How Can We Identify T1 or Shallow T2 Gallbladder Carcinoma Using Ultrasound? Comment on Okaniwa, S. How Can We Manage Gallbladder Lesions by Transabdominal Ultrasound? Diagnostics 2021, 11, 784
Institutional Review Board Statement
Conflicts of Interest
References
- Okaniwa, S. How Can We Manage Gallbladder Lesions by Transabdominal Ultrasound? Diagnostics 2021, 11, 784. [Google Scholar] [CrossRef] [PubMed]
- Wakai, T.; Shirai, Y.; Yokoyama, N.; Ajioka, Y.; Watanabe, H.; Hatakeyama, K. Depth of subserosal invasion predicts long-term survival after resection in patients with T2 gallbladder carcinoma. Ann. Surg. Oncol. 2003, 10, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Katayama, A.; Watanabe, H.; Noda, Y.; Abe, M.; Sato, M.; Yoshida, K. Morphological characteristics of early carcinoma of the gallbladder. Tan to Sui 1990, 11, 1115–1120. (In Japanese) [Google Scholar]
- Kijima, H. Morphological characteristics of gallbladder cancer. J. Jpn. Biliary Assoc. 2008, 22, 207–216, (In Japanese with English Abstract). [Google Scholar]
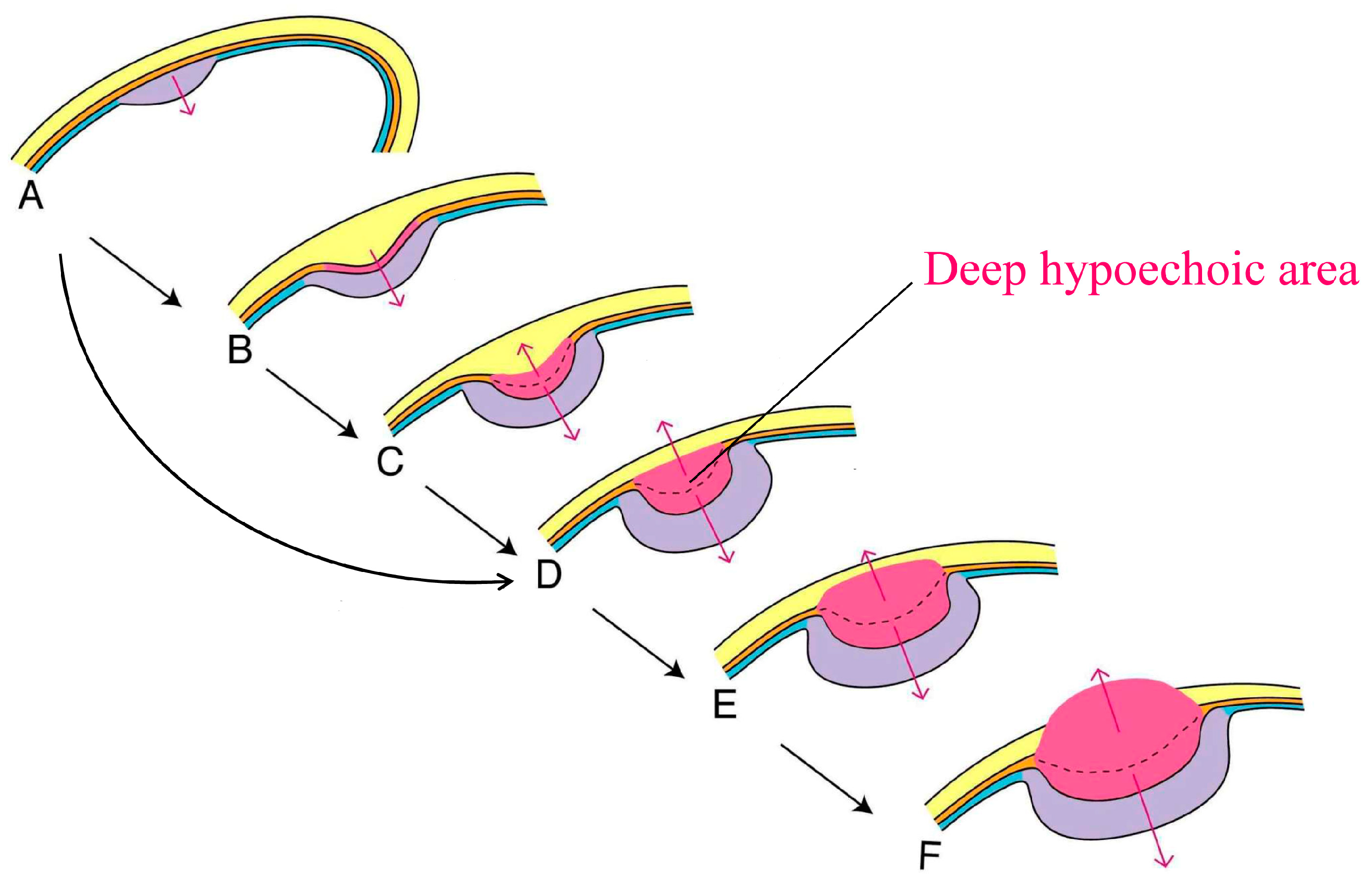
- Fujimoto, T.; Kato, Y. Polypoid gallbladder tumors with a deep hypoechoic area and a conically thickened outermost hyperechoic layer suggest shallow T2 carcinoma. Acta Radiol. Open 2019, 8, 2058460119847995. [Google Scholar] [CrossRef] [PubMed]
- Katayama, A. Morphological comparison between pm-carcinoma and minute ss-carcinoma of the gallbladder. Jpn. J. Gastroenterol. 1992, 89, 1260–1269, (In Japanese with English Abstract). [Google Scholar]
- Kanno, Y.; Ito, K.; Noda, Y.; Kobayashi, G.; Koshita, S.; Ogawa, T.; Masu, K.; Yamada, R.; Michikawa, Y.; Iwashita, Y. Diagnosis of gallbladder cancer on US and EUS. Tan to Sui 2015, 36, 25–30. (In Japanese) [Google Scholar]
- Ito, K.; Koshita, S.; Kanno, Y.; Ogawa, T.; Kusunose, H.; Sakai, T. Diagnosis by endoscopic ultrasonography and intraductal ultrasonography for biliary cancer. J. Jpn. Biliary Assoc. 2021, 35, 143–150, (In Japanese with English Abstract). [Google Scholar]
