The Usefulness of the Regression-Based Normed SKT Short Cognitive Performance Test in Detecting Cognitive Impairment in a Community Sample
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Cognitive Measures
2.2.1. SKT
2.2.2. MMSE
2.2.3. ACE-III
2.2.4. Data Collection
2.2.5. Consensus Diagnoses
2.2.6. Comparing Group Status across Measures
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
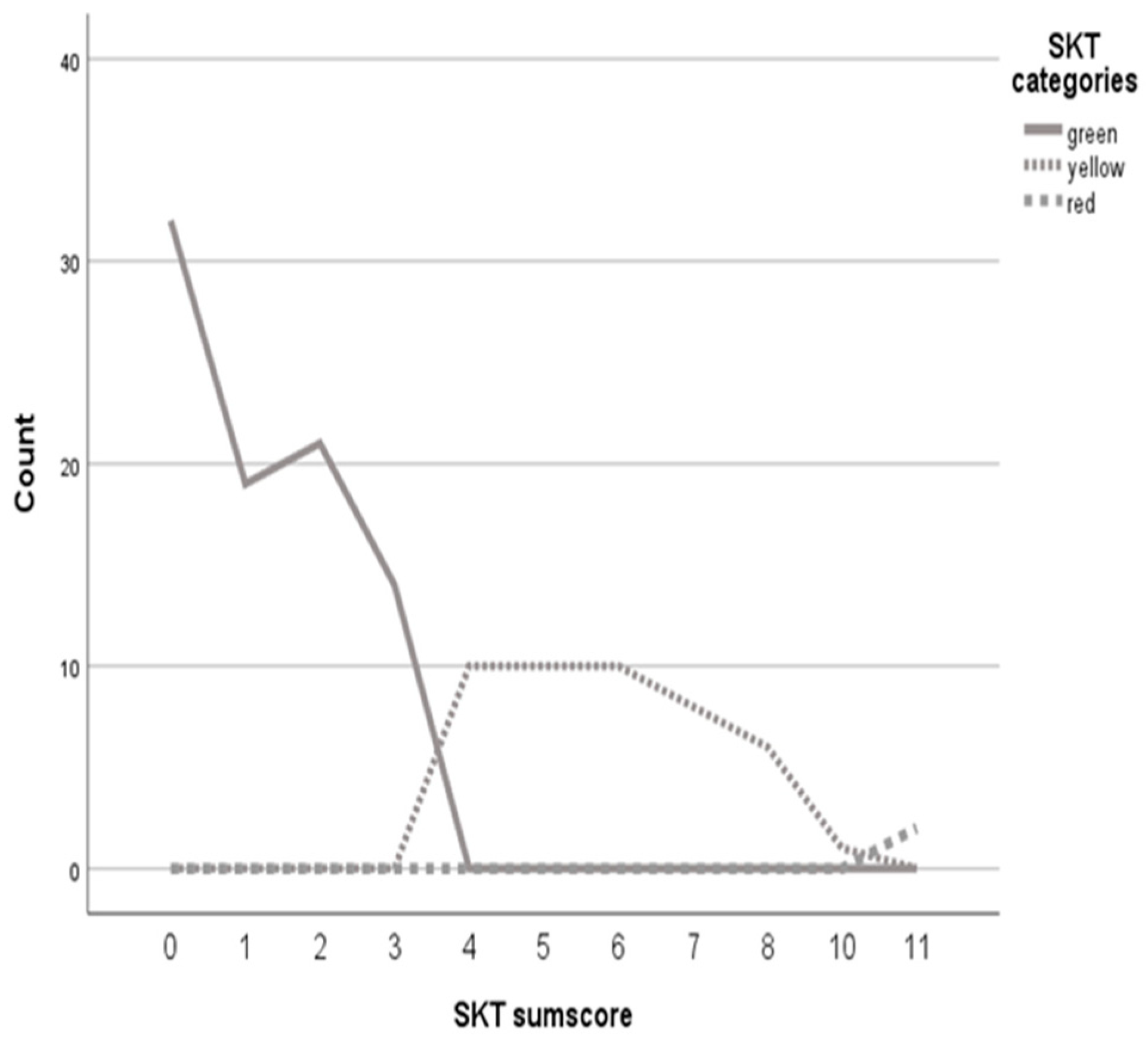
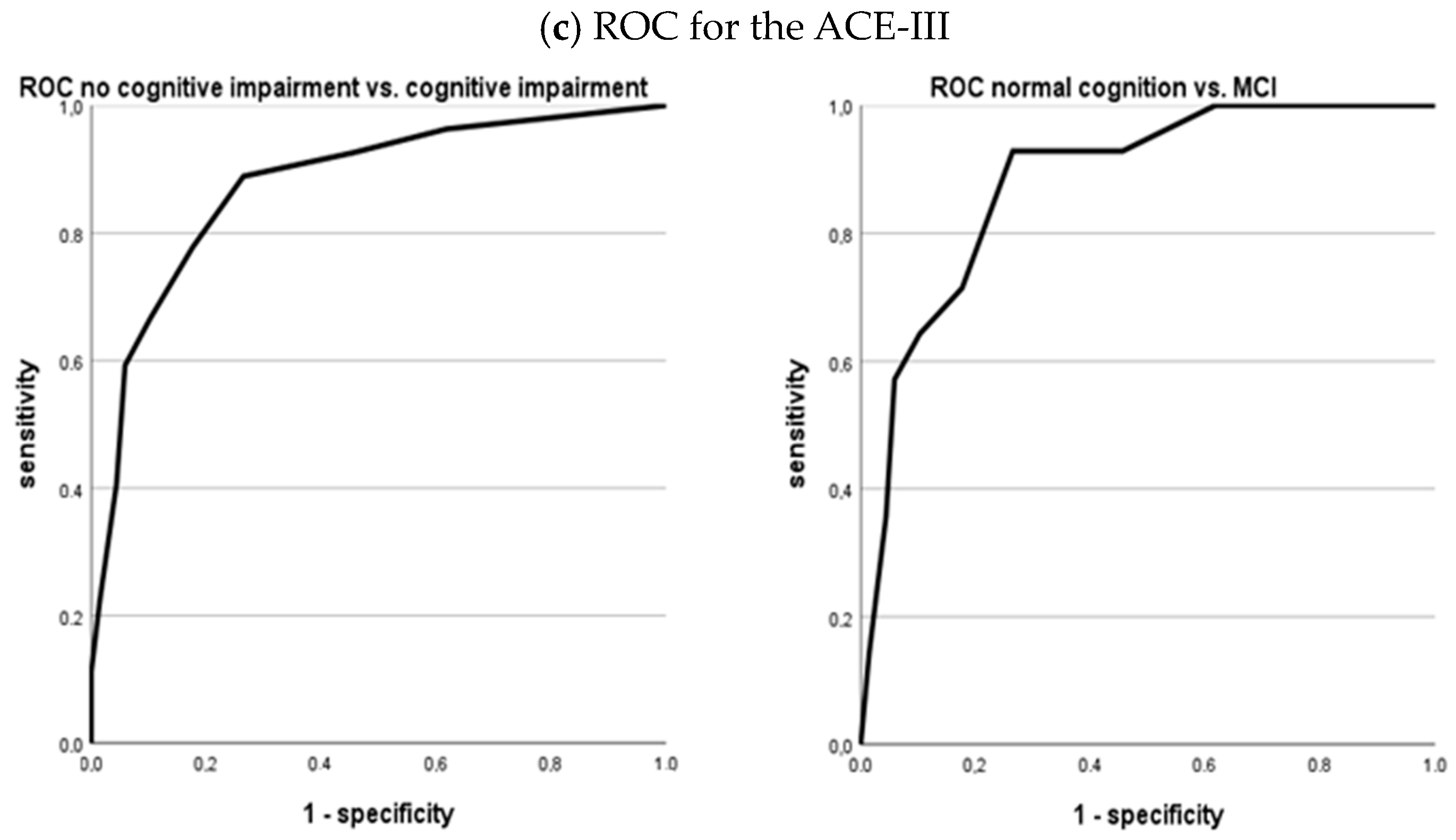
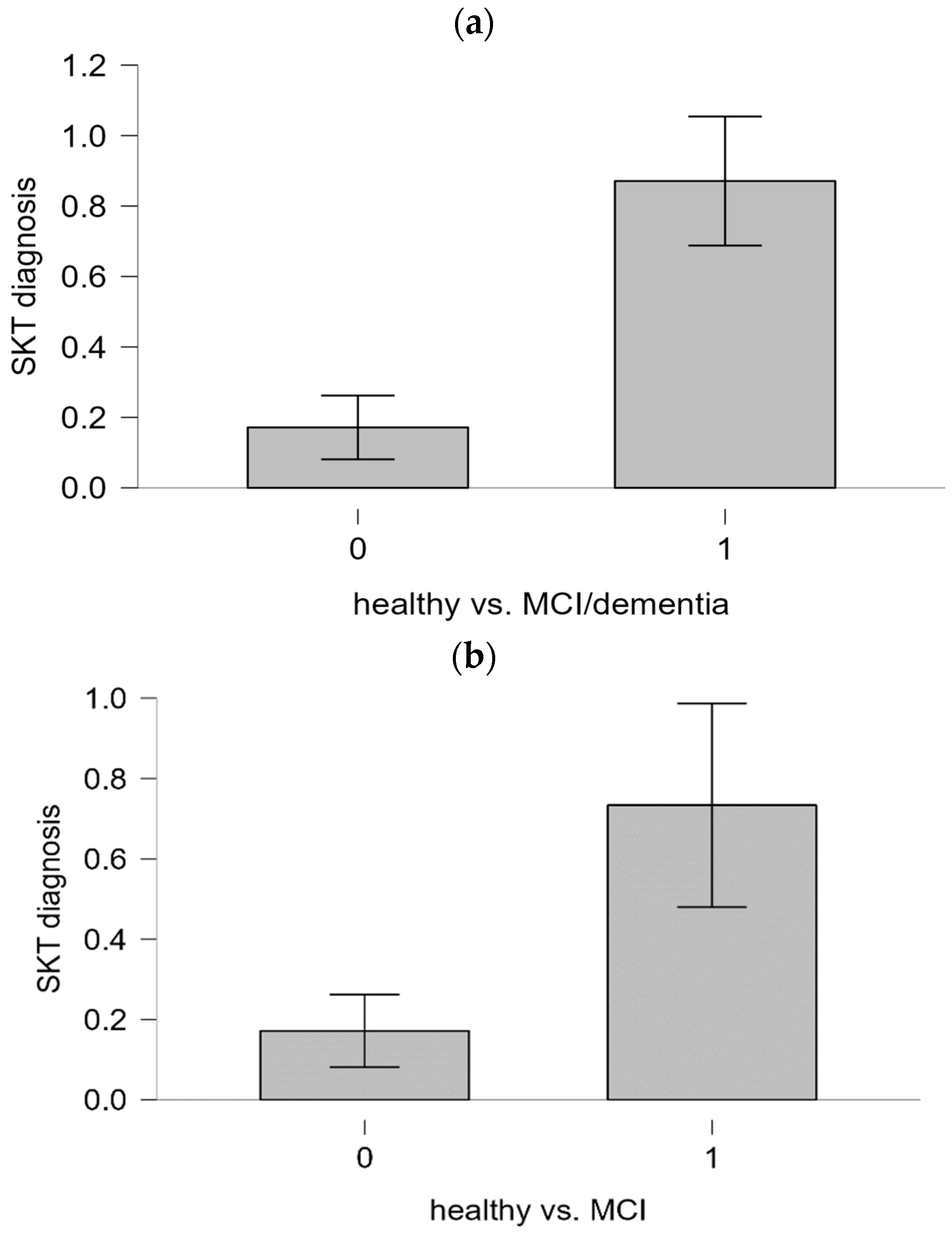
3.2. Diagnostic Congruency
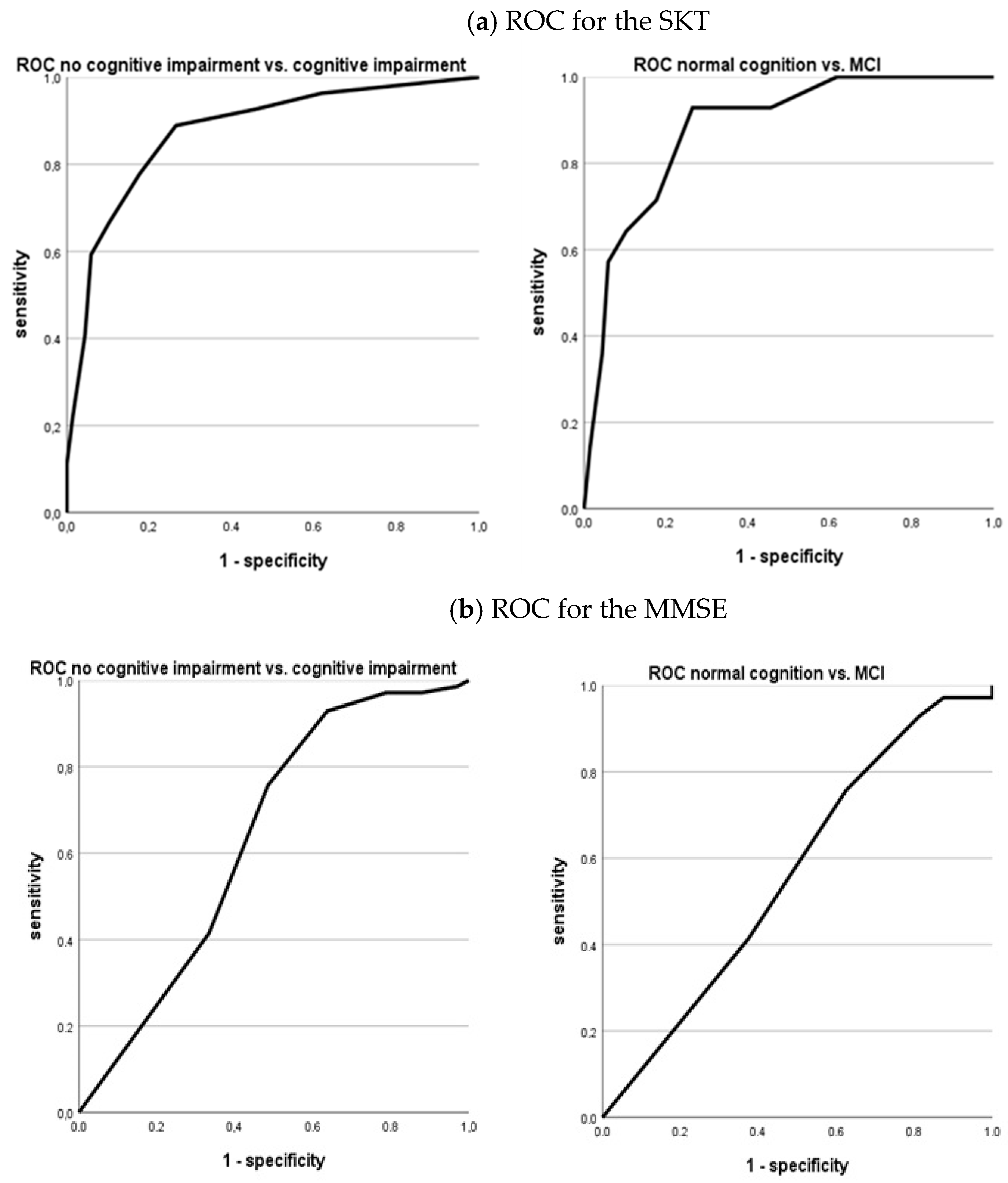
3.3. Sensitivity and Specificity
3.4. Concurrent Validity
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nichols, E.; Steinmetz, J.D.; Vollset, S.E.; Fukutaki, K.; Chalek, J.; Abd-Allah, F.; Abdoli, A.; Abualhasan, A.; Abu-Gharbieh, E.; Akram, T.T. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- Leifer, B.P. Early diagnosis of Alzheimer’s disease: Clinical and economic benefits. J. Am. Geriatr. Soc. 2003, 51, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Dubois, B.; Padovani, A.; Scheltens, P.; Rossi, A.; Dell’Agnello, G. Timely Diagnosis for Alzheimer’s Disease: A Literature Review on Benefits and Challenges. J. Alzheimer’s Dis. 2016, 49, 617–631. [Google Scholar] [CrossRef] [PubMed]
- Jeremic, D.; Navarro-López, J.D.; Jiménez-Díaz, L. Efficacy and safety of anti-amyloid-β monoclonal antibodies incurrent Alzheimer’s disease phase III clinical trials: A systematic review and interactive web app-based meta-analysis. Ageing Res. Rev. 2023, 90, 102012. [Google Scholar] [CrossRef] [PubMed]
- Sperling, R.A.; Donohue, M.C.; Raman, R.; Rafii, M.S.; Johnson, K.; Masters, C.L.; van Dyck, C.H.; Iwatsubo, T.; Marshall, G.A.; Yaari, R.; et al. Trial of Solanezumab in Preclinical Alzheimer’s Disease. N. Engl. J. Med. 2023, 389, 1096–1107. [Google Scholar] [CrossRef]
