Determination of Five Sit-to-Stand Test Performance at Discharge of Stroke Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Outcome Measures and Predictors
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics at Admission, T1, and Discharge
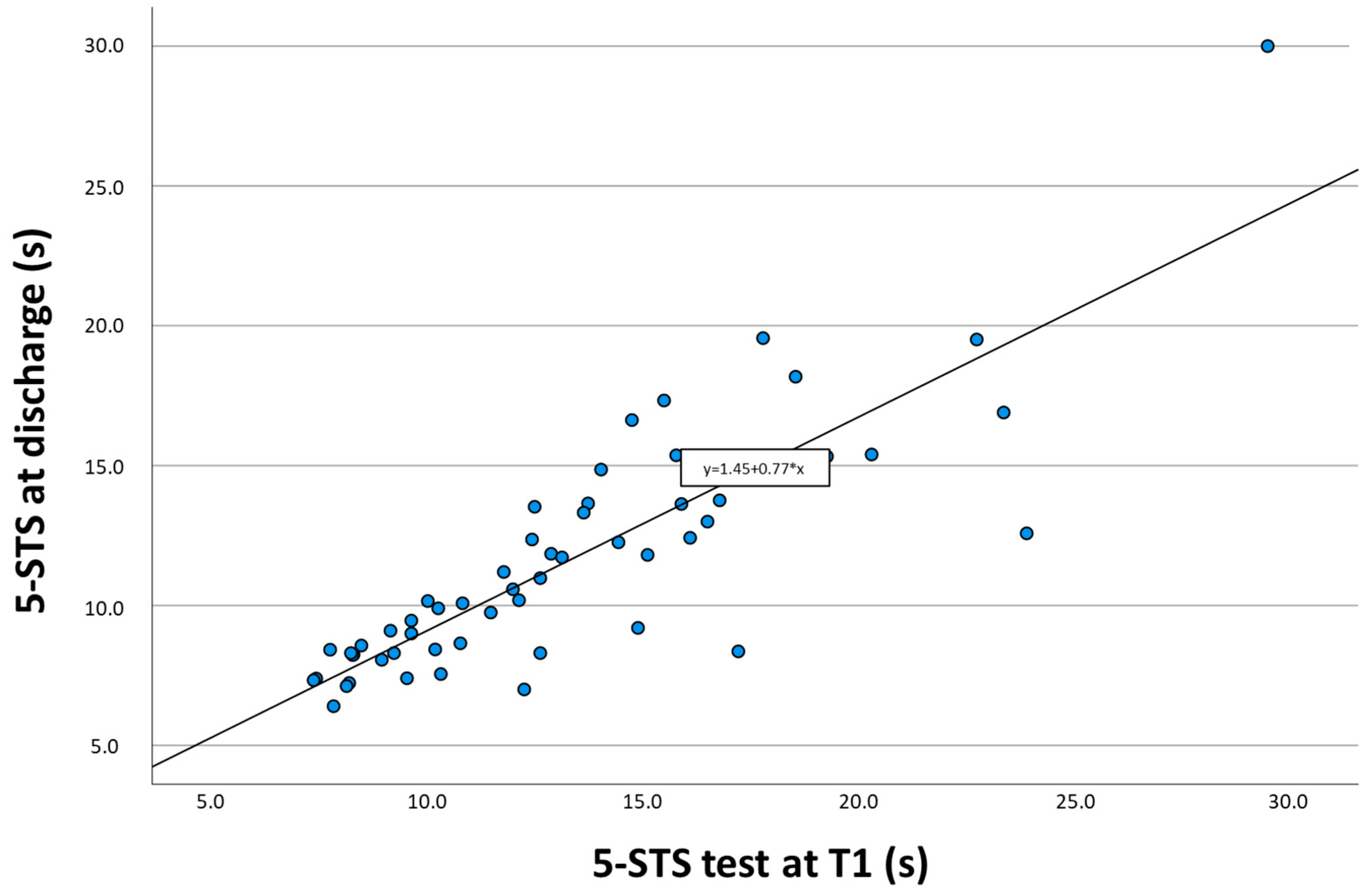
3.2. Predictive Ability of the 5-STS Test Performance at Discharge
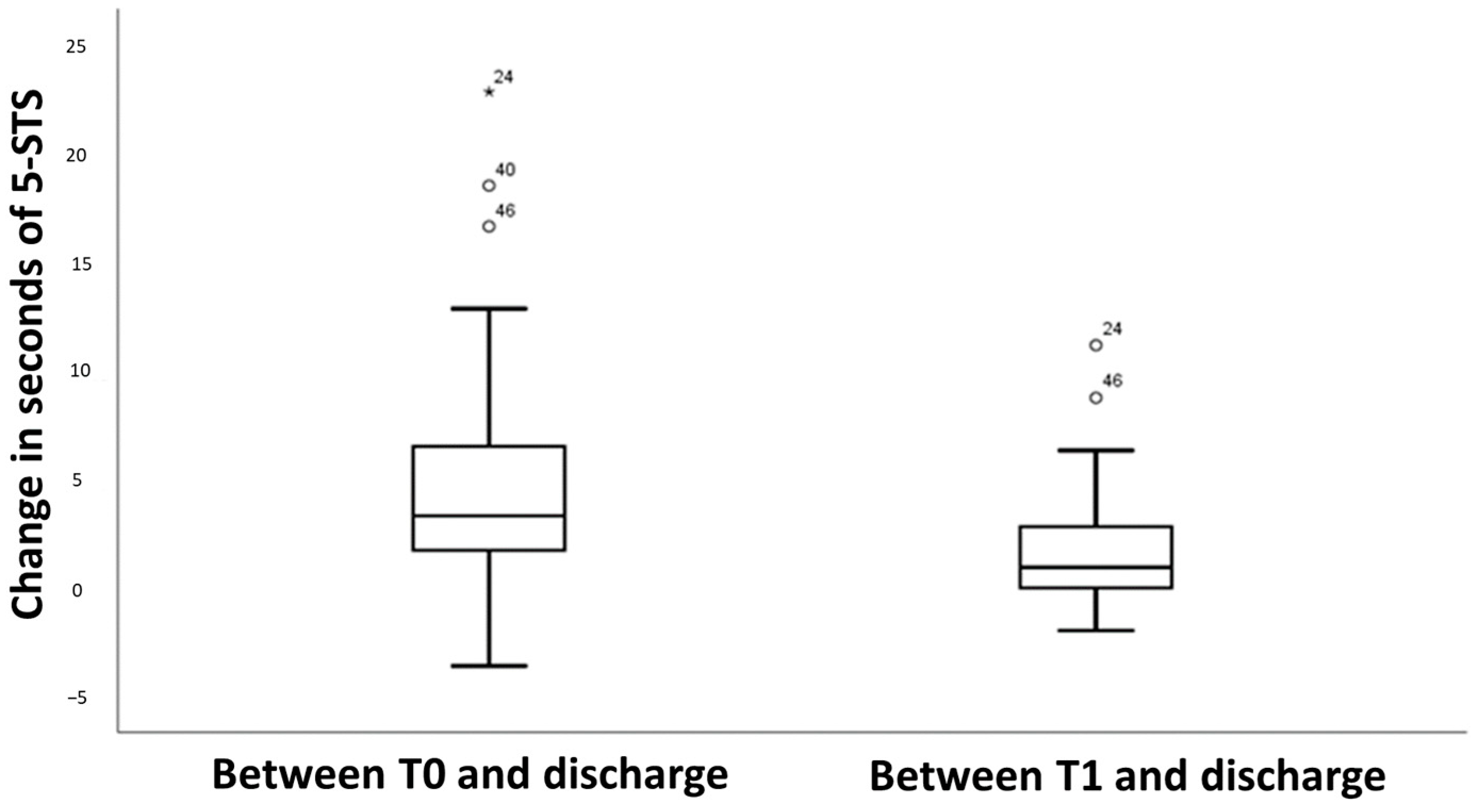
3.3. Predictive Ability for the Change in the 5-STS Test Results at Discharge
4. Discussion
4.1. Implications for Practice and Research
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cheung, C.M.; Tsoi, T.H.; Hon, S.F.K.; Au-Yeung, M.; Shiu, K.L.; Lee, C.N.; Huang, C.Y. Outcomes after First-Ever Stroke. Hong Kong Med. J. Xianggang Yi Xue Za Zhi 2007, 13, 95–99. [Google Scholar]
- Dean, C.M.; Channon, E.F.; Hall, J.M. Sitting Training Early after Stroke Improves Sitting Ability and Quality and Carries over to Standing up but Not to Walking: A Randomised Controlled Trial. Aust. J. Physiother. 2007, 53, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.E.; McPherson, K.; McNaughton, H.K.; Rochester, L.; Weatherall, M. Community Ambulation after Stroke: How Important and Obtainable Is It and What Measures Appear Predictive? Arch. Phys. Med. Rehabil. 2004, 85, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Knee Extension Strength and Body Weight Determine Sit-to-Stand Independence after Stroke. Physiother. Theory Pract. 2007, 23, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Lin, R.; Chiang, S.; Heitkemper, M.M.; Weng, S.; Lin, C.; Yang, F.; Lin, C. Effectiveness of Early Rehabilitation Combined With Virtual Reality Training on Muscle Strength, Mood State, and Functional Status in Patients With Acute Stroke: A Randomized Controlled Trial. Worldviews Evid. Based Nurs. 2020, 17, 158–167. [Google Scholar] [CrossRef]
- Mentiplay, B.F.; Clark, R.A.; Bower, K.J.; Williams, G.; Pua, Y.-H. Five Times Sit-to-Stand Following Stroke: Relationship with Strength and Balance. Gait Posture 2020, 78, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Kerr, A.; Dawson, J.; Robertson, C.; Rowe, P.; Quinn, T.J. Sit to Stand Activity during Stroke Rehabilitation. Top. Stroke Rehabil. 2017, 24, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Pollock, A.; Gray, C.; Culham, E.; Durward, B.R.; Langhorne, P. Interventions for Improving Sit-to-Stand Ability Following Stroke. Cochrane Database Syst. Rev. 2014, CD007232. [Google Scholar] [CrossRef] [PubMed]
