Assessing the Impact of Prolonged Averaging of Coronary Continuous Thermodilution Traces
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Coronary Angiography
2.3. Continuous Thermodilution Measurements
2.4. Analysis of Traces
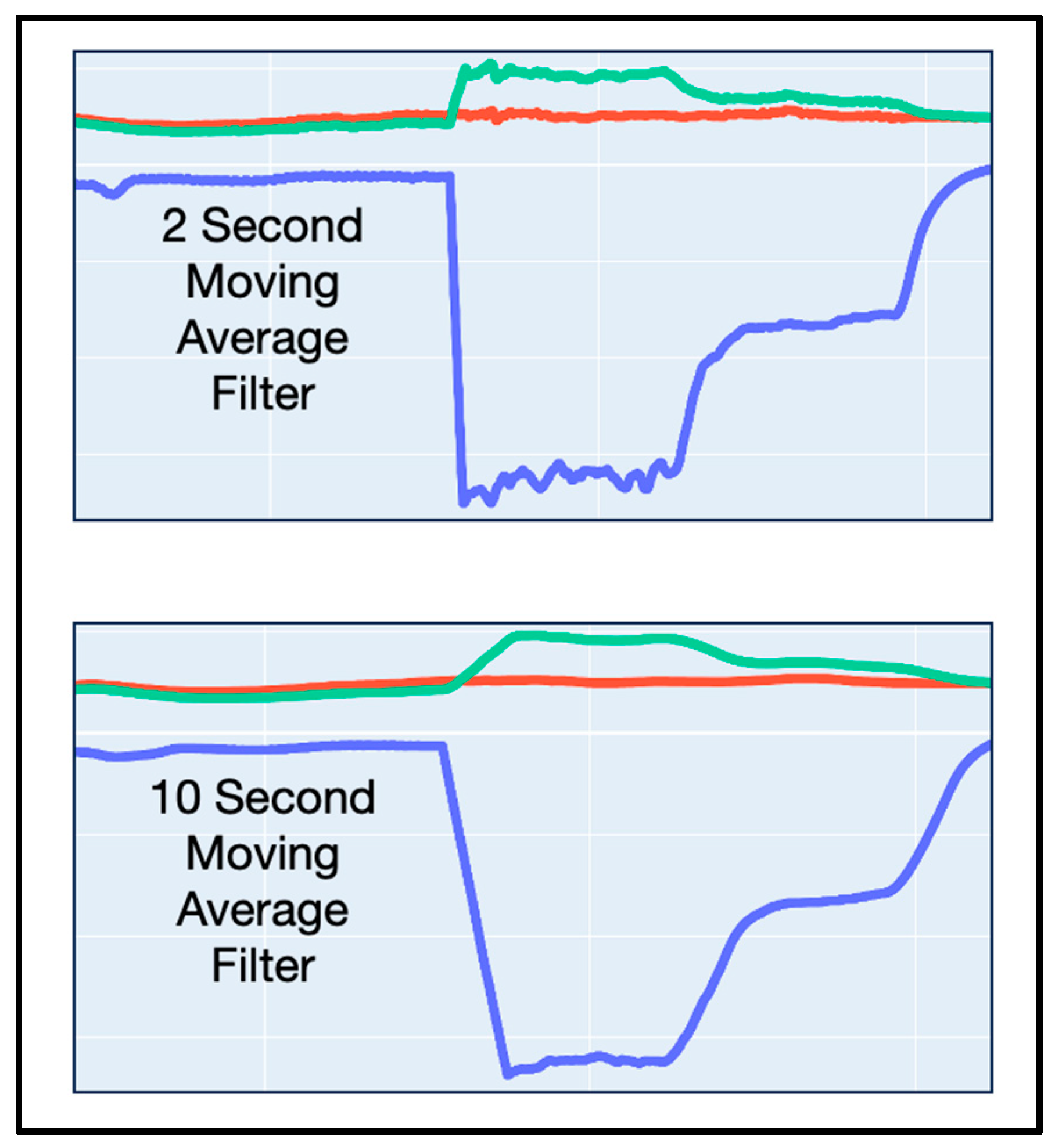
2.5. Definition of a Moving Average Filter
2.6. Calculation of Absolute Flow (Q)
2.7. Determination of Maximum Length of Average
2.8. Statistical Analysis
3. Results
3.1. Baseline and Procedural Data
3.2. Determination of Maximum Acceptable Average
3.3. Re-Analysis with a 10 s Moving Average Filter
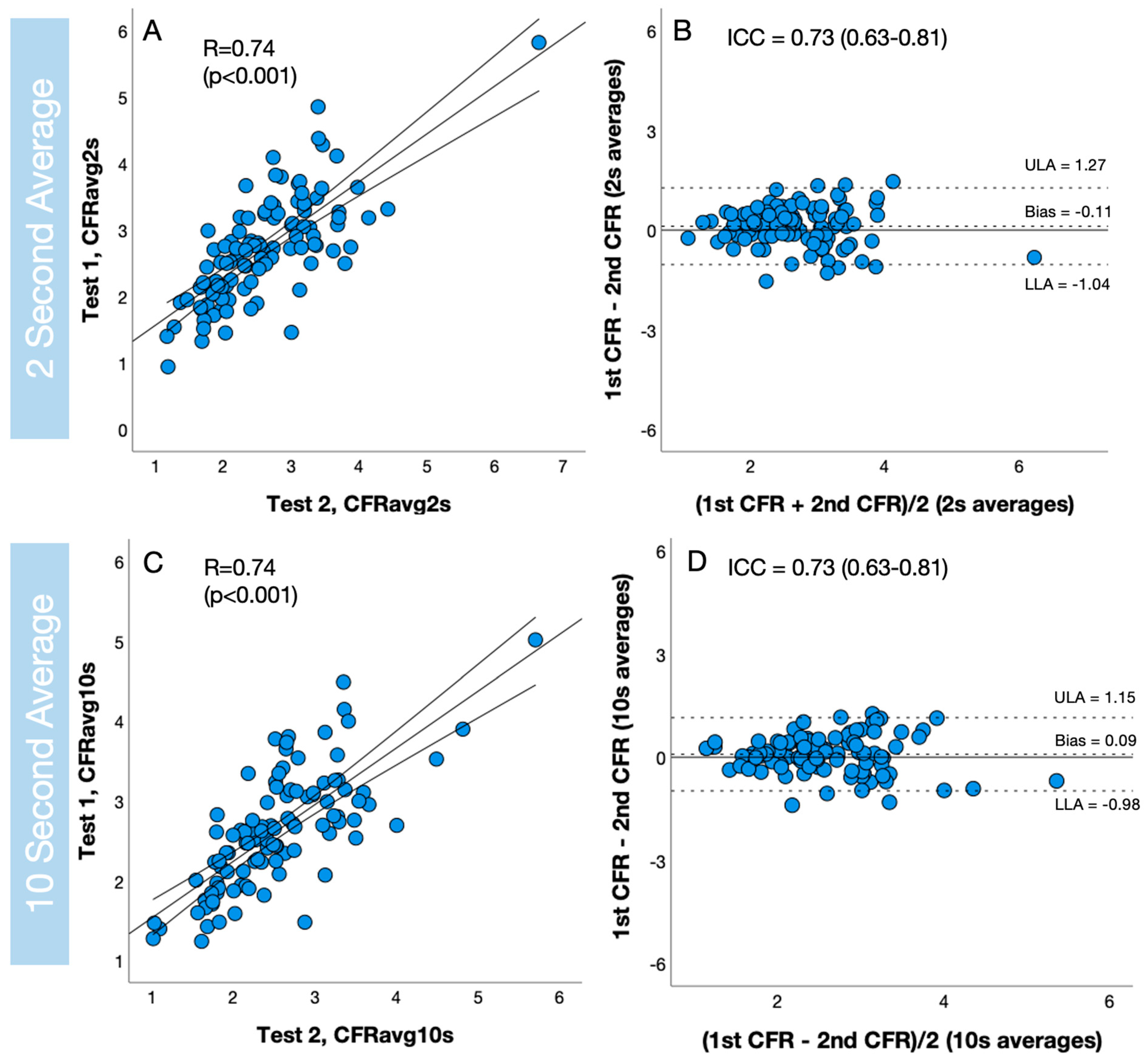
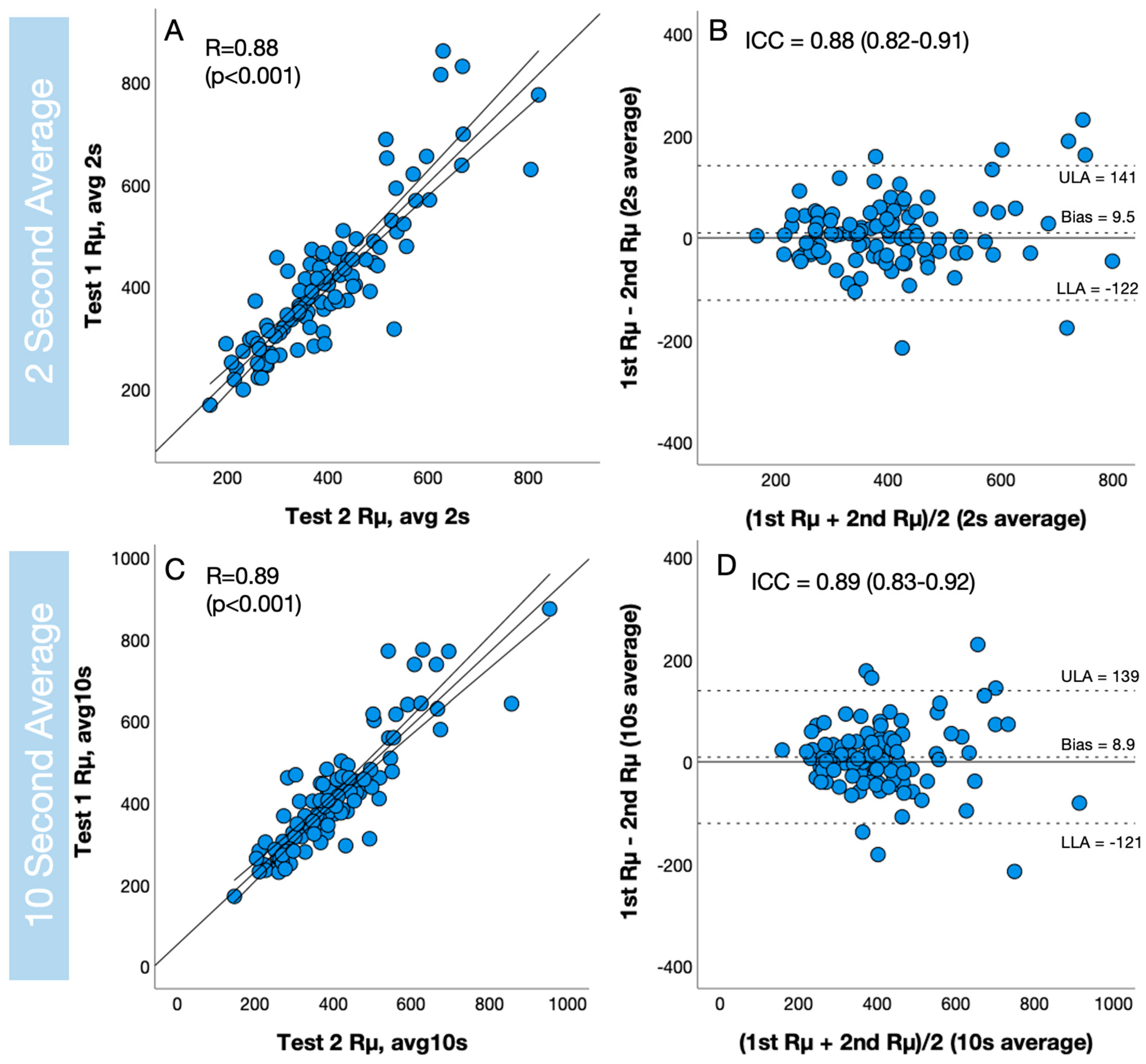
3.4. Assessment of Reproducibility
4. Discussion
4.1. Summary of Results
4.2. Reproducibility
4.3. Loss of Fidelity with 10 s Moving Average
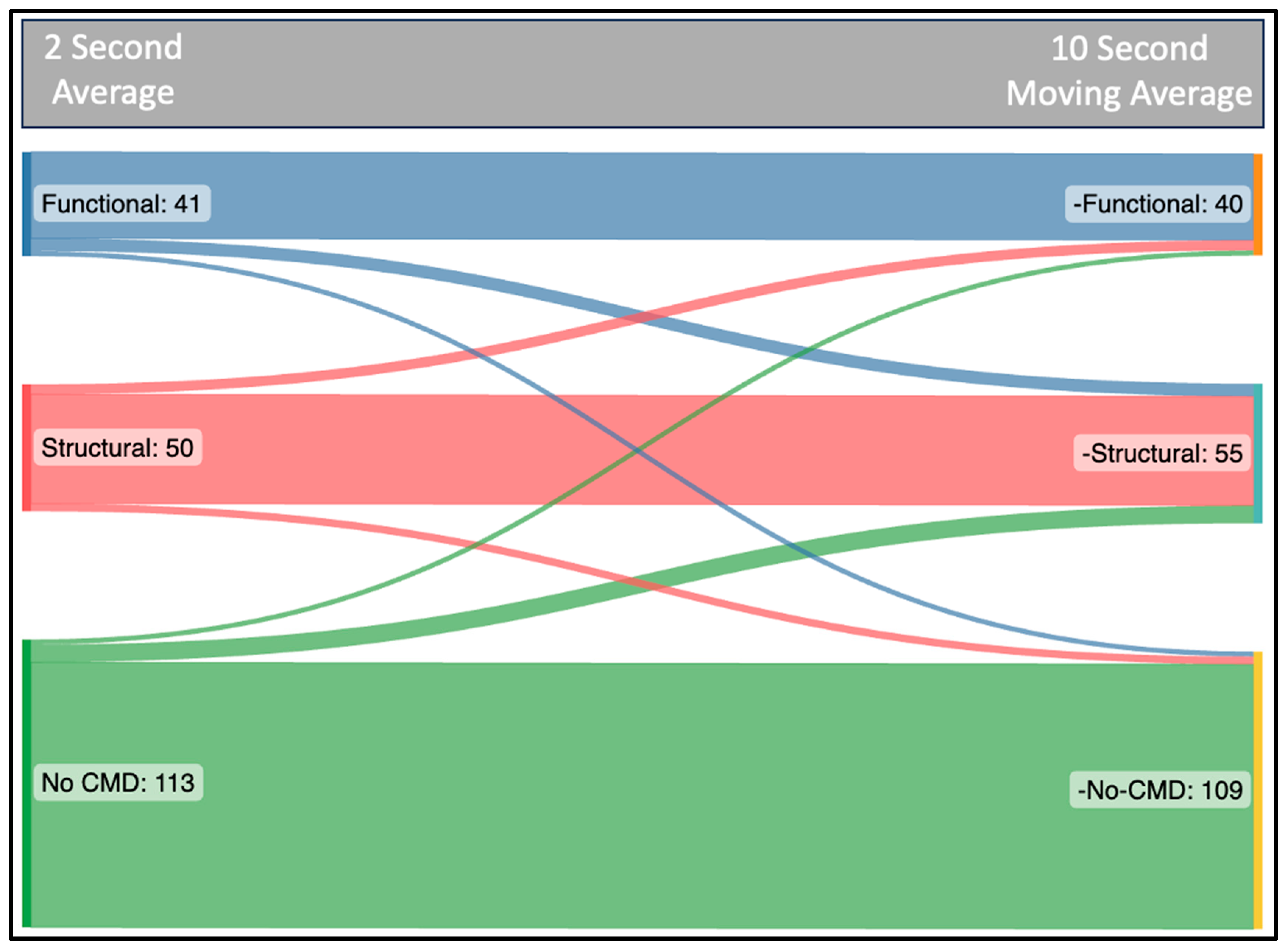
4.4. Diagnostic Mismatch
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANOCA | Angina with Non-Obstructive Coronary Artery Disease |
| CFR | Coronary Flow Reserve |
| CMD | Coronary Microvascular Dysfunction |
| FFR | Fractional Flow Reserve |
| MRR | Microvascular Resistance Reserve |
| Pa | Aortic pressure |
| Pa,rest | Aortic pressure at rest (mmHg) |
| Pa,hyper | Aortic pressure at maximum coronary hyperemia (mmHg) |
| Pd | Distal coronary pressure |
| Pd,rest | Distal coronary pressure at rest (mmHg) |
| Pd,hyper | Distal coronary pressure at maximum coronary hyperemia (mmHg) |
| PET | Positron Emission Tomography |
| Q | Absolute Coronary Flow (mL/min) |
| Qrest | Absolute Coronary Flow at rest (mL/min) |