- van Dyck, C.H.; Swanson, C.J.; Aisen, P.; Bateman, R.J.; Chen, C.; Gee, M.; Iwatsubo, T. Lecanemab in early Alzheimer’s disease. N. Engl. J. Med. 2023, 388, 9–21. [Google Scholar] [CrossRef]
- Sims, J.R.; Zimmer, J.A.; Evans, C.D.; Lu, M.; Ardayfio, P.; Sparks, J.; Kaul, S. Donanemab in early symptomatic Alzheimer disease: The TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA 2023, 330, 512–527. [Google Scholar] [CrossRef]
- Noone, P. Addenbrooke’s cognitive examination-III. Occup. Med. 2015, 65, 418–420. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Matías-Guiu, J.A.; Valles-Salgado, M.; Rognoni, T.; Hamre-Gil, F.; Moreno-Ramos, T.; Matías-Guiu, J. Comparative diagnostic accuracy of the ACE-III, MIS, MMSE, MoCA, and RUDAS for screening of Alzheimer disease. Geriatr. Cogn. Disord. 2017, 43, 237–246. [Google Scholar] [CrossRef]
- Senda, M.; Terada, S.; Takenoshita, S.; Hayashi, S.; Yabe, M.; Imai, N.; Yamada, N. Diagnostic utility of the Addenbrooke’s Cognitive Examination–III (ACE-III), Mini-ACE, Mini-Mental State Examination, Montreal Cognitive Assessment, and Hasegawa Dementia Scale-Revised for detecting mild cognitive impairment and dementia. Psychogeriatrics 2020, 20, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, T.E.; Harvey, P.D.; Wesnes, K.A.; Snyder, P.J.; Schneider, L.S. Practice effects due to serial cognitive assessment: Implications for preclinical Alzheimer’s disease randomized controlled trials. Alzheimers Dement. 