Diagnostic and Prognostic Value of Thrombocytopenia in Severe Burn Injuries
Abstract
1. Introduction
2. Materials and Methods
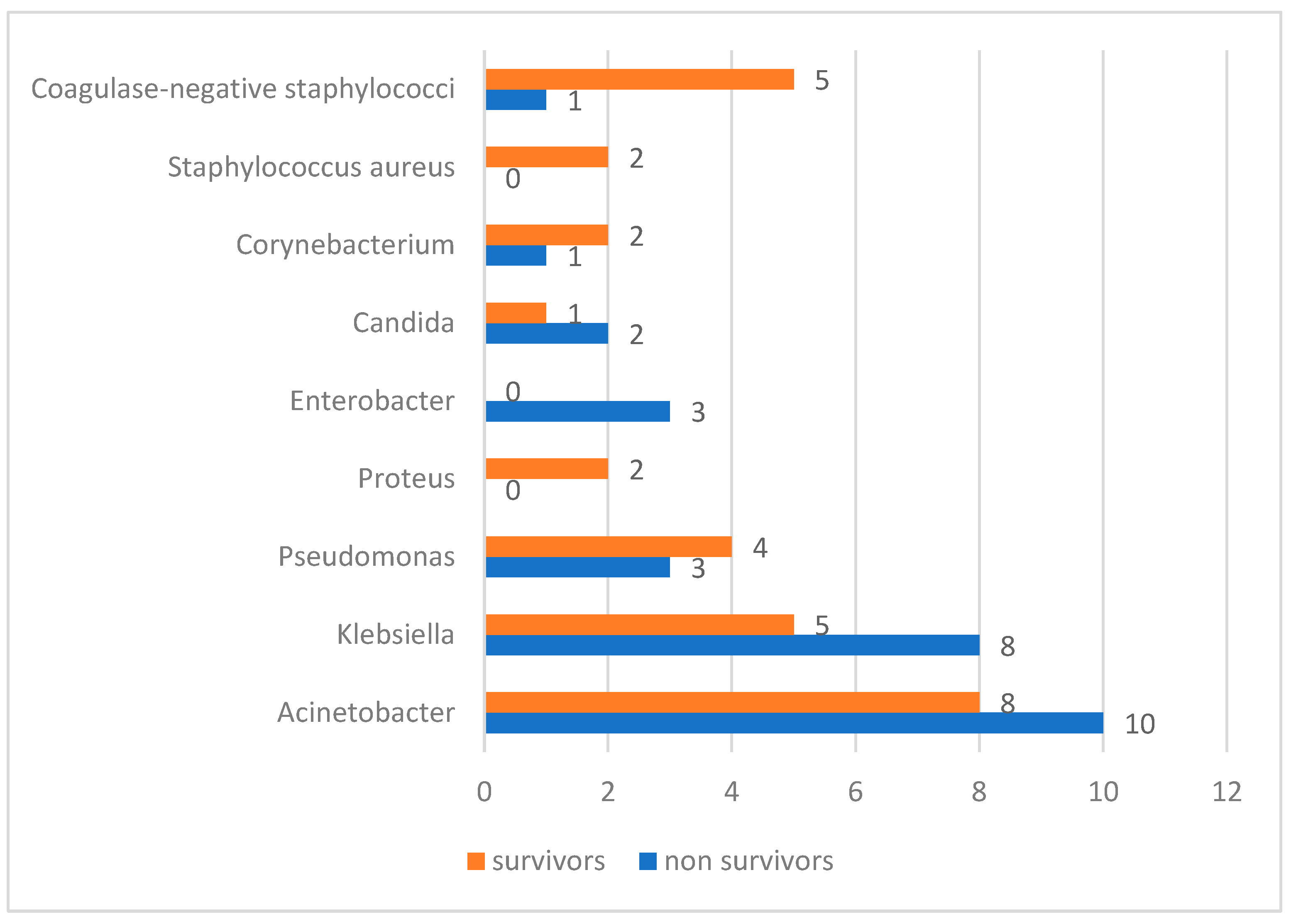
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Żwierełło, W.; Piorun, K.; Skórka-Majewicz, M.; Maruszewska, A.; Antoniewski, J.; Gutowska, I. Burns: Classification, Pathophysiology, and Treatment: A Review. Int. J. Mol. Sci. 2023, 24, 3749. [Google Scholar] [CrossRef]
- Datta, P.K.; Roy Chowdhury, S.; Aravindan, A.; Saha, S.; Rapaka, S. Medical and Surgical Care of Critical Burn Patients: A Comprehensive Review of Current Evidence and Practice. Cureus 2022, 14, e31550. [Google Scholar] [CrossRef]
- Pavic, M.; Milevoj, L. Platelet count monitoring in burn patients. Biochem. Medica 2007, 17, 212–219. [Google Scholar] [CrossRef]
- Semple, J.W.; Italiano, J.E.; Freedman, J. Platelets and the immune continuum. Nat. Rev. Immunol. 2011, 11, 264–274. [Google Scholar] [CrossRef]
- Li, Z.; Yang, F.; Dunn, S.; Gross, A.K.; Smyth, S.S. Platelets as immune mediators: Their role in host defense responses and sepsis. Thromb. Res. 2011, 127, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.R.; Lesur, O.; Tétrault, J.P.; Nault, V.; Pilon, D. Thrombocytopenia in the critically ill: Prevalence, incidence, risk factors, and clinical outcomes. Can. J. Anaesth. 2013, 60, 641–651. [Google Scholar] [CrossRef] [PubMed]
- Hui, P.; Cook, D.J.; Lim, W.; Fraser, G.A.; Arnold, D.M. The frequency and clinical significance of thrombocytopenia complicating critical illness: A systematic review. Chest 2011, 139, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Strauss, R.; Wehler, M.; Mehler, K.; Kreutzer, D.; Koebnick, C.; Hahn, E.G. Thrombocytopenia in patients in the medical intensive care unit: Bleeding prevalence, transfusion requirements, and outcome. Crit. Care Med. 2002, 30, 1765–1771. [Google Scholar] [CrossRef]
- El-Sonbaty, M.A.; El-Otiefy, M.A. Haematological change in severely burn patients. Ann. Burns Fire Disasters 1996, 9, 1–4. [Google Scholar]
