Exploring the Challenges of Using Minimal Invasive Surgery to Treat Stress Urinary Incontinence: Insights from a Retrospective Case-Control Study
Abstract
1. Introduction
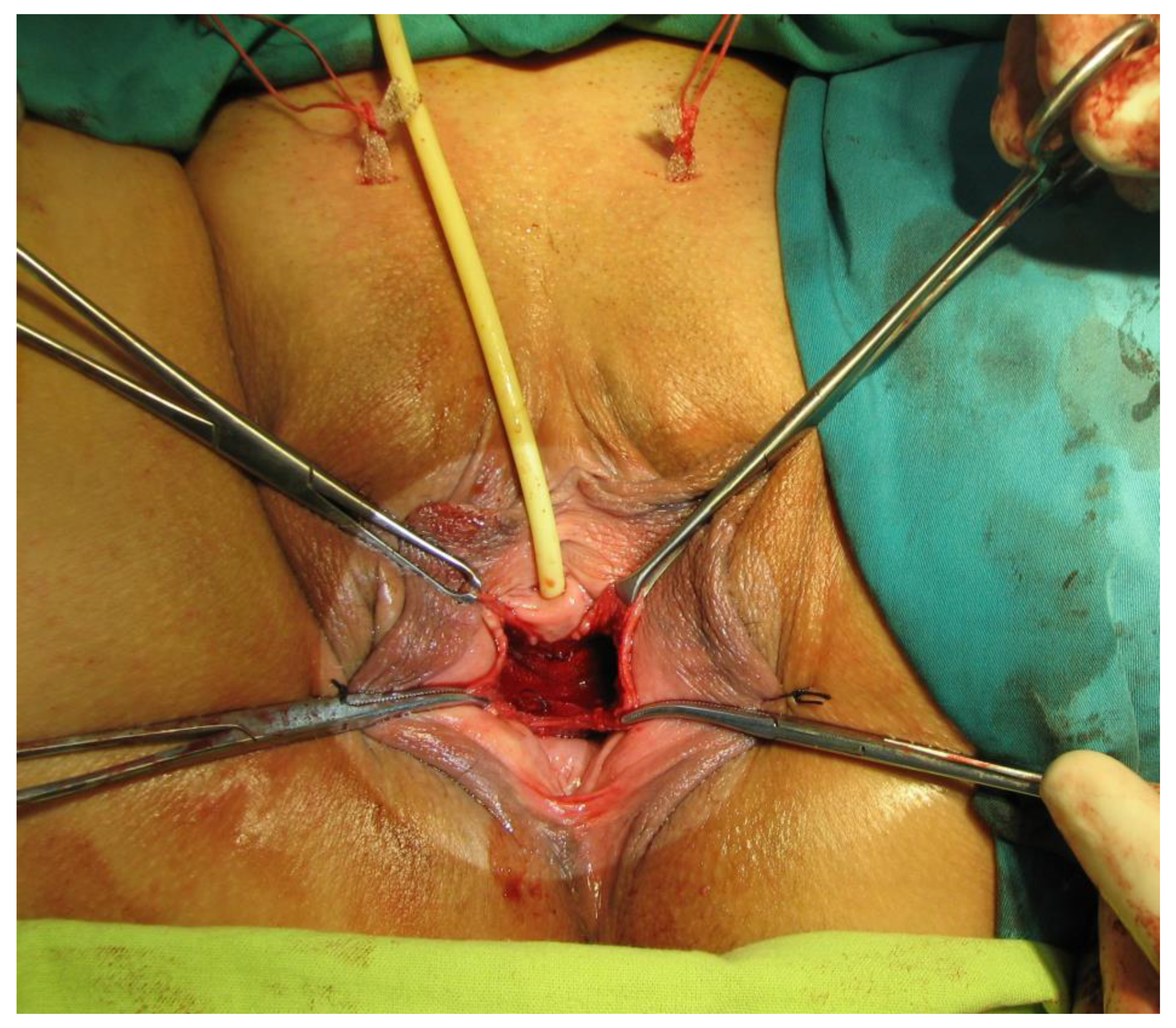
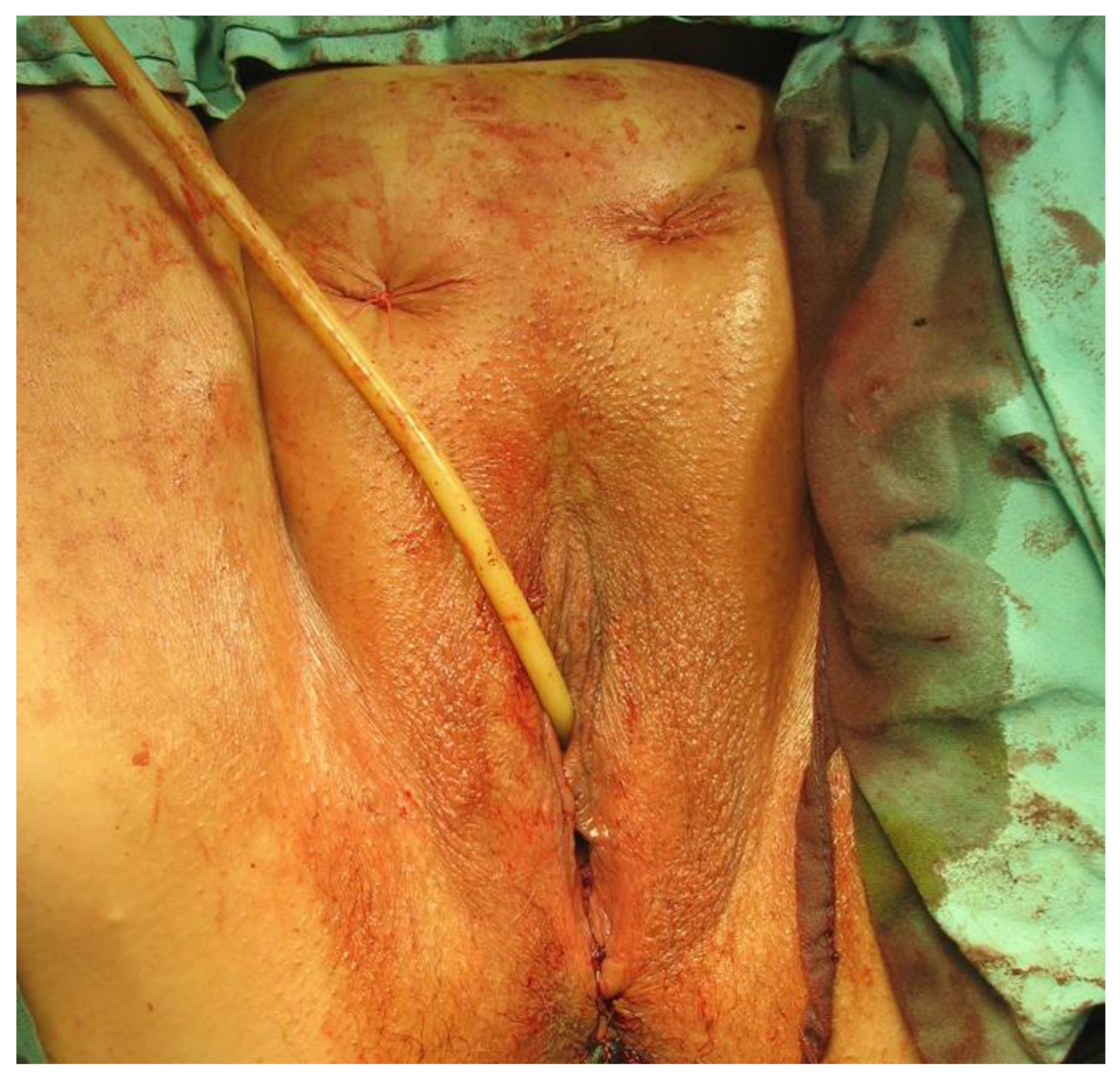
2. Materials and Method
3. Results
4. Discussion
5. Conclusions
Study Limitations and Strengths
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harland, N.; Walz, S.; Eberli, D.; Schmid, F.A.; Aicher, W.K.; Stenzl, A.; Amend, B. Stress Urinary Incontinence: An Unsolved Clinical Challenge. Biomedicines 2023, 11, 2486. [Google Scholar] [CrossRef] [PubMed]
- Debus, G.; Kästner, R. Psychosomatic Aspects of Urinary Incontinence in Women. Geburtshilfe Frauenheilkd. 2015, 75, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Chow, P.-M.; Chuang, Y.-C.; Hsu, K.C.P.; Shen, Y.-C.; Liu, S.-P. Impact of Female Stress Urinary Incontinence on Quality of Life, Mental Health, Work Limitation, and Healthcare Seeking in China, Taiwan, and South Korea (LUTS Asia): Results from a Cross-Sectional, Population-Based Study. Int. J. Women’s Health 2022, 14, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.Q.; Xia, M.C.; Cui, F.; Chen, J.W.; Bian, X.D.; Xie, H.J.; Shuang, W.B. Epidemiological Survey of Adult Female Stress Urinary Incontinence. BMC Women’s Health 2021, 21, 172. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.-M.; Xiao, H.; Ji, Z.-G.; Yan, W.-G.; Zhang, Y.-S. TVT versus TOT in the Treatment of Female Stress Urinary Incontinence: A Systematic Review and Meta-Analysis. Ther. Clin. Risk Manag. 2018, 14, 2293–2303. [Google Scholar] [CrossRef] [PubMed]
- Ulmsten, U.; Henriksson, L.; Johnson, P.; Varhos, G. An Ambulatory Surgical Procedure under Local Anesthesia for Treatment of Female Urinary Incontinence. Int. Urogynecol. J. 1996, 7, 81–86. [Google Scholar] [CrossRef]
- Ulmsten, U.; Falconer, C.; Johnson, P.; Jomaa, M.; Lannér, L.; Nilsson, C.G.; Olsson, I. A Multicenter Study of Tension-Free Vaginal Tape (TVT) for Surgical Treatment of Stress Urinary Incontinence. Int. Urogynecol. J. 1998, 9, 210–213. [Google Scholar] [CrossRef]
- Ford, A.A.; Rogerson, L.; Cody, J.D.; Aluko, P.; Ogah, J.A. Mid-Urethral Sling Operations for Stress Urinary Incontinence in Women. Cochrane Database Syst. Rev. 2017, 2017, CD006375. [Google Scholar] [CrossRef]