2015, 1, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Kvitting, A.S.; Fällman, K.; Wressle, E.; Marcusson, J. Age-Normative MMSE Data for Older Persons Aged 85 to 93 in a Longitudinal Swedish Cohort. J Am Geriatr Soc. 2019, 67, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Stemmler, M.; Lehfeld, H.; Erzigkeit, A. SKT. A Short Cognitive Performance Test according to Hellmut Erzigkeit. SKT English Manual Edition 2019; Geromed Publishing: Spardorf, Germany, 2019. [Google Scholar]
- Schneider, L.S. Rating Scales and Outcome Variables Used in Clinical Trials. In Alzheimer’s Disease: A Physician’s Guide to Practical Management; Richter, R.W., Richter, B.Z., Eds.; Humana Press: Totowa, NJ, USA, 2004; pp. 337–349. [Google Scholar]
- Kim, Y.S.; Nibbelink, D.W.; Overall, J.E. Factor structure and scoring of the SKT test battery. J. Clin. Psychol. 1993, 49, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Hessler, J.B.; Stemmler, M.; Horst, B. Cross-Validation of the Newly-Normed SKT for the Detection of MCI and Dementia. GeroPsych. 2017, 30, 19–25. [Google Scholar] [CrossRef]
- Fornazzari, L.; Cumsille, F.; Quevedo, F.; Quiroga, P.; Rioseco, P.; Klaasen, G.; Martinez, C.G.; Rhode, G.; Sacks, C.; Rivera, E.; et al. Spanish validation of the Syndrom Kurztest (SKT). Alzheimer Dis. Assoc. Disord. 2001, 15, 211–215. [Google Scholar] [CrossRef]
- Skjerve, A.; Nordhus, I.H.; Engedal, K.; Braekhus, A.; Nygaard, H.A.; Pallesen, S.; Haugen, P.K. Validation of the Seven Minute Screen and Syndrom Kurztest among elderly Norwegian outpatients. Int. Psychogeriatr. 2008, 20, 807–814. [Google Scholar] [CrossRef]
- Bruno, D.; Schurmann Vignaga, S. Addenbrooke’s cognitive examination III in the diagnosis of dementia: A critical review. Neuropsychiatr. Dis. Treat. 2019, 15, 441–447. [Google Scholar] [CrossRef]
- Crawford, J.R.; Garthwaite, P.H. Comparing patients’ predicted test scores from a regression equation with their obtained scores: A significance test and point estimate of abnormality with accompanying confidence limits. Neuropsychology 2006, 20, 259. [Google Scholar] [CrossRef]
