Abstract
Cervical cancer related to high-risk human papillomavirus (HR-HPV) is the second female cancer in Mauritania (Northwest Sahelian Africa). We assessed the distribution of HPV genotypes in Mauritanian women with high-grade cervical intraepithelial neoplasia (CIN2/3) or invasive cervical cancer (ICC). A prospective study was conducted in the Centre Hospitalier National, Nouakchott, Mauritania, to collect cervical biopsies among women suspected of CIN2/3 or cancer. HPV DNA detection and genotyping were carried out from formalin-fixed, paraffin-embedded biopsies using multiplex PCR (Human Papillomavirus Genotyping Real-Time PCR Kit, Bioperfectus Technologies Co., Taizhou, China). Fifty biopsies were included from women (mean age: 56.7 years) suffering from CIN2/3 (28.0%) and ICC (72.0%) which corresponded to 32 (64.0%) squamous cell carcinomas (SCC) and 4 (8.0%) adenocarcinomas (ADC). HPV DNA detection was successful in 47 (94.0%) samples. The most prevalent HR-HPV genotypes were HPV-45 (40.4%), HPV-16 (38.3%), HPV-39 and HPV-52 (23.4%), HPV-33 (17.0%), HPV-18 (14.9%), HPV-35 (4.2%), and HPV-56 (2.1%). The majority (93.6%) of HPV-positive biopsies contained at least one HPV type covered by the 9-valent Gardasil-9® vaccine, and 40.9% were infected by multiple vaccine HPV genotypes. To eradicate cervical cancer in Mauritania, prophylactic HPV vaccination must be combined with primary molecular screening of cervical HR-HPV infection.
1. Introduction
More than 170 human papillomavirus (HPV) genotypes have been identified [1]. Thirteen types are recognized as high-risk HPV (HR-HPV) and involved in HPV-associated cancers: HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, and -68 [2]. It is widely recognized that persistent HR-HPV infections are causally associated with anogenital cancers (particularly cervical cancer) [3,4,5]. Together, HPV-16 and HPV-18 cause about 70% of cervical cancers worldwide [5,6]. On the other hand, low-risk HPV causes benign pathologies, and HPV-6 and HPV-11 are responsible for about 90% of genital warts worldwide [7].
According to the World Health Organization (WHO), about 660,000 new cases of cervical cancer and 350,000 deaths were reported in 2022, making cervical cancer the ninth deadly female cancer worldwide [8]. Cervical cancer is the second most common cancer for women in developing countries and the second leading cause of cancer-related deaths in sub-Saharan Africa [8,9,10,11,12,13,14]. The estimates for Africa show that 125,699 new cases of cervical cancer (new cancers incidence rate of 18.5% in African women) and 80,614 associated deaths were recorded in 2022 [15]. Cervical cancer-associated mortality in sub-Saharan Africa is up to 10 times higher than in most European countries [9,15,16].
Knowledge of HPV prevalence and HR-HPV genotypes distribution is essential for the implementation of effective prophylactic vaccination programs and appropriate epidemiological monitoring of viral ecology before and after vaccination in specific populations and areas in sub-Saharan Africa [9,17,18,19]. Since the last decade, epidemiological studies have been conducted in several sub-Saharan African countries, showing high heterogeneity in the geographical distribution of the carcinogenic genotypes [9,20,21,22,23,24,25]. For example, adjusted HPV prevalences among sub-Saharan African women were estimated at 33.6%, 19.6%, and 17.4% in Eastern, Western, and Southern Africa, respectively [6].
The epidemiology of HPV infection remains poorly documented in Mauritania [14,24,25,26,27], a country located in northwest Africa with around 5 million inhabitants, one-third being women aged more than 15 years (Figure 1). According to the WHO, with an incidence rate of 14.3% (468 new cases) and a mortality rate of 13.5% (302 deaths) in 2022, cervical cancer ranks as both the 2nd most frequent and most deadly female cancer in Mauritania [14,24,25,26,27]. The estimated age-adjusted death rate associated with cervical cancer is 27.4 per 100,000 Mauritanian women, placing Mauritania at the 20th rank in terms of cervical cancer mortality in the world [28]. Despite this high burden of cervical cancer, molecular epidemiology of circulating HPV genotypes in Mauritania has not yet been reported. Nevertheless, in western Africa, the region Mauritania belongs to, the HPV-related disease burden is high. For instance, in Senegal, a neighboring country, 23.2% of adult women in the general population are estimated to harbor cervical HR-HPV infection [29], and 57.2% [30] to 71.3% [31] of invasive cervical cancers (ICC) are attributed to HPV-16 or HPV-18. Cervical cancer screening and vaccine coverage in Mauritania is currently limited. Prophylactic HPV vaccine is yet available, but the national prevention program has only begun in 2021 [14,24].
