Comprehensive Oral Diagnosis and Management for Women with Turner Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Dental Conditions Recorded
2.3. Statistical Analysis
3. Results
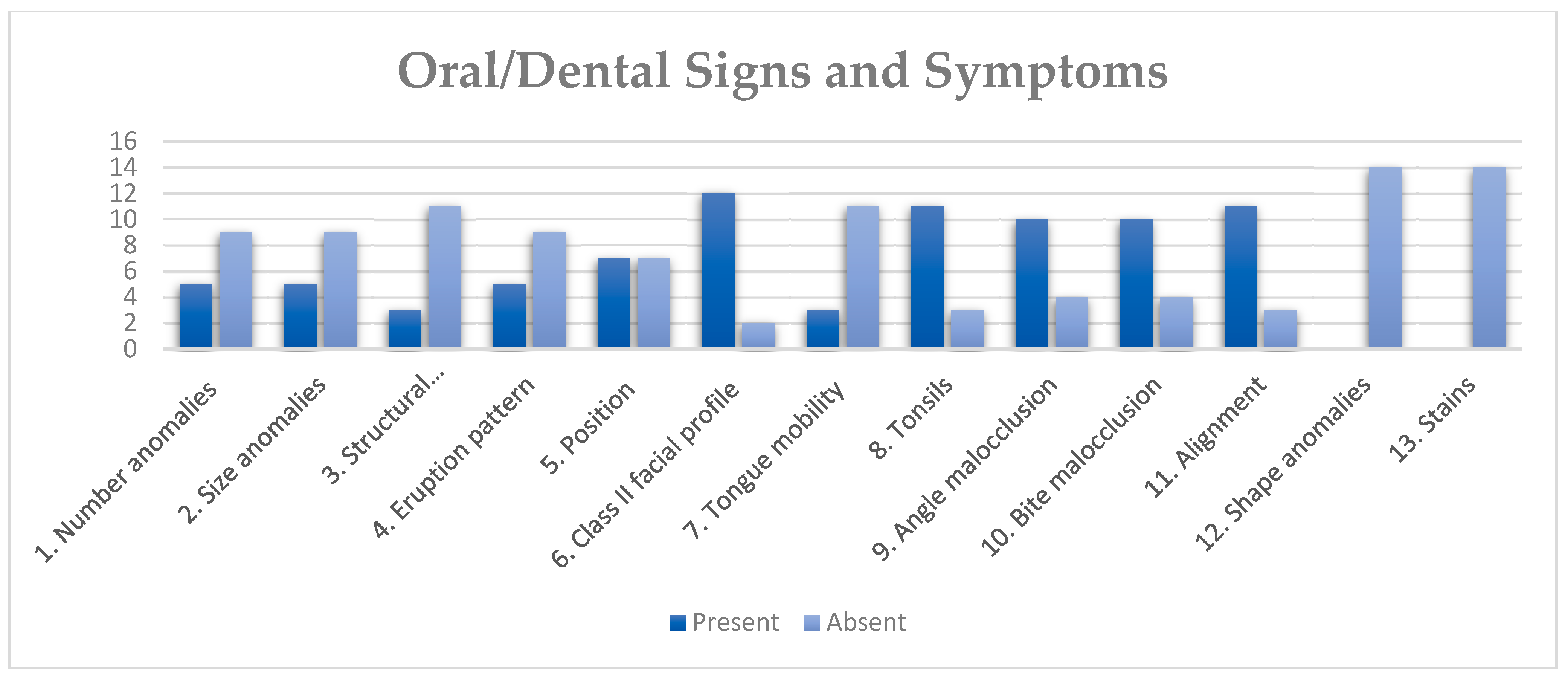
3.1. Clinical Findings
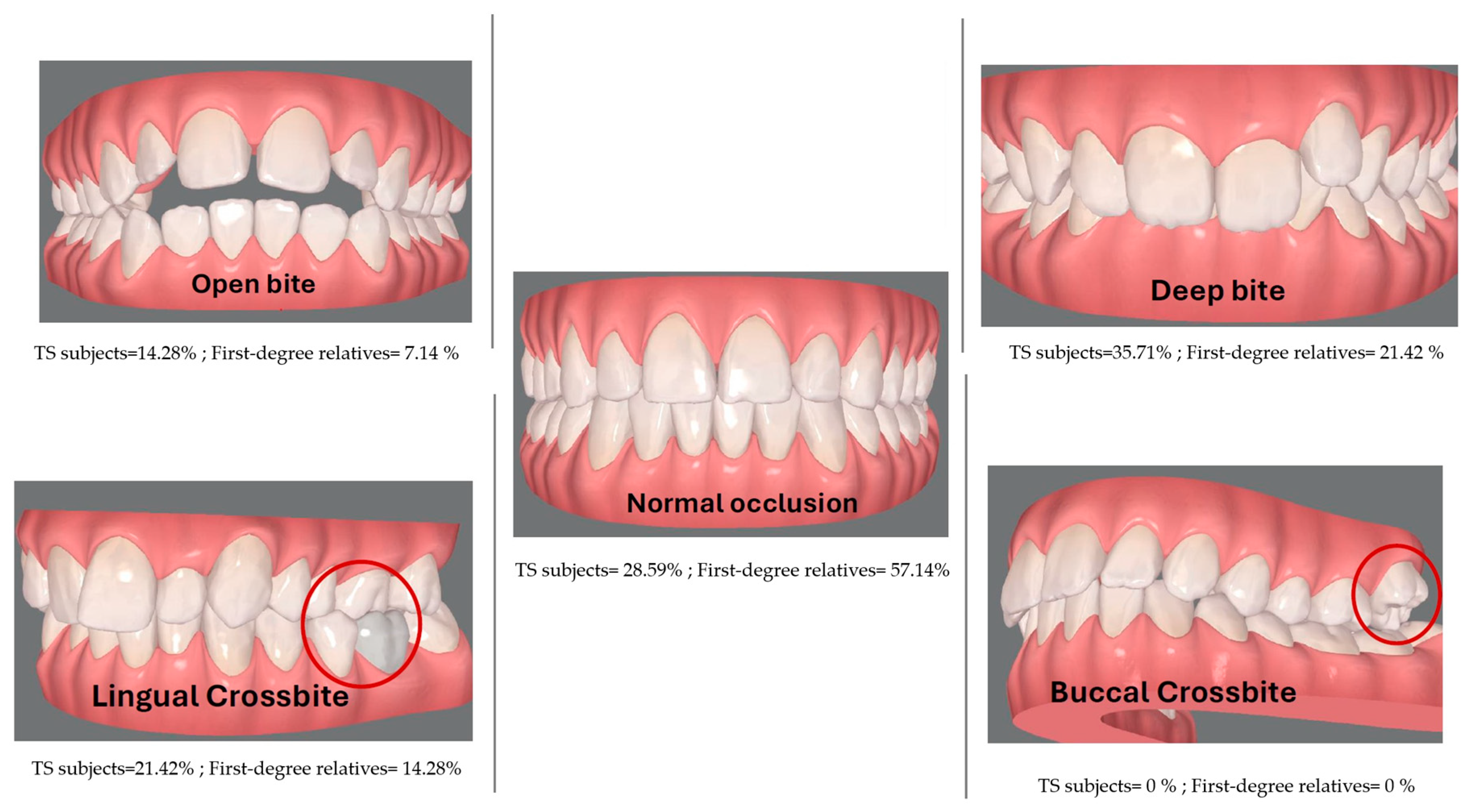
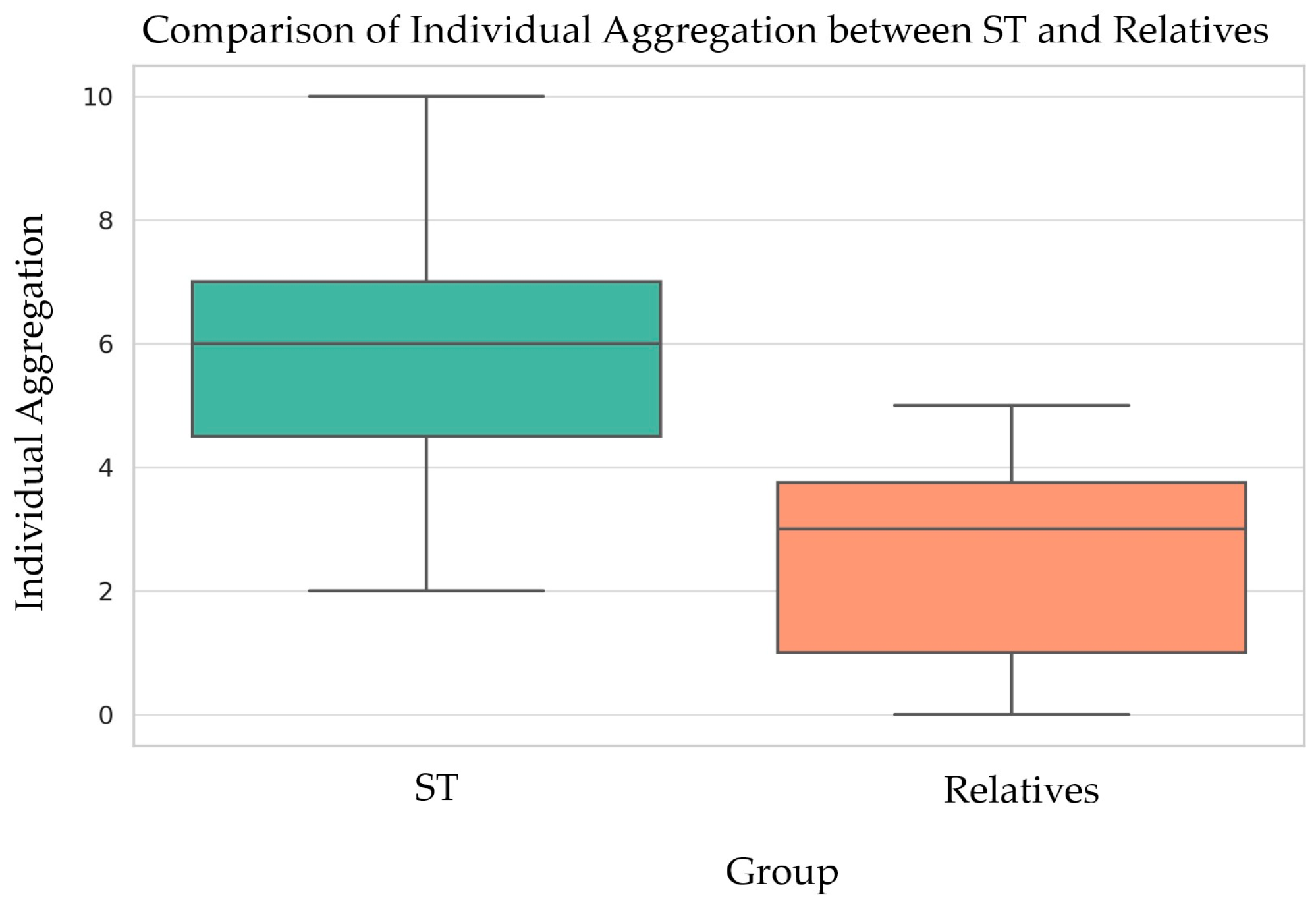
3.2. Dento-Craniofacial Findings
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nielsen, J.; Wohlert, M. Chromosome abnormalities found among 34,910 newborn children: Results from a 13-year incidence study in Arhus, Denmark. Hum. Genet. 1991, 87, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Gardner, R.J.M.; Amor, D.J. Gardner and Sutherland’s Chromosome Abnormalities and Genetic Counseling, 5th ed.; Oxford University Press: Oxford, UK, 2018; pp. 1–7. [Google Scholar]
- Berglund, A.; Stochholm, K.; Gravholt, C.H. The epidemiology of sex chromosome abnormalities. Am. J. Med. Genet. Part C Semin. Med. Genet. 2020, 184, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Brun, J.L.; Gangbo, F.; Wen, Z.Q.; Galant, K.; Taine, L.; Maugey-Laulom, B.; Roux, D.; Mangione, R.; Horovitz, J.; Saura, R. Prenatal diagnosis and management of sex chromosome aneuploidy: A report on 98 cases. Prenat. Diagn. 2004, 24, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Gunther, D.F.; Eugster, E.; Zagar, A.J.; Bryant, C.G.; Davenport, M.L.; Quigley, C.A. Ascertainment Bias in Turner Syndrome: New Insights From Girls Who Were Diagnosed Incidentally in Prenatal Life. Pediatrics 2004, 114, 640–644. [Google Scholar] [CrossRef] [PubMed]
