Musculoskeletal and Neuropathic Pain in COVID-19
Abstract
1. Introduction
2. Epidemiology of Musculoskeletal and Neuropathic Pain Pre-Pandemic
3. The Impact of COVID-19 on Healthcare
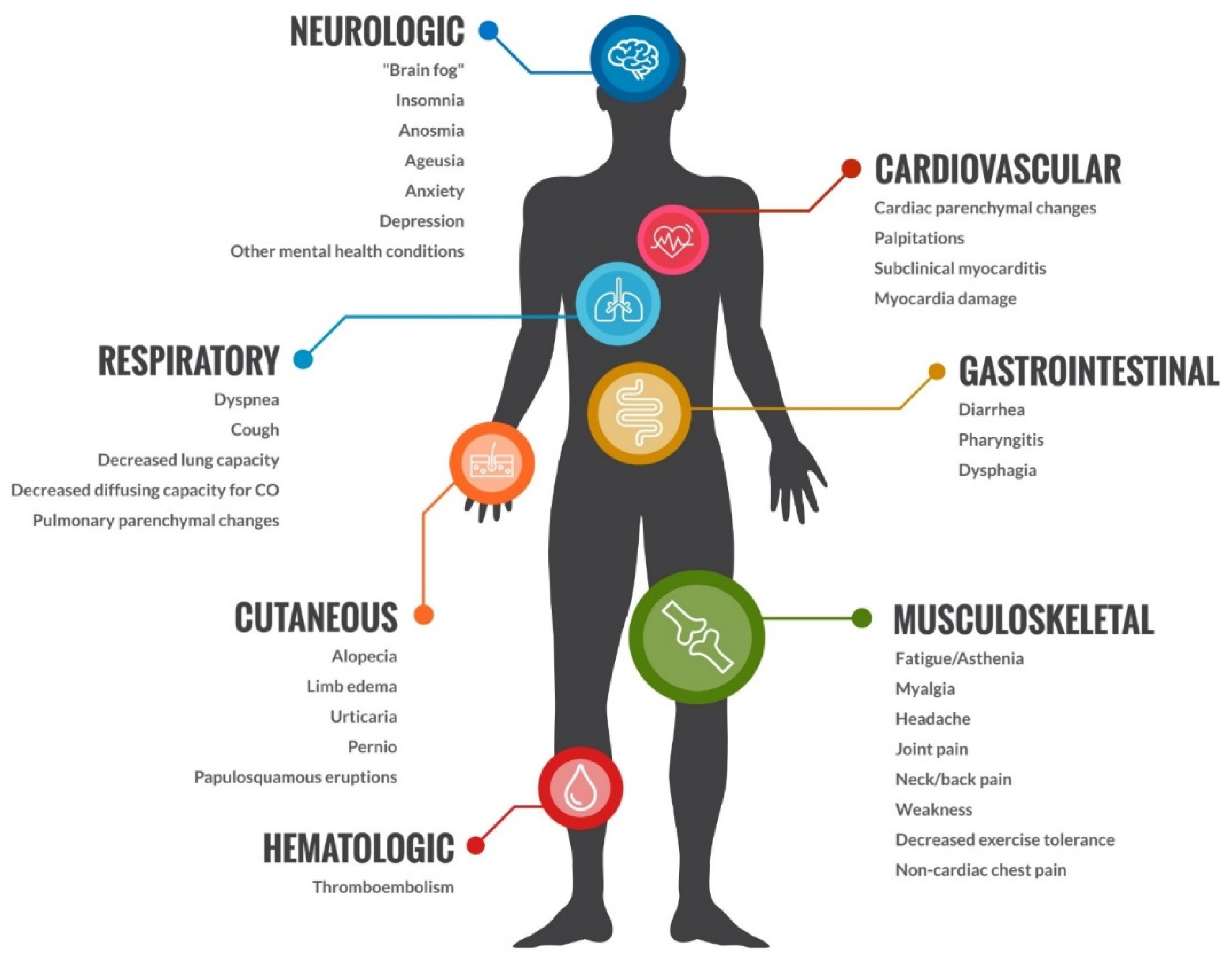
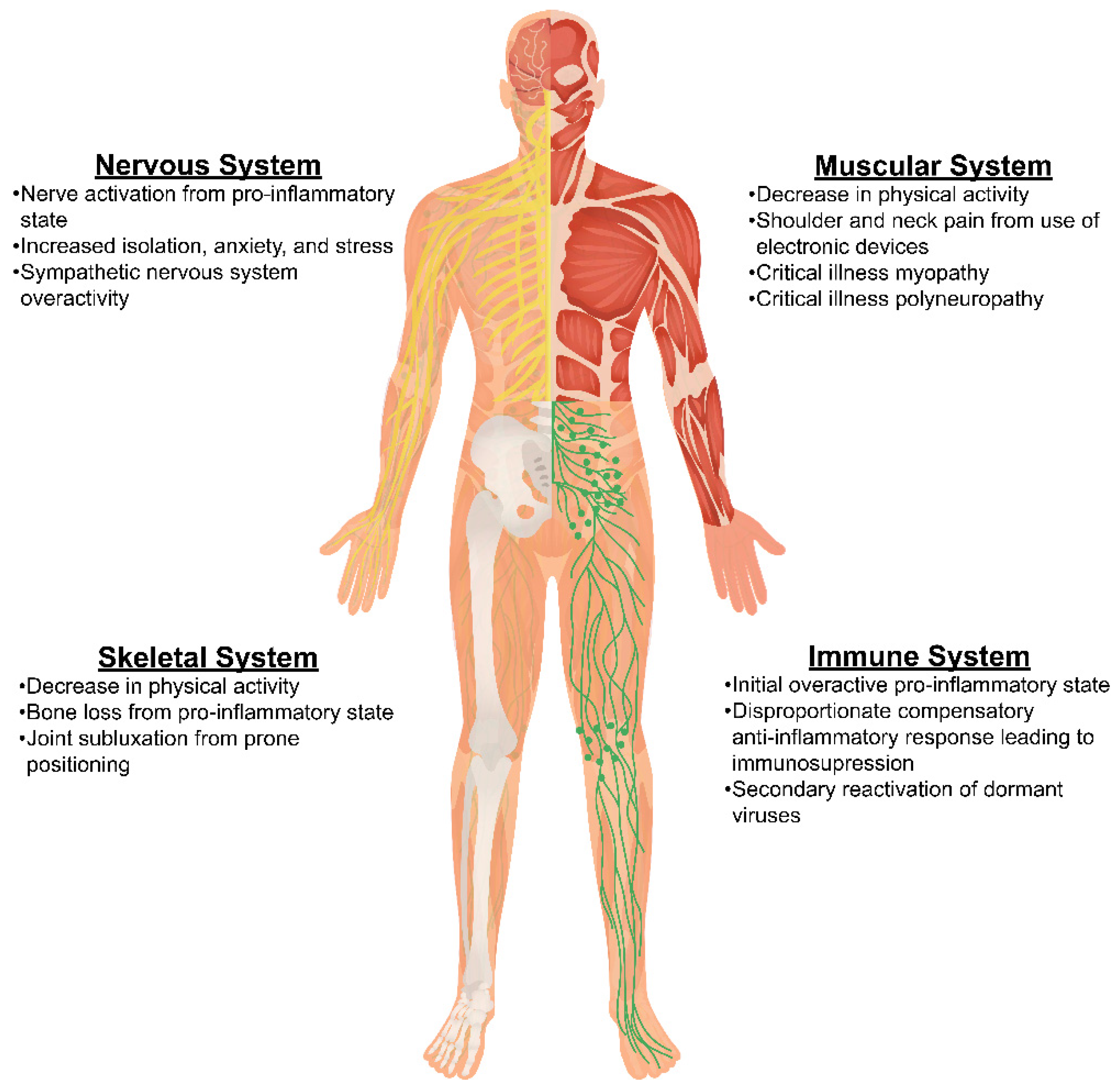
4. COVID-19 and Its Impact on Musculoskeletal and Neuropathic Pain
5. Emerging Perspectives on Underlying Mechanisms in Chronic Pain in COVID-19
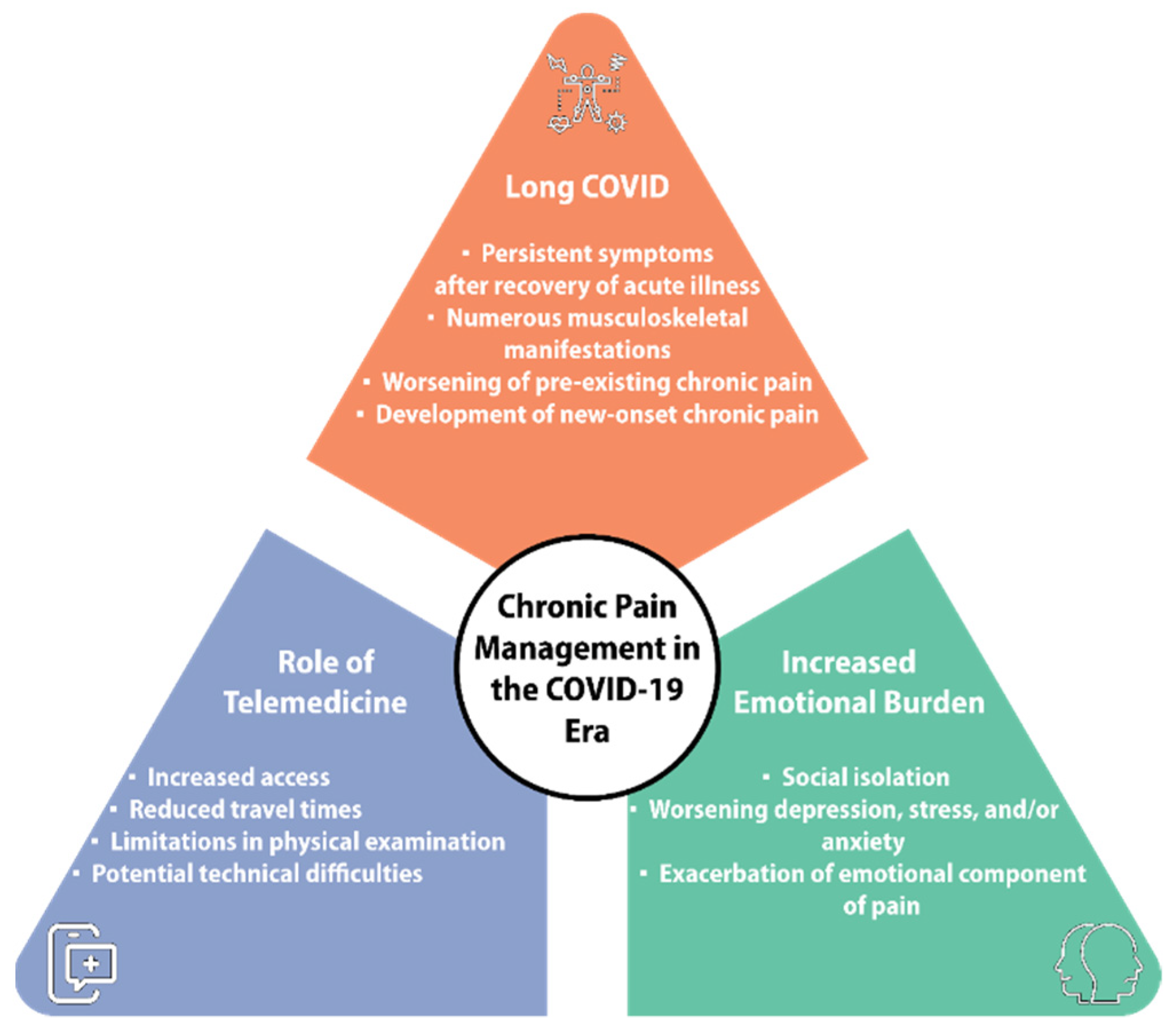
6. Management of Chronic Pain in the COVID-19 Era
6.1. Assessment of Chronic Pain Patients and Impact of COVID-19 Pandemic
6.2. Unique Diagnostic Challenges for Chronic Pain Physicians from COVID-19
6.3. Interplay between Persistent Symptoms after COVID-19 and Other Chronic Pain Conditions
6.4. Multidisciplinary Approach to Management of Chronic Pain in COVID-19
6.5. Emerging Techniques in Pain Management for COVID-19
7. Novel Pharmacological Treatments
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic Pain as a Symptom or a Disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Dieleman, J.L.; Cao, J.; Chapin, A.; Chen, C.; Li, Z.; Liu, A.; Horst, C.; Kaldjian, A.; Matyasz, T.; Scott, K.W.; et al. US Health Care Spending by Payer and Health Condition, 1996–2016. JAMA 2020, 323, 863–884. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, J.; Mei, H.; Fang, F.; Ma, X. What Is New in Classification, Diagnosis and Management of Chronic Musculoskeletal Pain: A Narrative Review. Front. Pain Res. 2022, 3, 937004. [Google Scholar] [CrossRef] [PubMed]
- Cimmino, M.A.; Ferrone, C.; Cutolo, M. Epidemiology of Chronic Musculoskeletal Pain. Best Pract. Res. Clin. Rheumatol. 2011, 25, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.L.; Bradley, E.C.B.; Brady, B.K.B.; Calfee, R.P.; Klesges, L.M.; Colditz, G.A.M.; Prather, H.D. The Influence of Race, Sex, and Social Disadvantage on Self-reported Health in Patients Presenting with Chronic Musculoskeletal Pain. Am. J. Phys. Med. Rehabil. 2022, 101, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Blyth, F.M.; Noguchi, N. Chronic Musculoskeletal Pain and its Impact on Older People. Best Pract. Res. Clin. Rheumatol. 2017, 31, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Mose, S.; Kent, P.; Smith, A.; Andersen, J.H.; Christiansen, D.H. Number of Musculoskeletal Pain Sites Leads to Increased Long-Term Healthcare Contacts and Healthcare Related Costs—A Danish Population-Based Cohort Study. BMC Health Serv. Res. 2021, 21, 980. [Google Scholar] [CrossRef]
- Chen, N.; Fong, D.Y.T.; Wong, J.Y.H. Health and Economic Outcomes Associated With Musculoskeletal Disorders Attributable to High Body Mass Index in 192 Countries and Territories in 2019. JAMA Netw. Open 2023, 6, e2250674. [Google Scholar] [CrossRef]
- Walsh, T.P.; Arnold, J.B.; Evans, A.M.; Yaxley, A.; Damarell, R.A.; Shanahan, E.M. The Association between Body Fat and Musculoskeletal Pain: A Systematic Review and Meta-Analysis. BMC Musculoskelet. Disord. 2018, 19, 233. [Google Scholar] [CrossRef]
- Dzakpasu, F.Q.S.; Carver, A.; Brakenridge, C.J.; Cicuttini, F.; Urquhart, D.M.; Owen, N.; Dunstan, D.W. Musculoskeletal Pain and Sedentary Behaviour in Occupational and Non-Occupational Settings: A Systematic Review with Meta-Analysis. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 159. [Google Scholar] [CrossRef]
- Brady, S.R.; Mamuaya, B.B.; Cicuttini, F.; Wluka, A.E.; Wang, Y.; Hussain, S.M.; Urquhart, D.M. Body Composition is Associated with Multisite Lower Body Musculoskeletal Pain in a Community-Based Study. J. Pain 2015, 16, 700–706. [Google Scholar] [CrossRef]
- Alkassabi, O.; Voogt, L.; Andrews, P.; Alhowimel, A.; Nijs, J.; Alsobayel, H. Risk Factors to Persistent Pain Following Musculoskeletal Injuries: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 9318. [Google Scholar] [CrossRef]