- Wang, Y.; Tang, H.T.; Xia, Z.F.; Zhu, S.H.; Ma, B.; Wei, W.; Sun, Y.; Lv, K.Y. Factors affecting survival in adult patients with massive burns. Burns 2010, 36, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Thiery-Antier, N.; Binquet, C.; Vinault, S.; Meziani, F.; Boisramé-Helms, J.; Quenot, J.-P. Is thrombocytopenia an early prognostic marker in septic shock? Crit. Care Med. 2016, 44, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Venkata, C.; Kashyap, R.; Farmer, J.C.; Afessa, B. Thrombocytopenia in adult patients with sepsis: Incidence, risk factors, and its association with clinical outcome. J. Intensive Care 2013, 1, 9. [Google Scholar] [CrossRef]
- Vanderschueren, S.; De Weerdt, A.; Malbrain, M.; Vankersschaever, D.; Frans, E.; Wilmer, A.; Bobbaers, H. Thrombocytopenia and prognosis in intensive care. Crit. Care Med. 2000, 28, 1871–1876. [Google Scholar] [CrossRef]
- Mavrommatis, A.C.; Theodoridis, T.; Orfanidou, A.; Roussos, C.; Christopoulou-Kokkinou, V.; Zakynthinos, S. Coagulation system and platelets are fully activated in uncomplicated sepsis. Crit. Care Med. 2000, 28, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Torres MJ, M.; Peterson, J.M.; Wolf, S.E. Detection of Infection and Sepsis in Burns. Surg. Infect. 2020, 22, 20–27. [Google Scholar] [CrossRef]
- Lachiewicz, A.M.; Hauck, C.G.; Weber, D.J.; Cairns, B.A.; Van Duin, D. Bacterial Infections After Burn Injuries: Impact of Multidrug Resistance. Clin. Infect. Dis. 2017, 65, 2130–2136. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, D.G.; Hill, D.M.; Burmeister, D.M.; Gus, E.I.; Cleland, H.; Padiglione, A.; Holden, D.; Huss, F.; Chew, M.S.; Kubasiak, J.C.; et al. Surviving sepsis after burn campaign. Burns 2023, 49, 1487–1524. [Google Scholar] [CrossRef]
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.; Sibbald, W.J. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef]
- Tobiasen, J.; Hiebert, J.; Edlich, R. The abbreviated burn severity index. Ann. Emerg. Med. 1982, 11, 260–262. [Google Scholar] [CrossRef]
- Jinna, S.; Khandhar, P.B. Thrombocytopenia. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK542208/ (accessed on 4 July 2023).
