Ibuprofen-Induced Multiple Fixed Drug Eruption Confirmed by Re-Challenge: A Case Report and Literature Review
Abstract
1. Introduction
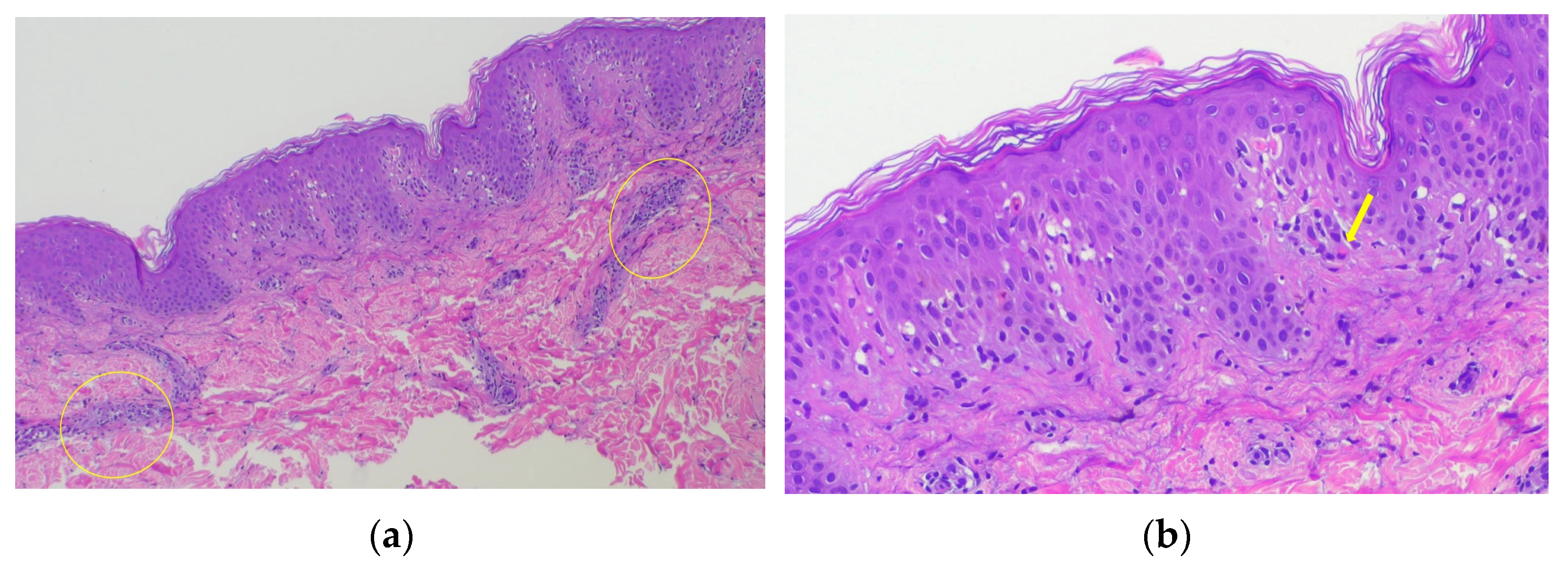
2. Case Presentation
3. Literature Review
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kanwar, A.J.; Bharija, S.C.; Belhaj, M.S. Fixed drug eruptions in children: A series of 23 cases with provocative tests. Dermatologica 1986, 172, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Flowers, H.; Brodell, R.; Brents, M.; Wyatt, J.P. Fixed drug eruptions: Presentation, diagnosis, and management. South. Med. J. 2014, 107, 724–727. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; John, A.M.; Handler, M.Z.; Schwartz, R.A. Fixed Drug Eruptions: An Update, Emphasizing the Potentially Lethal Generalized Bullous Fixed Drug Eruption. Am. J. Clin. Dermatol. 2020, 21, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.F.; Chiang, C.P. Answer: Can you identify this condition? Can. Fam. Physician 2012, 58, 660–661. [Google Scholar]
- Kordeva, S.; Cardoso, J.C.; Tchernev, G. Multifocal Fixed Drug Eruption Mimicking Acquired Dermal Melanocytosis. Georgian Med. News 2023, 335, 13–16. [Google Scholar]
- Bhanja, D.B.; Sil, A.; Panigrahi, A.; Chakraborty, S. Ibuprofen-induced generalised bullous fixed drug eruption. Postgrad. Med. J. 2020, 96, 706–707. [Google Scholar] [CrossRef]
- Cho, Y.T.; Lin, J.W.; Chen, Y.C.; Chang, C.Y.; Hsiao, C.H.; Chung, W.H.; Chu, C.Y. Generalized bullous fixed drug eruption is distinct from Stevens-Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J. Am. Acad. Dermatol. 2014, 70, 539–548. [Google Scholar] [CrossRef]
- Dharamsi, F.M.; Michener, M.D.; Dharamsi, J.W. Bullous fixed drug eruption masquerading as recurrent Stevens Johnson syndrome. J. Emerg. Med. 2015, 48, 551–554. [Google Scholar] [CrossRef]
- Lin, T.K.; Hsu, M.M.; Lee, J.Y. Clinical resemblance of widespread bullous fixed drug eruption to Stevens-Johnson syndrome or toxic epidermal necrolysis: Report of two cases. J. Formos. Med. Assoc. 2002, 101, 572–576. [Google Scholar]
- Roy Chowdhury, S. Genital Ulcers Are Not Always Because of Sexually Transmitted Infections: A Case Report of an Unusual Presentation of Fixed Drug Eruption in a Pediatric Patient. J. Pediatr. Health Care 2024, 38, 758–760. [Google Scholar] [CrossRef]
- Fischer, G. Vulvar fixed drug eruption. A report of 13 cases. J. Reprod. Med. 2007, 52, 81–86. [Google Scholar] [PubMed]
- Hara, N.; Saito-Sasaki, N.; Sawada, Y. Fixed Drug Eruption Caused by Garenoxacin: A Case Report and Literature Review. Cureus 2023, 15, e48596. [Google Scholar] [CrossRef] [PubMed]
- Vargas Mora, P.; García, S.; Valenzuela, F.; Morales, C. Generalized bullous fixed drug eruption successfully treated with cyclosporine. Dermatol. Ther. 2020, 33, e13492. [Google Scholar] [CrossRef] [PubMed]
- Abramowitz, E.W.; Noun, M.H. Fixed drug eruptions. Arch. Dermatol. Syphil 1997, 35, 875–892. [Google Scholar] [CrossRef]
- Matsumoto, K.; Mikoshiba, H.; Saida, T. Nonpigmenting solitary fixed drug eruption caused by a Chinese traditional herbal medicine, ma huang (Ephedra Hebra), mainly containing pseudoephedrine and ephedrine. J. Am. Acad. Dermatol. 2003, 48, 628–630. [Google Scholar] [CrossRef]
