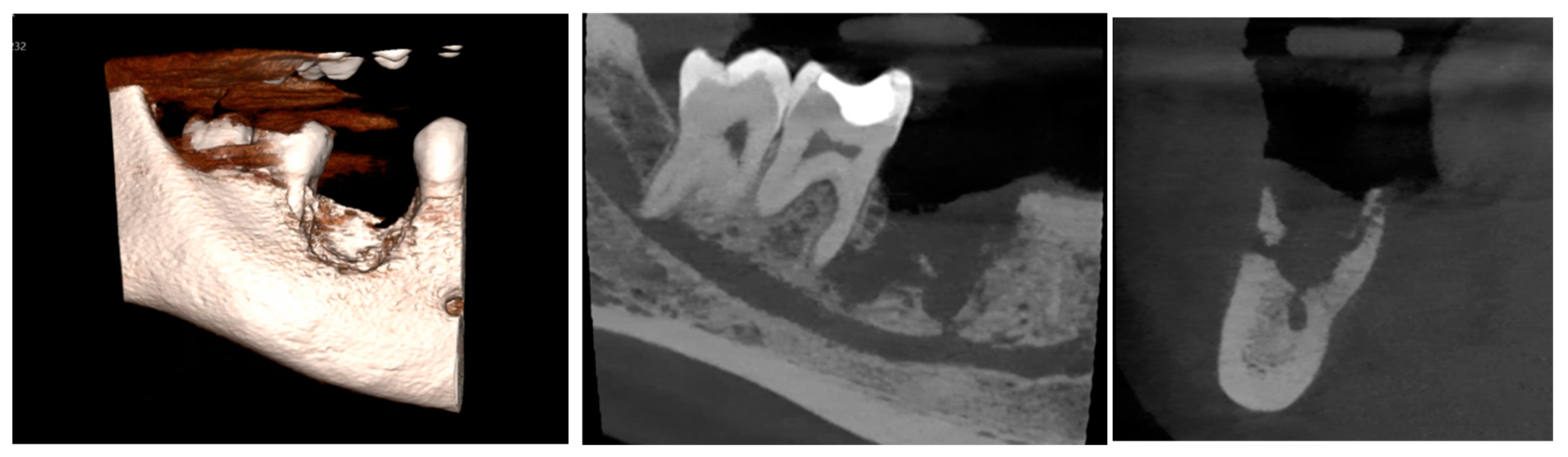
2. Case Presentation
2.1. Clinical Examination
2.2. Differential Diagnosis
2.3. Management and Intervention
2.4. Microscopic Description
2.5. Follow-Up and Outcomes
2.6. Review of the Literature
3. Discussion
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
List of Abbreviations
| LR6 | Lower right first molar |
| NaOCl | Sodium hypochlorite |
| L-PRF | Leukocyte–platelet-rich fibrin |
| PENTO | Pentoxifylline and tocopherol |
| HBOT | Hyperbaric oxygen therapy |
| OMFS | Oral and maxillofacial surgery department |
| RLDH | Royal London Dental Hospital |
| OPG | Orthopantomograph |
| CBCT | Cone-beam computed tomography |
| MRONJ | Medication-related osteonecrosis of the jaw |
| ORNJ | Osteoradionecrosis of the jaws |
References
- Fedorowicz, Z.; Nasser, M.; Sequeira-Byron, P.; de Souza, R.F.; Carter, B.; Heft, M. Irrigants for non-surgical root canal treatment in mature permanent teeth. Cochrane Database Syst. Rev. 2012, 2012, CD008948. [Google Scholar] [CrossRef] [PubMed]
- Pelka, M.; Petschelt, A. Permanent mimic musculature and nerve damage caused by sodium hypochlorite: A case report. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2008, 106, e80–e83. [Google Scholar] [CrossRef] [PubMed]
- Witton, R.; Brennan, P.A. Severe tissue damage and neurological deficit following extravasation of sodium hypochlorite solution during routine endodontic treatment. Br. Dent. J. 2005, 198, 749–750. [Google Scholar] [CrossRef] [PubMed]
- Silva, T.D.B.; Ferreira, C.B.T.; Leite, G.B.; Pontes, J.R.M.; Antunes, H.S. Oral manifestations of lymphoma: A systematic review. Ecancermedicalscience 2016, 10, 665. [Google Scholar] [CrossRef]
- Serper, A.; Özbek, M.; Çalt, S. Accidental sodium hypochlorite-induced skin injury during endodontic treatment. J. Endod. 2004, 30, 180–181. [Google Scholar] [CrossRef]
- Gatot, A.; Arbelle, J.; Leiberman, A.; Yanai-Inbar, I. Effects of sodium hypochlorite on soft tissues after its inadvertent injection beyond the root apex. J. Endod. 1991, 17, 573–574. [Google Scholar] [CrossRef]
- Akay, N.; Şimşek, G.; Taş, B.M.; Kılıç, R. Inadvertent injection of sodium hypochlorite to oral mucosa. Eur. J. Rhinol. Allergy 2019, 2, 32–34. [Google Scholar] [CrossRef]
- Faras, F.; Abo-Alhassan, F.; Sadeq, A.; Burezq, H. Complication of improper management of sodium hypochlorite accident during root canal treatment. J. Int. Soc. Prev. Community Dent. 2016, 6, 493–496. [Google Scholar] [CrossRef]
- Goswami, M.; Chhabra, N.; Kumar, G.; Verma, M.; Chhabra, A. Sodium hypochlorite dental accidents. Paediatr. Int. Child. Health. 2013, 34, 66–69. [Google Scholar] [CrossRef]
- Gernhardt, C.R.; Eppendorf, K.; Kozlowski, A.; Brandt, M. Toxicity of sodium hypochlorite used as an endodontic irrigant. Int. Endod. J. 2004, 37, 272–280. [Google Scholar] [CrossRef]
- Gallas-Torreira, M.M.; Reboiras-López, M.D.; García-García, A.; Gándara-Rey, J. Mandibular nerve paresthesia caused by endodontic treatment. Med. Oral. 2003, 8, 299–303. [Google Scholar] [PubMed]
- Motta, M.V.; Chaves-Mendonca, M.A.L.; Stirton, C.G.; Cardozo, H.F. Accidental injection with sodium hypochlorite: Report of a case. Int. Endod. J. 2009, 42, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Gursoy, U.K.; Bostancı, V.; Kosger, H.H. Palatal mucosa necrosis because of accidental sodium hypochlorite injection instead of anaesthetic solution. Int. Endod. J. 2006, 39, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Pontes, F.; Pontes, H.; Adachi, P.; Rodini, C.; Almeida, D.; Pinto, D., Jr. Gingival and bone necrosis caused by accidental sodium hypochlorite injection instead of anaesthetic solution. Int. Endod. J. 2008, 41, 267–270. [Google Scholar] [CrossRef]