- Uchida, K.; Murata, S.; Kawaharada, R.; Tsuboi, Y.; Isa, T.; Okumura, M.; Matsuda, N.; Nakatsuka, K.; Horibe, K.; Kogaki, M.; et al. Association Between Kinesiophobia and Life Space Among Community-Dwelling Older People with Chronic Musculoskeletal Pain. Pain Med. 2020, 21, 3360–3365. [Google Scholar] [CrossRef]
- Vargas-Prada, S.; Coggon, D. Psychological and Psychosocial Determinants of Musculoskeletal Pain and Associated Disability. Best Pract. Res. Clin. Rheumatol. 2015, 29, 374–390. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, D.H.; Nielsen, K.J.; Andersen, D.R.; Andersen, J.H. Musculoskeletal Health Climate is Associated with Musculoskeletal Pain and Sickness Absence among Workers: A Cross-Sectional Study. BMJ Open 2022, 12, e056485. [Google Scholar] [CrossRef]
- Nygaard, N.-P.B.; Thomsen, G.F.; Rasmussen, J.; Skadhauge, L.R.; Gram, B. Ergonomic and Individual Risk Factors for Musculoskeletal Pain in the Ageing Workforce. BMC Public Health 2022, 22, 1975. [Google Scholar] [CrossRef]
- Neupane, S.; Nygård, C.-H.; Prakash, K.C.; von Bonsdorff, M.B.; von Bonsdorff, M.E.; Seitsamo, J.; Rantanen, T.; Ilmarinen, J.; Leino-Arjas, P. Multisite Musculoskeletal Pain Trajectories from Midlife to Old Age: A 28-year Follow-Up of Municipal Employees. Occup. Environ. Med. 2018, 75, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Finnerup, N.B.; Kuner, R.; Jensen, T.S. Neuropathic Pain: From Mechanisms to Treatment. Physiol. Rev. 2021, 101, 259–301. [Google Scholar] [CrossRef] [PubMed]
- Bouhassira, D. Neuropathic pain: Definition, assessment and epidemiology. Rev. Neurol. 2019, 175, 16–25. [Google Scholar] [CrossRef]
- Colloca, L.; Ludman, T.; Bouhassira, D.; Baron, R.; Dickenson, A.H.; Yarnitsky, D.; Freeman, R.; Truini, A.; Attal, N.; Finnerup, N.; et al. Neuropathic pain. Nat. Rev. Dis. Primers 2017, 3, 17002. [Google Scholar] [CrossRef]
- Dib-Hajj, S.D.; Waxman, S.G. Sodium Channels in Human Pain Disorders: Genetics and Pharmacogenomics. Annu. Rev. Neurosci. 2019, 42, 87–106. [Google Scholar] [CrossRef]
- Han, C.; Themistocleous, A.C.; Estacion, M.; Dib-Hajj, F.B.; Blesneac, I.; Macala, L.; Fratter, C.; Bennett, D.L.; Waxman, S.G.; Dib-Hajj, S.D. The Novel Activity of Carbamazepine as an Activation Modulator Extends from NaV1.7 Mutations to the NaV1.8-S242T Mutant Channel from a Patient with Painful Diabetic Neuropathy. Mol. Pharmacol. 2018, 94, 1256–1269. [Google Scholar] [CrossRef] [PubMed]
- Kremeyer, B.; Lopera, F.; Cox, J.J.; Momin, A.; Rugiero, F.; Marsh, S.; Woods, C.G.; Jones, N.G.; Paterson, K.J.; Fricker, F.R.; et al. A Gain-of-Function Mutation in TRPA1 Causes Familial Episodic Pain Syndrome. Neuron 2010, 66, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Jensen, T.S.; Finnerup, N.B. Allodynia and Hyperalgesia in Neuropathic Pain: Clinical Manifestations and Mechanisms. Lancet Neurol. 2014, 13, 924–935. [Google Scholar] [CrossRef]
- van Hecke, O.; Austin, S.K.; Khan, R.A.; Smith, B.H.; Torrance, N. Neuropathic Pain in the General Population: A Systematic Review of Epidemiological Studies. Pain 2014, 155, 654–662. [Google Scholar] [CrossRef]
- Fernandes, Q.; Inchakalody, V.P.; Merhi, M.; Mestiri, S.; Taib, N.; El-Ella, D.M.A.; Bedhiafi, T.; Raza, A.; Al-Zaidan, L.; Mohsen, M.O.; et al. Emerging COVID-19 Variants and Their Impact on SARS-CoV-2 Diagnosis, Therapeutics and Vaccines. Ann. Med. 2022, 54, 524–540. [Google Scholar] [CrossRef]
- Kaye, A.D.; Okeagu, C.N.; Pham, A.D.; Silva, R.A.; Hurley, J.J.; Arron, B.L.; Sarfraz, N.; Lee, H.N.; Ghali, G.E.; Gamble, J.W.; et al. Economic Impact of COVID-19 Pandemic on Healthcare Facilities and Systems: International Perspectives. Best Pract. Res. Clin. Anaesthesiol. 2021, 35, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Colenda, C.C.; Applegate, W.B.; Reifler, B.V.; Blazer, D.G., 2nd. COVID-19: Financial Stress Test for Academic Medical Centers. Acad. Med. 2020, 95, 1143–1145. [Google Scholar] [CrossRef]