- Gupta, L.K.; Beniwal, R.; Khare, A.K.; Mittal, A.; Mehta, S.; Balai, M. Non-pigmenting fixed drug eruption due to fluoroquinolones. Indian J. Dermatol. Venereol. Leprol. 2017, 83, 108–112. [Google Scholar] [CrossRef]
- Singhal, R.R.; Sheth, N.K.; Nair, P.A. Non-Pigmented Fixed Drug Eruption Caused by Ibuprofen. Indian Dermatol. Online J. 2019, 10, 341–343. [Google Scholar]
- Nair, P.A. Ciprofloxacin induced bullous fixed drug reaction: Three case reports. J. Family Med. Prim. Care 2015, 4, 269–272. [Google Scholar] [CrossRef]
- Sinha, M.; Gautam, L.; Shukla, P.K.; Kaur, P.; Sharma, S.; Singh, T.P. Current perspectives in NSAID-induced gastropathy. Mediat. Inflamm. 2013, 2013, 258209. [Google Scholar] [CrossRef]
- Dajani, E.Z.; Islam, K. Cardiovascular and gastrointestinal toxicity of selective cyclo-oxygenase-2 inhibitors in man. J. Physiol. Pharmacol. 2008, 59, 117–133. [Google Scholar]
- Zadrazil, J. Nonsteroidal antiinflammatory drugs and the kidney. Vnitr. Lek. 2006, 52, 686–690. [Google Scholar] [PubMed]
- Risser, A.; Donovan, D.; Heintzman, J.; Page, T. NSAID prescribing precautions. Am. Fam. Physician 2009, 80, 1371–1378. [Google Scholar] [PubMed]
- Sánchez-Morillas, L.; Rojas Pérez-Ezquerra, P.; González Morales, M.L.; González-Mendiola, R.; Laguna Martínez, J.J. Fixed drug eruption due to ibuprofen with patch test positive on the residual lesion. Allergol. Immunopathol. 2013, 41, 203–204. [Google Scholar] [CrossRef] [PubMed]
- Shaker, G.; Mehendale, T.; De La Rosa, C. Fixed Drug Eruption: An Underrecognized Cutaneous Manifestation of a Drug Reaction in the Primary Care Setting. Cureus 2022, 14, e28299. [Google Scholar] [CrossRef]
- Mueller, S.N.; Gebhardt, T.; Carbone, F.R.; Heath, W.R. Memory T cell subsets, migration patterns, and tissue residence. Annu. Rev. Immunol. 2013, 31, 137–161. [Google Scholar] [CrossRef]
- Shiohara, T. Fixed drug eruption: Pathogenesis and diagnostic tests. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 316–321. [Google Scholar] [CrossRef]
- Mizukawa, Y.; Yamazaki, Y.; Shiohara, T. In vivo dynamics of intraepidermal CD8+ T cells and CD4+ T cells during the evolution of fixed drug eruption. Br. J. Dermatol. 2008, 158, 1230–1238. [Google Scholar] [CrossRef]
- Rönnau, A.C.; Sachs, B.; von Schmiedeberg, S.; Hunzelmann, N.; Ruzicka, T.; Gleichmann, E.; Schuppe, H.C. Cutaneous adverse reaction to ciprofloxacin: Demonstration of specific lymphocyte proliferation and cross-reactivity to ofloxacin in vitro. Acta Derm. Venereol. 1997, 77, 285–288. [Google Scholar] [CrossRef]
- Teraki, Y.; Shiohara, T. IFN-gamma-producing effector CD8+ T cells and IL-10-producing regulatory CD4+ T cells in fixed drug eruption. J. Allergy Clin. Immunol. 2003, 112, 609–615. [Google Scholar] [CrossRef]
- Mizukawa, Y.; Shiohara, T. Fixed drug eruption: A prototypic disorder mediated by effector memory T cells. Curr. Allergy Asthma Rep. 2009, 9, 71–77. [Google Scholar] [CrossRef]
- Hanafusa, T.; Azukizawa, H.; Matsumura, S.; Murakami, Y.; Tanaka, A.; Kurachi, K.; Katayama, I. Non-pigmenting fixed drug eruption caused by an over-the-counter non-steroidal anti-inflammatory drug: Drug-specific CD8+ T lymphocytes identified in peripheral blood. Eur. J. Dermatol. 2012, 22, 680–682. [Google Scholar] [CrossRef] [PubMed]