- Aslan, M.; Özcan, M. Accidental injection of sodium hypochlorite into buccal mucosa before endodontic treatment: Case report. Essent. Dent. 2023, 2, 66–69. [Google Scholar] [CrossRef]
- Salvadori, M.; Venturi, G.; Bertoletti, P.; Francinelli, J.; Tonini, R.; Garo, M.L.; Salgarello, S. Sodium hypochlorite accident during canal treatment: Report of four cases documented according to new standards. Appl. Sci. 2022, 12, 8525. [Google Scholar] [CrossRef]
- da Fonseca Wastner, B.; de Souza Lessa, M.; Sassi, L.M.; Pianovski, M.A. Life-threatening reaction of a pediatric cancer patient to sodium hypochlorite. Res. Soc. Dev. 2021, 10, e282101320446. [Google Scholar]
- Coaguila-Llerena, H.; Denegri-Hacking, A.; Lucano-Tinoco, L.; Aquino, C.E. Accidental extrusion of sodium hypochlorite in a patient taking alendronate: A case report with an 8-year follow-up. J. Endod. 2021, 47, 1983–1989. [Google Scholar] [CrossRef]
- Aslam, R.D.; Pitros, P.; Liew, J.; Besi, E. The adjunctive use of Leukocyte-Platelet Rich Fibrin (L-PRF) in the management of Medication Related Osteonecrosis of the Jaw (MRONJ): A retrospective observational study. Oral. Maxillofac. Surg. 2024, 28, 1605–1615. [Google Scholar] [CrossRef] [PubMed]
- Besi, E.; Pitros, P. The role of leukocyte and platelet-rich fibrin in the prevention of medication-related osteonecrosis of the jaw, in patients requiring dental extractions: An observational study. Oral. Maxillofac. Surg. 2024, 28, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Arqueros-Lemus, M.; Mariño-Recabarren, D.; Niklander, S.; Martínez-Flores, R.; Moraga, V. Pentoxifylline and tocopherol for the treatment of osteoradionecrosis of the jaws. A systematic review. Med. Oral. Patol. Oral. Cir. Bucal. 2023, 28, e293–e300. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bennett, M.H.; Feldmeier, J.; Hampson, N.B.; Smee, R.; Milross, C. Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Database Syst. Rev. 2016, 4, CD005005, Update in: Cochrane Database Syst. Rev. 2023, 8, CD005005. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ruggiero, S.L.; Dodson, T.B.; Aghaloo, T.; Carlson, E.R.; Ward, B.B.; Kademani, D. American Association of Oral and Maxillofacial Surgeons’ position paper on medication-related osteonecrosis of the jaw—2022 update. J. Oral. Maxillofac. Surg. 2022, 80, 920–943. [Google Scholar] [CrossRef] [PubMed]
- Lajolo, C.; Rupe, C.; Gioco, G.; Troiano, G.; Patini, R.; Petruzzi, M.; Miccichè, F.; Giuliani, M. Osteoradionecrosis of the jaws due to teeth extractions during and after radiotherapy: A systematic review. Cancers 2021, 13, 5798. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.E. Osteoradionecrosis: A new concept of its pathophysiology. J. Oral. Maxillofac. Surg. 1983, 41, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Cortese, A.; Casarella, A.; Howard, C.M.; Claudio, P.P. Epi-mucosa fixation and autologous platelet-rich fibrin treatment in medication-related osteonecrosis of the jaw. Dent. J. 2021, 9, 50. [Google Scholar] [CrossRef]
- Zelinka, J.; Blahak, J.; Perina, V.; Pacasova, R.; Treglerova, J.; Bulik, O. The use of platelet-rich fibrin in the surgical treatment of medication-related osteonecrosis of the jaw: 40 patients prospective study. Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc Czech Repub. 2021, 165, 322–327. [Google Scholar] [CrossRef]




| Reference | Signs and Symptoms | Duration | Managements | Outcomes |
|---|---|---|---|---|