| Qhyper | Absolute Coronary Flow during hyperemia (mL/min) |
| Qi | Saline Infusion Rate |
| Rµ,hyper | Hyperemic Microvascular Resistance |
| WU | Woods Units |
| T | Distal Coronary Mixed Temperature |
| Ti | Difference between blood temperature and the temperature of saline at the exit of the infusion catheter (°C) |
References
- Ford, T.J.; Stanley, B.; Good, R.; Rocchiccioli, P.; McEntegart, M.; Watkins, S.; Eteiba, H.; Shaukat, A.; Lindsay, M.; Robertson, K.; et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina: The CorMicA Trial. J. Am. Coll. Cardiol. 2018, 72, 2841–2855. [Google Scholar] [CrossRef] [PubMed]
- Sinha, A.; Rahman, H.; Douiri, A.; Demir, O.M.; De Silva, K.; Clapp, B.; Webb, I.; Gulati, A.; Pinho, P.; Dutta, U.; et al. ChaMP-CMD: A Phenotype-Blinded, Randomized Controlled, Cross-Over Trial. Circulation 2023, 149, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Kelshiker, M.A.; Seligman, H.; Howard, J.P.; Rahman, H.; Foley, M.; Nowbar, A.N.; Rajkumar, C.A.; Shun-Shin, M.J.; Ahmad, Y.; Sen, S.; et al. Coronary flow reserve and cardiovascular outcomes: A systematic review and meta-analysis. Eur. Heart J. 2022, 43, 1582–1593. [Google Scholar] [CrossRef]
- Fawaz, S.; Khan, S.; Simpson, R.; Clesham, G.; Cook, C.M.; Davies, J.R.; Karamasis, G.; Keeble, T.R. Invasive Detection of Coronary Microvascular Dysfunction: How It Began, and Where We Are Now. Interv. Cardiol. Rev. 2023, 18, e07. [Google Scholar] [CrossRef] [PubMed]