- Janssen, W.; Bussmann, J.; Selles, R.; Koudstaal, P.; Ribbers, G.; Stam, H. Recovery of the Sit-to-Stand Movement After Stroke: A Longitudinal Cohort Study. Neurorehabil. Neural Repair 2010, 24, 763–769. [Google Scholar] [CrossRef]
- Ingemanson, M.L.; Rowe, J.R.; Chan, V.; Wolbrecht, E.T.; Reinkensmeyer, D.J.; Cramer, S.C. Somatosensory System Integrity Explains Differences in Treatment Response after Stroke. Neurology 2019, 92, e1098–e1108. [Google Scholar] [CrossRef]
- Goldie, P.A.; Matyas, T.A.; Kinsella, G.J.; Galea, M.P.; Evans, O.M.; Bach, T.M. Prediction of Gait Velocity in Ambulatory Stroke Patients during Rehabilitation. Arch. Phys. Med. Rehabil. 1999, 80, 415–420. [Google Scholar] [CrossRef]
- Kuys, S.S.; Bew, P.G.; Lynch, M.R.; Morrison, G.; Brauer, S.G. Measures of Activity Limitation on Admission to Rehabilitation after Stroke Predict Walking Speed at Discharge: An Observational Study. Aust. J. Physiother. 2009, 55, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association with Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Mong, Y.; Teo, T.W.; Ng, S.S. 5-Repetition Sit-to-Stand Test in Subjects With Chronic Stroke: Reliability and Validity. Arch. Phys. Med. Rehabil. 2010, 91, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Goto, Y.; Otaka, Y.; Suzuki, K.; Inoue, S.; Kondo, K.; Shimizu, E. Incidence and Circumstances of Falls among Community-Dwelling Ambulatory Stroke Survivors: A Prospective Study: Falls in Community-Dwelling Stroke. Geriatr. Gerontol. Int. 2019, 19, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Pua, Y.-H.; Thumboo, J.; Clark, R.A. Correspondence: Time-Based versus Repetition-Based Sit-to-Stand Measures: Choice of Metrics Matters. J. Physiother. 2018, 64, 200–201. [Google Scholar] [CrossRef]
- Agustín, R.M.-S.; Crisostomo, M.J.; Sánchez-Martínez, M.P.; Medina-Mirapeix, F. Responsiveness and Minimal Clinically Important Difference of the Five Times Sit-to-Stand Test in Patients with Stroke. Int. J. Environ. Res. Public. Health 2021, 18, 2314. [Google Scholar] [CrossRef]