- Stochholm, K.; Juul, S.; Juel, K.; Naeraa, R.W.; Gravholt, C.H. Prevalence, Incidence, Diagnostic Delay, and Mortality in Turner Syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 3897–3902. [Google Scholar] [CrossRef] [PubMed]
- Berglund, A.; Viuff, M.H.; Skakkebæk, A.; Chang, S.; Stochholm, K.; Gravholt, C.H. Changes in the cohort composition of turner syndrome and severe non-diagnosis of Klinefelter, 47,XXX and 47,XYY syndrome: A nationwide cohort study. Orphanet J. Rare Dis. 2019, 14, 16. [Google Scholar] [CrossRef] [PubMed]
- Gravholt, C.H.; Andersen, N.H.; Conway, G.S.; Dekkers, O.M.; Geffner, M.E.; Klein, K.O.; Lin, A.E.; Mauras, N.; Quigley, C.A.; Rubin, K.; et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: Proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur. J. Endocrinol. 2017, 177, G1–G70. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Viuff, M.; Just, J.; Sandahl, K.; Brun, S.; Van Der Velden, J.; Andersen, N.H.; Skakkebaek, A. The Changing Face of Turner Syndrome. Endocr. Rev. 2023, 44, 33–69. [Google Scholar] [CrossRef]
- Frelich, J.; Irzyniec, T.; Lepska, K.; Jeż, W. New insights into clinical features, karyotypes, and age at diagnosis in women with Turner syndrome. Endokrynol. Pol. 2019, 70, 342–349. [Google Scholar] [CrossRef]
- Witkowska-Krawczak, E.; Erazmus, M.; Majcher, A.; Pyrżak, B.; Kucharska, A.M. Predicted health care profile after transition to adult care in Turner syndrome children—Experience of single center. Front. Pediatr. 2023, 11, 1173419. [Google Scholar] [CrossRef]
