Coexistence of Hashimoto’s Thyroiditis in Differentiated Thyroid Cancer: Post-Operative Monitoring of Anti-Thyroglobulin Antibodies and Assessment of Treatment Response
Abstract
1. Introduction
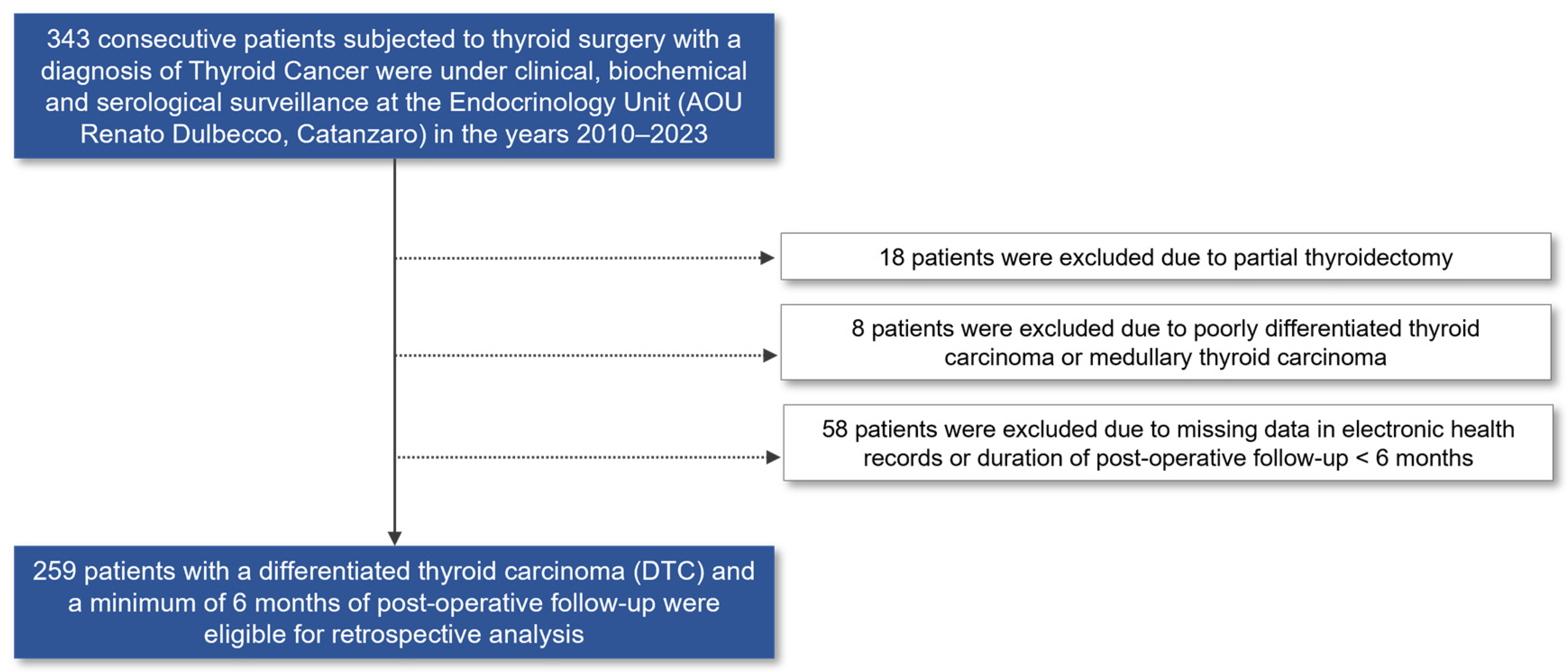
2. Materials and Methods
2.1. Study Population
2.2. Outcome Assessment and Laboratory Determinations
2.3. Statistical Analysis
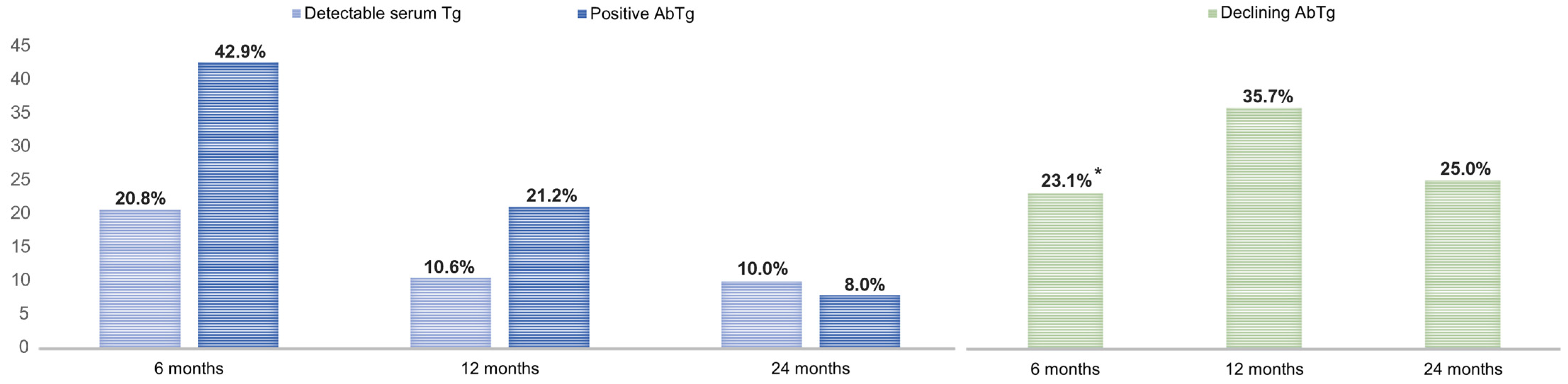
3. Results
3.1. Characteristics of Patients with Differentiated Thyroid Cancer (DTC) Compared by Pre-Operative Hashimoto’s Thyroiditis (HT) Status
3.2. Outcomes of DTC by Pre-Operative HT Status and Predictors of Persistence of Indeterminate Response
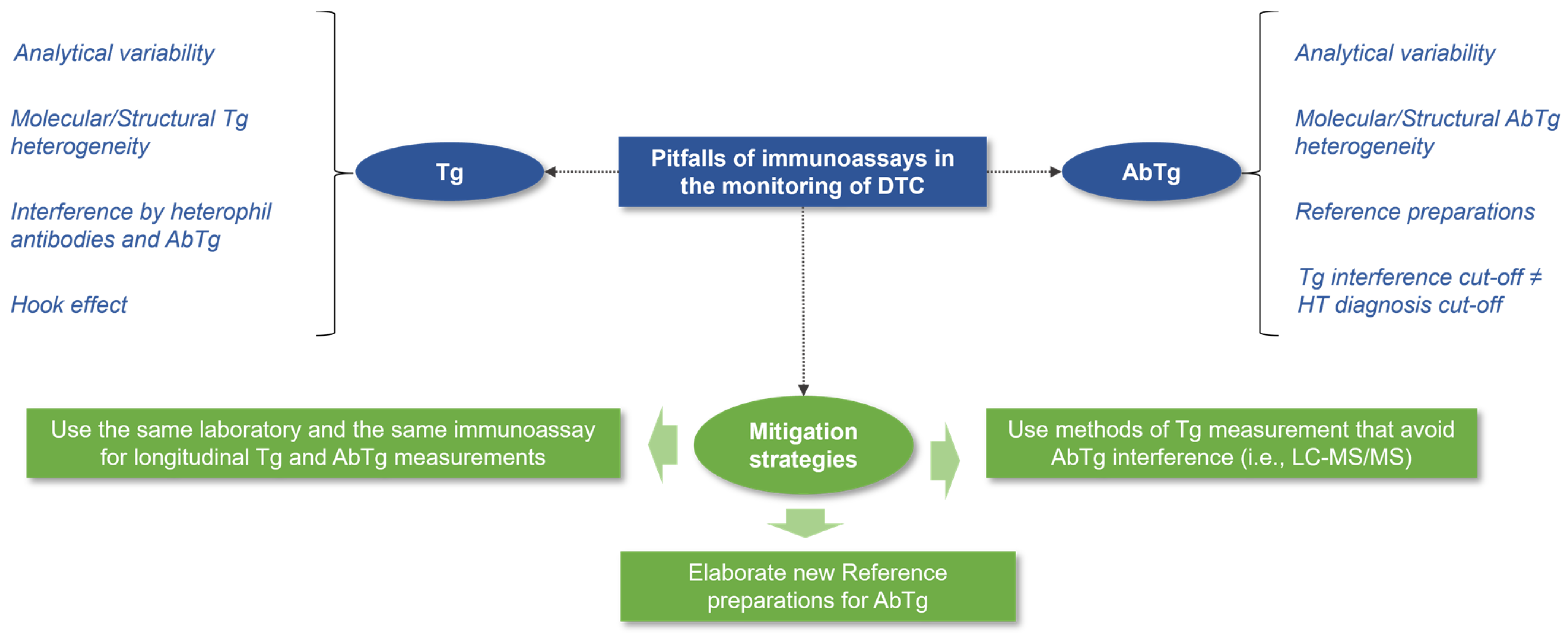
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, J.H.; Kim, Y.; Choi, J.W.; Kim, Y.S. The association between papillary thyroid carcinoma and histologically proven Hashimoto’s thyroiditis: A meta-analysis. Eur. J. Endocrinol. 2013, 168, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Kim, W.G.; Kim, W.B.; Kim, T.Y.; Kim, H.M.; Ryu, J.-S.; Hong, S.J.; Gong, G.; Shong, Y.K. Coexistence of chronic lymphocytic thyroiditis is associated with lower recurrence rates in patients with papillary thyroid carcinoma. Clin. Endocrinol. 2009, 71, 581–586. [Google Scholar] [CrossRef]
- Lai, X.; Xia, Y.; Zhang, B.; Li, J.; Jiang, Y. A meta-analysis of Hashimoto’s thyroiditis and papillary thyroid carcinoma risk. Oncotarget 2017, 8, 62414–62424. [Google Scholar] [CrossRef] [PubMed]
- Resende de Paiva, C.; Grønhøj, C.; Feldt-Rasmussen, U.; von Buchwald, C. Association between Hashimoto’s Thyroiditis and Thyroid Cancer in 64,628 Patients. Front. Oncol. 2017, 7, 53. [Google Scholar] [CrossRef] [PubMed]
- Weetman, A.P. Cellular immune responses in autoimmune thyroid disease. Clin. Endocrinol. 2004, 61, 405–413. [Google Scholar] [CrossRef]