- Mishra, V.; Verneker, R.; Lamba, S. Bladder Perforation: A Missed Diagnosis Posttransobturator Tape. J. Mid-Life Health 2018, 9, 216. [Google Scholar] [CrossRef] [PubMed]
- Peyrat, L.; Boutin, J.M.; Bruyere, F.; Haillot, O.; Fakfak, H.; Lanson, Y. Intestinal Perforation as a Complication of Tension–Free Vaginal Tape Procedure for Urinary Incontinence. Eur. Urol. 2001, 39, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Delorme, E. Transobturator Urethral Suspension: Mini-Invasive Procedure in the Treatment of Urinary Stress Incontinence in Women. Prog. Urol. 2001, 11, 1306–1313. [Google Scholar]
- Wolf, M.T.; Carruthers, C.A.; Dearth, C.L.; Crapo, P.M.; Huber, A.; Burnsed, O.A.; Londono, R.; Johnson, S.A.; Daly, K.A.; Stahl, E.C.; et al. Polypropylene Surgical Mesh Coated with Extracellular Matrix Mitigates the Host Foreign Body Response: Polypropylene Surgical Mesh Coated with ECM. J. Biomed. Mater. Res. 2014, 102, 234–246. [Google Scholar] [CrossRef]
- Grigore, N.; Pirvut, V.; Mihai, I.; Hasegan, A.; Antonescu, E.; Coldea, L.; Mitariu, S.I.C. Polypropylene Mesh in Minimally Invasive Treatment of Female Stress Urinary Incontinence. Mater. Plast. 2017, 54, 635–638. [Google Scholar] [CrossRef]
- Saha, T.; Wang, X.; Padhye, R.; Houshyar, S. A Review of Recent Developments of Polypropylene Surgical Mesh for Hernia Repair. OpenNano 2022, 7, 100046. [Google Scholar] [CrossRef]
- ElSheemy, M.S.; Ghamrawy, H.; Fathy, H.; Hussein, H.A.; Hussein, E.A.; Aly, A.; Rahman, S.A. Use of Surgeon-Tailored Polypropylene Mesh as a Needle-Less Single-Incision Sling for Treating Female Stress Urinary Incontinence: Preliminary Results. Arab J. Urol. 2015, 13, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Grigore, N.; Pirvut, V.; Mihai, I.; Cernusca Mitariu, S.I.; Sava, M.; Hasegan, A. A Polymer Ligating Clips in Urologic Laparoscopic Surgery. Mater. Plast. 2017, 54, 295–297. [Google Scholar] [CrossRef]
- MacCraith, E.; O’Brien, F.J.; Davis, N.F. Biodegradable Materials for Surgical Management of Stress Urinary Incontinence: A Narrative Review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 259, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Karim, N.B.; Lo, T.-S.; Nawawi, E.A.B.; Wu, P.-Y. Review on Midurethral Sling Procedures for Stress Urinary Incontinence. Gynecol. Minim. Invasive Ther. 2015, 4, 33–36. [Google Scholar] [CrossRef]