- Urban, J.; Scherrer, V.; Strobel, A.; Preckel, F. Continuous norming approaches: A systematic review and real data example. Assessment 2024, 10731911241260545. [Google Scholar] [CrossRef]
- Stemmler, M.; Schneider, S.M.; Poon, L.W. The application of the skt short cognitive performance test to english-speaking populations. Psych 2021, 3, 717–727. [Google Scholar] [CrossRef]
- Sachdev, P.S.; Brodaty, H.; Reppermund, S.; Kochan, N.A.; Trollor, J.N.; Draper, B.; Slavin, M.J.; Crawford, J.; Kang, K.; Broe, G.A.; et al. The Sydney Memory and Ageing Study (MAS): Methodology and baseline medical and neuropsychiatric characteristics of an elderly epidemiological non-demented cohort of Australians aged 70–90 years. Int. Psychoger. 2010, 22, 1248–1264. [Google Scholar] [CrossRef] [PubMed]
- Winblad, B.; Palmer, K.; Kivipelto, M.; Jelic, V.; Fratiglioni, L.; Wahlund, L.O.; Petersen, R.C. Mild cognitive impairment–beyond controversies, towards a consensus: Report of the International Working Group on Mild Cognitive Impairment. J. Int. Med. 2004, 256, 240–246. [Google Scholar] [CrossRef]
- APA American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV; American Psychiatric Pub: Washington, DC, USA, 2000; Volume 4. [Google Scholar]
- APA American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub: Washington, DC, USA, 2013. [Google Scholar]
- Spreen, O.; Benton, A.L. Neurosensory Center Comprehensive Examination for Aphasia (NCCEA); University of Victoria: Victoria, BC, Canada, 1977. [Google Scholar]
- Wechsler, D.; Coalson, D.L.; Raiford, S.E. WAIS-IV Technical and Interpretive Manual; Pearson: Boston, MA, USA, 2008. [Google Scholar]