- Pandit, A.A.; Vijay Warde, M.; Menon, P.S. Correlation of number of intrathyroid lymphocytes with antimicrosomal antibody titer in Hashimoto’s thyroiditis. Diagn. Cytopathol. 2003, 28, 63–65. [Google Scholar] [CrossRef]
- McLachlan, S.M.; Rapoport, B. Why measure thyroglobulin autoantibodies rather than thyroid peroxidase autoantibodies? Thyroid 2004, 14, 510–520. [Google Scholar] [CrossRef]
- Hu, X.; Chen, Y.; Shen, Y.; Tian, R.; Sheng, Y.; Que, H. Global prevalence and epidemiological trends of Hashimoto’s thyroiditis in adults: A systematic review and meta-analysis. Front. Public Health 2022, 10, 1020709. [Google Scholar] [CrossRef]
- Zhang, L.; Zhou, L.; Feng, Q.; Li, Q.; Ge, M. Mutation of Hashimoto’s Thyroiditis and Papillary Thyroid Carcinoma Related Genes and the Screening of Candidate Genes. Front. Oncol. 2021, 11, 813802. [Google Scholar] [CrossRef]
- Xu, J.; Ding, K.; Mu, L.; Huang, J.; Ye, F.; Peng, Y.; Guo, C.; Ren, C. Hashimoto’s Thyroiditis: A “Double-Edged Sword” in Thyroid Carcinoma. Front. Endocrinol. 2022, 13, 801925. [Google Scholar] [CrossRef]
- Marotta, V.; Guerra, A.; Zatelli, M.C.; Degli Uberti, E.; Di Stasi, V.; Faggiano, A.; Colao, A.; Vitale, M. BRAF mutation positive papillary thyroid carcinoma is less advanced when Hashimoto’s thyroiditis lymphocytic infiltration is present. Clin. Endocrinol. 2013, 79, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Giordano, C.; Barone, I.; Marsico, S.; Bruno, R.; Bonofiglio, D.; Catalano, S.; Andò, S. Endemic Goiter and Iodine Prophylaxis in Calabria, a Region of Southern Italy: Past and Present. Nutrients 2019, 11, 2428. [Google Scholar] [CrossRef] [PubMed]
- Chiefari, E.; Innaro, N.; Gervasi, R.; Mirabelli, M.; Giuliano, S.; Donnici, A.; Obiso, S.; Brunetti, F.S.; Foti, D.P.; Brunetti, A. Incidental thyroid carcinoma in an endemic goiter area in Italy: Histopathological features and predictors of a common finding. Endocrine, 2023; accepted for publication—In press. [Google Scholar]