- Lin, A.E.; Prakash, S.K.; Andersen, N.H.; Viuff, M.H.; Levitsky, L.L.; Rivera-Davila, M.; Crenshaw, M.L.; Hansen, L.; Colvin, M.K.; Hayes, F.J.; et al. Recognition and management of adults with Turner syndrome: From the transition of adolescence through the senior years. Am. J. Med. Genet. 2019, 179, 1987–2033. [Google Scholar] [CrossRef] [PubMed]
- Bagattoni, S.; Lardani, L.; Vanni, A.; Costi, T. Craniofacial and occlusal features of individuals with Turner Syndrome: A cephalometric study. J. Biol. Regul. Homeost. Agents. 2021, 35, 95–106. [Google Scholar] [PubMed]
- Svanberg, C.; Norevall, L.I.; Ekman, B.; Wahlberg, J.; Bågesund, M. Cephalometric analysis of adults with Turner syndrome. Swed. Dent. J. 2016, 40, 33–41. [Google Scholar] [PubMed]
- Cazzolla, A.P.; Lo Muzio, L.; Di Fede, O.; Lacarbonara, V.; Colaprico, A.; Testa, N.F.; Giuseppe, T.; Zhurakivska, K.; Marzo, G.; Lacaita, M.G. Orthopedic-orthodontic treatment of the subject with Turner’s syndrome: Review of the literature and case report. Spec. Care Dentist. 2018, 38, 239–248. [Google Scholar] [CrossRef] [PubMed]
- Juloski, J.; Dumančić, J.; Šćepan, I.; Lauc, T.; Milašin, J.; Kaić, Z.; Dumić, M.; Babić, M. Growth hormone positive effects on craniofacial complex in Turner syndrome. Arch. Oral Biol. 2016, 71, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Wójcik, D.; Beń-Skowronek, I. Craniofacial Morphology in Children with Growth Hormone Deficiency and Turner Syndrome. Diagnostics 2020, 10, 88. [Google Scholar] [CrossRef]
- Redhead, Y.; Gibbins, D.; Lana-Elola, E.; Watson-Scales, S.; Dobson, L.; Krause, M.; Liu, K.J.; Fisher, E.M.C.; Green, J.B.A.; Tbulewicz, V.L.J. Craniofacial dysmorphology in Down syndrome is caused by increased dosage of Dyrk1a and at least three other genes. Development. 2023, 150, dev201077. [Google Scholar] [CrossRef]