- AlQuaiz, A.M.; Kazi, A.; AlYousefi, N.; Alwatban, L.; AlHabib, Y.; Turkistani, I. Urinary Incontinence Affects the Quality of Life and Increases Psychological Distress and Low Self-Esteem. Healthcare 2023, 11, 1772. [Google Scholar] [CrossRef] [PubMed]
- Mangir, N.; Aldemir Dikici, B.; Chapple, C.R.; MacNeil, S. Landmarks in Vaginal Mesh Development: Polypropylene Mesh for Treatment of SUI and POP. Nat. Rev. Urol. 2019, 16, 675–689. [Google Scholar] [CrossRef] [PubMed]
- Mayekar, R.; Bhosale, A.; Kandhari, K.; Nandanwar, Y.; Shaikh, S. A Study of Transobturator Tape in Stress Urinary Incontinence. Urol. Ann. 2017, 9, 9. [Google Scholar] [CrossRef]
- Harding, C.K.; Horsburgh, B.; Page, T.; Thorpe, A.C. A Prospective Study of Surgeon and Patient-Perceived Outcome Following Transobturator Tape Insertion for Treatment of Urodynamic Stress Incontinence. Br. J. Med. Surg. Urol. 2009, 2, 197–201. [Google Scholar] [CrossRef]
- Ward, K.; Hilton, P. UK and Ireland TVT Trial Group Tension-free Vaginal Tape versus Colposuspension for Primary Urodynamic Stress Incontinence: 5-year Follow Up. BJOG 2008, 115, 226–233. [Google Scholar] [CrossRef]
- Abrar, S.; Razzak, L.; Rizvi, R.M. The Practice of Burch Colposuspension versus Mid Urethral Slings for the Treatment of Stress Urinary Incontinence in Developing Country. Pak. J. Med. Sci. 2021, 37, 1359. [Google Scholar] [CrossRef] [PubMed]
- Szymański, J.K.; Zaręba, K.; Jakiel, G.; Słabuszewska-Jóźwiak, A. Intraoperative and Early Postoperative Complications in Women with Stress Urinary Incontinence Treated with Suburethral Slings: A Randomised Trial. Videosurg. Miniinv. 2020, 15, 18–29. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, B.D.; McCreery, A.; Redmond, A.E.; Keane, D.P. The Efficacy and Complications of Retropubic Tension-free Vaginal Tapes after 20 Years: A Prospective Observational Study. BJOG 2023, 130, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Rechberger, T.; Futyma, K.; Jankiewicz, K.; Adamiak, A.; Skorupski, P. The Clinical Effectiveness of Retropubic (IVS-02) and Transobturator (IVS-04) Midurethral Slings: Randomized Trial. Eur. Urol. 2009, 56, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Barski, D.; Deng, D.Y. Management of Mesh Complications after SUI and POP Repair: Review and Analysis of the Current Literature. BioMed Res. Int. 2015, 2015, 831285. [Google Scholar] [CrossRef]