- Mohammadi, B.; Dua, K.; Saghafi, M.; Singh, S.K.; Heydarifard, Z.; Zandi, M. COVID-19-induced autoimmune thyroiditis: Exploring molecular mechanisms. J. Med. Virol. 2023, 95, e29001. [Google Scholar] [CrossRef] [PubMed]
- Tsang, V.H.M.; Gild, M.; Glover, A.; Clifton-Bligh, R.; Robinson, B.G. Thyroid cancer in the age of COVID-19. Endocr. Relat. Cancer 2020, 27, R407–R416. [Google Scholar] [CrossRef]
- Spencer, C.A.; Takeuchi, M.; Kazarosyan, M.; Wang, C.C.; Guttler, R.B.; Singer, P.A.; Fatemi, S.; LoPresti, J.S.; Nicoloff, J.T. Serum thyroglobulin autoantibodies: Prevalence, influence on serum thyroglobulin measurement, and prognostic significance in patients with differentiated thyroid carcinoma. J. Clin. Endocrinol. Metab. 1998, 83, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Bayer, M.F.; Kriss, J.P. Immunoradiometric assay for serum thyroglobulin: Semiquantitative measurement of thyroglobulin in antithyroglobulin-positive sera. J. Clin. Endocrinol. Metab. 1979, 49, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Feldt-Rasmussen, U.; Rasmussen, A.K. Autoimmunity in differentiated thyroid cancer: Significance and related clinical problems. Hormones 2010, 9, 109–117. [Google Scholar] [CrossRef]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- De Leo, S.; D’Elia, S.; Grani, G.; Dondi, F.; Bertagna, F.; Puxeddu, E.; Morelli, S.; Piovesan, A.; Nervo, A.; Zatelli, M.C.; et al. A Prospective Multicenter Study Examining the Relationship Between Thyroid Cancer Treatment Outcomes and the Presence of Autoimmune Thyroiditis. Thyroid 2023, 33, 1318–1326. [Google Scholar] [CrossRef]
- Benvenga, S.; Trimarchi, F. Changed presentation of Hashimoto’s thyroiditis in North-Eastern Sicily and Calabria (Southern Italy) based on a 31-year experience. Thyroid 2008, 18, 429–441. [Google Scholar] [CrossRef]