- Morice, A.; Taverne, M.; Eché, S.; Griffon, L.; Fauroux, B.; Leboulanger, N.; Couloigner, V.; Baujat, G.; Cormier-Daire, V.; Picard, A.; et al. Craniofacial growth and function in achondroplasia: A multimodal 3D study on 15 subjects. Orphanet J. Rare Dis. 2023, 18, 88. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.L.; Li, F.; Chen, W.; Liu, L.; Cheng, H.J.; He, Z.X.; Ai, R. “Liu-Liang-Chung” syndrome with multiple congenital anomalies and the distinctive craniofacial features caused by dominant ZEB2 gene gain mutation. BMC Pediatr. 2023, 23, 480. [Google Scholar] [CrossRef]
- Dumancic, J.; Kaic, Z.; Varga, M.L.; Lauc, T.; Dumic, M.; Milosevic, S.A.; Brkic, H. Characteristics of the craniofacial complex in Turner syndrome. Arch. Oral Biol. 2010, 55, 81–88. [Google Scholar] [CrossRef]
- Perkiomaki, M.R.; Kyrkanides, S.; Niinimaa, A.; Alvesalo, L. The relationship of distinct craniofacial features between Turner syndrome females and their parents. Eur. J. Orthod. 2005, 27, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Kusiak, A.; Sadlak, N.J.; Limon, J.; Kochanska, B. Root morphology of mandibular premolars in 40 subjects with Turner syndrome. Int. Endod. J. 2005, 38, 822–826. [Google Scholar] [CrossRef] [PubMed]
- Townsend, G.; Jensen, B.L.; Alvesalo, L. Reduced tooth size in 45,X (Turner syndrome) females. Am. J. Phys. Anthropol. 1984, 65, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Maier, C.; Dumančić, J.; Brkić, H.; Kaić, Z.; Savić Pavičin, I.; Poje, Z.; Scott, G.R. Tooth Crown Morphology in Turner and Klinefelter Syndrome Individuals from a Croatian Sample. Acta Stomatol. Croat. 