- Codru, I.R.; Sava, M.; Vintilă, B.I.; Bereanu, A.S.; Bîrluțiu, V. A Study on the Contributions of Sonication to the Identification of Bacteria Associated with Intubation Cannula Biofilm and the Risk of Ventilator-Associated Pneumonia. Medicina 2023, 59, 1058. [Google Scholar] [CrossRef]
- Vintila, B.I.; Arseniu, A.M.; Butuca, A.; Sava, M.; Bîrluțiu, V.; Rus, L.L.; Axente, D.D.; Morgovan, C.; Gligor, F.G. Adverse Drug Reactions Relevant to Drug Resistance and Ineffectiveness Associated with Meropenem, Linezolid, and Colistin: An Analysis Based on Spontaneous Reports from the European Pharmacovigilance Database. Antibiotics 2023, 12, 918. [Google Scholar] [CrossRef]
- Hasegan, A.; Totan, M.; Antonescu, E.; Bumbu, A.G.; Pantis, C.; Furau, C.; Urducea, C.B.; Grigore, N. Prevalence of Urinary Tract Infections in Children and Changes in Sensitivity to Antibiotics of E. Coli Strains. Rev. Chim. 2019, 70, 3788–3792. [Google Scholar] [CrossRef]
- Boicean, A.; Bratu, D.; Bacila, C.; Tanasescu, C.; Fleacă, R.S.; Mohor, C.I.; Comaniciu, A.; Băluță, T.; Roman, M.D.; Chicea, R.; et al. Therapeutic Perspectives for Microbiota Transplantation in Digestive Diseases and Neoplasia—A Literature Review. Pathogens 2023, 12, 766. [Google Scholar] [CrossRef]
- Grigore, N.; Totan, M.; Pirvut, V.; Cernusca Mitariu, S.I.; Chicea, R.; Sava, M.; Hasegan, A. A Risk Assessment of Clostridium Difficile Infection after Antibiotherapy for Urinary Tract Infections in the Urology Department for Hospitalized Patients. Rev. Chim. 2017, 68, 1453–1456. [Google Scholar] [CrossRef]
- Mihai, I.; Boicean, A.; Teodoru, C.A.; Grigore, N.; Iancu, G.M.; Dura, H.; Bratu, D.G.; Roman, M.D.; Mohor, C.I.; Todor, S.B.; et al. Laparoscopic Adrenalectomy: Tailoring Approaches for the Optimal Resection of Adrenal Tumors. Diagnostics 2023, 13, 3351. [Google Scholar] [CrossRef]
- Popovici, R.F.; Alexa, I.F.; Novac, O.; Vrinceanu, N.; Popovici, E.; Lupusoru, C.E.; Voicu, V.A. Pharmacokinetics Study on Mesoporous Silica-Captopril. Dig. J. Nanomater. Biostruct. 2011, 6, 1619–1630. [Google Scholar]