- DeMartino, J.K.; Swallow, E.; Goldschmidt, D.; Yang, K.; Viola, M.; Radtke, T.; Kirson, N. Direct Health Care Costs Associated with COVID-19 in the United States. J. Manag. Care Spéc. Pharm. 2022, 28, 936–947. [Google Scholar] [CrossRef]
- Di Fusco, M.; Shea, K.M.; Lin, J.; Nguyen, J.L.; Angulo, F.J.; Benigno, M.; Malhotra, D.; Emir, B.; Sung, A.H.; Hammond, J.L.; et al. Health Outcomes and Economic Burden of Hospitalized COVID-19 Patients in the United States. J. Med. Econ. 2021, 24, 308–317. [Google Scholar] [CrossRef]
- Xu, H.; Intrator, O.; Bowblis, J.R. Shortages of Staff in Nursing Homes During the COVID-19 Pandemic: What are the Driving Factors? J. Am. Med. Dir. Assoc. 2020, 21, 1371–1377. [Google Scholar] [CrossRef]
- Shen, K.; McGarry, B.E.; Grabowski, D.C.; Gruber, J.; Gandhi, A.D. Staffing Patterns in US Nursing Homes During COVID-19 Outbreaks. JAMA Health Forum 2022, 3, e222151. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.K.; Carter, M.W.; Nelson, H.W. Trends in COVID-19 Cases, Deaths, and Staffing Shortages in US Nursing Homes by Rural and Urban Status. Geriatr. Nurs. 2021, 42, 1356–1361. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.A.; Rocco, G.; Stievano, A. Nurse and Health Professional Migration during COVID-19. Prof. Inferm. 2020, 73, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Mascha, E.J.; Schober, P.; Schefold, J.C.; Stueber, F.; Luedi, M.M. Staffing With Disease-Based Epidemiologic Indices May Reduce Shortage of Intensive Care Unit Staff During the COVID-19 Pandemic. Anesth Analg. 2020, 131, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Doraiswamy, S.; Abraham, A.; Mamtani, R.; Cheema, S. Use of Telehealth During the COVID-19 Pandemic: Scoping Review. J. Med. Internet Res. 2020, 22, e24087. [Google Scholar] [CrossRef] [PubMed]
- Wijesooriya, N.R.; Mishra, V.; Brand, P.L.; Rubin, B.K. COVID-19 and Telehealth, Education, and Research Adaptations. Paediatr. Respir. Rev. 2020, 35, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Garfan, S.; Alamoodi, A.; Zaidan, B.; Al-Zobbi, M.; Hamid, R.A.; Alwan, J.K.; Ahmaro, I.Y.; Khalid, E.T.; Jumaah, F.; Albahri, O.; et al. Telehealth Utilization during the COVID-19 Pandemic: A Systematic Review. Comput. Biol. Med. 2021, 138, 104878. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major Findings, Mechanisms and Recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Akbarialiabad, H.; Taghrir, M.H.; Abdollahi, A.; Ghahramani, N.; Kumar, M.; Paydar, S.; Razani, B.; Mwangi, J.; Asadi-Pooya, A.A.; Malekmakan, L.; et al. Long COVID, a Comprehensive Systematic Scoping Review. Infection 2021, 49, 1163–1186. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Navarro-Santana, M.P.; Plaza-Manzano, G.; Palacios-Ceña, D.; Arendt-Nielsen, L.D.M. Time Course Prevalence of Post-COVID Pain Symptoms of Musculoskeletal Origin in Patients who had Survived Severe Acute Respiratory Syndrome Coronavirus 2 Infection: A Systematic Review and Meta-Analysis. Pain 2022, 163, 1220–1231. [Google Scholar] [CrossRef] [PubMed]
- Karaarslan, F.; Güneri, F.D.; Kardeş, S. Long COVID: Rheumatologic/Musculoskeletal Symptoms in Hospitalized COVID-19 Survivors at 3 and 6 Months. Clin. Rheumatol. 2022, 41, 289–296. [Google Scholar] [CrossRef]