2019, 53, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Durán Von Arx, J.; Merino Arends, M.; Echarri, P.; Carrasco, P. Tabla de diagnóstico y tratamiento Multifuncion System “MSF”, herramienta básica de la estimuloterapia programada. DENTUM 2009, 9, 119–125. [Google Scholar]
- Durán Von Arx, J.; Ustrell Torrent, M.J. Técnica, M.S.F. Diagnóstico de la matriz functional: Codificación. Ortodon. Clin. 2003, 6, 138–140. [Google Scholar]
- Pinho, T.; Maciel, P.; Lemos, C.; Sousa, A. Familial aggregation of maxillary lateral incisor agenesis. J. Dent. Res. 2010, 89, 621–625. [Google Scholar] [CrossRef] [PubMed]
- Tallón-Walton, V.; Nieminen, P.; Arte, S.; Ustrell-Torrent, J.M.; Carvalho-Lobato, P.; Manzanares-Céspedes, M.C. Oral findings in Midline Syndrome: A case report and literature review. Med Oral Patol Oral Cir Bucal. 2010, 15, e579–e582. [Google Scholar] [CrossRef][Green Version]
- Grandi, D. The “Interdisciplinary Orofacial Examination Protocol for Children and Adolescents”: A resource for the interdisciplinary assessment of the stomatognatic system. Int. J. Orofac. Myol. 2012, 38, 15–26. [Google Scholar] [CrossRef]
- De La Dure-Molla, M.; Fournier, B.P.; Manzanares, M.C.; Acevedo, A.C.; Hennekam, R.C.; Friedlander, L.; Boy-Lefèvre, M.L.; Kerner, S.; Toupenay, S.; Garrec, P.; et al. Elements of morphology: Standard terminology for the teeth and classifying genetic dental disorders. Am. J. Med. Genet. A. 2019, 179, 1913–1981. [Google Scholar] [CrossRef]
- ORPHANET. Available online: https://www.orpha.net/es/disease/detail/881?name=S%C3%ADndrome%20de%20Turner&mode=name (accessed on 26 March 2024).