- Sattler, J.M.; Ryan, J.J. Assessment with the WAIS-IV; Jerome M Sattler Publisher: La Mesa, CA, USA, 2009. [Google Scholar]
- Hsieh, S.; Schubert, S.; Hoon, C.; Mioshi, E.; Hodges, J.R. Validation of the Addenbrooke’s Cognitive Examination III in frontotemporal dementia and Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 2013, 36, 242–250. [Google Scholar] [CrossRef]
- Ellison, J.M.; Harper, D.G.; Berlow, Y.; Zeranski, L. Beyond the “C” in MCI: Noncognitive symptoms in amnestic and non-amnestic mild cognitive impairment. CNS Spect. 2008, 13, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Salthouse, T.A. The processing-speed theory of adult age differences in cognition. Psychol. Rev. 1996, 103, 403. [Google Scholar] [CrossRef]
- Lu, Y.; Hu, J.; Stemmler, M.; Guo, Q. Validation of Chinese version of SKT (Syndrom Kurztest): A short cognitive performance test for the assessment of memory and attention. Diagnostics 2021, 11, 2253. [Google Scholar] [CrossRef]
- Stemmler, M.; Lehfeld, H.; Siebert, J.; Horn, R. Ein kurzer Leistungstest zur Erfassung von Störungen des Gedächtnisses und der Aufmerksamkeit: SKT Manual Edition 2015–und der regressionsbasierte Ansatz [A brief performance test to assess impairment of memory and attention: SKT Manual Edition 2015-and the regression-based approach]. Diagnostica 2017, 63, 243–255. [Google Scholar]
- Kochhann, R.; Varela, J.S.; Lisboa, C.S.D.M.; Chaves, M.L.F. The Mini Mental State Examination: Review of cutoff points adjusted for schooling in a large Southern Brazilian sample. Dement. Neuropsychol. 2010, 4, 35–41. [Google Scholar] [CrossRef]
- Bartos, A.; Raisova, M. The Mini-Mental State Examination: Czech norms and cutoffs for mild dementia and mild cognitive impairment due to Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 2016, 42, 50–57. [Google Scholar] [CrossRef]