- Lloyd, R.V.; Osamura, R.Y.; Klöppel, G.; Rosai, J. WHO Classification of Tumours of Endocrine Organs, 4th ed.; IARC: Lyon, France, 2017.
- Tuttle, R.M.; Haugen, B.; Perrier, N.D. Updated American Joint Committee on Cancer/Tumor-Node-Metastasis Staging System for Differentiated and Anaplastic Thyroid Cancer (Eighth Edition): What Changed and Why? Thyroid 2017, 27, 751–756. [Google Scholar] [CrossRef]
- Giuliano, S.; Mirabelli, M.; Chiefari, E.; Vergine, M.; Gervasi, R.; Brunetti, F.S.; Innaro, N.; Donato, G.; Aversa, A.; Brunetti, A. Malignancy Analyses of Thyroid Nodules in Patients Subjected to Surgery with Cytological- and Ultrasound-Based Risk Stratification Systems. Endocrines 2020, 1, 102–118. [Google Scholar] [CrossRef]
- Giuliano, S.; Mirabelli, M.; Chiefari, E.; Tocci, V.; Donnici, A.; Iuliano, S.; Salatino, A.; Foti, D.P.; Aversa, A.; Brunetti, A. The Initial ATA Risk Classification, but Not the AJCC/TNM Stage, Predicts the Persistence or Relapse of Differentiated Thyroid Cancer in Long-Term Surveillance. Endocrines 2022, 3, 512–521. [Google Scholar] [CrossRef]
- Feldt-Rasmussen, U.; Profilis, C.; Colinet, E.; Black, E.; Bornet, H.; Bourdoux, P.; Carayon, P.; Ericsson, U.B.; Koutras, D.A.; de Leon, L.L.; et al. Human thyroglobulin reference material (CRM 457). 1st Part: Assessment of homogeneity, stability and immunoreactivity. Ann. Biol. Clin. 1996, 54, 337–342. [Google Scholar]
- Feldt-Rasmussen, U.; Profilis, C.; Colinet, E.; Black, E.; Bornet, H.; Bourdoux, P.; Carayon, P.; Ericsson, U.B.; Koutras, D.A.; de Leon, L.L.; et al. Human thyroglobulin reference material (CRM 457). 2nd Part: Physicochemical characterization and certification. Ann. Biol. Clin. 1996, 54, 343–348. [Google Scholar]
- Standard MRC 65; International Reference Preparation. National Council for Biological Standards and Control: London, UK, 1993.