- Lee, G.; An, S.; Lee, Y.; Park, D.-S. Clinical Measures as Valid Predictors and Discriminators of the Level of Community Ambulation of Hemiparetic Stroke Survivors. J. Phys. Ther. Sci. 2016, 28, 2184–2189. [Google Scholar] [CrossRef]
- Lee, K.B.; Lim, S.H.; Ko, E.H.; Kim, Y.S.; Lee, K.S.; Hwang, B.Y. Factors Related to Community Ambulation in Patients with Chronic Stroke. Top. Stroke Rehabil. 2015, 22, 63–71. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Pearson/Allyn & Bacon: Boston, MA, USA, 2007; ISBN 978-0-205-45938-4. [Google Scholar]
- Kwakkel, G.; Kollen, B.; Twisk, J. Impact of Time on Improvement of Outcome after Stroke. Stroke 2006, 37, 2348–2353. [Google Scholar] [CrossRef]
- Gresham, G.E. Stroke Outcome Research. Stroke 1986, 17, 358–360. [Google Scholar] [CrossRef]
- Jørgensen, H.S.; Nakayama, H.; Raaschou, H.O.; Vive-Larsen, J.; Støier, M.; Olsen, T.S. Outcome and Time Course of Recovery in Stroke. Part II: Time Course of Recovery. The Copenhagen Stroke Study. Arch. Phys. Med. Rehabil. 1995, 76, 406–412. [Google Scholar] [CrossRef]
- Skilbeck, C.E.; Wade, D.T.; Hewer, R.L.; Wood, V.A. Recovery after Stroke. J. Neurol. Neurosurg. Psychiatry 1983, 46, 5–8. [Google Scholar] [CrossRef]
- Loewen, S.C.; Anderson, B.A. Predictors of Stroke Outcome Using Objective Measurement Scales. Stroke 1990, 21, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Vanclay, F. Functional Outcome Measures in Stroke Rehabilitation. Stroke 1991, 22, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.D.; Hayden, J.A.; Steyerberg, E.W.; Moons, K.G.M.; Abrams, K.; Kyzas, P.A.; Malats, N.; Briggs, A.; Schroter, S.; Altman, D.G.; et al. Prognosis Research Strategy (PROGRESS) 2: Prognostic Factor Research. PLoS Med. 2013, 10, e1001380. [Google Scholar] [CrossRef]
- Boukadida, A.; Piotte, F.; Dehail, P.; Nadeau, S. Determinants of Sit-to-Stand Tasks in Individuals with Hemiparesis Post Stroke: A Review. Ann. Phys. Rehabil. Med. 2015, 58, 167–172. [Google Scholar] [CrossRef] [PubMed]

| Variable | All (n = 56) |
|---|---|
| Demographics | |
| Age. years; mean (SD) | 62.7 (13.0) |
| Gender (male) | 33 (58.9%) |
| Stroke characteristics | |