- Mehta, M.; Tudor, G.J. Parkland Formula. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537190/ (accessed on 19 June 2023).
- The American Burn Association Consensus Conference on Burn Sepsis and Infection Group; Greenhalgh, D.G.; Saffle, J.R.; Holmes, J.H.; Gamelli, R.L.; Palmieri, T.L.; Horton, J.W.; Tompkins, R.G.; Traber, D.L.; Mozingo, D.W.; et al. American Burn Association Consensus Conference to Define Sepsis and Infection in Burns. J. Burn. Care Res. 2007, 28, 776–790. [Google Scholar] [CrossRef]
- Ball, R.L.; Keyloun, J.W.; Brummel-Ziedins, K.; Orfeo, T.; Palmieri, T.L.; Johnson, L.S.; Moffatt, L.T.; Pusateri, A.E.; Shupp, J.W. Burn-Induced Coagulopathies: A Comprehensive Review. Shock 2020, 54, 154–167. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers. 2020, 6, 11. [Google Scholar] [CrossRef]
- Sarda, D.K.; Dagwade, A.M.; Lohiya, S.; Kamble, A.T. Evaluation of platelet count as a prognostic indicator in early detection of post burn septicemia. Bombay Hosp. J. 2005, 47, 3–6. [Google Scholar]
- Gajbhiye, A.S.; Meshram, M.M.; Kathod, A.P. Platelet count as a prognostic indicator in burn septicemia. Indian J. Surg. 2013, 75, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.C.; Wu, G.H.; Zheng, J.J.; Chen, Z.H.; Chen, X.D. Prognostic Values of Platelet Distribution Width and Platelet Distribution Width-to-Platelet Ratio in Severe Burns. Shock 2022, 57, 494–500. [Google Scholar] [CrossRef]
- Marck, R.E.; Montagne, H.L.; Tuinebreijer, W.E.; Breederveld, R.S. Time course of thrombocytes in burn patients and its predictive value for outcome. Burns 2013, 39, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Sen, S.; Hsei, L.; Tran, N.; Romanowski, K.; Palmieri, T.; Greenhalgh, D.; Cho, K. Early clinical complete blood count changes in severe burn injuries. Burns 2019, 45, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Warner, P.; Fields, A.L.; Braun, L.C.; James, L.E.; Bailey, J.K.; Yakuboff, K.P.; Kagan, R.J. Thrombocytopenia in the pediatric burn patient. J. Burn. Care Res. 2011, 32, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Akca, S.; Haji-Michael, P.; de Mendonça, A.; Suter, P.; Levi, M.; Vincent, J.L. Time course of platelet counts in critically ill patients. Crit. Care Med. 2002, 30, 753–756. [Google Scholar] [CrossRef]
- Zarychanski, R.; Houston, D.S. Assessing thrombocytopenia in the intensive care unit: The past, present, and future. Hematology Am. Soc. Hematol. Educ. Program 2017, 2017, 660–666. [Google Scholar] [CrossRef]
- Barbier, J.M.; Viana, M.V.; Pantet, O.; Alberio, L.; Berger, M.M. Blood coagulation alterations over the first 10 days after severe burn injury. Burns Open 2022, 6, 10–18. [Google Scholar] [CrossRef]