- Noel, J.E.; Thatipamala, P.; Hung, K.S.; Chen, J.; Shi, R.Z.; Orloff, L.A. Pre-Operative Antithyroid Antibodies in Differentiated Thyroid Cancer. Endocr. Pract. 2021, 27, 1114–1118. [Google Scholar] [CrossRef]
- Ullmann, T.M.; Papaleontiou, M.; Sosa, J.A. Current Controversies in Low-Risk Differentiated Thyroid Cancer: Reducing Overtreatment in an Era of Overdiagnosis. J. Clin. Endocrinol. Metab. 2023, 108, 271–280. [Google Scholar] [CrossRef]
- Lim, E.S.; Shah, S.G.; Waterhouse, M.; Akker, S.; Drake, W.; Plowman, N.; Berney, D.M.; Richards, P.; Adams, A.; Nowosinska, E.; et al. Impact of thyroiditis on 131I uptake during ablative therapy for differentiated thyroid cancer. Endocr. Connect. 2019, 8, 571–578. [Google Scholar] [CrossRef]
- Dvorkin, S.; Robenshtok, E.; Hirsch, D.; Strenov, Y.; Shimon, I.; Benbassat, C.A. Differentiated thyroid cancer is associated with less aggressive disease and better outcome in patients with coexisting Hashimotos thyroiditis. J. Clin. Endocrinol. Metab. 2013, 98, 2409–2414. [Google Scholar] [CrossRef]
- Liu, J.; Xu, T.; Ma, L.; Chang, W. Signal Pathway of Estrogen and Estrogen Receptor in the Development of Thyroid Cancer. Front. Oncol. 2021, 11, 593479. [Google Scholar] [CrossRef]
- Hay, I.D.; Johnson, T.R.; Thompson, G.B.; Sebo, T.J.; Reinalda, M.S. Minimal extrathyroid extension in papillary thyroid carcinoma does not result in increased rates of either cause-specific mortality or postoperative tumor recurrence. Surgery 2016, 159, 11–19. [Google Scholar] [CrossRef]
- Görges, R.; Maniecki, M.; Jentzen, W.; Sheu, S.N.-Y.; Mann, K.; Bockisch, A.; Janssen, O.E. Development and clinical impact of thyroglobulin antibodies in patients with differentiated thyroid carcinoma during the first 3 years after thyroidectomy. Eur. J. Endocrinol. 2005, 153, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Wild, D. The Immunoassay Handbook: Theory and Applications of Ligand Binding, Elisa and Related Techniques, 4th ed.; Elsevier Ltd.: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Tate, J.; Ward, G. Interferences in immunoassay. Clin. Biochem. Rev. 2004, 25, 105–120. [Google Scholar]
- Spencer, C.; Fatemi, S.; Singer, P.; Nicoloff, J.; Lopresti, J. Serum Basal thyroglobulin measured by a second-generation assay correlates with the recombinant human thyrotropin-stimulated thyroglobulin response in patients treated for differentiated thyroid cancer. Thyroid 2010, 20, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Malandrino, P.; Latina, A.; Marescalco, S.; Spadaro, A.; Regalbuto, C.; Fulco, R.A.; Scollo, C.; Vigneri, R.; Pellegriti, G. Risk-adapted management of differentiated thyroid cancer assessed by a sensitive measurement of basal serum thyroglobulin. J. Clin. Endocrinol. Metab. 2011, 96, 1703–1709. [Google Scholar] [CrossRef] [PubMed]
- Chindris, A.M.; Diehl, N.N.; Crook, J.E.; Fatourechi, V.; Smallridge, R.C. Undetectable sensitive serum thyroglobulin (<0.1 ng/ml) in 163 patients with follicular cell-derived thyroid cancer: Results of rhTSH stimulation and neck ultrasonography and long- term biochemical and clinical follow-up. J. Clin. Endocrinol. Metab. 2012, 97, 2714–2723. [Google Scholar] [CrossRef][Green Version]
