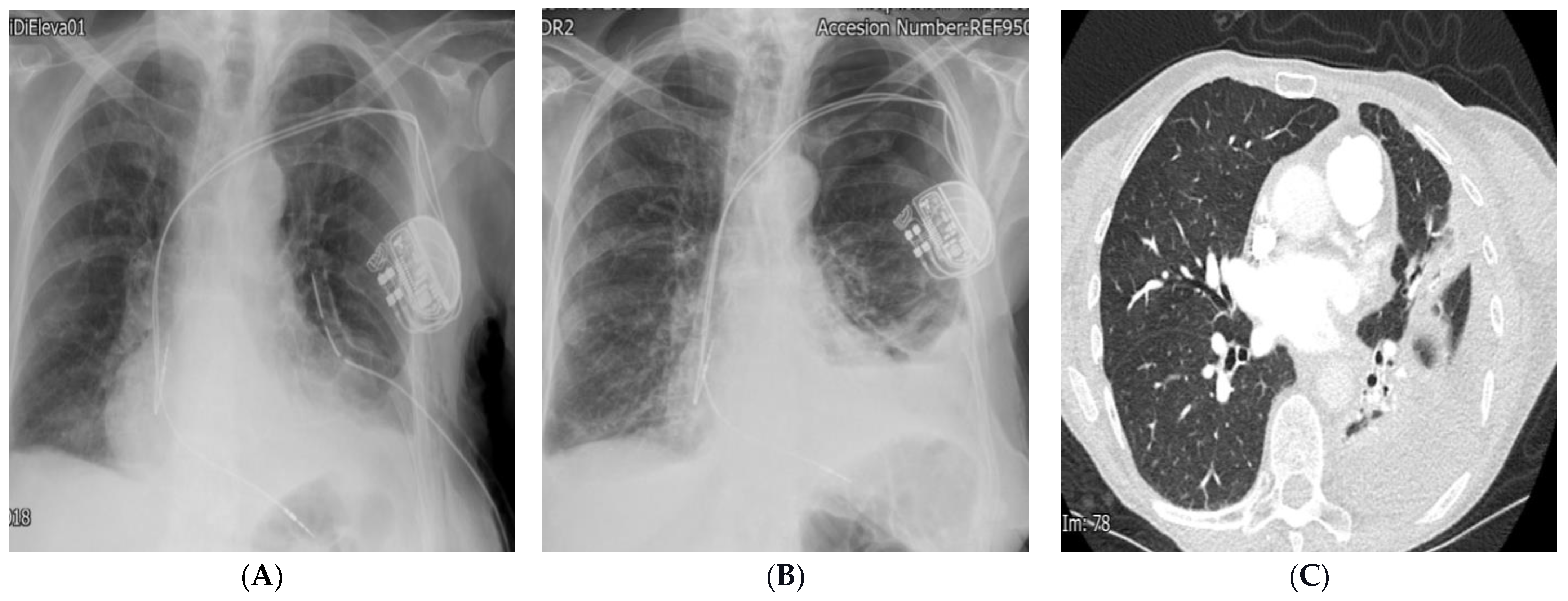
Dual Chamber Pacemaker Implant in Coronary Sinus Leading to Several Complications
Abstract
- Learning Points
- Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carrión-Camacho, M.R.; Marín-León, I.; Molina-Doñoro, J.M.; González-López, J.R. Safety of Permanent Pacemaker Implantation: A Prospective Study. J. Clin. Med. 2019, 8, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muthumala, A.; Herring, N.; Wong, K. A case of difficult RV lead placement. Heart 2013, 100, 434–435. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, A.; Farmer, D.M.; Homoud, M. Pacemaker Interrogation and Programming. In Cardiology Procedures; Hendel, R.C., Kimmelstiel, C., Eds.; Springer: Cham, Switzerland, 2013. [Google Scholar] [CrossRef]
- Squara, F.; Scarlatti, D.; Riccini, P.; Garret, G.; Moceri, P.; Ferrari, E. Individualized Left Anterior Oblique Projection. A Highly Reliable Patient-Tailored Fluoroscopy Criterion for Right Ventricular Lead Positioning. Circ. Arrhythmia Electrophysiol. 2018, 11, e006107. [Google Scholar] [CrossRef] [PubMed]
- Mathew, R.P.; Alexander, T.; Patel, V.; Low, G. Chest radiographs of cardiac devices (Part 1): Cardiovascular implantable electronic devices, cardiac valve prostheses and Amplatzer occluder devices. SA J. Radiol. 2019, 23, 1730, Erratum in SA J. Radiol. 2021, 25, 2256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wassef, N.; Ibrahim, M.; Botrous, C.; Anos, A.; Hogrefe, K.; Pathiraja, J. Dual Chamber Pacemaker Implant in Coronary Sinus Leading to Several Complications. Diagnostics 2024, 14, 2465. https://doi.org/10.3390/diagnostics14222465
Wassef N, Ibrahim M, Botrous C, Anos A, Hogrefe K, Pathiraja J. Dual Chamber Pacemaker Implant in Coronary Sinus Leading to Several Complications. Diagnostics. 2024; 14(22):2465. https://doi.org/10.3390/diagnostics14222465
Chicago/Turabian StyleWassef, Nancy, Mina Ibrahim, Christine Botrous, Amr Anos, Kai Hogrefe, and Janaka Pathiraja. 2024. "Dual Chamber Pacemaker Implant in Coronary Sinus Leading to Several Complications" Diagnostics 14, no. 22: 2465. https://doi.org/10.3390/diagnostics14222465
APA StyleWassef, N., Ibrahim, M., Botrous, C., Anos, A., Hogrefe, K., & Pathiraja, J. (2024). Dual Chamber Pacemaker Implant in Coronary Sinus Leading to Several Complications. Diagnostics, 14(22), 2465. https://doi.org/10.3390/diagnostics14222465