- Vanyi, J.; Bowers, T.; Jarvis, G.; White, C.W. Can an intracoronary doppler wire accurately measure changes in coronary blood flow velocity? Catheter. Cardiovasc. Diagn. 1993, 29, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Doucette, J.W.; Corl, P.D.; Payne, H.M.; Flynn, A.E.; Goto, M.; Nassi, M.; Segal, J. Validation of a Doppler guide wire for intravascular measurement of coronary artery flow velocity. Circulation 1992, 85, 1899–1911. [Google Scholar] [CrossRef] [PubMed]
- De Bruyne, B.; Pijls, N.H.; Smith, L.; Wievegg, M.; Heyndrickx, G.R. Coronary thermodilution to assess flow reserve: Experimental validation. Circulation 2001, 104, 2003–2006. [Google Scholar] [CrossRef] [PubMed]
- Pijls, N.H.; De Bruyne, B.; Smith, L.; Aarnoudse, W.; Barbato, E.; Bartunek, J.; Bech, G.J.W.; Van De Vosse, F. Coronary thermodilution to assess flow reserve: Validation in humans. Circulation 2002, 105, 2482–2486. [Google Scholar] [CrossRef]
- Gutiérrez-Barrios, A.; Izaga-Torralba, E.; Crespo, F.R.; Gheorghe, L.; Cañadas-Pruaño, D.; Gómez-Lara, J.; Silva, E.; Noval-Morillas, I.; Rueda, R.Z.; Calle-Pérez, G.; et al. Continuous Thermodilution Method to Assess Coronary Flow Reserve. Am. J. Cardiol. 2021, 141, 31–37. [Google Scholar] [CrossRef]
- Aarnoudse, W.; Veer, M.V.; Pijls, N.H.; ter Woorst, J.; Vercauteren, S.; Tonino, P.; Geven, M.; Rutten, M.; van Hagen, E.; de Bruyne, B.; et al. Direct Volumetric Blood Flow Measurement in Coronary Arteries by Thermodilution. J. Am. Coll. Cardiol. 2007, 50, 2294–2304. [Google Scholar] [CrossRef]