Figure 1.
Geographical map of Mauritania. Mauritania, officially the Islamic Republic of Mauritania, is a sovereign country in northwest Africa. It is bordered by the Atlantic Ocean to the West, western Sahara to the north and the northwest, Algeria to the northeast, Mali to the east and the southeast, and Senegal to the southwest. Mauritania is the 11th largest country in Africa, and 90% of its territory is situated in the Sahara Desert. Most of its population of 4.73 million inhabitants live in the temperate south of the country, with roughly one-third concentrated in the capital and largest city, Nouakchott, located on the Atlantic coast. All study participants were included in the Centre Hospitalier National in Nouakchott.
We herein conducted a prospective, descriptive study on HPV genotypes distribution in women suffering from high-grade cervical intraepithelial neoplasia (CIN2/3) or ICC. The aim of this study was to assess the HPV epidemiology and the predictive effectiveness of prophylactic HPV vaccination in Mauritania.
2. Materials and Methods
2.1. Study Design and Participants
A mono-center, descriptive, prospective, population-based study was conducted between 2022 and 2023, in the Centre Hospitalier National, Nouakchott, Mauritania. Over a 12-month period, all adult (≥18-year-old) women followed for suspected high-grade lesions or cervical cancers were recruited after informed consent. Patients with a history of total uterine or cervical resection and those with a history of chemotherapy were excluded. Socio-demographic characteristics including age, educational level, gravidity, parity, menopause, clinical data, and previous HPV screening and vaccination were collected from each patient.
2.2. Collection of Biopsy Samples and Processing
Cervical biopsies were performed before treatment for CIN2/3 and ICC through colposcopic examination for histological analysis at the pathology laboratory of the Centre Hospitalier National. The biopsies were fixed in formalin 10% overnight and included in paraffin. The formalin-fixed, paraffin-embedded (FFPE) blocks were further processed using standard histopathological methods and evaluated by a certified pathologist. Histological sections were stained with hematoxylin and eosin (H&E) to identify areas containing abnormal cells. Women diagnosed histologically with either CIN2/3, adenocarcinoma (ADC), or squamous cell carcinoma (SCC) were included in this study. The histopathological examination assessed the representativeness of the biological specimen by evaluating the tumor cellularity with the percentage of tumor cells. The virological analysis was performed accordingly by choosing the most representative inclusion blocks. Depending on the size of the biopsy, five to seven sections of 5–20 µm thick were cut from each FFPE block, placed on a slide for molecular investigations, and sent to the virology laboratory of the Georges Pompidou European Hospital, Paris, France. The patients were staged according to the International Federation of Gynecology and Obstetrics (FIGO) staging system 2009 [32].
2.3. DNA Extraction
Sections of FFPE biopsy samples were deparaffinized overnight at +56 °C with 40 µL of proteinase K (Qiagen, Hilden, Germany) and 360 µL of ATL buffer (Qiagen). Afterwards, 200 µL of ATL buffer was added and incubated for 10 min at +70 °C. DNA was further extracted using QIAamp® DNA Mini Kit (Qiagen) according to manufacturer’s instructions and eluted in 100 µL of the kit elution buffer before genotyping. Extracted DNA was stored at −20 °C until analysis.
DNA was quantified using a Qubit® dsDNA BR Assay kit with the Qubit 2.0 fluorimeter (Thermo Fisher Scientific Inc., Waltham, MA, USA).