- Awosanya, O.D.; Dadwal, U.C.; Imel, E.A.; Yu, Q.; Kacena, M.A. The Impacts of COVID-19 on Musculoskeletal Health. Curr. Osteoporos. Rep. 2022, 20, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Ramani, S.L.; Samet, J.; Franz, C.K.; Hsieh, C.; Nguyen, C.V.; Horbinski, C.; Deshmukh, S. Musculoskeletal Involvement of COVID-19: Review of Imaging. Skelet. Radiol. 2021, 50, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Nogueira, Ó.; Leirós-Rodríguez, R.; Benítez-Andrades, J.; Álvarez-Álvarez, M.; Marqués-Sánchez, P.; Pinto-Carral, A. Musculoskeletal Pain and Teleworking in Times of the COVID-19: Analysis of the Impact on the Workers at Two Spanish Universities. Int. J. Environ. Res. Public Health 2020, 18, 31. [Google Scholar] [CrossRef]
- Salameh, M.A.; Boyajian, S.D.; Odeh, H.N.; Amaireh, E.A.; Funjan, K.I.; Al-Shatanawi, T.N. Increased Incidence of Musculoskeletal Pain in Medical Students during Distance Learning Necessitated by the COVID-19 Pandemic. Clin. Anat. 2022, 35, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Hirko, K.A.; Kerver, J.M.; Ford, S.; Szafranski, C.; Beckett, J.; Kitchen, C.; Wendling, A.L. Telehealth in Response to the COVID-19 Pandemic: Implications for Rural Health Disparities. J. Am. Med. Informatics Assoc. 2020, 27, 1816–1818. [Google Scholar] [CrossRef]
- Joshi, D.; Gyanpuri, V.; Pathak, A.; Chaurasia, R.N.; Mishra, V.N.; Kumar, A.; Singh, V.K.; Dhiman, N.R. Neuropathic Pain Associated with COVID-19: A Systematic Review of Case Reports. Curr. Pain Headache Rep. 2022, 26, 595–603. [Google Scholar] [CrossRef]
- Su, S.; Cui, H.; Wang, T.; Shen, X.; Ma, C. Pain: A Potential New Label of COVID-19. Brain Behav. Immun. 2020, 87, 159–160. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Nijs, J.; Neblett, R.; Polli, A.; Moens, M.; Goudman, L.; Patil, M.S.; Knaggs, R.D.; Pickering, G.; Arendt-Nielsen, L. Phenotyping Post-COVID Pain as a Nociceptive, Neuropathic, or Nociplastic Pain Condition. Biomedicines 2022, 10, 2562. [Google Scholar] [CrossRef]
- Herrero-Montes, M.; Fernández-De-Las-Peñas, C.; Ferrer-Pargada, D.; Tello-Mena, S.; Cancela-Cilleruelo, I.; Rodríguez-Jiménez, J.; Palacios-Ceña, D.; Parás-Bravo, P. Prevalence of Neuropathic Component in Post-COVID Pain Symptoms in Previously Hospitalized COVID-19 Survivors. Int. J. Clin. Pract. 2022, 2022, 3532917. [Google Scholar] [CrossRef] [PubMed]
- Fernández-De-Las-Peñas, C.; Valera-Calero, J.A.; Herrero-Montes, M.; Del-Valle-Loarte, P.; Rodríguez-Rosado, R.; Ferrer-Pargada, D.; Arendt-Nielsen, L.; Parás-Bravo, P. The Self-Reported Leeds Assessment of Neuropathic Symptoms and Signs (S-LANSS) and PainDETECT Questionnaires in COVID-19 Survivors with Post-COVID Pain. Viruses 2022, 14, 1486. [Google Scholar] [CrossRef] [PubMed]
- Shanthanna, H.; Nelson, A.M.; Kissoon, N.; Narouze, S. The COVID-19 Pandemic and Its Consequences for Chronic Pain: A Narrative Review. Anaesthesia 2022, 77, 1039–1050. [Google Scholar] [CrossRef] [PubMed]
- Kemp, H.I.; Corner, E.; Colvin, L.A. Chronic Pain after COVID-19: Implications for Rehabilitation. Br. J. Anaesth. 2020, 125, 436–440. [Google Scholar] [CrossRef]
- Fiala, K.; Martens, J.; Abd-Elsayed, A. Post-COVID Pain Syndromes. Curr. Pain Headache Rep. 2022, 26, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Puntillo, F.; Giglio, M.; Brienza, N.; Viswanath, O.; Urits, I.; Kaye, A.D.; Pergolizzi, J.; Paladini, A.; Varrassi, G. Impact of COVID-19 Pandemic on Chronic Pain Management: Looking for the Best Way to Deliver Care. Best Pract. Res. Clin. Anaesthesiol. 2020, 34, 529–537. [Google Scholar] [CrossRef] [PubMed]
- NEJM Catalyst. What is Telehealth? NEJM Catalyst 2018, 4, 1. [Google Scholar] [CrossRef]
- Chou, R.; Gordon, D.B.; de Leon-Casasola, O.A.; Rosenberg, J.M.; Bickler, S.; Brennan, T.; Carter, T.; Cassidy, C.L.; Chittenden, E.H.; Degenhardt, E.; et al. Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J. Pain 2016, 17, 131–157. [Google Scholar] [CrossRef]