| [2] | Pain and swelling, paresthesia in the infraorbital nerve area and weakness in the buccal branch of the facial nerve, leading to loss of upper lip and cheek function. | Pain and swelling lasted for about 1 week. Paresthesia persisted for 3 years with no signs of improvement in the facial nerve weakness. | Local anesthesia, cold compress, antibiotics, and analgesics. The patient was later referred to a neurologist for further assessment of the persistent sensory and motor deficits. The patient underwent prosthetic rehabilitation to replace the upper front teeth. | The patient experienced permanent facial nerve weakness and reduced sensitivity in the infraorbital region. No significant improvement occurred even after 3 years, despite daily attempts to train the mimic musculature. Permanent paresthesia and weakness of the mimic musculature, causing difficulty with facial movements like smiling and uncontrolled salivation. |
| [3] | Pain and swelling, weakness of the buccal branch of the facial nerve, leading to loss of upper lip and cheek function, with the mouth corner being pulled down by unopposed lower lip muscles. Infra-orbital ecchymosis and altered sensation in the right infra-orbital nerve area. | One month later: Swelling had almost resolved, mouth opening was improved, and the patient was pain-free. However, there was no improvement in facial nerve weakness after one month. | The patient was treated with intravenous dexamethasone (8 mg, three times a day) and co-amoxiclav (1.2 g, three times a day), along with regular analgesia. | Outcome after one month: The patient was free from pain, with significant improvement in mouth opening. However, the weakness of the facial nerve persisted, and there was minimal improvement in infra-orbital nerve paresthesia. |
| [5] | Burning sensation around the rubber dam during sodium hypochlorite irrigation. A rash developed around the patient’s chin, which later formed scabs. | Burning sensation ceased after 3 days, and the scab began to fall off after 7 days. The skin discoloration from the burn disappeared after 3 months, and the patient fully recovered. | The patient was treated with topical Hamamelis virginiana extract (Hametan) twice a day for 2 weeks. | The patient fully recovered with no long-term effects. The burning sensation and skin discoloration were alleviated, and there were no further complications after 3 months. |
| [6] | Pain and massive edema on the right cheek and upper lip. The swelling extended to the right orbit, and the patient experienced right eye pain, blurred vision, and corneal discoloration. A necrotic area appeared on the upper lip mucosa. | The symptoms developed rapidly within minutes to hours, with the swelling extending over two weeks. | The patient received intravenous hydrocortisone and penicillin G for swelling and pain control. Surgical debridement was performed to excise the necrotic mucosa and clean the affected area. The area was irrigated daily with saline to remove necrotic tissue, and intravenous antibiotics were administered to treat the infection. | After two weeks, the wound healed, but the patient experienced long-term scarring, dimples, and right infraorbital nerve anesthesia. |