- Gomelsky, A.; Steckenrider, H.; Dmochowski, R. Urgency and Urgency Incontinence Following Stress Urinary Incontinence Surgery: A Review of Evaluation and Management. Indian J. Urol. 2022, 38, 268. [Google Scholar] [CrossRef] [PubMed]
- Kenton, K.; Stoddard, A.M.; Zyczynski, H.; Albo, M.; Rickey, L.; Norton, P.; Wai, C.; Kraus, S.R.; Sirls, L.T.; Kusek, J.W.; et al. 5-Year Longitudinal Followup after Retropubic and Transobturator Mid Urethral Slings. J. Urol. 2015, 193, 203–210. [Google Scholar] [CrossRef]
- Gomelsky, A.; Dmochowski, R.R. Treatment of Mixed Urinary Incontinence. Cent. Eur. J. Urol. 2011, 64, 120–126. [Google Scholar] [CrossRef]
- Pergialiotis, V.; Mudiaga, Z.; Perrea, D.N.; Doumouchtsis, S.K. De Novo Overactive Bladder Following Midurethral Sling Procedures: A Systematic Review of the Literature and Meta-Analysis. Int. Urogynecol. J. 2017, 28, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Al-Zahrani, A.A.; Gajewski, J. Long-term Patient Satisfaction after Retropubic and Transobturator Mid-urethral Slings for Female Stress Urinary Incontinence. J. Obstet. Gynaecol. Res. 2016, 42, 1180–1185. [Google Scholar] [CrossRef] [PubMed]
- Morling, J.R.; McAllister, D.A.; Agur, W.; Fischbacher, C.M.; Glazener, C.M.A.; Guerrero, K.; Hopkins, L.; Wood, R. Adverse Events after First, Single, Mesh and Non-Mesh Surgical Procedures for Stress Urinary Incontinence and Pelvic Organ Prolapse in Scotland, 1997–2016: A Population-Based Cohort Study. Lancet 2017, 389, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Chughtai, B.; Barber, M.D.; Mao, J.; Forde, J.C.; Normand, S.-L.T.; Sedrakyan, A. Association between the Amount of Vaginal Mesh Used with Mesh Erosions and Repeated Surgery after Repairing Pelvic Organ Prolapse and Stress Urinary Incontinence. JAMA Surg. 2017, 152, 257. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, R.; Burkhard, F.C.; Tubaro, A. Re: Association between the Amount of Vaginal Mesh Used with Mesh Erosions and Repeated Surgery after Repairing Pelvic Organ Prolapse and Stress Urinary Incontinence. Eur. Urol. 2019, 75, 196–197. [Google Scholar] [CrossRef] [PubMed]
- Bach, F.; Hill, S.; Toozs-Hobson, P. The Effect of Body Mass Index on Retropubic Midurethral Slings. Am. J. Obstet. Gynecol. 2019, 220, 371.-e1–371.e9. [Google Scholar] [CrossRef]
