Development of a Short-Form Hwa-Byung Symptom Scale Using Machine Learning Approaches
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Statistical Analysis and Machine Learning Algorithms
2.3.1. Data Preprocessing
2.3.2. Item Grouping with EFA
2.3.3. Model Development and Evaluation
2.3.4. Performance Measures
2.4. Software and Tools
2.5. Ethical Considerations
3. Results
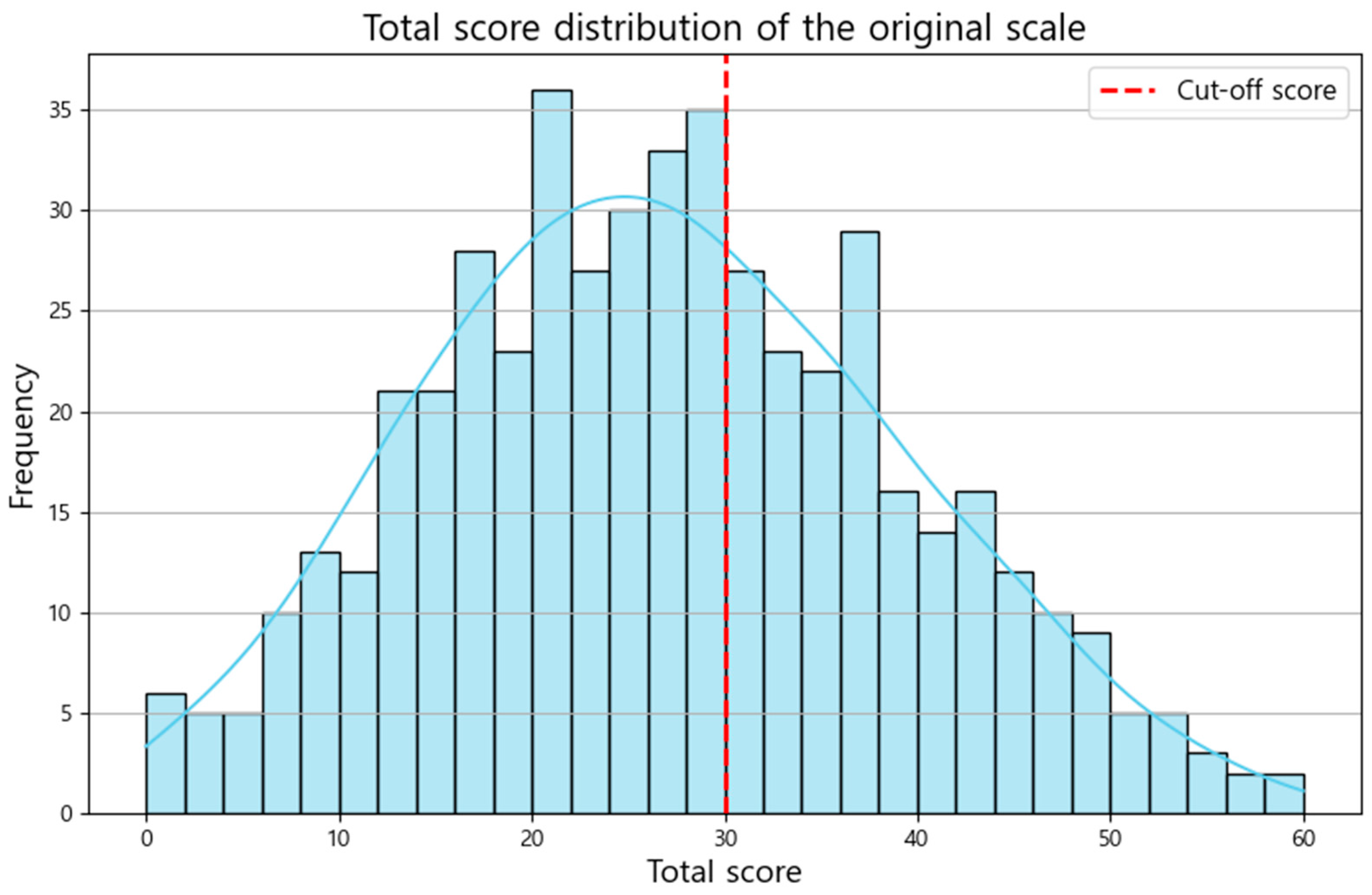
3.1. Data Description
3.2. HB Symptom Scale Items Grouped by Factor Composition
3.3. Prediction of the Presence of HB
4. Discussion
4.1. Findings of This Study
4.2. Interpretation of the Findings
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kwon, C.Y.; Chung, S.Y.; Kim, J.W. Hwabyung: A Mental Disorder Related to Suppressed Emotions and Somatic Symptoms Reminiscent of Being on Fire. Psychosom. Med. 2020, 82, 529–531. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Wachholtz, A.; Choi, K.H. A Review of the Korean Cultural Syndrome Hwa-Byung: Suggestions for Theory and Intervention. Asia Taepyongyang Sangdam Yongu 2014, 4, 49. [Google Scholar] [CrossRef] [PubMed]
- Suh, H.W.; Lee, K.B.; Chung, S.Y.; Park, M.; Jang, B.H.; Kim, J.W. How Suppressed Anger Can Become an Illness: A Qualitative Systematic Review of the Experiences and Perspectives of Hwabyung Patients in Korea. Front. Psychiatry 2021, 12, 637029. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-G.; Lee, J.-H. Study on the Prevalence of Hwa-Byung Diagnosed by HBDIS in General Population in Kang-won Province. J. Orient. Neuropsychiatry 2008, 19, 133–140. [Google Scholar]
- Kwon, J.-H.; Park, D.-G.; Kim, J.-W.; Lee, M.-S.; Min, S.-G.; Kwon, H.-I. Development and validation of the Hwa-Byung Scale. Korean J. Clin. Psychol. 2008, 27, 237–252. [Google Scholar] [CrossRef]
- Min, S.K. Clinical correlates of hwa-byung and a proposal for a new anger disorder. Psychiatry Investig. 2008, 5, 125–141. [Google Scholar] [CrossRef][Green Version]
- The Korean Society of Oriental Neuropsychiatry. Clinical Practice Guideline of Korean Medicine of Hwabyung; National Institute for Korean Medicine Development: Seoul, Republic of Korea, 2021. [Google Scholar]
- Min, S.K.; Suh, S.Y.; Song, K.J. Symptoms to use for diagnostic criteria of hwa-byung, an anger syndrome. Psychiatry Investig. 2009, 6, 7–12. [Google Scholar] [CrossRef]
- Chung, S.-Y.; Park, Y.-J.; Kim, J.-W.; Park, Y.-B. Validation of the Hwa-Byung Scale and its relationship with cardiovascular autonomic function. Eur. J. Integr. Med. 2015, 7, 409–416. [Google Scholar] [CrossRef]