- Jahagirdar, V.R.; Strouhal, P.; Holder, G.; Gama, R.; Singh, B.M. Thyrotoxicosis factitia masquerading as recurrent Graves’ disease: Endogenous antibody immunoassay interference, a pitfall for the unwary. Ann. Clin. Biochem. 2008, 45 Pt 3, 325–327. [Google Scholar] [CrossRef]
- Netzel, B.C.; Grebe, S.K.; Carranza Leon, B.G.; Castro, M.R.; Clark, P.M.; Hoofnagle, A.N.; Spencer, C.A.; Turcu, A.F.; Algeciras-Schimnich, A. Thyroglobulin (Tg) Testing Revisited: Tg Assays, TgAb Assays, and Correlation of Results with Clinical Outcomes. J. Clin. Endocrinol. Metab. 2015, 100, E1074–E1083. [Google Scholar] [CrossRef]
- Schoonen, L.; Neele, M.; van Toor, H.; van Kinschot, C.M.J.; van Noord, C.; Visser, W.E.; Groen, J.; Boesten, L.S.M.; Lentjes, E.G.W.M.; van den Berg, S.A.A.; et al. Impact of Thyroglobulin and Thyroglobulin Antibody Assay Performance on the Differential Classification of DTC Patients. J. Endocr. Soc. 2021, 6, bvab166. [Google Scholar] [CrossRef]
- Latrofa, F.; Ricci, D.; Sisti, E.; Piaggi, P.; Nencetti, C.; Marinò, M.; Vitti, P.; Dekker, B.L.; van der Horst-Schrivers, A.N.; Sluiter, W.J.; et al. Significance of Low Levels of Thyroglobulin Autoantibodies Associated with Undetectable Thyroglobulin After Thyroidectomy for Differentiated Thyroid Carcinoma. Thyroid 2016, 26, 798–806. [Google Scholar] [CrossRef]
- Spencer, C.; Petrovic, I.; Fatemi, S. Current thyroglobulin autoantibody (TgAb) assays often fail to detect interfering TgAb that can result in the reporting of falsely low/undetectable serum Tg IMA values for patients with differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 2011, 96, 1283–1291. [Google Scholar] [CrossRef] [PubMed]
- Pickett, A.J.; Jones, M.; Evans, C. Causes of discordance between thyroglobulin antibody assays. Ann. Clin. Biochem. 2012, 49 Pt 5, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Katrangi, W.; Grebe, S.K.G.; Algeciras-Schimnich, A. Analytical and clinical performance of thyroglobulin autoantibody assays in thyroid cancer follow-up. Clin. Chem. Lab. Med. 2017, 55, 1987–1994. [Google Scholar] [CrossRef] [PubMed]
- Feldt-Rasmussen, U.; Schlumberger, M. European interlaboratory comparison of serum thyroglobulin measurement. J. Endocrinol. Investig. 1988, 11, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Tozzoli, R.; D’Aurizio, F.; Villalta, D.; Giovanella, L. Evaluation of the first fully automated immunoassay method for the measurement of stimulating TSH receptor autoantibodies in Graves’ disease. Clin. Chem. Lab. Med. 2017, 55, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Spencer, C.A.; Lopresti, J.S. Measuring thyroglobulin and thyroglobulin autoantibody in patients with differentiated thyroid cancer. Nat. Clin. Pract. Endocrinol. Metab. 2008, 4, 223–233. [Google Scholar] [CrossRef]
- Schlumberger, M.; Leboulleux, S.; Catargi, B.; Deandreis, D.; Zerdoud, S.; Bardet, S.; Rusu, D.; Godbert, Y.; Buffet, C.; Schvartz, C.; et al. Outcome after ablation in patients with low-risk thyroid cancer (ESTIMABL1): 5-year follow-up results of a randomised, phase 3, equivalence trial. Lancet Diabetes Endocrinol. 2018, 6, 618–626. [Google Scholar] [CrossRef]