- Tulokas, S.; Mentula, M.; Härkki, P.; Brummer, T.; Kuittinen, T.; Mikkola, T.; Rahkola-Soisalo, P. Effect of Hysterectomy on Re-Operation for Stress Urinary Incontinence: 10 Year Follow-Up. Arch. Gynecol. Obstet. 2022, 306, 2069–2075. [Google Scholar] [CrossRef] [PubMed]
- Aydın, S.; Arıoğlu Aydın, Ç. Effect of Concomitant Single Incision Vaginal Surgery on Mid Urethral Sling Success. Neurourol. Urodyn. 2016, 35, 995–999. [Google Scholar] [CrossRef]
- Shirvan, M.K.; Rahimi, H.R.; Darabi Mahboub, M.R.; Sheikhi, Z. Tension-Free Vaginal Tape versus Transobturator Tape for Treatment of Stress Urinary Incontinence: A Comparative Randomized Clinical Trial Study. Urol. Sci. 2014, 25, 54–57. [Google Scholar] [CrossRef]
- Offiah, I.; Freeman, R.; MONARCTM study group. Long-term Efficacy and Complications of a Multicentre Randomised Controlled Trial Comparing Retropubic and Transobturator Mid-urethral Slings: A Prospective Observational Study. BJOG 2021, 128, 2191–2199. [Google Scholar] [CrossRef]
- Kim, H.G.; Park, H.K.; Paick, S.H.; Choi, W.S. Comparison of Effectiveness between Tension-Free Vaginal Tape (TVT) and Trans-Obturator Tape (TOT) in Patients with Stress Urinary Incontinence and Intrinsic Sphincter Deficiency. PLoS ONE 2016, 11, e0156306. [Google Scholar] [CrossRef]
- Salo, H.; Sova, H.; Laru, J.; Talvensaari-Mattila, A.; Nyyssönen, V.; Santala, M.; Piltonen, T.; Koivurova, S.; Rossi, H.-R. Long-Term Results of a Prospective Randomized Trial Comparing Tension-Free Vaginal Tape versus Transobturator Tape in Stress Urinary Incontinence. Int. Urogynecol. J. 2023, 34, 2249–2256. [Google Scholar] [CrossRef]
- Teo, R.; Moran, P.; Mayne, C.; Tincello, D. Randomized Trial of Tension-Free Vaginal Tape and Tension-Free Vaginal Tape-Obturator for Urodynamic Stress Incontinence in Women. J. Urol. 2011, 185, 1350–1355. [Google Scholar] [CrossRef] [PubMed]
- Maruthappu, M.; Duclos, A.; Zhou, C.D.; Lipsitz, S.R.; Wright, J.; Orgill, D.; Carty, M.J. The Impact of Team Familiarity and Surgical Experience on Operative Efficiency: A Retrospective Analysis. J. R. Soc. Med. 2016, 109, 147–153. [Google Scholar] [CrossRef] [PubMed]


| Intraoperative Complications | TOT (353 p) | TVT (102 p) | p-Value |