- Human Phenotype Ontology (HPO). Available online: https://hpo.jax.org/app/browse/term/HP:0000347 (accessed on 26 March 2024).
- Kruszka, P.; Addissie, Y.A.; Tekendo-Ngongang, C.; Jones, K.L.; Savage, S.K.; Gupta, N.; Sirisena, N.D.; Dissanayake, V.H.W.; Paththinige, C.S.; Aravena, T.; et al. Turner syndrome in diverse populations. Am. J. Med. Genet. A. 2020, 182, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.D.; Bamba, V.; Bothwell, S.; Fechner, P.Y.; Furniss, A.; Ikomi, C.; Nahata, L.; Nokoff, N.J.; Pyle, L.; Seyoum, H.; et al. Development and Validation of a Computable Phenotype for Turner Syndrome Utilizing Electronic Health Records from a National Pediatric Network. medRxiv. 2023. preprint. [Google Scholar] [CrossRef]
- Bilge, N.H.; Yeşiltepe, S.; Törenek Ağırman, K.; Çağlayan, F.; Bilge, O.M. Investigation of prevalence of dental anomalies by using digital panoramic radiographs. Folia Morphol. 2018, 77, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Wagner, V.P.; Arrué, T.; Hilgert, E.; Arús, N.A.; Da Silveira, H.L.D.; Martins, M.D.; Rodrigues, J.A. Prevalence and distribution of dental anomalies in a paediatric population based on panoramic radiographs analysis. Eur. J. Paediatr. Dent. 2020, 21, 292–298. [Google Scholar] [PubMed]
- Sella Tunis, T.; Sarne, O.; Hershkovitz, I.; Finkelstein, T.; Pavlidi, A.M.; Shapira, Y.; Davidovitch, M.; Shpack, N. Dental Anomalies’ Characteristics. Diagnostics 2021, 11, 1161. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P.; Ansari, A.A.; Choudhary, K.; Saxena, A. Familial aggregation of maxillary lateral incisor agenesis (MLIA). BMJ Case Rep. 2013, 26, bcr2012007846. [Google Scholar] [CrossRef] [PubMed]
- Jeong, K.H.; Kim, D.; Song, Y.M.; Sung, J.; Kim, Y.H. Epidemiology and genetics of hypodontia and microdontia: A study of twin families. Angle Orthod. 2015, 85, 980–985. [Google Scholar] [CrossRef]
- Kantaputra, P.; Jatooratthawichot, P.; Chintakanon, K.; Intachai, W.; Pradermdutsadeeporn, P.; Adisornkanj, P.; Tongsima, S.; Ngamphiw, C.; Olsen, B.; Tucker, A.S.; et al. Mutations in LRP6 highlight the role of WNT signaling in oral exostoses and dental anomalies. Arch Oral Biol. 2022, 142, 105514. [Google Scholar] [CrossRef]
- Salanitri, S.; Seow, W.K. Developmental enamel defects in the primary dentition: Aetiology and clinical management. Aust. Dent. J. 2013, 58, 133–140. [Google Scholar] [CrossRef]
- Vélez-León, E.; Albaladejo-Martínez, A.; Pacheco-Quito, E.M.; Armas-Vega, A.; Delgado-Gaete, A.; Pesántez-Ochoa, D.; Melo, M. Developmental Enamel Defects in Children from the Southern Region of Ecuador. Children 2022, 9, 1755. [Google Scholar] [CrossRef]
- Reis, C.L.B.; Barbosa, M.C.F.; De Lima, D.C.; Brancher, J.A.; Lopes, C.M.C.F.; Baratto-Filho, F.; Küchler, E.C.; De Oliveira, D.S.B. Risk factors for developmental defects of enamel in children from southeastern Brazil. Community Dent. Health 2021, 38, 178–181. [Google Scholar] [PubMed]