- Scarsini, R.; Shanmuganathan, M.; Kotronias, R.A.; Terentes-Printzios, D.; Borlotti, A.; Langrish, J.P.; Lucking, A.J.; OxAMI Study Investigators; Ribichini, F.; Ferreira, V.M.; et al. Angiography-derived index of microcirculatory resistance (IMR angio) as a novel pressure-wire-free tool to assess coronary microvascular dysfunction in acute coronary syndromes and stable coronary artery disease. Int. J. Cardiovasc. Imaging 2021, 37, 1801–1813. [Google Scholar] [CrossRef]
- Askin, L.; Tanriverdi, O.; Gul, E. Functional Evaluation of Coronary Stenosis: Is Quantitative Flow Ratio a Step Forward? Cor et Vasa 2022, 64, 300–304. [Google Scholar] [CrossRef]
- Tebaldi, M.; Biscaglia, S.; Di Girolamo, D.; Erriquez, A.; Penzo, C.; Tumscitz, C.; Campo, G. Angio-based index of microcirculatory resistance for the assessment of the coronary resistance: A proof of concept study. J. Interv. Cardiol. 2020, 2020, 8887369. [Google Scholar] [CrossRef]
- Demir, O.M.; Boerhout, C.K.M.; de Waard, G.A.; van de Hoef, T.P.; Patel, N.; Beijk, M.A.; Williams, R.; Rahman, H.; Everaars, H.; Kharbanda, R.K.; et al. Comparison of Doppler Flow Velocity and Thermodilution Derived Indexes of Coronary Physiology. JACC Cardiovasc. Interv. 2022, 15, 1060–1070. [Google Scholar] [CrossRef]
- Gallinoro, E.; Bertolone, D.T.; Fernandez-Peregrina, E.; Paolisso, P.; Bermpeis, K.; Esposito, G.; Gomez-Lopez, A.; Candreva, A.; Mileva, N.; Belmonte, M.; et al. Reproducibility of bolus versus continuous thermodilution for assessment of coronary microvascular function in patients with ANOCA. EuroIntervention 2023, 19, e155–e166. [Google Scholar] [CrossRef] [PubMed]