| Side affected (right) | 27 (48.2%) |
| Type of stroke (ischemic) | 42 (75.0%) |
| Time from stroke to admission ORP. days; mean (SD) | 48.4 (30.3) |
| Time in ORP. days; mean (SD) | 70.7 (40.4) |
| FAC (score 0–5), median (IQR) | 4.0 (1.0) |
| Gait speed. m/s; mean (SD) | 0.62 (0.32) |
| 5-STS at T0. s; mean (SD) | 16.10 (6.72) |
| 5-STS at T1. s; mean (SD) | 13.2 (4.7) |
| 5-STS at discharge. s; mean (SD) | 11.6 (4.25) |
| Variable | Multivariate Models | ||
|---|---|---|---|
| B (95%CI) | p-Value | R2 | |
| Model 1 | 0.577 | ||
| 5-STS at T0 | 0.36 (0.23–0.48) | <0.001 | |
| Age, y | 0.03 (−0.02–0.09) | 0.249 | |
| Time from stroke to admission ORP, days | 0.04 (0.01–0.07) | 0.002 | |
| Model 2 | 0.755 | ||
| 5-STS at T1 | 0.69 (0.54–0.83) | <0.001 | |
| Age, y | 0.01 (−0.03–0.06) | 0.512 | |
| Time from stroke to admission ORP, days | 0.02 (0.00–0.04) | 0.019 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Martínez, M.P.; Crisostomo, M.J.; Martín-San Agustín, R.; Montilla-Herrador, J.; Escolar-Reina, M.P.; Valera-Novella, E.; Medina-Mirapeix, F. Determination of Five Sit-to-Stand Test Performance at Discharge of Stroke Patients. Diagnostics 2024, 14, 521. https://doi.org/10.3390/diagnostics14050521
Sánchez-Martínez MP, Crisostomo MJ, Martín-San Agustín R, Montilla-Herrador J, Escolar-Reina MP, Valera-Novella E, Medina-Mirapeix F. Determination of Five Sit-to-Stand Test Performance at Discharge of Stroke Patients. Diagnostics. 2024; 14(5):521. https://doi.org/10.3390/diagnostics14050521
Chicago/Turabian StyleSánchez-Martínez, Maria Piedad, María José Crisostomo, Rodrigo Martín-San Agustín, Joaquina Montilla-Herrador, María Pilar Escolar-Reina, Elisa Valera-Novella, and Francesc Medina-Mirapeix. 2024. "Determination of Five Sit-to-Stand Test Performance at Discharge of Stroke Patients" Diagnostics 14, no. 5: 521. https://doi.org/10.3390/diagnostics14050521
APA StyleSánchez-Martínez, M. P., Crisostomo, M. J., Martín-San Agustín, R., Montilla-Herrador, J., Escolar-Reina, M. P., Valera-Novella, E., & Medina-Mirapeix, F. (2024). Determination of Five Sit-to-Stand Test Performance at Discharge of Stroke Patients. Diagnostics, 14(5), 521. https://doi.org/10.3390/diagnostics14050521