- Matías-Guiu, J.A.; Fernández-Bobadilla, R.; Fernández-Oliveira, A.; Valles-Salgado, M.; Rognoni, T.; Cortés-Martínez, A.; Matías-Guiu, J. Normative data for the Spanish version of the Addenbrooke’s Cognitive Examination III. Dement. Geriatr. Cogn. Disord. 2016, 41, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.J.; Sattler, J.M.; Lopez, S.J. Age effects on Wechsler Adult Intelligence Scale-III subtests. Arch. Clin. Neuropsychol. 2000, 15, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Tombaugh, T.N.; Kozak, J.; Rees, L. Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Arch. Clin. Neuropsychol. 1999, 14, 167–177. [Google Scholar] [PubMed]
| Wave 6 | Wave 7 | Total Number of Persons Used for Calculations | |
|---|---|---|---|
| Consensus Diagnosis | 33 | 78 | 111 |
| SKT | 34 | 106 | 140 |
| MMSE | 142 | 109 | 143 |
| ACE-III | 142 | 0 | 142 |
| N | Min | Max | Mean | SD | |
|---|---|---|---|---|---|
| Age | 143 | 83 | 98 | 87.73 | 3.54 |
| Sex * | 143 | 0 | 1 | 0.63 | 0.49 |
| Years of Education | 143 | 6 | 24 | 12.63 | 3.46 |
| Digital Symbol Coding | 137 | 12 | 78 | 42.14 | 12.22 |
| F-A-S Test | 139 | 12 | 71 | 37.78 | 12.86 |
| SKT | 139 | 0 | 11 | 2.99 | 2.84 |
| ACE-III | 142 | 63 | 100 | 89.58 | 5.96 |
| MMSE | 143 | 24 | 30 | 28.87 | 1.41 |
| SKT | Green (No Cognitive Impairment) N (%) | Yellow (MCI) N (%) | Red (Suspected Dementia) N (%) | ||
|---|---|---|---|---|---|
| Consensus Diagnosis | |||||
| No cognitive impairment | 58 (82.9) | 12 (17.1) | 0 (0) | 70 | |
| MCI | 4 (26.7) | 11 (73.3) | 0 (0) | 15 | |
| Dementia | 2 (12.5) | 12 (75) | 2 (12.5) | 16 | |
| Total | 64 | 35 | 2 | 101 | |
| Sensitivity | Specificity | Area under the Curve | ||
|---|---|---|---|---|
| SKT | no cognitive impairment vs. cognitive impairment | 80.6 | 82.9 | 87.5 |