| [7] | The patient reported burning, stinging, and sharp pain during the injection of 1% sodium hypochlorite. Edema, difficulty swallowing, redness on the cheek, and loss of sensation were noted in the mental nerve area. | The patient underwent regular debridement of necrotic tissue, and re-epithelialization was observed by the third month. All symptoms resolved by the sixth month. | The patient was administered pheniramine maleate, dexamethasone, and intraoral antibiotics (1000 mg of amoxicillin, twice a day, for two weeks), along with alpha-lipoic acid (300 mg, daily, for one month). Regular clinical follow-up was performed, and necrotic tissue was debrided every 3 days for 4 weeks. The patient was advised to avoid smoking and consuming hot food and alcohol. | Re-epithelialization of necrotic tissue was observed after one month. The paresthesia of the mental nerve decreased after three months, and all symptoms completely disappeared by the sixth month. |
| [8] | Severe chemical burn on the right infraorbital area and partial necrosis of the hard palate. Erythematous, tender skin on the right cheek, numbness, and blackish discharge from the nose. | Mucosal damage healed completely after six weeks, but facial scar discoloration remained. | The patient was treated with creams and ointments for chemical burns. The symptoms were managed conservatively without surgical intervention. The patient was monitored for two weeks and did not require further surgical treatment. | The facial scar remained, but the mucosal damage healed nearly completely. The patient recovered without significant long-term complications, though facial discoloration remained. |
| [9] | Case 1: Gross left facial swelling extending from the mandible to the zygomatic arch with diffuse subcutaneous ecchymosis, mouth-opening limited to 20 mm, and intra-oral necrosis, ulceration, and ecchymosis. Case 2: Severe pain and swelling in the left cheek, extending from the mandible to the left eye, with no intra-oral tissue damage. | The swelling and pain reduced significantly within a few days. In Case 1, mouth opening and facial swelling improved by the 7th day, and by the 3rd week, and the face and mouth were normal. In Case 2, the symptoms improved significantly within 4 weeks. | Case 1: The oral cavity was irrigated with normal saline, and ice packs were applied for 1 day, followed by warm saline rinses. Prednisone was prescribed to control inflammation, and co-amoxiclav and analgesics were given. Regular monitoring was undertaken over the next few days. Case 2: Cold and warm compresses, saline rinses, acetaminophen-based narcotic analgesics, prophylactic antibiotics, and corticosteroids were prescribed. | Case 1: Complete resolution of symptoms, normal mouth opening, and absence of pain by 3 weeks. Case 2: All symptoms resolved satisfactorily after 4 weeks. The root canal treatment was successfully completed with alternative irrigants (hydrogen peroxide and chlorhexidine gluconate). |
| [10] | Severe burning pain, swelling of the surrounding tissue, and redness observed at the tissues beyond the root apex. Profuse bleeding, severe tissue necrosis, and potential nerve involvement. | Symptoms improved appropriately, but full resolution may take several weeks, and nerve recovery could take several months. | Immediate irrigation with normal saline to flush out the NaOCl, followed by ice packs to reduce swelling. Steroids like prednisone were administered to control inflammation. Antibiotics to prevent secondary infections were prescribed, along with warm compresses to stimulate healing and improve circulation after the initial 24 h period. | The patient showed significant improvement over several weeks, with the swelling and ecchymosis reducing. In some cases, tissue necrosis was resolved after several weeks with non-surgical interventions, but facial nerve damage (e.g., numbness or weakness) could persist for a few months. |