- Kuligowski, M.E.; Chang, A.; Rath, R. Multiple fixed drug eruption due to ibuprofen. Contact Dermat. 1991, 25, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Malviya, N.; Cyrus, N.; Vandergriff, T.; Mauskar, M. Generalized bullous fixed drug eruption treated with cyclosporine. Dermatol. Online J. 2017, 23, 8. [Google Scholar] [CrossRef]
- Fazeli, S.A.; Abbasi, M.; Jalali, H.; Eskandari, S.; Shamshirgaran, F.; Dehghani, Z.; Golabchifard, R.; Ghiyasvand, S.; Ghannad, K. Bullous Fixed Drug Eruption Following Ibuprofen Ingestion. J. Res. Pharm. Pract. 2018, 7, 51–56. [Google Scholar]
- Tavares Almeida, F.; Caldas, R.; André Oliveira, Á.; Pardal, J.; Pereira, T.; Brito, C. Generalized bullous fixed drug eruption caused by ibuprofen. Contact Dermat. 2019, 80, 238–239. [Google Scholar] [CrossRef]
- Barootes, H.C.; Peebles, E.R.; Matsui, D.; Rieder, M.; Abuzgaia, A.; Mohammed, J.A. Severe Generalized Bullous Fixed Drug Eruption Treated with Cyclosporine: A Case Report and Literature Review. Case Rep. Dermatol. 2021, 13, 154–163. [Google Scholar] [CrossRef]
- Yadav, P.; Bhatia, R.; Vasisht, S.; Sethi, J. Patch test with multiple antipyretics in a case of fixed drug eruption in a child. Contact Dermat. 2024, 90, 422–423. [Google Scholar] [CrossRef]
- Anderson, H.J.; Lee, J.B. A Review of Fixed Drug Eruption with a Special Focus on Generalized Bullous Fixed Drug Eruption. Medicina (Kaunas) 2021, 57, 925. [Google Scholar] [CrossRef]
- Lerch, M.; Mainetti, C.; Terziroli Beretta-Piccoli, B.; Harr, T. Current Perspectives on Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clin. Rev. Allergy Immunol. 2018, 54, 147–176. [Google Scholar] [CrossRef]
- Drago, F.; Cogorno, L.; Agnoletti, A.F.; Ciccarese, G.; Parodi, A. A retrospective study of cutaneous drug reactions in an outpatient population. Int. J. Clin. Pharm. 2015, 37, 739–743. [Google Scholar] [CrossRef]
- Phillips, E.J.; Bigliardi, P.; Bircher, A.J.; Broyles, A.; Chang, Y.S.; Chung, W.H.; Lehloenya, R.; Mockenhaupt, M.; Peter, J.; Pirmohamed, M.; et al. Controversies in drug allergy: Testing for delayed reactions. J. Allergy Clin. Immunol. 2019, 143, 66–73. [Google Scholar] [CrossRef]
- Katoh, Y.; Natsume, O.; Matsunaga, M.; Takayanagi, F.; Uchida, H.; Yasuoka, R. Diagnosis of non-immediate hypersensitivity to amoxicillin in children by skin test and drug provocation tests: A retrospective case-series study. Allergol. Int. 2022, 71, 131–136. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions, and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |



| Age | Sex | Past Medical History | Onset After Drug Intake | Experience of Repeated Rash Emergence | Skin Manifestation | Region of Rash | Treatment | Basis for Diagnosis | |
|---|---|---|---|---|---|---|---|---|---|
| Kuligowski ME et al. [32] | 49 | Female | None | Unknown | None | Edematous erythema | Extremities | None | Patch test |
| Chen JF et al. [4] | 29 | Male | None | 6 h | None | Dusky red patches with a few overlying blisters and erosions | Trunk, proximal extremities, lip, and foreskin | None | Clinical course |