|---|---|---|---|
| Overall complications | 7 (1.98%) | 9 (8.82%) | 0.0009 * |
| Bladder injury | 3 (0.84%) | 6 (5.88%) | 0.001 * |
| Vaginal injury | 4 (1.13%) | 0 | 0.953 |
| Retropubic hematoma | 0 | 3 (2.94%) | 0.011 * |
| History of Urogynecology Surgery | N | Bladder Injury | Vaginal Injury | Retropubic Hematoma | |||
|---|---|---|---|---|---|---|---|
| TVT N = 6 | TOT N = 3 | TVT N = 0 | TOT N = 4 | TVT N = 3 | TOT N = 0 | ||
| Hysterectomy | 101 | 3 (2.94%) | 0 | 0 | 0 | 2 (1.96%) | 0 |
| Anterior colporrhaphy | 32 | 0 | 0 | 0 | 4 (1.13%) | 1 (0.98%) | 0 |
| Posterior colporrhapy | 22 | 0 | 0 | 0 | 0 | 0 | 0 |
| Burch procedure | 11 | 0 | 3 (0.84%) | 0 | 0 | 0 | 0 |
| No history | 289 | 3 (2.94%) | 0 | 0 | 0 | 0 | 0 |
| Variable | TOT (n = 7) | TVT (n = 9) | p-Value |
|---|---|---|---|
| Age (years) | 66 (64–67.5) | 67 (66–69) | 0.368 |
| Obesity | 2 (28%) | 8 (88%) | 0.013 * |
| Clinical History | |||
| Hysterectomy | 0 | 4 (44%) | 0.307 |
| Anterior Colporraphy | 4 (57%) | 2 (22%) | 0.157 |
| Burch Procedure | 3 (42%) | 0 | 0.072 |
| No history | 0 | 3(33%) | 0.401 |
| Variable | TVT (102 p) | TOT (353 p) | p-Value |
|---|---|---|---|
| Immediate postoperative complications | |||
| Overall | 18 (17.64%) | 5 (1.41%) | <0.001 * |
| Acute retention of urine | 14 (13.72%) | 5 (1.41%) | <0.001 * |
| Febrile syndrome | 1 (0.98%) | 0 (0%) | 0.968 |
| Urinary tract infection | 3 (2.95%) | 0 (0%) | 0.687 |
| Late postoperative complications | |||
| Overall | 13 (12.74%) | 20 (5.66%) | 0.0001 * |
| Vaginal erosion | 2 (1.96%) | 4 (1.13%) | 0.618 |
| Recurrence of incontinence | 0 (0%) | 13 (3.7%) | 0.047 * |
| De novo urgency | 6 (5.88%) | 1 (0.28%) | 0.0006 * |
| Chronic retention of urine | 5 (4.90%) | 2 (0.57%) | 0.0002 * |
| Variable | TVT | TOT | p-Value |
|---|---|---|---|
| Preoperative symptom | |||
| Urgency | 3 (2.9%) | 48 (13.5%) | 0.002 * |
| Pelvic pain | 6 (5.8%) | 91 (25.6%) | 0.0001 * |
| Dispareunia | 7 (6.8%) | 37 (10.4%) | 0.282 |
| Postoperative symptom alleviation | |||
| Incontinence | 102 (100%) | 340 (96.3%) | 0.047 * |
| Urgency | 2 (66%) | 36 (75%) | 0.103 |
| Pelvic pain | 5 (83.3%) | 81(89.01%) | 0.180 |
| Dispareunia | 5 (71.42%) | 33 (89.18%) | 0.209 |
| Variable | Univariable Logistic Regression | Multivariable Logistic Regression | ||||||