| [11] | Sudden onset of pain in the left hemimandible and numbness in the left lower lip. Persistent pain in the left lower molar region and the left lower lip remained numb after the initial procedure. | Pain and numbness persisted for 15 days. After the gutta-percha point was removed surgically, pain subsided within 15 days, but numbness in the lower lip persisted for about a month before resolving completely. | A surgical procedure was performed to remove the gutta-percha point that had overfilled the root canal and entered the mandibular canal. The patient underwent an outpatient surgical procedure to remove the gutta-percha point, with the lesion being addressed by raising a mucoperiosteal flap for ostectomy and careful curettage. | The pain was resolved after the surgical removal of the gutta-percha, although the paresthesia (numbness) persisted for a while. The numbness in the lower lip was fully recovered within a month after the surgery. |
| [12] | Severe pain at the injection site, which began immediately after the sodium hypochlorite was injected instead of the anesthetic solution. Rapid development of local edema and tissue necrosis, labial ptosis (drooping), paresthesia in the upper lip, and visual blurring. | The severe pain and edema appeared immediately. The visual discomfort resolved after 8 days. The mucosal injury healed with scarring after 60 days. The labial ptosis resolved after 3 months, but the lip paresthesia persisted for 3 years. | The patient was given Arcoxia (anti-inflammatory), amoxicillin (antibiotic), and dexamethasone with B-complex vitamins for inflammation control. The patient received a combination of antibiotics and anti-inflammatory medications to manage the necrosis and prevent infection. Regular follow-up ensured proper tissue healing and symptom management. | The edema and necrosis resolved with scarring. Lip ptosis improved within 3 months, but paresthesia in the lip persisted for 3 years despite treatment. |
| [13] | Severe pain upon injection, which was followed by tissue necrosis in the palatal mucosa. Swelling and discoloration (purple) around the necrotic area, with the center being yellow-white. The area was painless during palpation. | Pain persisted for 2 days after the injection, after which it subsided. Swelling and tissue necrosis were visible for the next 15 days. | The patient was monitored conservatively as the mucosa showed signs of healing. No surgical intervention was needed since the tissue was healing naturally. Regular monitoring was carried out for 30 days, ensuring that no further complications arose. | Complete healing without scarring was achieved within 30 days. No long-term complications were reported, and the mucosal tissue healed effectively. |
| [14] | Severe pain occurred immediately after the accidental injection of NaOCl instead of the intended anesthetic solution. Swelling of the gingiva and surrounding tissues, followed by the formation of necrotic tissue and bone sequestration. | Pain persisted for 3 days after the injection. Swelling and tissue necrosis were present for the following 2 months. | The patient was treated with anti-inflammatory medication (diclofenac) and antibiotics (amoxicillin) to manage pain, inflammation, and prevent infection. After 2 months, surgical coverage with a laterally positioned flap was performed to address the necrotic tissue and bone sequestration. | The area affected by chemical necrosis healed after 3 weeks, with no further tissue damage or complications. The root canal treatment of the adjacent tooth was completed 30 days after the surgical procedure. |