- Slattery, B.W.; Haugh, S.; O’Connor, L.; Francis, K.; Dwyer, C.P.; O’Higgins, S.; Egan, J.; McGuire, B.E. An Evaluation of the Effectiveness of the Modalities Used to Deliver Electronic Health Interventions for Chronic Pain: Systematic Review With Network Meta-Analysis. J. Med. Internet Res. 2019, 21, e11086. [Google Scholar] [CrossRef]
- El-Tallawy, S.N.; Perglozzi, J.V.; Ahmed, R.S.; Kaki, A.M.; Nagiub, M.S.; LeQuang, J.K.; Hadarah, M.M. Pain Management in the Post-COVID Era—An Update: A Narrative Review. Pain Ther. 2023, 12, 423–448. [Google Scholar] [CrossRef]
- Areias, A.C.; Costa, F.; Janela, D.; Molinos, M.; Moulder, R.G.; Lains, J.; Scheer, J.K.; Bento, V.; Yanamadala, V.; Correia, F.D. Long-Term Clinical Outcomes of a Remote Digital Musculoskeletal Program: An Ad Hoc Analysis from a Longitudinal Study with a Non-Participant Comparison Group. Healthcare 2022, 10, 2349. [Google Scholar] [CrossRef]
- Gilam, G.; Gross, J.J.; Wager, T.D.; Keefe, F.J.; Mackey, S.C. What Is the Relationship between Pain and Emotion? Bridging Constructs and Communities. Neuron 2020, 107, 17–21. [Google Scholar] [CrossRef]
- Koppert, T.Y.; Jacobs, J.W.; Lumley, M.A.; Geenen, R. The Impact of COVID-19 Stress on Pain and Fatigue in People with and without a Central Sensitivity Syndrome. J. Psychosom. Res. 2021, 151, 110655. [Google Scholar] [CrossRef]
- Macfarlane, G.J.; Hollick, R.J.; Morton, L.; Heddle, M.; Bachmair, E.-M.; Anderson, R.S.; Whibley, D.; Keenan, K.F.; Murchie, P.; Stelfox, K.; et al. The Effect of COVID-19 Public Health Restrictions on the Health of People with Musculoskeletal Conditions and Symptoms: The CONTAIN Study. Rheumatology 2021, 60, SI13–SI24. [Google Scholar] [CrossRef]
- Harnik, M.A.; Blättler, L.; Limacher, A.; Reisig, F.; Grosse Holtforth, M.; Streitberger, K. Telemedicine for Chronic Pain Treatment during the COVID-19 Pandemic: Do Pain Intensity and Anxiousness Correlate with Patient Acceptance? Pain Pract. 2021, 21, 934–942. [Google Scholar] [CrossRef]
- Kleinmann, B.; Abberger, B.; Kieselbach, K.; Wolter, T. Patients with Chronic Pain Prefer Maintenance of Pain Treatment Despite COVID-19 Pandemic Restrictions. Pain Physician 2021, 24, 165–173. [Google Scholar]
- Bushnell, M.C.; Ceko, M.; Low, L.A. Cognitive and Emotional Control of Pain and its Disruption in Chronic Pain. Nat. Rev. Neurosci. 2013, 14, 502–511. [Google Scholar] [CrossRef]
- Edwards, R.R.; Dworkin, R.H.; Sullivan, M.D.; Turk, D.C.; Wasan, A.D. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. J. Pain 2016, 17 (Suppl. S9), T70–T92. [Google Scholar] [CrossRef] [PubMed]
- Crook, H.; Raza, S.; Nowell, J.; Young, M.; Edison, P. Long COVID—Mechanisms, Risk Factors, and Management. Br. Med. J. 2021, 374, n1648. [Google Scholar] [CrossRef] [PubMed]
- Clauw, D.J.; Häuser, W.; Cohen, S.P.; Fitzcharles, M.-A. Considering the Potential for an Increase in Chronic Pain after the COVID-19 Pandemic. Pain 2020, 161, 1694–1697. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, R.; Aghsaeifard, Z. Does COVID19 Activates Previous Chronic Pain? A Case Series. Ann. Med. Surg. 2021, 61, 169–171. [Google Scholar] [CrossRef] [PubMed]
- Fernández-De-Las-Peñas, C.M.; Cancela-Cilleruelo, I.P.; Moro-López-Menchero, P.P.; Rodríguez-Jiménez, J.P.; Pellicer-Valero, O.J.; Martín-Guerrero, J.D.; Arendt-Nielsen, L.M. Exploring the Trajectory Curve of Long-Term Musculoskeletal Post-COVID Pain Symptoms in Hospitalized COVID-19 Survivors: A Multicenter Study. Pain 2023, 164, 413–420. [Google Scholar] [CrossRef]
- Kubota, G.T.; Soares, F.H.C.; da Fonseca, A.S.; Rosa, T.d.S.; da Silva, V.A.; Gouveia, G.R.; Faria, V.G.; da Cunha, P.H.M.; Brunoni, A.R.; Teixeira, M.J.; et al. Pain Paths among Post-COVID-19 Condition Subjects: A Prospective Cross-Sectional Study with In-Person Evaluation. Eur. J. Pain 2023, 27, 636–650. [Google Scholar] [CrossRef] [PubMed]