- Everaars, H.; de Waard, G.A.; Driessen, R.S.; Danad, I.; van de Ven, P.M.; Raijmakers, P.G.; Lammertsma, A.A.; van Rossum, A.C.; Knaapen, P.; van Royen, N. Doppler Flow Velocity and Thermodilution to Assess Coronary Flow Reserve: A Head-to-Head Comparison With [15O]H2O PET. JACC Cardiovasc. Interv. 2018, 11, 2044–2054. [Google Scholar] [CrossRef]
- Everaars, H.; De Waard, G.A.; Schumacher, S.P.; Zimmermann, F.M.; Bom, M.J.; Van De Ven, P.M.; Raijmakers, P.G.; Lammertsma, A.A.; Götte, M.J.; Van Rossum, A.C.; et al. Continuous thermodilution to assess absolute flow and microvascular resistance: Validation in humans using [15O]H2O positron emission tomography. Eur. Heart J. 2019, 40, 2350–2359. [Google Scholar] [CrossRef] [PubMed]
- Candreva, A.; Gallinoro, E.; van’t Veer, M.; Sonck, J.; Collet, C.; Di Gioia, G.; Kodeboina, M.; Mizukami, T.; Nagumo, S.; Keulards, D.; et al. Basics of Coronary Thermodilution. JACC Cardiovasc. Interv. 2021, 14, 595–605. [Google Scholar] [CrossRef]
- Keulards, D.C.; Veer, M.V.T.; Zelis, J.M.; el Farissi, M.; Zimmermann, F.M.; de Vos, A.; Teeuwen, K.; Brueren, G.R.; Wijnbergen, I.F.; Vlaar, P.-J.; et al. Safety of absolute coronary flow and microvascular resistance measurements by thermodilution. EuroIntervention 2021, 17, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Xaplanteris, P.; Fournier, S.; Keulards, D.C.J.; Adjedj, J.; Ciccarelli, G.; Milkas, A.; Pellicano, M.; Van’t Veer, M.; Barbato, E.; Pijls, N.H.; et al. Catheter-Based Measurements of Absolute Coronary Blood Flow and Microvascular Resistance: Feasibility, Safety, and Reproducibility in Humans. Circ. Cardiovasc. Interv. 2018, 11, e006194. [Google Scholar] [CrossRef] [PubMed]