2.4. HPV Detection and Genotyping by Multiplex PCR
HPV detection and genotyping was carried out using the fluorescence-based Bioperfectus Multiplex Real-Time (BMRT) Human Papillomavirus Genotyping Real-Time PCR Kit (Jiangsu Bioperfectus Technologies Co., Ltd., Taizhou, Jiangsu Province, China). The BMRT HPV kit contains primers and corresponding TaqMan probes that amplify a 100-base pairs L1 amplicon, as previously described [33]. According to the HPV classification nomenclature provided by the International Agency for Research on Cancer (IARC) [2], the BMRT HPV Genotyping Real-Time PCR Kit allows to distinguish each of the 21 most prevalent HPV genotypes, including 13 HR-HPV (HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, and -68), 5 possibly oncogenic HPV (HPV-26, -53, -66, -73, and -82), and 3 LR-HPV (HPV-6, -11, and -81). The BMRT HPV kit was used according to the manufacturer’s instructions. Briefly, eight reactions per sample were performed simultaneously. Among them, the reactions A, B, C, D, E, F, and G were prepared to detect and differentiate in FAM™/ VIC® (HEX)/ROX™ fluorescent channels, HPV-16/-18/-31, HPV-59/-66/-53, HPV-33/-58/-45, HPV-56/-52/-35, HPV-68/-51/-39, HPV-73/-26/-82, and HPV-6/-11/-81, respectively. In addition, an internal control (IC) with the housekeeping single-copy gene encoding human DNA topoisomerase III (TOP3) [34], in reaction tube H (FAM™ channel), was set to identify possible PCR inhibition and to confirm the reliability of the reagents in this kit.
PCR amplification was conducted using 96-well reaction plate, in a total reaction volume of 20 μL per well, which comprised 2 μL DNA samples (up to 50 ng), 10 μL of PCR mix containing dUTP instead of dTTP and Uracil-DNA-Glycosylase (UDG), and 8 μL of reaction mix A, B, C, D, E, or F, containing 10 pmol of each primer and 1–5 pmol of each probe (FAM™, VIC®, and ROX™ dye). Positive and blank controls were also included in each specimen PCR detection. The reaction plates were sealed with a suitable plastic sheet, centrifuged for 30 s at approximately 2000 revolutions per minute, and subjected to a final PCR amplification. To prevent reamplification of carry-over PCR products, all reactions with UDG were pre-incubated at 50 °C for 5 min, followed by an initial denaturation at 95 °C for 10 min, which also inactivates UDG but activates the DNA polymerase, and 45 cycles at 95 °C for 10 s, 58 °C for 40 s. PCR was performed on the CFX96 real-time PCR instrument (Bio-Rad, Marnes-la-Coquette, France).
The emitted fluorescence was measured by the optical unit of the real-time PCR system. To validate the PCR reaction, the cycle threshold (Ct) values of positive controls had to be less than or equal to the cut-off value of 30.0 in FAM™, VIC® (HEX), and ROX™, and the blank controls had to be undetectable. For each of the 21 detected HPV genotypes, the qualitative reference values of positive cut-off were assessed by the manufacturer using ROC curves based on clinical trial results. Specimens with Ct values less than or equal to the cut-off value of one given HPV type were considered as positive for this HPV genotype. Conversely, specimens with Ct values above the cut-off value of one given HPV type were considered negative. Specimens with Ct values of the internal TOP3 channel above the cut-off value of 30.0 were considered invalid.
The virology laboratory was accredited in 2013 by the Comité Français d’Accréditation (COFRAC) according to the ISO 15189 Norma for the biological markers of specialized molecular medical virology (markers “VIROH”).
2.5. Statistical Analysis
Statistical analysis was performed using GraphPad Prism version 8.4.2 (GraphPad Software, Inc., San Diego, CA, USA). Means and standard deviations (SD) were calculated for quantitative variables and proportions for categorical variables. The results were presented along with their 95% confidence interval (CI). Pearson’s χ2 or Fisher’s exact tests were used for categorical variables and the non-parametric Mann–Whitney U-test or Kruskal–Wallis’ rank sum test for quantitative variables. Logistic regression models using univariate and multivariate analyses were performed to determine the association of independent variables with HPV type-specific cervical infections (i.e., genital infection with any HPV type and HR-HPV), high-grade lesions and cervical cancer. All statistically significant variables (p < 0.05) in the univariate analysis were calculated in a multivariate logistic regression analysis. The crude odds ratio (cOR) and adjusted odds ratio (aOR) were calculated, where appropriate, along with their 95% CI. Finally, a risk factor was defined as an independent variable yielding in the univariate analysis a cOR strictly greater than “1” with a p-value less than 0.05. An aOR strictly greater than “1” with a p value less than 0.05 defined a risk factor in multivariate analysis.