- Leboulleux, S.; Bournaud, C.; Chougnet, C.N.; Zerdoud, S.; Catargi, B.N.; Cao, C.D.; Kelly, A.; Barge, M.-L.; Dygay, I.; Vera, P.; et al. Estimabl2: Is There a Need for Radioiodine Ablation in Low Risk Differentiated Thyroid Cancer (DTC) Patients?: Results From the French Randomized Phase III Prospective Trial on 776 Patients (NCT 01837745). J. Endocr. Soc. 2021, 5 (Suppl. S1), A875. [Google Scholar] [CrossRef]
- Scharpf, J.; Tuttle, M.; Wong, R.; Ridge, D.; Smith, R.; Hartl, D.; Levine, R.; Randolph, G. Comprehensive management of recurrent thyroid cancer: An American Head and Neck Society consensus statement: AHNS consensus statement. Head Neck 2016, 38, 1862–1869. [Google Scholar] [CrossRef]
- Stevic, I.; Dembinski, T.C.; Pathak, K.A.; Leslie, W.D. Transient early increase in thyroglobulin levels post-radioiodine ablation in patients with differentiated thyroid cancer. Clin. Biochem. 2015, 48, 658–661. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Du, W.H.; Zhang, C.X.; Zhao, S.-X.; Song, H.-D.; Gao, G.-Q.; Dong, M. The effect of radioiodine treatment on the characteristics of TRAb in Graves’ disease. BMC Endocr. Disord. 2021, 21, 238. [Google Scholar] [CrossRef] [PubMed]
- Yin, N.; Sherman, S.I.; Pak, Y.; Litofsky, D.R.; Gianoukakis, A.G.; National Thyroid Cancer Treatment Cooperative Study Group. The De Novo Detection of Anti-Thyroglobulin Antibodies and Differentiated Thyroid Cancer Recurrence. Thyroid 2020, 30, 1490–1495. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | HT-Negative (n = 182) | HT-Positive (n = 77) | p |
|---|---|---|---|
| Females, n | 137 (74.7%) | 67 (87.0%) | 0.028 |
| Age at diagnosis, years | 46 (36–57) | 43 (32–51) | 0.058 |
| Follow-up duration, years | 5 (2–10) | 3 (1–6) | 0.001 |
| Thyroidectomy was performed due to a cytologically suspicious nodular disease †, n | 76 (58.9% *) | 30 (46.1% *) | 0.092 |
| TIR 3b | 26 (34.2%) | 8 (26.7%) | |
| TIR 4 | 31 (40.8%) | 14 (46.6%) | |
| TIR 5 | 19 (25.0%) | 8 (26.7%) | |
| DTC histology, n | 0.026 | ||
| PTC | 157 (86.3%) | 75 (97.4%) | |
| High risk PTC subtypes ** | 9 (5.7% of all PTCs) | 9 (11.7% of all PTCs) | |
| FTC | 17 (9.3%) | 1 (1.3%) | |
| HCC | 8 (4.3%) | 1 (1.3%) | |
| Tumor size, mm | 13.5 (8.0–19.5) | 11.0 (8.0–18.0) | 0.408 |
| Tumor size category, n | |||
| T1a | 61 (33.5%) | 32 (41.5%) | |
| T1b | 53 (29.1%) | 24 (31.2%) | |
| T2 | 15 (8.3%) | 10 (13.0%) | |
| T3a | 4 (2.2%) | 2 (2.6%) | |
| T3b | 49 (26.9%) | 9 (11.7%) | |
| T4a | 0 (0%) | 0 (0%) | |
| T4b | 0 (0%) | 0 (0%) | |
| ETE, n | 72 (39.6%) | 17 (22.1%) | 0.007 |
| Minimal ETE | 23 (31.9% of all ETE) | 8 (47.1% of all ETE) | |
| Multifocality, n | 38 (30.9%) | 18 (23.4%) | 0.655 |
| Lymph node metastasis, n | 28 (15.4%) | 11 (14.3%) | 0.821 |
| Distant site metastasis, n | 3 (1.6%) | 0 (0%) | 0.257 |
| AJCC/TNM stage, n | 0.741 | ||
| Stage 1 | 173 (95.1%) | 74 (96.1%) | |
| Stage 2 | 3 (1.6%) | 2 (2.6%) | |
| Stage 3 | 2 (1.1%) | 1 (1.3%) | |
| Stage 4a | 2 (1.1%) | 0 (0%) | |
| Stage 4b | 2 (1.1%) | 0 (0%) | |
| ATA risk stage, n | 0.409 | ||
| Low | 102 (56.0%) | 50 (64.9%) | |
| Intermediate | 52 (28.6%) | 18 (23.4%) | |
| High | 28 (15.4%) | 9 (11.7%) | |
| Adjuvant RAI, n | 123 (67.6%) | 44 (57.1%) | 0.202 |
| >1 cycle | 16 (13.0% of all RAI) | 2 (4.5% of all RAI) | |