- De Bruyne, B.; Pijls, N.H.J.; Gallinoro, E.; Candreva, A.; Fournier, S.; Keulards, D.C.; Sonck, J.; Veer, M.V.; Barbato, E.; Bartunek, J.; et al. Microvascular Resistance Reserve for Assessment of Coronary Microvascular Function. J. Am. Coll. Cardiol. 2021, 78, 1541–1549. [Google Scholar] [CrossRef] [PubMed]
- Candreva, A.; Gallinoro, E.; Peregrina, E.F.; Sonck, J.; Keulards, D.C.J.; Veer, M.V.; Mizukami, T.; Pijls, N.H.J.; Collet, C.; De Bruyne, B. Automation of intracoronary continuous thermodilution for absolute coronary flow and microvascular resistance measurements. Catheter. Cardiovasc. Interv. 2022, 100, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Van’t Veer, M.; Adjedj, J.; Wijnbergen, I.; Tóth, G.G.; Rutten, M.C.; Barbato, E.; van Nunen, L.X.; Pijls, N.H.; De Bruyne, B. Novel monorail infusion catheter for volumetric coronary blood flow measurement in humans: In vitro validation. EuroIntervention 2016, 12, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Gallinoro, E.; Candreva, A.; Colaiori, I.; Kodeboina, M.; Fournier, S.; Nelis, O.; Di Gioia, G.; Sonck, J.; Van’t Veer, M.; Pijls, N.H.; et al. Thermodilution-derived volumetric resting coronary blood flow measurement in humans. EuroIntervention 2021, 17, E672–E679. [Google Scholar] [CrossRef]