3. Results
3.1. Study Population
Out of 85 women enrolled, 68 biopsies were performed in women with CIN or ICC. Biopsies for which socio-demographic information were not precisely known or with insufficient FFPE biopsy material were excluded. Finally, a total of 50 biopsies samples were used in this study. Table 1 presents the socio-demographic characteristics of the study women, the histological diagnosis of cervical lesions, and the distribution of HPV genotypes in cervical biopsy samples.

Table 1.
Socio-demographic characteristics, histological diagnosis of cervical lesions, and distribution of HPV types in the study’s 50 adult women suffering from cervical intraepithelial neoplasia or invasive cervical cancer, and living in the urban setting of Nouakchott, the capital city of Mauritania.
All women lived in the urban setting of Nouakchott. The mean age of the study population was 56.7 years (range, 35 to 73 years). Most women (40.0%) were aged 60–69 years and the second most frequent age group (26.0%) was women aged 50–59 years. Most participants were engaged in a life couple with a male partner (80.0%), with a low education level (78%), and half of them (48%) had never been to school. All women were multiparous, with a mean number of four children (range, 2 to 6). The majority of them were postmenopausal (84.0%). Only a minority (18.0%) of study women had previously received HPV cervical screening, mainly those diagnosed with CIN2/3 (26.4%). Note that none of the study’s women had ever received prophylactic HPV vaccination and none of them were infected with HIV.
The histological analysis identified 14 (28.0%) CIN2/3 and 36 (72.0%) ICC, including 4 (8.0%) ADC and 32 (64.0%) SCC. Clinical stages I and II were mostly represented with 28.0% and 24.0% of cases, respectively, while extensive cancer (stages III and IV) could be observed in only 1 case out of 5.
3.2. Overall Prevalence of HPV and HPV Genotypes Distribution
Molecular detection of the TOP3 gene used as an internal control was conclusive for all samples. A total of 85 interpretable HPV-positive results were detected by the BMRT HPV Genotyping Real-Time PCR Kit in 47 biopsies (94.0%), including 42.5% (n = 20) of single HPV genotype infection and 57.5% (n = 27) of multiple HPV genotypes infection. Multiple HPV infections were observed in 58.3% of CIN2/3 (7/12), 75.0% of ADC (3/4), and 61.2% of SCC (19/31), without statistical differences in this limited series (p = 0.83). The mean number (range) of HPV genotypes detected per sample was 1.58 (1–2) for CIN2/3, 1.75 (1–3) for ADC, and 2.06 (1–4) for SCC, without significant difference between the three categories (p = 0.37). A total of 90.6% (77/85) and 3.5% (3/85) of HPV-positive results corresponded to HR-HPV and possibly oncogenic HPV genotypes, respectively, whereas 5.9% (5/85) corresponded to LR-HPV, exclusively HPV-81.
Regarding HPV molecular typing, eleven different genotypes were identified in the 47 biopsy samples (Table 1). The most prevalent HR-HPV genotypes were HPV-45 (n = 19; 40.4%), HPV-16 (n = 18; 38.3%), HPV-39 and HPV-52 (n = 11; 23.4%), HPV-33 (n = 8; 17.0%), HPV-18 (n = 7; 14.9%), HPV-35 (n = 2; 4.2%), and HPV-56 (n = 1; 2.1%). Two possibly carcinogenic HPV genotypes were identified, HPV-73 (n = 2; 4.2%) and HPV-53 (n = 1; 2.1%). Finally, the only LR-HPV was HPV-81 (n = 5; 10.6%).