- Fernández-De-Las-Peñas, C.D.M.; Rodríguez-Jiménez, J.; Fuensalida-Novo, S.P.; Palacios-Ceña, M.; Gómez-Mayordomo, V.; Florencio, L.L.; Hernández-Barrera, V.; Arendt-Nielsen, L.D.M. Myalgia as a Symptom at Hospital Admission by Severe Acute Respiratory Syndrome Coronavirus 2 Infection Is Associated with Persistent Musculoskeletal Pain as Long-Term Post-COVID Sequelae: A Case-Control Study. Pain 2021, 162, 2832–2840. [Google Scholar] [CrossRef]
- Alonso-Matielo, H.; Oliveira, V.R.d.S.; de Oliveira, V.T.; Dale, C.S. Pain in COVID Era. Front. Physiol. 2021, 12, 624154. [Google Scholar] [CrossRef] [PubMed]
- Bair, M.J.; Robinson, R.L.; Katon, W.; Kroenke, K. Depression and Pain Comorbidity: A literature Review. Arch. Intern. Med. 2003, 163, 2433–2445. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, J.-C.; Hannerz, J.; Ingvar, M. Right-Lateralised Central Processing for Pain of Nitroglycer-Induced Cluster Headache. Pain 1996, 67, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Shiner, C.T.; Gardner, T.; Haskelberg, H.; Li, I.; Faux, S.G.; Millard, M.; Mahoney, A.E.J. The Uptake and Effectiveness of a Multidisciplinary Online Program for Managing Chronic Pain before and During the COVID-19 Pandemic. Pain Med. 2022, 23, 1621–1630. [Google Scholar] [CrossRef]
- Eccleston, C.; Blyth, F.M.; Dear, B.F.; Fisher, E.A.; Keefe, F.J.; Lynch, M.E.; Palermo, T.M.; Reid, M.C.; de C Williams, A.C. Managing Patients with Chronic Pain during the COVID-19 Outbreak: Considerations for the Rapid Introduction of Remotely Supported (eHealth) Pain Management Services. Pain 2020, 161, 889–893. [Google Scholar] [CrossRef]
- Lacasse, A.; Pagé, M.G.; Dassieu, L.; Sourial, N.; Janelle-Montcalm, A.; Dorais, M.; Nguefack, H.L.N.; Godbout-Parent, M.; Hudspith, M.; Moor, G.; et al. Impact of the COVID-19 Pandemic on the Pharmacological, Physical, and Psychological Treatments of Pain: Findings from the Chronic Pain & COVID-19 Pan-Canadian Study. Pain Rep. 2021, 6, e891. [Google Scholar] [CrossRef] [PubMed]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The Biopsychosocial Approach to Chronic Pain: Scientific Advances and Future Directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef]
- Pangarkar, S.S.; Kang, D.G.; Sandbrink, F.; Bevevino, A.; Tillisch, K.; Konitzer, L.; Sall, J. VA/DoD Clinical Practice Guideline: Diagnosis and Treatment of Low Back Pain. J. Gen. Intern. Med. 2019, 34, 2620–2629. [Google Scholar] [CrossRef] [PubMed]
- Ojeda, A.; Calvo, A.; Cuñat, T.; Artigas, R.M.; Comino-Trinidad, O.; Aliaga, J.; Arias, M.; Ahuir, M.; Ferrando, C.; Dürsteler, C. Rationale and Study Design of an Early Care, Therapeutic Education, and Psychological Intervention Program for the Management of Post-Intensive Care Syndrome and Chronic Pain after COVID-19 Infection (PAIN-COVID): Study Protocol for a Randomized Controlled Trial. Trials 2021, 22, 486. [Google Scholar] [CrossRef]
- Flynn, D.M. Chronic Musculoskeletal Pain: Nonpharmacologic, Noninvasive Treatments. Am. Fam. Physician 2020, 102, 465–477. [Google Scholar]
- Ao, G.; Li, T.; Wang, Y.; Li, J.; Tran, C.; Chen, M.; Qi, X. Opioid Usage and COVID-19 Prognosis: A Systematic Review and Meta-Analysis. Am. J. Emerg. Med. 2022, 56, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Struyf, T.; Deeks, J.J.; Dinnes, J.; Takwoingi, Y.; Davenport, C.; Leeflang, M.M.; Spijker, R.; Hooft, L.; Emperador, D.; Domen, J.; et al. Signs and Symptoms to Determine if a Patient Presenting in Primary Care or Hospital Outpatient Settings Has COVID-19. Cochrane Database Syst. Rev. 2022, 5, CD013665. [Google Scholar] [CrossRef]
- Aylward, B.; Liang, W. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19); World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19) (accessed on 28 November 2023).