- Kim, N.-S.; Lee, K.-E. Gender differences in factors affecting Hwa-byung symptoms with middle-age people. J. Korean Acad. Fundam. Nurs. 2012, 19, 98–108. [Google Scholar] [CrossRef][Green Version]
- Min, S.K.; Suh, S.Y. The anger syndrome hwa-byung and its comorbidity. J. Affect. Disord. 2010, 124, 211–214. [Google Scholar] [CrossRef]
- Hur, Y.M.; Jin, H.J.; Lee, S.; Kim, J.W. Shared Genetic Etiology of Hwabyung (Anger Syndrome) and Somatization Symptoms in South Korean Adolescent and Young Adult Twins. Twin Res. Hum. Genet. 2019, 22, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Hur, Y.M.; Choi, E.J.; Kim, J.W.; Jin, H.J.; Lee, S. Heritability of Hwabyung Symptoms in South Korean Adolescent and Young Adult Twins. Twin Res. Hum. Genet. 2018, 21, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Park, S.A.; Lee, S.; Kwan, Y.; Choi, S.W. Revision and Validation of the Hwa-Byung Scale. Eur. Psychiatry 2022, 65, S544. [Google Scholar] [CrossRef]
- Lee, S.; Kim, J.; Park, S.A.; Kwan, Y.; Choi, S.W. Study for revision of Hwa-Byung Scale: The Delphi Method. Eur. Psychiatry 2022, 65, S548–S549. [Google Scholar] [CrossRef]
- Rim, S.J.; Hahm, B.J.; Seong, S.J.; Park, J.E.; Chang, S.M.; Kim, B.S.; An, H.; Jeon, H.J.; Hong, J.P.; Park, S. Prevalence of Mental Disorders and Associated Factors in Korean Adults: National Mental Health Survey of Korea 2021. Psychiatry Investig 2023, 20, 262–272. [Google Scholar] [CrossRef]
- Solmi, M.; Durbaba, S.; Ashworth, M.; Fusar-Poli, P. Proportion of young people in the general population consulting general practitioners: Potential for mental health screening and prevention. Early Interv. Psychiatry 2020, 14, 631–635. [Google Scholar] [CrossRef]
- Kim, J. Fairness in Korean Society: Assessing the Perspective of Millennials. Tech. Soc. Sci. J. 2020, 11, 482–495. [Google Scholar] [CrossRef]
- Shin, J.; Lee, Y.; Cho, S.I.; Sung, J.; Kim, S.; Lee, S.; Choi, I.; Han, C.; You, M. Implication of findings from a two-wave survey on embitterment in South Korea for strategies to promote mental health of the general public. Psychol. Trauma. 2023. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, S. Exposure to Negative Life Events and Post-Traumatic Embitterment Symptoms in Young Adults in Korea: Cumulative and Differential Effects. Psychopathology 2019, 52, 18–25. [Google Scholar] [CrossRef]