Analysis of the different genotypes according to histology is depicted in Figure 2. The most frequent HR-HPV in CIN2/3 were HPV-45 (n = 5; 41.7%), HPV-16 (n = 4; 33.3%), HPV-39 (n = 3; 25.0%), HPV-33,HPV-52 and HPV-81 (n = 2; 16.6%) and HPV-18 (n = 1; 8.3%); in ADC, HPV-16 (n = 3; 75.0%) followed by HPV-18, HPV-33, HPV-39, HPV-45, and HPV-52 (n = 1; 25.5%); and in SCC, HPV-45 (n = 13; 41.9%), HPV-16 (n = 11; 35.5%), HPV-39 (n = 7; 22.6%), HPV-18 and HPV-33 (n = 5; 16.1%), HPV-81 (n = 3;9.7%), HPV-35 and HPV-73 (n = 2; 6.4%), and HPV-53 and HPV-56 (n = 1; 3.2%). The proportions of the detected HR-HPV genotypes were not different between the respective histological types.
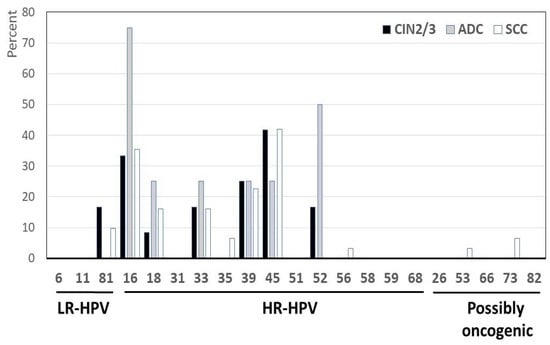
Figure 2.
Distribution of HPV types by histology. The samples were classified as high-grade cervical intraepithelial neoplasia (CIN2/3) or invasive cervical cancer, including adenocarcinoma (ADC) or squamous cell carcinoma (SCC). Nota bene: According to the manufacturer’s instructions and in accordance with the HPV classification nomenclature provided by the International Agency for Research on Cancer, the BMRT HPV Genotyping Real-Time PCR Kit distinguishes 21 HPV genotypes, including 14 genotypes (HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, -66, and -68), 3 LR-HPV types (HPV-6, -11, and -81), and 4 genotypes classified as possibly oncogenic (HPV-26, -53, -73, and -82).
3.3. Possible Efficiencies of Cervical HPV Prevention by Gardasil® Vaccines
The potential efficacy of cervical HPV prevention with Gardasil-4® and Gardasil-9® vaccines was further assessed according to the cervical HPV genotypes detected.
Overall, 48.0% (24/50) and 88.0% (44/50) of cervical biopsy samples showed at least one 4-valent and 9-valent HPV vaccine genotype, respectively (Table 1).
Less than 30% (24/85; 28.2%) of the HPV-positive results corresponded to one of the four genotypes covered by the Gardasil-4® vaccine, and none (0.0%) of the cervical biopsy samples contained simultaneously several of these 4-valent vaccine genotypes.
The distribution of cervical HPV genotypes according to their inclusion in the 9-valent vaccine is depicted in the Figure 3. For the Gardasil-9® vaccine, 74.1% (63/85) of HPV-positive results corresponded to one HPV type prevented by the 9-valent vaccine (HPV-6, -11, -16, -18, -31, -33, -45, -52, and -58). In addition, 93.6% (44/47) of HPV-positive cervical biopsy samples harbored at least one HR-HPV genotype covered by the Gardasil-9® vaccine, with the majority (26/44; 59.1%) being infected by only one of the 9-valent vaccine HPV genotypes. Moreover, 40.9% (18/44) of these biopsies harbored multiple 9-valent vaccine HPV genotypes simultaneously, including the couples HPV-16 and HPV-45 (n = 4), HPV-33 and HPV-45 (n = 3), HPV-45 and HPV-52 (n = 3), HPV-16 and HPV-33 (n = 2), HPV-18 and HPV-45 (n = 2), HPV-16 and HPV-52 (n = 1), HPV-18 and HPV-52 (n = 1), HPV-33 and HPV-58 (n = 1), and one biopsy infected with three-vaccine HPV (HPV-16, HPV-45, and HPV-52). Finally, HPV-45 (19/47; 40.4%) and HPV-16 (18/47; 38.9%) were the predominant Gardasil-9® vaccine genotypes, followed by HPV-52 (11/47; 23.4%), HPV-33 (8/47; 17.0%), and HPV-18 (7/47; 14.9%). The Gardasil-9® vaccine HR-HPV types 31 and 58 as well as the LR-HPV types 6 and 11 were not observed.