- Nunez Lopez, O.; Cambiaso-Daniel, J.; Branski, L.K.; Norbury, W.B.; Herndon, D.N. Predicting and managing sepsis in burn patients: Current perspectives. Ther. Clin. Risk Manag. 2017, 13, 1107–1117. [Google Scholar] [CrossRef] [PubMed]
- Janu, V.S.; Bhadauria, N.S.; Kumar, P. A prospective study of platelet count as a prognostic indicator in burn septicemia. Int. J. Surg. Sci. 2020, 4, 74–78. [Google Scholar] [CrossRef]
- de Stoppelaar, S.F.; van’t Veer, C.; van der Poll, T. The role of platelets in sepsis. Thromb. Haemost. 2014, 112, 666–677. [Google Scholar]
- François, B.; Trimoreau, F.; Vignon, P.; Fixe, P.; Praloran, V.; Gastinne, H. Thrombocytopenia in the sepsis syndrome: Role of hemophagocytosis and macrophage colony-stimulating factor. Am. J. Med. 1997, 103, 114–120. [Google Scholar] [CrossRef]
- Stéphan, F.; Cheffi, M.A.; Kaplan, C.; Maillet, J.; Novara, A.; Fagon, J.; Bonnet, F. Autoantibodies against platelet glycoproteins in critically ill patients with thrombocytopenia. Am. J. Med. 2000, 108, 554–560. [Google Scholar] [CrossRef]
- Vardon-Bounes, F.; Ruiz, S.; Gratacap, M.P.; Garcia, C.; Payrastre, B.; Minville, V. Platelets Are Critical Key Players in Sepsis. Int. J. Mol. Sci. 2019, 20, 3494. [Google Scholar] [CrossRef]
- Levi, M.; Ten Cate, H. Disseminated intravascular coagulation. N. Engl. J. Med. 1999, 341, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Singbartl, K.; Singbartl, G.; Schleinzer, W. Hemodilution induced thrombocytopenia. Anesth. Analg. 1999, 88, 100. [Google Scholar] [CrossRef]
- Gonzalez, D.A.; Kumar, R.; Asif, S.; Bali, A.; Dang, A.K. Sepsis and Thrombocytopenia: A Nowadays Problem. Cureus 2022, 14, e25421. [Google Scholar] [CrossRef] [PubMed]
- Richwagen, N.; Lyles, J.T.; Dale, B.L.F.; Quave, C.L. Antibacterial activity of Kalanchoe mortagei and K. fedtschenkoi against ESKAPE pathogens. Front. Pharmacol. 2019, 10, 67. [Google Scholar] [CrossRef]
- Hodea, F.V.; Lazarescu, A.L.; Grosu-Bularda, A.; Cretu, A.; Teodoreanu, R.N.; Lascar, I.; Hariga, C.S. Antimicrobial resistance of ESKAPE pathogens in major burns patients-one-year retrospective study. Farmacia 2023, 71, 549–555. [Google Scholar] [CrossRef]
- Belba, M.K.; Petrela, E.Y.; Belba, A.G. Epidemiology and outcome analysis of sepsis and organ dysfunction/failure after burns. Burns 2017, 43, 1335–1347. [Google Scholar] [CrossRef]
- Cumming, J.; Purdue, G.F.; Hunt, J.L.; O’Keefe, G.E. Objective estimates of the incidence and consequences of multiple organ dysfunction and sepsis after burn trauma. J. Trauma 2001, 50, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Fitzwater, J.; Purdue, G.F.; Hunt, J.L.; O’Keefe, G.E. The risk factors and time courses sepsis and organ dysfunction after burn trauma. J. Trauma 2003, 54, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kym, D.; Park, J.; Yoon, J.; Cho, Y.S.; Hur, J.; Chun, W.; Yoon, D. Big data insights into the diagnostic values of CBC parameters for sepsis and septic shock in burn patients: A retrospective study. Sci. Rep. 2024, 14, 800. [Google Scholar] [CrossRef] [PubMed]