| Sánchez-Morillas L et al. [23] | 64 | Male | None | A few hours | None | Pruritic erythematous macules | Trunk, extremities, and oral mucosa | None | Patch test |
| Dharamsi FM et al. [8] | 30 | Male | None | 24 h | Yes | Hyperpigmented plaques, some with inlying blisters and erosions | Lips, eyelids, penis, and scrotum | None | Clinical course |
| Malviya N et al. [33] | 40 | Male | Asthma | 24 h | Yes | Erythematous to violaceous oval macules, coalescing into confluent patches | Trunk, extremities, and periorbital area | Intravenous cyclosporine | Clinical course |
| Fazeli SA et al. [34] | 65 | Male | None | 24 h | None | Erythematous lesion and oral ulcer | Trunk, extremities, and oral mucosa | Oral corticosteroid and antihistamines, and topical corticosteroids | Clinical course |
| Singhal RR et al. [17] | 71 | Female | Diabetes mellitus and hypertension | Unknown | Yes | Erythematous lesions, healed with no pigmentation | Trunk and extremities | None | Clinical course |
| Tavares Almeida F et al. [35] | 47 | Female | None | Unknown | None | Annular erythematous plaques with vesicles and pustules | Trunk and extremities | None | Patch test |
| Bhanja DB et al. [6] | 20 | Male | None | 24 h | Yes | Bullous lesions and erosion | Trunk, extremities, oral mucosa, glans penis, and lips | Oral corticosteroid and antihistamines, and topical corticosteroids | Clinical course |
| Barootes HC et al. [36] | 7 | Female | None | 4 days | Yes | Erythematous-to-brown patches | Trunk and extremities | Oral corticosteroid and cyclosporine | Drug-induced lymphocyte stimulation test |
| Shaker G et al. [24] | 33 | Female | Hypertension, diabetes, and dysmenorrhea | 6 h | Yes | Circular patches with a dusky violaceous appearance and surrounding rings of erythema | Trunk and extremities | Topical corticosteroids | Clinical course |
| Yadav P et al. [37] | 10 | Male | None | 24 h | None | Edematous erythema | Face and trunk | None | Patch test |
| Our case | 23 | Male | None | 4 h | Yes | Edematous erythema or erythematous patches, some with hyperpigmentation | Trunk and extremities | Topical corticosteroids | Clinical course (reproduction of the rash immediately after taking the causative drug) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mima, Y.; Yamamoto, M.; Obikane, H.; Norimatsu, Y.; Iozumi, K. Ibuprofen-Induced Multiple Fixed Drug Eruption Confirmed by Re-Challenge: A Case Report and Literature Review. Diagnostics 2025, 15, 48. https://doi.org/10.3390/diagnostics15010048
Mima Y, Yamamoto M, Obikane H, Norimatsu Y, Iozumi K. Ibuprofen-Induced Multiple Fixed Drug Eruption Confirmed by Re-Challenge: A Case Report and Literature Review. Diagnostics. 2025; 15(1):48. https://doi.org/10.3390/diagnostics15010048
Chicago/Turabian StyleMima, Yoshihito, Masako Yamamoto, Hiyo Obikane, Yuta Norimatsu, and Ken Iozumi. 2025. "Ibuprofen-Induced Multiple Fixed Drug Eruption Confirmed by Re-Challenge: A Case Report and Literature Review" Diagnostics 15, no. 1: 48. https://doi.org/10.3390/diagnostics15010048
APA StyleMima, Y., Yamamoto, M., Obikane, H., Norimatsu, Y., & Iozumi, K. (2025). Ibuprofen-Induced Multiple Fixed Drug Eruption Confirmed by Re-Challenge: A Case Report and Literature Review. Diagnostics, 15(1), 48. https://doi.org/10.3390/diagnostics15010048