- Mottiar, M.; Hendin, A.; Fischer, L.; Roze des Ordons, A.; Hartwick, M. End-of-Life Care in Patients with a Highly Transmissible Respiratory Virus: Implications for COVID-19. Can. J. Anaesth. 2020, 67, 1417–1423. [Google Scholar] [CrossRef]
- Bonneau, A. Cough in the Palliative Care Setting. Can. Fam. Physician 2009, 55, 600–602. [Google Scholar] [PubMed]
- Andreas, M.; Piechotta, V.; Skoetz, N.; Grummich, K.; Becker, M.; Joos, L.; Becker, G.; Meissner, W.; Boehlke, C. Interventions for Palliative Symptom Control in COVID-19 Patients. Cochrane Database Syst. Rev. 2021, 8, CD015061. [Google Scholar] [CrossRef]
- Smith, V.; Warty, R.R.; Sursas, J.A.; Payne, O.; Nair, A.; Krishnan, S.; Costa, F.d.S.; Wallace, E.M.; Vollenhoven, B. The Effectiveness of Virtual Reality in Managing Acute Pain and Anxiety for Medical Inpatients: Systematic Review. J. Med. Internet Res. 2020, 22, e17980. [Google Scholar] [CrossRef]
- Pallavicini, F.; Pepe, A.; Clerici, M.; Mantovani, F. Virtual Reality Applications in Medicine During the COVID-19 Pandemic: Systematic Review. JMIR Serious Games 2022, 10, e35000. [Google Scholar] [CrossRef]
- Hetherington, L.; Johnston, B.; Kotronoulas, G.; Finlay, F.; Keeley, P.; McKeown, A. COVID-19 and Hospital Palliative Care—A Service Evaluation Exploring the Symptoms and Outcomes of 186 Patients and the Impact of the Pandemic on Specialist Hospital Palliative Care. Palliat. Med. 2020, 34, 1256–1262. [Google Scholar] [CrossRef]
- Strang, P.; Martinsson, L.; Bergström, J.; Lundström, S. COVID-19: Symptoms in Dying Residents of Nursing Homes and in Those Admitted to Hospitals. J. Palliat. Med. 2021, 24, 1067–1071. [Google Scholar] [CrossRef]
- Dantzer, R.; O’Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From Inflammation to Sickness and Depression: When the Immune System Subjugates the Brain. Nat. Rev. Neurosci. 2008, 9, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.D.; Duricka, D.L. Stellate Ganglion Block Reduces Symptoms of Long COVID: A Case Series. J. Neuroimmunol. 2022, 362, 577784. [Google Scholar] [CrossRef] [PubMed]
- Patterson, B.K.; Guevara-Coto, J.; Yogendra, R.; Francisco, E.B.; Long, E.; Pise, A.; Rodrigues, H.; Parikh, P.; Mora, J.; Mora-Rodríguez, R.A. Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning. Front. Immunol. 2021, 12, 700782. [Google Scholar] [CrossRef] [PubMed]
- Puente de la Vega Costa, K.; Perez, M.A.G.; Roqueta, C.; Fischer, L. Effects on Hemodynamic Variables and Echocardiographic Parameters after a Stellate Ganglion Block in 15 Healthy Volunteers. Auton. Neurosci. 2016, 197, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Fischer, L.; Barop, H.; Ludin, S.M.; Schaible, H.-G. Regulation of Acute Reflectory Hyperinflammation in Viral and Other Diseases by Means of Stellate Ganglion Block. A Conceptual View with a Focus on COVID-19. Auton. Neurosci. 2021, 237, 102903. [Google Scholar] [CrossRef] [PubMed]
- Fischer, L. Neuraltherapie: Neurophysiologie, Injektionstechnik und Therapievorschläge, 5th ed.; Thieme: Stuttgart, Germany, 2019; ISBN 9783132426863. [Google Scholar]
- Khan, M.H.; Kirkpatrick, K.P.; Deng, Y.; Shah, K.B. Stellate Ganglion Block for Long COVID Symptom Management: A Case Report. Cureus 2022, 14, e32295. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, G.; Upadhyay, A.; Khanduja, S.; Emerick, T. Stellate Ganglion Block for Anosmia and Dysgeusia Due to Long COVID. Cureus 2022, 14, e27779. [Google Scholar] [CrossRef]
- Pinto, C.N.; Oliveira, E.; Agualusa, L. Stellate Ganglion Block for Complex Regional Pain Syndrome Treatment After SARS-CoV-2 Vaccine: A Case Report. Cureus 2023, 15, e38318. [Google Scholar] [CrossRef]
- Kirkpatrick, K.; Khan, M.H.; Deng, Y.; Shah, K.B. A Review of Stellate Ganglion Block as an Adjunctive Treatment Modality. Cureus 2023, 15, e35174. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Krames, E.; Peckham, H.P.; Rezai, A.R. Neuromodulation: Comprehensive Textbook of Pinciples, Technologies, and Therapies, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 9780128053539. [Google Scholar]
- Bonaz, B.; Sinniger, V.; Pellissier, S. Targeting the Cholinergic Anti-Inflammatory Pathway with Vagus Nerve Stimulation in Patients with COVID-19? Bioelectron. Med. 2020, 6, 15. [Google Scholar] [CrossRef] [PubMed]
- Fact Sheet for Healthcare Providers: Emergency Use of gammaCore Sapphire CV During the COVID-19 Pandemic; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2020.