| 2 s Average (Reference) Mean ± SD | 10 s Average | 15 s Average | 20 s Average | |
|---|---|---|---|---|
| Mean Bias (95% CI) | Mean Bias (95% CI) | Mean Bias (95% CI) | ||
| Qrest | 82 ± 30 mL/min | −1.02 (−1.66–−0.39) | −1.76 (−2.52–−1.00) | −2.71 (−3.59–−1.84) |
| Qhyper | 211 ± 77 mL/min | 2.71 (0.91–4.51) | 4.03 (1.80–6.26) | 6.13 (3.04–9.23) |
| Rµ,hyper | 403 ± 135 WU | −4.86 (−7.86–−1.87) | −6.56 (−10.63–−2.5) | −11.3 (−17.18–−5.08) |
| CFR | 2.67 ± 0.81 | 0.07 (0.05–0.10) | 0.12 (0.08–0.15) | 0.17 (0.13–0.21) |
| MRR | 3.24 ± 0.96 | 0.10 (0.06–0.13) | 0.13 (0.09–0.17) | 0.20 (0.15–0.25) |
| Accuracy (%) | ||||
| CFR (<2.5) | 90% | 87% | 84% | |
| Rµ,hyper (>400) | 95% | 92% | 90% | |
| 2 s Average | 10 s Moving Average Filter | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Test 1 | Test 2 | R (95% CI) | ICC (95% CI) | Var (%) | Test 1 | Test 2 | R (95% CI) | ICC (95% CI) | Var (%) | |
| CFR | 2.73 ± 0.80 | 2.61 ± 0.82 | 0.74 (0.63–0.81) | 0.73 (0.62–0.81) | 17.8 ± 12.4 | 2.62 ± 0.73 | 2.54 ± 0.76 | 0.74 (0.63–0.81) | 0.73 (0.63–0.81) | 16.2 ± 12.1 |
| MRR | 3.27 ± 0.95 | 3.22 ± 0.97 | 0.72 (0.61–0.80) | 0.72 (0.61–0.80) | 16.5 ± 12.4 | 3.16 ± 0.89 | 3.11 ± 0.91 | 0.73 (0.63–0.81) | 0.73 (0.63–0.81) | 16.2 ± 11.8 |
| Rµ,hyper | 408 ± 142 | 398 ± 129 | 0.88 (0.83–0.92) | 0.88 (0.82–0.91) | 11.9 ± 9.9 | 412 ± 139 | 403 ± 137 | 0.89 (0.83–0.92) | 0.89 (0.83–0.92) | 11.4 ± 10 |
| Qrest | 79 ± 28 | 86 ± 32 | 0.73 (0.62–0.81) | 0.70 (0.57–0.79) | 20.3 ± 16.0 | 80 ± 28 | 88 ± 34 | 0.77 (0.76–0.84) | 0.73 (0.59–0.82) | 20 ± 14.8 |