| [15] | Severe pain upon injection, swelling, and hyperemia in the right half of the face, along with black necrotic areas on the right buccal mucosa. No facial paralysis, but the patient exhibited significant tissue damage and edema in the affected area. | Severe swelling, pain, and necrosis developed within 4–5 h of the accidental injection. After 24 h of treatment, the patient’s symptoms regressed. Full recovery occurred within 4 weeks, with no residual effects. | The patient was hospitalized and treated with IV antibiotics (ceftriaxone and metronidazole), anti-inflammatory medication (dexketoprofen), and analgesics (paracetamol). Cold compresses and bed rest were recommended. The patient was monitored for 4 weeks, after which they showed complete recovery with no complications. | The patient recovered fully without any long-term effects, and the necrotic tissue healed completely within a month. There were no additional issues reported after the treatment. |
| [16] | Report A: Swelling and ecchymosis on the right side of the face, particularly around the mouth and periorbital region. Ulcerative lesions on the internal lip mucosa. Report B: Mild edema and ecchymosis on the right commissure lip with no mucosal lesions. Report C: Swelling and ecchymosis on the left side of the face, particularly near the mouth and periorbital region. Report D: Severe pain and bleeding from the root canal, followed by mild edema and swelling on the face. | Report A: Swelling and bruising peaked within 24 h, which improved significantly after 3–5 days. Report B: Swelling and ecchymosis persisted for 5 days but resolved with minimal symptoms remaining. Report C: Symptoms like swelling and ecchymosis reduced after 5 days. Report D: Swelling persisted for several days, but pain and symptoms resolved within 6 days. | Report A: Cold compress, antibiotic (amoxicillin with clavulanic acid), pain control (paracetamol and ibuprofen), and corticosteroids (prednisone). Report B: Saline solution flush, cold compress, and prescribed medications (ciprofloxacin, paracetamol, ibuprofen, and betamethasone). Report C: Saline flush, cold compress, and medications (amoxicillin, prednisone, and ibuprofen). Report D: Saline flush, cold compress, and prescribed medications (amoxicillin, prednisone, and ibuprofen). | Report A: Significant improvement in 3–5 days, with the continuation of root canal treatment using chlorhexidine. Report B: Symptoms reduced significantly after 5 days; root canal treatment continued with chlorhexidine. Report C: Recovery within 5 days, root canal treatment continued with a side-vented needle after CBCT revealed apical fenestration. Report D: Significant reduction in symptoms after 6 days, treatment completed with no legal actions taken. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfurhud, A.A. One-Year Follow-Up of Non-Healing Socket in Hodgkin’s Lymphoma Patient: Case Report and Literature Review on Management Strategies. Diagnostics 2025, 15, 1215. https://doi.org/10.3390/diagnostics15101215
Alfurhud AA. One-Year Follow-Up of Non-Healing Socket in Hodgkin’s Lymphoma Patient: Case Report and Literature Review on Management Strategies. Diagnostics. 2025; 15(10):1215. https://doi.org/10.3390/diagnostics15101215
Chicago/Turabian StyleAlfurhud, Ahmed Ata. 2025. "One-Year Follow-Up of Non-Healing Socket in Hodgkin’s Lymphoma Patient: Case Report and Literature Review on Management Strategies" Diagnostics 15, no. 10: 1215. https://doi.org/10.3390/diagnostics15101215
APA StyleAlfurhud, A. A. (2025). One-Year Follow-Up of Non-Healing Socket in Hodgkin’s Lymphoma Patient: Case Report and Literature Review on Management Strategies. Diagnostics, 15(10), 1215. https://doi.org/10.3390/diagnostics15101215