| Adjuvant TKI therapy, n | 4 (2.2%) | 0 (0%) | 0.321 |
| Pre-operative positive AbTg antibodies, n | _ | 13 (16.9%) |
| Response to DTC Therapy | 6 Months | 12 Months | 24 Months | >24 Months * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HT Negative (n = 182) | HT Positive (n = 77) | p | HT Negative (n = 161) | HT Positive (n = 66) | p | HT Negative (n = 142) | HT Positive (n = 50) | p | HT Negative (n = 125 †) | HT Positive (n = 40) | p | |
| Excellent, n | 107 (58.8%) | 35 (45.5%) | <0.001 | 127 (78.9%) | 55 (83.3%) | 0.029 | 117 (82.4%) | 44 (88.0%) | 0.145 | 101 (80.8%) | 38 (95.0%) | 0.509 |
| Biochemically incomplete, n | 29 (15.9%) | 7 (9.1%) | 15 (9.3%) | 1 (1.5%) | 9 (6.4%) | 0 (0%) | 9 (7.2%) | 0 (0%) | ||||
| Indeterminate, n | 34 (18.7%) | 35 (45.4%) | 10 (6.2%) | 9 (13.6%) | 8 (5.6%) | 5 (10.0%) | 8 (6.4%) | 1 (2.5%) | ||||
| Structurally incomplete, n | 12 (6.6%) | 0 (0%) | 9 (5.6%) | 1 (1.5%) | 8 (5.6%) | 1 (2.0%) | 6 (4.8%) | 1 (2.5%) | ||||
| Persistence of indeterminate response, n | 5/34 (14.7%) | 7/35 (20.0%) | 0.752 | 4/10 (40.0%) | 3/9 (33.3%) | 0.999 | ||||||
| New onset indeterminate response, n | 5/10 (50.0%) | 2/9 (22.2%) | 0.349 | 4/8 (50.0%) | 2/5 (40.0%) | 0.999 | ||||||
| Standardized β | Odds Ratio | 95% CI | p | |
|---|---|---|---|---|
| Male sex | 0.466 | 13.355 | 1.551–114.994 | 0.018 |
| Age at diagnosis | −2.092 | 1.030 | 0.967–1.113 | 0.306 |
| Tumor size | 2.592 | 0.976 | 0.906–1.052 | 0.529 |
| HT-positive status | 1.086 | 2.962 | 0.512–17.132 | 0.225 |
| Adjuvant RAI | −1.041 | 0.353 | 0.047–2.644 | 0.311 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donnici, A.; Mirabelli, M.; Giuliano, S.; Misiti, R.; Tocci, V.; Greco, M.; Aiello, V.; Brunetti, F.S.; Chiefari, E.; Aversa, A.; et al. Coexistence of Hashimoto’s Thyroiditis in Differentiated Thyroid Cancer: Post-Operative Monitoring of Anti-Thyroglobulin Antibodies and Assessment of Treatment Response. Diagnostics 2024, 14, 166. https://doi.org/10.3390/diagnostics14020166
Donnici A, Mirabelli M, Giuliano S, Misiti R, Tocci V, Greco M, Aiello V, Brunetti FS, Chiefari E, Aversa A, et al. Coexistence of Hashimoto’s Thyroiditis in Differentiated Thyroid Cancer: Post-Operative Monitoring of Anti-Thyroglobulin Antibodies and Assessment of Treatment Response. Diagnostics. 2024; 14(2):166. https://doi.org/10.3390/diagnostics14020166
Chicago/Turabian StyleDonnici, Alessandra, Maria Mirabelli, Stefania Giuliano, Roberta Misiti, Vera Tocci, Marta Greco, Vincenzo Aiello, Francesco S. Brunetti, Eusebio Chiefari, Antonio Aversa, and et al. 2024. "Coexistence of Hashimoto’s Thyroiditis in Differentiated Thyroid Cancer: Post-Operative Monitoring of Anti-Thyroglobulin Antibodies and Assessment of Treatment Response" Diagnostics 14, no. 2: 166. https://doi.org/10.3390/diagnostics14020166
APA StyleDonnici, A., Mirabelli, M., Giuliano, S., Misiti, R., Tocci, V., Greco, M., Aiello, V., Brunetti, F. S., Chiefari, E., Aversa, A., Foti, D. P., & Brunetti, A. (2024). Coexistence of Hashimoto’s Thyroiditis in Differentiated Thyroid Cancer: Post-Operative Monitoring of Anti-Thyroglobulin Antibodies and Assessment of Treatment Response. Diagnostics, 14(2), 166. https://doi.org/10.3390/diagnostics14020166