- Boehm, D.; Menke, H. Sepsis in Burns-Lessons Learnt from Developments in the Management of Septic Shock. Medicina 2021, 58, 26. [Google Scholar] [CrossRef] [PubMed]
- Manning, J. Sepsis in the burn patient. Crit. Care Nurs. Clin. North. Am. 2018, 30, 423–430. [Google Scholar] [CrossRef] [PubMed]



| Variables | Classification | Cases | Proportion (%) |
|---|---|---|---|
| Sex | Female | 30 | 33.3% |
| Male | 60 | 66.7% | |
| Age | ≤40 | 23 | 25.5% |
| 41–60 | 25 | 27.8% | |
| 61–80 | 31 | 34.4% | |
| >80 | 11 | 12.2% | |
| Mechanism of injury | Flame | 77 | 85.5% |
| Scalds | 8 | 8.9% | |
| Electrical burns | 4 | 4.4% | |
| Contact burns | 1 | 1.1% | |
| Burn setting | Domestic accident | 71 | 78.9% |
| Work accident | 3 | 3.3% | |
| Self-harm | 12 | 13.3% | |
| Burning aggression | 2 | 2.2% | |
| Undetermined | 2 | 2.2% | |
| TBSA | 20–40 | 48 | 53.3% |
| 41–60 | 19 | 21.1% | |
| 61–80 | 16 | 17.8% | |
| 81–100% | 7 | 7.8% | |
| 3rd-degree burns | No | 22 | 24.4% |
| Yes | 68 | 75.6% | |
| Inhalation injuries | No | 26 | 28.9% |
| Yes | 64 | 71.1% |
| Thrombocytopenia—day 3/Survival (n = 88) | Survivors | Non-survivors | p * | ||
| No. | Percent | No. | Percent | ||
| Normal TPC | 18 | 56.30% | 11 | 19.60% | 0.001 |
| Thrombocytopenia | 14 | 43.80% | 45 | 80.40% | |
| Thrombocytopenia—day 7/Survival (n = 84) | Survivors | Non-survivors | p * | ||
| No. | Percent | No. | Percent | ||
| Normal TPC | 26 | 81.30% | 8 | 15.40% | <0.001 |
| Thrombocytopenia | 6 | 18.80% | 44 | 84.60% | |
| Thrombocytopenia—day 14/Survival (n = 65) | Survivors | Non-survivors | p * | ||
| No. | Percent | No. | Percent | ||
| Normal TPC | 31 | 100% | 13 | 38.20% | <0.001 |
| Thrombocytopenia | 0 | 0% | 21 | 61.80% | |
| Thrombocytopenia—day 21/Survival (n = 45) | Survivors | Non-survivors | p * | ||
| No. | Percent | No. | Percent | ||
| Normal TPC | 24 | 96% | 11 | 55% | 0.002 |
| Thrombocytopenia | 1 | 4% | 9 | 45% | |
| Thrombocytopenia—day 28/Survival (n = 36) | Survivors | Non-survivors | p * | ||
| No. | Percent | No. | Percent | ||
| Normal TPC | 19 | 95% | 10 | 62.50% | 0.03 |
| Thrombocytopenia | 1 | 5% | 6 | 37.50% | |
| Thrombocytopenia—day 45/Survival (n = 21) | Survivors | Non-survivors | p * | ||
| No. | Percent | No. | Percent | ||
| Normal TPC | 10 | 90.90% | 4 | 40% | 0.024 |
| Thrombocytopenia | 1 | 9.10% | 6 | 60% | |
| Thrombocytopenia—day 60/Survival (n = 13) | Survivors | Non-survivors | p * | ||
| No. | Percent | No. | Percent | ||
| Normal TPC | 7 | 100% | 2 | 33.30% | 0.021 |
| Thrombocytopenia | 0 | 0% | 4 | 66.70% | |
| Thrombocytopenia—day 3 post-burn Absent Present | Mean (95% CI) | Median (IQR) | p * |