- Funnell, E.L.; Spadaro, B.; Martin-Key, N.; Metcalfe, T.; Bahn, S. mHealth Solutions for Mental Health Screening and Diagnosis: A Review of App User Perspectives Using Sentiment and Thematic Analysis. Front. Psychiatry 2022, 13, 857304. [Google Scholar] [CrossRef]
- Tavakol, M.; Wetzel, A. Factor Analysis: A means for theory and instrument development in support of construct validity. Int. J. Med. Educ. 2020, 11, 245–247. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.; Bell, M. XGBoost, A Novel Explainable AI Technique, in the Prediction of Myocardial Infarction: A UK Biobank Cohort Study. Clin. Med. Insights Cardiol. 2022, 16, 11795468221133611. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Jo, H.; Jeon, H.J.; Ahn, J.; Jeon, S.; Kim, J.K.; Chung, S. Dysfunctional Beliefs and Attitudes about Sleep-6 (DBAS-6): Data-driven shortened version from a machine learning approach. Sleep. Med. 2024, 119, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Wall, D.P.; Dally, R.; Luyster, R.; Jung, J.Y.; Deluca, T.F. Use of artificial intelligence to shorten the behavioral diagnosis of autism. PLoS ONE 2012, 7, e43855. [Google Scholar] [CrossRef]
- Moon, S.; Kim, Y. Subjective Perceptions of ‘Meaning of Work’ of Generation MZ Employees of South Korean NGOs. Behav. Sci. 2023, 13, 461. [Google Scholar] [CrossRef]
- Wood, N.D.; Akloubou Gnonhosou, D.C.; Bowling, J. Combining Parallel and Exploratory Factor Analysis in Identifying Relationship Scales in Secondary Data. Marriage Fam. Rev. 2015, 51, 385–395. [Google Scholar] [CrossRef]
- Braeken, J.; van Assen, M. An empirical Kaiser criterion. Psychol. Methods 2017, 22, 450–466. [Google Scholar] [CrossRef]
- Gholamy, A.; Kreinovich, V.; Kosheleva, O. Why 70/30 or 80/20 relation between training and testing sets: A pedagogical explanation. Int. J. Intell. Technol. Appl. Stat. 2018, 11, 105–111. [Google Scholar]
- Wang, S.M.; Kim, S.H.; Choi, W.S.; Lim, H.K.; Woo, Y.S.; Pae, C.U.; Bahk, W.M. The Impact of COVID-19 on Psychiatric Health in the Korean Population. Clin. Psychopharmacol. Neurosci. 2023, 21, 410–418. [Google Scholar] [CrossRef]
- Min, J.; Kwon, D.; Lee, W.; Kang, C.; Park, C.; Heo, S.; Bell, M.L.; Kim, H. Individual and regional characteristics associated with changes in mental health before and during the COVID-19 pandemic in South Korea. Sci. Rep. 2022, 12, 14189. [Google Scholar] [CrossRef]
- Montesinos López, O.A.; Montesinos López, A.; Crossa, J. Overfitting, model tuning, and evaluation of prediction performance. In Multivariate Statistical Machine Learning Methods for Genomic Prediction; Springer: Cham, Switzerland, 2022; pp. 109–139. [Google Scholar]