| Qhyper | 207 ± 73 | 216 ± 81 | 0.87 (0.81–0.91) | 0.86 (0.80–0.90) | 12.5 ± 11.1 | 202 ± 67 | 215 ± 81 | 0.89 (0.84–0.92) | 0.86 (0.79–0.91) | 13 ± 11.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fawaz, S.; Munhoz, D.; Mahendiran, T.; Gallinoro, E.; Mizukami, T.; Khan, S.A.; Simpson, R.F.G.; Svanerud, J.; Cook, C.M.; Davies, J.R.; et al. Assessing the Impact of Prolonged Averaging of Coronary Continuous Thermodilution Traces. Diagnostics 2024, 14, 285. https://doi.org/10.3390/diagnostics14030285
Fawaz S, Munhoz D, Mahendiran T, Gallinoro E, Mizukami T, Khan SA, Simpson RFG, Svanerud J, Cook CM, Davies JR, et al. Assessing the Impact of Prolonged Averaging of Coronary Continuous Thermodilution Traces. Diagnostics. 2024; 14(3):285. https://doi.org/10.3390/diagnostics14030285
Chicago/Turabian StyleFawaz, Samer, Daniel Munhoz, Thabo Mahendiran, Emanuele Gallinoro, Takuya Mizukami, Sarosh A. Khan, Rupert F. G. Simpson, Johan Svanerud, Christopher M. Cook, John R. Davies, and et al. 2024. "Assessing the Impact of Prolonged Averaging of Coronary Continuous Thermodilution Traces" Diagnostics 14, no. 3: 285. https://doi.org/10.3390/diagnostics14030285
APA StyleFawaz, S., Munhoz, D., Mahendiran, T., Gallinoro, E., Mizukami, T., Khan, S. A., Simpson, R. F. G., Svanerud, J., Cook, C. M., Davies, J. R., Karamasis, G. V., De Bruyne, B., & Keeble, T. R. (2024). Assessing the Impact of Prolonged Averaging of Coronary Continuous Thermodilution Traces. Diagnostics, 14(3), 285. https://doi.org/10.3390/diagnostics14030285