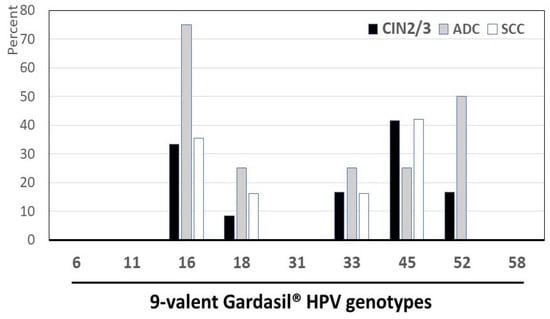
Figure 3.
Distribution of HPV genotypes according to their inclusion in the 9-valent Gardasil-9® vaccine: Percentage of low-risk (LR), high-risk (HR), and possibly carcinogenic HPV genotypes in 47 cervical samples positive for HPV DNA by molecular biology according to their possible prevention by Gardasil-9® vaccine among adult women living in Mauritania. Nota bene: The 9-valent Gardasil-9® vaccine (Merck & Co. Inc., Rahway, NJ, USA) targets the seven HR-HPV genotypes predominantly isolated in cervical cancer (HPV-16, -18, -31, -33, -45, -52, and -58) and two LR-HPV (HPV-6 and HPV-11).
A total of 25.9% (22/85) of HPV-positive results corresponded to HPV genotypes not covered by the Gardasil-9® vaccine, including HPV-39 (11/47; 23.4%), HPV-81 (5/47; 10.6%), HPV-35 (2/47; 4.2%), HPV-73 (2/47; 4.2%), HPV-53 (1/47; 2.1%), and HPV-56 (1/47; 2.1%). Therefore, the majority of nonvaccine types were HR-HPV (14/22; 63.6%) (Figure 4). Thus, among all detected HR-HPV types, HPV-39, HPV-35, and HPV-56, representing 16.5% (14/85) of HPV-positive results, were not targeted by the Gardasil-9® vaccine. In other terms, the majority (5/8; 62.5%) of the eight detected HR-HPV genotypes were covered by the 9-valent HPV vaccine, while the remaining (37.5%) corresponded to nonvaccine types. Finally, nonvaccine HR-HPV detected in biopsy samples were frequently co-infected with vaccine-targeted HR-HPV in 64.3% (9/14).
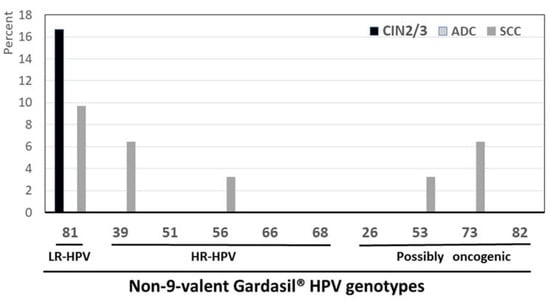
Figure 4.
Percentage of low-risk (LR), high-risk (HR), and possibly carcinogenic HPV genotypes in 47 cervical biopsies samples from adult women living in Mauritania, positive for HPV DNA not targeted by the 9-valent Gardasil-9® vaccine by using the BMRT HPV Genotyping Real-Time PCR Kit. Nota bene: The 9-valent Gardasil-9® vaccine (Merck & Co. Inc., Rahway, NJ, USA) targets the seven HR-HPV genotypes predominantly isolated in cervical cancer (HPV-16, -18, -31, -33, -45, -52, and -58) and two LR-HPV (HPV-6 and HPV-11).
3.4. Determinants of HPV Outcomes and High-Grade Cervical Lesions and Invasive Carcinoma Using Logistic Regression Analyses
To identify factors that determine the HPV infection profile and the occurrence of high-grade cervical lesions and invasive cervical carcinoma among these Mauritanian women, sociodemographic and clinical characteristics of the participants and the distribution of HPV genotypes were calculated in simple and multivariate logistic regression analyses. The results are presented in Table 2, Table 3 and Table 4.

Table 2.
Risk factors associated with HPV outcomes using simple logistic regression analysis in 50 adult women living in Nouakchott, Mauritania.