- Lin, S.; Wang, C.; Jiang, X.; Zhang, Q.; Luo, D.; Li, J.; Li, J.; Xu, J. Using machine learning to develop a five-item short form of the children’s depression inventory. BMC Public Health 2024, 24, 1118. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.A.; Edwards, C.; Davey-Rothwell, M.A.; Tobin, K.E. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict. Behav. 2017, 73, 133–136. [Google Scholar] [CrossRef] [PubMed]

| Questions | Psychological | Somatic | |
|---|---|---|---|
| 1 | My life is rather unhappy. | O | |
| 2 | There are times when I feel deep regret or resentment. | O | |
| 3 | I feel that my life is sorrowful. | O | |
| 4 | I feel sorrowful. | O | |
| 5 | I feel wronged. | O | |
| 6 * | My nerves are so fragile that I can’t control my emotions. | O | O |
| 7 | My hands and feet tremble, and I feel restless. | O | |
| 8 | I often feel disappointed in myself. | O | |
| 9 | My face often flushes with heat. | O | |
| 10 | I often feel a heat buildup in my chest. | O | |
| 11 | I often feel something rising from below (legs or abdomen) to above (chest). | O | |
| 12 | When I get angry, my hands feel numb or tremble. | O | |
| 13 | I have indigestion and often feel bloated. | O | |
| 14 * | I am very exhausted. | O | O |
| 15 | I feel that the world is unfair. | O | |
| Questions | Factor 1 | Factor 2 | |
|---|---|---|---|
| 1 | My life is rather unhappy. | 0.70 | 0.38 |
| 2 | There are times when I feel deep regret or resentment. | 0.77 | 0.27 |
| 3 | I feel that my life is sorrowful. | 0.83 | 0.36 |
| 4 | I feel sorrowful. | 0.82 | 0.37 |
| 5 | I feel wronged. | 0.70 | 0.44 |
| 6 | My nerves are so fragile that I can’t control my emotions. | 0.45 | 0.63 |
| 7 | My hands and feet tremble, and I feel restless. | 0.34 | 0.70 |
| 8 | I often feel disappointed in myself. | 0.58 | 0.43 |
| 9 | My face often flushes with heat. | 0.31 | 0.66 |
| 10 | I often feel a heat buildup in my chest. | 0.36 | 0.80 |
| 11 | I often feel something rising from below (legs or abdomen) to above (chest). | 0.30 | 0.77 |
| 12 | When I get angry, my hands feel numb or tremble. | 0.27 | 0.59 |
| 13 | I have indigestion and often feel bloated. | 0.29 | 0.54 |
| 14 | I am very exhausted. | 0.42 | 0.35 |
| 15 | I feel that the world is unfair. | 0.60 | 0.31 |
| k Value | Number of Selected Items | Cross-Validation Score (±SD) | t-Value (p-Value) | ANOVA (p-Value) |
|---|---|---|---|---|
| 1 | 2 | 0.8920 (±0.0248) | NA | F = 0.8593 (0.5051) |