| 65.1 (46.3–83.9) | 63 (19–97) | 0.025 | |
| 39.4 (28.9–49.9) | 20 (10–60) | ||
| Thrombocytopenia—day 7 post-burn Absent Present | Mean (95% CI) | Median (IQR) | p * |
| 80.1 (64.0–96.2) | 97 | <0.001 | |
| 30.1 (20.8–39.3) | 16 (9–39) | ||
| Thrombocytopenia—day 14 post-burn Absent Present | Mean (95% CI) | Median (IQR) | p * |
| 75.9 (62.9–88.9) | 77 | <0.001 | |
| 27.1 (17.2–37.1) | 18 (16–26) | ||
| Thrombocytopenia—day 21 post-burn Absent Present | Mean (95% CI) | Median (IQR) | p * |
| 83.9 (69.9–97.8) | 97 (63–113) | <0.001 | |
| 34.3 (24.4–44.2) | 27 (21–50) | ||
| Thrombocytopenia—day 28 post-burn Absent Present | Mean (95% CI) | Median (IQR) | p * |
| 84.4 (69.8–99) | 97 (63–113) | <0.001 | |
| 42.2 (30.8–53.7) | 45 (27–60) |
| Platelet count—day 3 Normal TPC (p = 0.400 **) Thrombocytopenia (p = 0.125 **) | Mean ± SD | Median (IQR) | p * (p = 0.365 ***) |
| 8.41 ± 1.84 | 8 (7–9.5) | <0.001 | |
| 10.81 ± 2.15 | 11 (9–12) | ||
| Platelet count—day 7 Normal TPC (p = 0.288 **) Thrombocytopenia (p = 0.320 **) | Mean ± SD | Median (IQR) | p * (p = 0.197 ***) |
| 8.32 ± 1.59 | 8 (7–9) | <0.001 | |
| 10.98 ± 2.05 | 11 (10–12) | ||
| Platelet count—day 14 Normal TPC (p = 0.155 **) Thrombocytopenia (p = 0.13 7 **) | Mean ± SD | Median (IQR) | p * (p = 0.805 ***) |
| 8.80 ± 1.72 | 9 (8–10) | <0.001 | |
| 10.67 ± 1.68 | 11 (9.5–12) |
| Platelet count—day 3 post-burn | Mean ± SD | Median (IQR) | p * |
| Normal range (p = 0.134 **) | 48.2 ± 16.7 | 44 (36–61.5) | 0.002 |
| Thrombocytopenia (p = 0.006 **) | 61.1 ± 17.7 | 66 (44–76) | |
| * Mann–Whitney U Test, ** Shapiro–Wilk Test | |||
| Platelet count—day 7 post-burn | Mean ± SD | Median (IQR) | p * |
| Normal range (p = 0.055 **) | 48.7 ± 17.8 | 44 (34.7–61.2) | 0.002 |
| Thrombocytopenia (p = 0.039 **) | 61.7 ± 16.8 | 65 (47.7–76.2) | |
| * Mann–Whitney U Test, ** Shapiro–Wilk Test | |||
| Platelet count—day 14 post-burn | Mean ± SD | Median (IQR) | p * (p = 0.644 ***) |
| Normal range (p = 0.077 **) | 52.4 ± 17.8 | 48.5 (38.5–69.5) | 0.015 |
| Thrombocytopenia (p = 0.389 **) | 64 ± 16.9 | 64 (49–78.5) | |
| * Student t-Test, ** Shapiro–Wilk Test, *** Levene’s Test for Equality of Variances | |||
| Platelet count—day 21 post-burn | Mean ± SD | Median (IQR) | p * (p = 0.039 ***) |
| Normal range (p = 0.090 **) | 53.1 ± 19 | 47 (38–71) | 0.056 |
| Thrombocytopenia (p = 0.398 **) | 63.2 ± 12.1 | 62.5 (49.7–73.5) | |
| * Welch t-Test, ** Shapiro–Wilk Test, *** Levene’s Test for Equality of Variances | |||
| Platelet count—day 28 post-burn | Mean ± SD | Median (IQR) | p * |
| Normal range (p = 0.155 **) | 54.1 ± 17.4 | 51 (40.5–71) | 0.036 |
| Thrombocytopenia (p = 0.013 **) | 70.7 ± 18.8 | 76 (70–82) | |
| * Mann–Whitney U Test, ** Shapiro–Wilk Test | |||
| Platelet count—day 45 post-burn | Mean ± SD | Median (IQR) | p * (p = 0.306 ***) |