- Fujita, N.; Noda, Y.; Kobayashi, G.; Kimura, K.; Yago, A. Diagnosis of the depth of invasion of gallbladder carcinoma by EUS. Gastrointest Endosc. 1999, 50, 659–663. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, T.; Morita, S.; Tsuchiya, S. What condition does gallbladder tumor with a deep hypoechoic area suggest except T2 carcinoma? J. Clin. Ultrasound 2022, 51, 184–186. [Google Scholar] [CrossRef] [PubMed]
- Mitake, M.; Nakazawa, S.; Naitoh, Y.; Kimoto, E.; Tsukamoto, Y.; Asai, T.; Yamao, K.; Inui, K.; Morita, K.; Hayashi, Y. Endoscopic ultrasonography in diagnosis of the extent of gallbladder carcinoma. Gastrointest. Endosc. 1990, 36, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Okaniwa, S. Role of conventional ultrasonography in the diagnosis of gallbladder polypoid lesions. J. Med. Ultrason. 2021, 48, 149–157. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujimoto, T. How Can We Identify T1 or Shallow T2 Gallbladder Carcinoma Using Ultrasound? Comment on Okaniwa, S. How Can We Manage Gallbladder Lesions by Transabdominal Ultrasound? Diagnostics 2021, 11, 784. Diagnostics 2024, 14, 164. https://doi.org/10.3390/diagnostics14020164
Fujimoto T. How Can We Identify T1 or Shallow T2 Gallbladder Carcinoma Using Ultrasound? Comment on Okaniwa, S. How Can We Manage Gallbladder Lesions by Transabdominal Ultrasound? Diagnostics 2021, 11, 784. Diagnostics. 2024; 14(2):164. https://doi.org/10.3390/diagnostics14020164
Chicago/Turabian StyleFujimoto, Taketoshi. 2024. "How Can We Identify T1 or Shallow T2 Gallbladder Carcinoma Using Ultrasound? Comment on Okaniwa, S. How Can We Manage Gallbladder Lesions by Transabdominal Ultrasound? Diagnostics 2021, 11, 784" Diagnostics 14, no. 2: 164. https://doi.org/10.3390/diagnostics14020164
APA StyleFujimoto, T. (2024). How Can We Identify T1 or Shallow T2 Gallbladder Carcinoma Using Ultrasound? Comment on Okaniwa, S. How Can We Manage Gallbladder Lesions by Transabdominal Ultrasound? Diagnostics 2021, 11, 784. Diagnostics, 14(2), 164. https://doi.org/10.3390/diagnostics14020164