| 2 | 4 | 0.9160 (±0.0307) | k = 1 vs. k = 2: t = −2.7530 (0.0512) | |
| 3 | 6 | 0.9140 (±0.0206) | k = 1 vs. k = 3: t = −1.5039 (0.2070) | |
| 4 | 8 | 0.9100 (±0.0303) | k = 1 vs. k = 4: t = −0.9705 (0.3868) | |
| 5 | 10 | 0.9240 (±0.0162) | k = 1 vs. k = 5: t = −1.9332 (0.1254) |
| Model | Class | Precision | Recall | F1-Score | Support |
|---|---|---|---|---|---|
| XGBoost | No HB | 0.89 | 0.94 | 0.92 | 89 |
| HB | 0.91 | 0.84 | 0.87 | 61 | |
| Accuracy | 0.90 | 150 | |||
| Macro avg | 0.90 | 0.89 | 0.89 | 150 | |
| Weighted avg | 0.90 | 0.90 | 0.90 | 150 | |
| LR | No HB | 0.87 | 0.97 | 0.91 | 89 |
| HB | 0.94 | 0.79 | 0.86 | 61 | |
| Accuracy | 0.89 | 150 | |||
| Macro avg | 0.90 | 0.88 | 0.89 | 150 | |
| Weighted avg | 0.90 | 0.89 | 0.89 | 150 | |
| RF | No HB | 0.89 | 0.94 | 0.92 | 89 |
| HB | 0.91 | 0.84 | 0.87 | 61 | |
| Accuracy | 0.90 | 150 | |||
| Macro avg | 0.90 | 0.89 | 0.89 | 150 | |
| Weighted avg | 0.90 | 0.90 | 0.90 | 150 | |
| SVM | No HB | 0.89 | 0.94 | 0.92 | 89 |
| HB | 0.91 | 0.84 | 0.87 | 61 | |
| Accuracy | 0.90 | 150 | |||
| Macro avg | 0.90 | 0.89 | 0.89 | 150 | |
| Weighted avg | 0.90 | 0.90 | 0.90 | 150 | |
| DT | No HB | 0.89 | 0.94 | 0.92 | 89 |
| HB | 0.91 | 0.84 | 0.87 | 61 | |
| Accuracy | 0.90 | 150 | |||
| Macro avg | 0.90 | 0.89 | 0.89 | 150 | |
| Weighted avg | 0.90 | 0.90 | 0.90 | 150 | |
| MLP | No HB | 0.89 | 0.94 | 0.92 | 89 |
| HB | 0.91 | 0.84 | 0.87 | 61 | |
| Accuracy | 0.90 | 150 | |||
| Macro avg | 0.90 | 0.89 | 0.89 | 150 | |
| Weighted avg | 0.90 | 0.90 | 0.90 | 150 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, C.-Y.; Lee, B.; Kim, S.-H.; Jeong, S.C.; Kim, J.-W. Development of a Short-Form Hwa-Byung Symptom Scale Using Machine Learning Approaches. Diagnostics 2024, 14, 2419. https://doi.org/10.3390/diagnostics14212419
Kwon C-Y, Lee B, Kim S-H, Jeong SC, Kim J-W. Development of a Short-Form Hwa-Byung Symptom Scale Using Machine Learning Approaches. Diagnostics. 2024; 14(21):2419. https://doi.org/10.3390/diagnostics14212419
Chicago/Turabian StyleKwon, Chan-Young, Boram Lee, Sung-Hee Kim, Seok Chan Jeong, and Jong-Woo Kim. 2024. "Development of a Short-Form Hwa-Byung Symptom Scale Using Machine Learning Approaches" Diagnostics 14, no. 21: 2419. https://doi.org/10.3390/diagnostics14212419
APA StyleKwon, C.-Y., Lee, B., Kim, S.-H., Jeong, S. C., & Kim, J.-W. (2024). Development of a Short-Form Hwa-Byung Symptom Scale Using Machine Learning Approaches. Diagnostics, 14(21), 2419. https://doi.org/10.3390/diagnostics14212419