| Normal range (p = 0.345 **) | 52.2 ± 18.1 | 49 (38.7–72.2) | 0.019 |
| Thrombocytopenia (p = 0.503 **) | 72.1 ± 13.4 | 76 (59–82) | |
| * Student t-Test, ** Shapiro–Wilk Test, *** Levene’s Test for Equality of Variances | |||
| Platelet count—day 60 post-burn | Mean ± SD | Median (IQR) | p * |
| Normal range (p = 0.073 **) | 51 ± 18.2 | 44 (37.5–73.5) | 0.020 |
| Thrombocytopenia (p = 0.003 **) | 74 ± 15.3 | 81.5 (58.5–82) | |
| * Mann–Whitney U Test, ** Shapiro–Wilk Test | |||
| Thrombocytopenia—day 3 post-burn | Mean TBSA ± SD | Median TBSA (IQR) | p * |
| Absent (p < 0.001 **) | 39.3 ± 15.4 | 35 (27.5–40) | 0.004 |
| Present (p = 0.006 **) | 51.9 ± 19.7 | 50 (35–70) | |
| Thrombocytopenia—day 7 post-burn | Mean TBSA ± SD | Median TBSA (IQR) | p * |
| Absent (p = 0.004 **) | 38.3 ± 13.1 | 35 (25–42.5) | 0.001 |
| Present (p = 0.011 **) | 52.6 ± 20 | 50 (35–70) |
| TPC—day 3 | Without 3rd-degree burns | 3rd-degree burns | p * | No inhalation injury | Inhalation injury | p * |
| Normal TPC | 12 patients (54.5%) | 17 patients (25.8%) | 0.019 | 12 patients (46.2%) | 17 patients (27.4%) | 0.135 |
| Thrombocytopenia | 10 patients (45.5%) | 49 patients (74.2%) | 14 patients (53.8%) | 45 patients (72.6%) | ||
| TPC—day 7 | Without 3rd-degree burns | 3rd-degree burns | p * | No inhalation injury | Inhalation injury | p * |
| Normal TPC | 14 patients (63.6%) | 20 patients (32.3%) | 0.013 | 15 patients (60%) | 19 patients (32.2%) | 0.028 |
| Thrombocytopenia | 8 patients (36.4%) | 42 patients (67.7%) | 10 patients (40%) | 40 patients (67.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bordeanu-Diaconescu, E.-M.; Grosu-Bularda, A.; Frunza, A.; Grama, S.; Andrei, M.-C.; Neagu, T.-P.; Lascar, I.; Hariga, C.-S. Diagnostic and Prognostic Value of Thrombocytopenia in Severe Burn Injuries. Diagnostics 2024, 14, 582. https://doi.org/10.3390/diagnostics14060582
Bordeanu-Diaconescu E-M, Grosu-Bularda A, Frunza A, Grama S, Andrei M-C, Neagu T-P, Lascar I, Hariga C-S. Diagnostic and Prognostic Value of Thrombocytopenia in Severe Burn Injuries. Diagnostics. 2024; 14(6):582. https://doi.org/10.3390/diagnostics14060582
Chicago/Turabian StyleBordeanu-Diaconescu, Eliza-Maria, Andreea Grosu-Bularda, Adrian Frunza, Sabina Grama, Mihaela-Cristina Andrei, Tiberiu-Paul Neagu, Ioan Lascar, and Cristian-Sorin Hariga. 2024. "Diagnostic and Prognostic Value of Thrombocytopenia in Severe Burn Injuries" Diagnostics 14, no. 6: 582. https://doi.org/10.3390/diagnostics14060582
APA StyleBordeanu-Diaconescu, E.-M., Grosu-Bularda, A., Frunza, A., Grama, S., Andrei, M.-C., Neagu, T.-P., Lascar, I., & Hariga, C.-S. (2024). Diagnostic and Prognostic Value of Thrombocytopenia in Severe Burn Injuries. Diagnostics, 14(6), 582. https://doi.org/10.3390/diagnostics14060582