- Tornero, C.; Pastor, E.; Garzando, M.D.M.; Orduña, J.; Forner, M.J.; Bocigas, I.; Cedeño, D.L.; Vallejo, R.; McClure, C.K.; Czura, C.J.; et al. Non-invasive Vagus Nerve Stimulation for COVID-19: Results From a Randomized Controlled Trial (SAVIOR I). Front. Neurol. 2022, 13, 820864. [Google Scholar] [CrossRef]
- Verbanck, P.; Clarinval, A.M.; Burton, F.; Corazza, F.; Nagant, C.; Cheron, G. Transcutaneous Auricular Vagus Nerve Stimulation (tVNS) can Reverse the Manifestations of the Long-COVID Syndrome: A Pilot Study. Adv. Neurol Nerosci Res. 2021, 2, 10. [Google Scholar] [CrossRef]
- Badran, B.W.; Huffman, S.M.; Dancy, M.; Austelle, C.W.; Bikson, M.; Kautz, S.A.; George, M.S. A Pilot Randomized Controlled Trial of Supervised, At-Home, Self-Administered Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) to Manage Long COVID Symptoms. Bioelectron. Med. 2022, 8, 13. [Google Scholar] [CrossRef]
- Vagal Nerve Stimulation for Post COVID Fatigue. ClinicalTrials.gov Identifier: NCT05445427. 2023; [Updated 14 February 2023]. Available online: https://clinicaltrials.gov/study/NCT05445427?id=NCT05445427&rank=1 (accessed on 28 November 2023).
- O’Kelly, B.; Vidal, L.; McHugh, T.; Woo, J.; Avramovic, G.; Lambert, J.S. Safety and Efficacy of Low Dose Naltrexone in a Long COVID Cohort: An Interventional Pre-Post Study. Brain Behav. Immun.-Health 2022, 24, 100485. [Google Scholar] [CrossRef]
- Drożdżal, S.; Rosik, J.; Lechowicz, K.; Machaj, F.; Szostak, B.; Majewski, P.; Rotter, I.; Kotfis, K. COVID-19: Pain Management in Patients with SARS-CoV-2 Infection—Molecular Mechanisms, Challenges, and Perspectives. Brain Sci. 2020, 10, 465. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Nijs, J.; Giordano, R.; Arendt-Nielsen, L. Precision Management of Post-COVID Pain: An Evidence and Clinical-Based Approach. Eur. J. Pain 2023, 27, 1107–1125. [Google Scholar] [CrossRef]
- Pal, A.; Roongta, R.; Mondal, S.; Sinha, D.; Sinhamahapatra, P.; Ghosh, A.; Chattopadhyay, A. Does Post-COVID Reactive Arthritis Exist? Experience of a Tertiary Care Centre with a Review of the Literature. Reumatol. Clin. 2023, 19, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Cordani, C.; Lazzarini, S.G.; DEL Furia, M.J.; Kiekens, C.; Arienti, C.; Negrini, S. Arthralgia: A Map of Cochrane Evidence Relevant to Rehabilitation for People with Post COVID-19 Condition. Eur. J. Phys. Rehabil. Med. 2022, 58, 870–874. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.; Flores, J.A. Musculoskeletal Physiotherapy in Physical Sequelae of SARS-CoV-2 Infection: A Case Report. Physiother. Res. Int. 2022, 27, e1938. [Google Scholar] [CrossRef] [PubMed]
- Scuteri, D.; Guida, F.; Boccella, S.; Palazzo, E.; Maione, S.; Rodríguez-Landa, J.F.; Martínez-Mota, L.; Tonin, P.; Bagetta, G.; Corasaniti, M.T. Effects of Palmitoylethanolamide (PEA) on Nociceptive, Musculoskeletal and Neuropathic Pain: Systematic Review and Meta-Analysis of Clinical Evidence. Pharmaceutics 2022, 14, 1672. [Google Scholar] [CrossRef] [PubMed]
- Fonnesu, R.; Thunuguntla, V.B.S.C.; Veeramachaneni, G.K.; Bondili, J.S.; La Rocca, V.; Filipponi, C.; Spezia, P.G.; Sidoti, M.; Plicanti, E.; Quaranta, P.; et al. Palmitoylethanolamide (PEA) Inhibits SARS-CoV-2 Entry by Interacting with S Protein and ACE-2 Receptor. Viruses 2022, 14, 1080. [Google Scholar] [CrossRef] [PubMed]
- Raciti, L.; De Luca, R.; Raciti, G.; Arcadi, F.A.; Calabrò, R.S. The Use of Palmitoylethanolamide in the Treatment of Long COVID: A Real-Life Retrospective Cohort Study. Med. Sci. 2022, 10, 37. [Google Scholar] [CrossRef]
- Finnerup, N.B.; Attal, N.; Haroutounian, S.; McNicol, E.; Baron, R.; Dworkin, R.H.; Gilron, I.; Haanpää, M.; Hansson, P.; Jensen, T.S.; et al. Pharmacotherapy for Neuropathic Pain in Adults: A Systematic Review and Meta-Analysis. Lancet Neurol. 2015, 14, 162–173. [Google Scholar] [CrossRef]
- Frontera, J.A.; Thorpe, L.E.; Simon, N.M.; de Havenon, A.; Yaghi, S.; Sabadia, S.B.; Yang, D.; Lewis, A.; Melmed, K.; Balcer, L.J.; et al. Post-Acute Sequelae of COVID-19 Symptom Phenotypes and Therapeutic Strategies: A Prospective, Observational Study. PLoS ONE 2022, 17, e0275274. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lam, C.M.; Sanderson, M.; Vu, D.T.; Sayed, D.; Latif, U.; Chadwick, A.L.; Staats, P.; York, A.; Smith, G.; Velagapudi, V.; et al. Musculoskeletal and Neuropathic Pain in COVID-19. Diagnostics 2024, 14, 332. https://doi.org/10.3390/diagnostics14030332
Lam CM, Sanderson M, Vu DT, Sayed D, Latif U, Chadwick AL, Staats P, York A, Smith G, Velagapudi V, et al. Musculoskeletal and Neuropathic Pain in COVID-19. Diagnostics. 2024; 14(3):332. https://doi.org/10.3390/diagnostics14030332
Chicago/Turabian StyleLam, Christopher M., Miles Sanderson, Dan T. Vu, Dawood Sayed, Usman Latif, Andrea L. Chadwick, Peter Staats, Abigail York, Gabriella Smith, Vivek Velagapudi, and et al. 2024. "Musculoskeletal and Neuropathic Pain in COVID-19" Diagnostics 14, no. 3: 332. https://doi.org/10.3390/diagnostics14030332
APA StyleLam, C. M., Sanderson, M., Vu, D. T., Sayed, D., Latif, U., Chadwick, A. L., Staats, P., York, A., Smith, G., Velagapudi, V., & Khan, T. W. (2024). Musculoskeletal and Neuropathic Pain in COVID-19. Diagnostics, 14(3), 332. https://doi.org/10.3390/diagnostics14030332