Table 3.
Risk factors associated with HPV outcomes using multivariate logistic regression analysis in 50 adult women living in Nouakchott, Mauritania.

Table 4.
Risk factors associated with high-grade cervical lesions and invasive cervical carcinoma using simple and multivariate logistic regression analysis.
3.4.1. Simple Logistic Regression Analysis
Older women, particularly those aged 60–69 years old, had increased likelihood of being infected with several HR-HPV genotypes (cOR: 3.21, 95% CI: 1.01–10.95, p = 0.048), especially those high-risk genotypes targeted by the Gardasil-9® vaccine (cOR: 4.02, 95% CI: 1.22–14.30, p = 0.022) (Table 2). On the other hand, these women aged 60–69 years old showed a reduced risk of having CIN2/3 cervical lesions (cOR: 0.16, 95% CI: 0.03–0.72, p = 0.015) (Table 4). In addition, having stopped schooling at high-school level was associated with an increased risk of being both infected with possibly oncogenic HPV genotypes (cOR: 7.8, 95% CI: 1.18–54.18, p = 0.034) as well as harboring CIN2/3 lesions (cOR: 6.11, 95% CI: 1.26–34.78, p = 0.024) (Table 2 and Table 4). Regarding the childbearing status of the women, while having had at least six pregnancies was associated with a reduced risk of being infected with nonvaccine HR-HPV genotypes (cOR: 0.154, 95% CI: 0.01–0.92, p = 0.038), having had up to three pregnancies was associated with an increased likelihood of harboring CIN2/3 lesions (cOR: 6.8, 95% CI: 1.15–54.58, p = 0.034), (Table 2 and Table 4). In addition, having given birth up to four times was significantly associated with an increased risk of being infected with several HR-HPV genotypes (cOR: 4.09, 95% CI: 1.26–14.55, p = 0.017) (Table 2). Concerning the impact of the stages of the cervical lesions and cancer, the FIGO stages IA/B were associated with a reduced risk of being infected with either several HPV genotypes (cOR: 0.136, 95% CI: 0.03–0.53, p = 0.003), several HR-HPV genotypes (cOR: 0.195, 95% CI: 0.04–0.75, p = 0.016), or several high-risk genotypes targeted by the Gardasil-9® vaccine (cOR: 0.208, 95% CI: 0.03–0.91, p = 0.036) (Table 2). Interestingly, while women exhibiting FIGO stages IA/B had an increased likelihood of harboring a cervical ADC (cOR: 9.54, 95% CI: 1.09–204.2, p = 0.041), those exhibiting neoplasia with FIGO stages IIA/B were more likely to have cervical squamous cell carcinoma (cOR: 8.91, 95% CI: 1.5–171.0, p = 0.013) (Table 4). On the other hand, women having neoplasia with FIGO stages IIIA/B were more likely to carry HR-HPV genotypes targeted by the Gardasil® vaccine (cOR: 9.33, 95% CI: 1.47–182.6, p = 0.015) (Table 2). Women who reported having had previous HPV screening had higher likelihood of harboring CIN2/3 lesions (cOR: 8.25, 95% CI: 1.79–46.46, p = 0.006), while showing a reduced risk of harboring SCC (cOR: 0.21, 95% CI: 0.04–0.92, p = 0.037) (Table 4). The younger age, marital status, and the clinical symptoms did not show any association with any of the HPV outcomes and cervical high-grade lesions and cancers in the simple logistic regression analyses. Likewise, the HPV genotypes distribution did not show any association with either CIN2/3 lesions, SCC or ADC.