- Torlińska-Walkowiak, N.; Majewska, K.A.; Sowińska, A.; Kędzia, A.; Opydo-Szymaczek, J. Developmental enamel defects and dental anomalies of number and size in children with growth hormone deficiency. Sci. Rep. 2023, 13, 14707. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, M.; Lähdesmäki, R.; Niinimaa, A.; Alvesalo, L. Molar morphology and the expression of Carabelli’s trait in 45,X females. Am. J. Hum. Biol. 2015, 27, 486–493. [Google Scholar] [CrossRef]
- Torlińska-Walkowiak, N.; Majewska, K.A.; Sowińska, A.; Kędzia, A.; Opydo-Szymaczek, J. Skeletal and dental age discrepancy and occlusal traits in children with growth hormone deficiency and idiopathic short stature. Clin. Oral Investig. 2022, 26, 6165–6175. [Google Scholar] [CrossRef] [PubMed]
- Torlińska-Walkowiak, N.; Majewska, K.A.; Kędzia, A.; Opydo-Szymaczek, J. Clinical Implications of Growth Hormone Deficiency for Oral Health in Children: A Systematic Review. J. Clin Med. 2021, 10, 3733. [Google Scholar] [CrossRef] [PubMed]
- Drenski Balija, N.; Aurer, B.; Meštrović, S.; Lapter Varga, M. Prevalence of Dental Anomalies in Orthodontic Subjects. Acta Stomatol. Croat. 2022, 56, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Vinjolli, F.; Zeqaj, M.; Dragusha, E.; Malara, A.; Danesi, C.; Laganà, G. Dental anomalies in an Albanian orthodontic sample: A retrospective study. BMC Oral Health. 2023, 23, 47. [Google Scholar] [CrossRef]
- Laganà, G.; Venza, N.; Borzabadi-Farahani, A.; Fabi, F.; Danesi, C.; Cozza, P. Dental anomalies: Prevalence and associations between them in a large sample of non-orthodontic subjects, a cross-sectional study. BMC Oral Health. 2017, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Ashoori, N.; Ghorbanyjavadpour, F.; Rakhshan, V. Associations between 44 nonmetric permanent dental traits or anomalies with skeletal sagittal malocclusions and sex, besides correlations across the variations or abnormalities. BMC Oral Health. 2022, 22, 544. [Google Scholar] [CrossRef]
- Salerno, C.; D’Avola, V.; Oberti, L.; Almonte, E.; Bazzini, E.M.; Tartaglia, G.M.; Cagetti, M.G. Rare Genetic Syndromes and Oral Anomalies: A Review of the Literature and Case Series with a New Classification Proposal. Children 2021, 9, 12. [Google Scholar] [CrossRef]
- Vahid-Dastjerdi, E.; Borzabadi-Farahani, A.; Mahdian, M.; Amini, N. Non-syndromic hypodontia in an Iranian orthodontic population. J. Oral. Sci. 2010, 52, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Vahid-Dastjerdi, E.; Borzabadi-Farahani, A.; Mahdian, M.; Amini, N. Supernumerary teeth amongst Iranian orthodontic patients. A retrospective radiographic and clinical survey. Acta Odontol. Scand. 2011, 69, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Golovcencu, L.; Romanec, C.; Martu, M.A.; Anistoroaiei, D.; Pacurar, M. Particularities of orthodontic treatment in patients with dental anomalies that need orthodontic-restorative therapeutic approach. Rev. Chim. 2019, 70, 3046–3049. [Google Scholar] [CrossRef]