|---|---|---|---|---|---|---|---|---|
| Odd Ratio | p Value | CI of 95% | Odd Ratio | p-Value | CI of 95% | |||
| Hysterectomy | 1.895 | 0.785 | 0.456 | 3.124 | 1.452 | 0.825 | 0.402 | 3.125 |
| Burch procedure | 8.856 | 0.072 | 0.986 | 34.123 | 6.145 | 0.096 | 0.953 | 28.124 |
| Age | 1.122 | 0.132 | 0.913 | 1.225 | 1.023 | 0.175 | 0.894 | 1.329 |
| Obesity * | 1.862 | 0.002 * | 1.356 | 2.102 | 1.125 | 0.037 * | 1.105 | 1.533 |
| Anterior colporrhaphy | 7.758 | 0.096 | 0.975 | 31.125 | 5.566 | 0.102 | 0.932 | 25.223 |
| Posterior colporrhaphy | 0.356 | 0.956 | 0.015 | 0.452 | 0.326 | 0.988 | 0.014 | 0.325 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hașegan, A.; Mihai, I.; Teodoru, C.A.; Matacuta, I.B.; Dura, H.; Todor, S.B.; Ichim, C.; Tanasescu, D.; Grigore, N.; Bolca, C.N.; et al. Exploring the Challenges of Using Minimal Invasive Surgery to Treat Stress Urinary Incontinence: Insights from a Retrospective Case-Control Study. Diagnostics 2024, 14, 323. https://doi.org/10.3390/diagnostics14030323
Hașegan A, Mihai I, Teodoru CA, Matacuta IB, Dura H, Todor SB, Ichim C, Tanasescu D, Grigore N, Bolca CN, et al. Exploring the Challenges of Using Minimal Invasive Surgery to Treat Stress Urinary Incontinence: Insights from a Retrospective Case-Control Study. Diagnostics. 2024; 14(3):323. https://doi.org/10.3390/diagnostics14030323
Chicago/Turabian StyleHașegan, Adrian, Ionela Mihai, Cosmin Adrian Teodoru, Ioana Bogdan Matacuta, Horațiu Dura, Samuel Bogdan Todor, Cristian Ichim, Denisa Tanasescu, Nicolae Grigore, Ciprian Nicolae Bolca, and et al. 2024. "Exploring the Challenges of Using Minimal Invasive Surgery to Treat Stress Urinary Incontinence: Insights from a Retrospective Case-Control Study" Diagnostics 14, no. 3: 323. https://doi.org/10.3390/diagnostics14030323
APA StyleHașegan, A., Mihai, I., Teodoru, C. A., Matacuta, I. B., Dura, H., Todor, S. B., Ichim, C., Tanasescu, D., Grigore, N., Bolca, C. N., Mohor, C. I., Mohor, C. I., Bacalbașa, N., Bratu, D. G., & Boicean, A. (2024). Exploring the Challenges of Using Minimal Invasive Surgery to Treat Stress Urinary Incontinence: Insights from a Retrospective Case-Control Study. Diagnostics, 14(3), 323. https://doi.org/10.3390/diagnostics14030323