| normal cognition vs. MCI | 73.3 | 82.9 | 88 | |
| MMSE | no cognitive impairment vs. cognitive impairment | 21.2 | 97.1 | 63.7 |
| normal cognition vs. MCI | 12.5 | 98.6 | 56.3 | |
| ACE-III | no cognitive impairment vs. cognitive impairment | 70 | 84.1 | 83 |
| normal cognition vs. MCI | 72.7 | 86.6 | 83.7 |
| Consensus Diagnosis | SKT | MMSE | |
|---|---|---|---|
| SKT | 0.60 ** | ||
| MMSE | 0.32 ** | −0.24 ** | |
| ACE-III | 0.54 ** | −0.32 ** | 0.34 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stemmler, M.; Arnold, M.; Numbers, K.; Kochan, N.A.; Sachdev, P.S.; Brodaty, H. The Usefulness of the Regression-Based Normed SKT Short Cognitive Performance Test in Detecting Cognitive Impairment in a Community Sample. Diagnostics 2024, 14, 2199. https://doi.org/10.3390/diagnostics14192199
Stemmler M, Arnold M, Numbers K, Kochan NA, Sachdev PS, Brodaty H. The Usefulness of the Regression-Based Normed SKT Short Cognitive Performance Test in Detecting Cognitive Impairment in a Community Sample. Diagnostics. 2024; 14(19):2199. https://doi.org/10.3390/diagnostics14192199
Chicago/Turabian StyleStemmler, Mark, Melina Arnold, Katya Numbers, Nicole A. Kochan, Perminder S. Sachdev, and Henry Brodaty. 2024. "The Usefulness of the Regression-Based Normed SKT Short Cognitive Performance Test in Detecting Cognitive Impairment in a Community Sample" Diagnostics 14, no. 19: 2199. https://doi.org/10.3390/diagnostics14192199
APA StyleStemmler, M., Arnold, M., Numbers, K., Kochan, N. A., Sachdev, P. S., & Brodaty, H. (2024). The Usefulness of the Regression-Based Normed SKT Short Cognitive Performance Test in Detecting Cognitive Impairment in a Community Sample. Diagnostics, 14(19), 2199. https://doi.org/10.3390/diagnostics14192199