| ID | Number + Size + Shape + Structure + Position + Alignment | Malocclusion | Tongue Mobility + Tonsils | Class II Facial Profile | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TS Subject | % Signs | % First-Degree Relatives (Mother|Father) | % Signs | % in First-Degree Relatives (Mother|Father) | % Signs | % in First-Degree Relatives (Mother|Father) | % signs | % in First-Degree Relatives (Mother|Father) | |||||
| ESTM0003 | 50% | NA | 100% | NA | 50% | NA | 0% | NA | |||||
| ESTM0016 | 33% | NA | 50% | NA | 0% | NA | 100% | NA | |||||
| ESTM0021 | 0% | 33% | 0% | 0% | 50% | 0% | 0% | 0% | |||||
| ESTM0022 | 50% | 17% | 17% | 100% | 50% | 50% | 50% | 0% | 0% | 100% | 0% | 0% | |
| ESTM0026 | 66% | NA | 100% | NA | 100% | NA | 100% | NA | |||||
| ESTM0027 | 33% | NA | 100% | NA | 50% | NA | 100% | NA | |||||
| ESTM0028 | 33% | 50% | 100% | 100% | 50% | 0% | 100% | 0% | |||||
| ESTM0030 | 50% | NA | 100% | NA | 50% | NA | 100% | NA | |||||
| ESTM0031 | 50% | 0% | 33% | 100% | 50% | 0% | 50% | 0% | 0% | 100% | 0% | 100% | |
| ESTM0034 | 33% | 33% | 17% | 50% | 0% | 0% | 0% | 0% | 50% | 100% | 0% | 0% | |
| ESTM0037 | 50% | 17% | 50% | 100% | 50% | 0% | 100% | 100% | |||||
| ESTM0041 | 16% | 17% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 100% | 0% | 0% | |
| ESTM0045 | 33% | 0% | 50% | 0% | 100% | 0% | 100% | 0% | |||||
| ESTM0047 | 16% | NA | 100% | NA | 100% | NA | 100% | NA | |||||
| Average | 37% | 24% | 71% | 29% | 50% | 4% | 86% | 16% | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tallón-Walton, V.; Sánchez-Molins, M.; Hu, W.; Martínez-Abadías, N.; Casado, A.; Manzanares-Céspedes, M.C. Comprehensive Oral Diagnosis and Management for Women with Turner Syndrome. Diagnostics 2024, 14, 769. https://doi.org/10.3390/diagnostics14070769
Tallón-Walton V, Sánchez-Molins M, Hu W, Martínez-Abadías N, Casado A, Manzanares-Céspedes MC. Comprehensive Oral Diagnosis and Management for Women with Turner Syndrome. Diagnostics. 2024; 14(7):769. https://doi.org/10.3390/diagnostics14070769
Chicago/Turabian StyleTallón-Walton, Victoria, Meritxell Sánchez-Molins, Wenwen Hu, Neus Martínez-Abadías, Aroa Casado, and María Cristina Manzanares-Céspedes. 2024. "Comprehensive Oral Diagnosis and Management for Women with Turner Syndrome" Diagnostics 14, no. 7: 769. https://doi.org/10.3390/diagnostics14070769
APA StyleTallón-Walton, V., Sánchez-Molins, M., Hu, W., Martínez-Abadías, N., Casado, A., & Manzanares-Céspedes, M. C. (2024). Comprehensive Oral Diagnosis and Management for Women with Turner Syndrome. Diagnostics, 14(7), 769. https://doi.org/10.3390/diagnostics14070769