3.4.2. Multivariate Logistic Regression Analysis
Only the independent variables with a statistically significant association (p < 0.05) in the simple logistic regression analysis were computed in the multivariate logistic regression (Table 3 and Table 4). Women aged 60–69 years old had an increased risk of being infected with HR-HPV genotypes targeted by the Gardasil-9® vaccine (aOR: 4.25, 95% CI: 1.17–15.42, p = 0.028). Likewise, those who had stopped schooling at high-school level were more at risk of being infected with possibly oncogenic HPV genotypes (aOR: 7.8, 95% CI: 1.22–49.67, p = 0.03) (Table 3). In addition, women who reported having given birth up to four times had a significant increased risk of being infected with several HR-HPV genotypes (aOR: 4.22, 95% CI: 1.10–16.10, p = 0.035) (Table 3). Regarding the FIGO stages of cervical cancer, stages IA/B remained associated with a reduced likelihood of being infected with several HPV genotypes (aOR: 0.136, 95% CI: 0.03–0.58, p = 0.007) and HR-HPV genotypes (aOR: 0.16, 95% CI: 0.03–0.77, p = 0.022) (Table 3). On the other hand, women with cervical neoplasia of stages IIA/B and IIIA/B had significantly high likelihoods of harboring SCC (aOR: 11.12, 95% CI: 1.12–109.99, p = 0.039) and Gardasil® vaccine genotypes (aOR: 9.33, 95% CI: 1.05–82.78, p = 0.045), respectively (Table 3 and Table 4). Interestingly, while the high likelihood of harboring CIN2/3 lesions which was associated with reporting having previously been screened for HPV was lost in the multivariate regression analysis, the protective effect of a history of previous HPV screening against the occurrence of SCC was significantly confirmed in the multivariate analysis (aOR: 0.16, 95% CI: 0.03–0.94, p = 0.043) (Table 4).
4. Discussion
We herein evaluated for the first time the HPV genotypes distribution in Mauritanian women suffering from CIN2/3 or ICC, with the perspective of prophylactic vaccination against HPV. The results showed that single or multiple HR-HPV genotypes were generally detected by molecular biology in cervical biopsy material from CIN2/3, ADC, and SCC tissues. Interestingly, only a limited number of HR-HPV types, including mainly HPV-45, HPV-16, HPV-39, HPV-52, and HPV-33, were detected. This distribution possibly reflects a specific molecular epidemiology signature of HR-HPV associated with cervical lesions in Mauritania. In addition, the majority (88% of all biopsies and 93.6% of HPV-positive results) of study women suffering from severe cervical dysplasia, ADC, or SCC were infected by vaccine HR-HPV genotypes, including mostly HPV-45, HPV-16, HPV-52, HPV-33, and HPV-18. However, other aggressive nonvaccine HR-HPV genotypes were also detected, indicating their circulation in the adult female population in Mauritania. Taken together, our observations confirm the association of HR-HPV with the genesis of precancerous and cancerous cervical lesions in Mauritanian women. Undoubtedly, these observations indicate the existence of a specific epidemiological profile with highly pathogenic HR-HPV types circulating in the country. These findings also demonstrate the frequent involvement of nonvaccine HR-HPV genotypes, in cervical precancerous and cancerous lesions, mostly in co-infection with vaccine HR-HPV types. On public health perspective, our findings point out that prophylactic HPV vaccination must be necessarily combined with primary molecular screening of cervical HR-HPV infection. Combining these two preventive strategies would help in reaching the objectives of the WHO global strategy to accelerate the elimination of cervical cancer in 2030 [17], and ultimately to eradicate the second most prevalent female cancer in Mauritania.
Geographical distribution of HPV genotypes provides specific molecular epidemiology of circulating HPV strains that varies according to regions and countries. As a first approach, we evaluated the distribution of HPV genotypes associated with high-grade lesions or ICC in women living in Mauritania. HPV DNA was detected in the majority (94.0%) of cervical biopsies from study women presenting with CIN2/3, ADC, and SCC, with at least one HR-HPV in all HPV-positive samples and frequent (48.0%) multiple HR-HPV infections. Similar high prevalence rates of cervical HPV and HR-HPV infections are generally reported in adult women living in sub-Saharan Africa suffering from HPV-related cervical lesions, with wide variations between regions or countries, ranging from 85.9% in Senegal [31], 90.4% in Ghana, Nigeria, and South Africa [21], 92.4% [35] and 100% [36] in Gabon, 94.1% in Ethiopia and the Sudan [37], 100% in Zambia [38] and in Republic of Congo [39].
The diversity of HR-HPV genotypes detected in FFPE biopsy samples from Mauritanian women appeared limited, as previously reported in other studies conducted in FFPE cervical high-grade tumor biopsies in sub-Saharan Africa. Thus, only six oncogenic genotypes were detected in study women (HPV-45, HPV-16, HPV-39, HPV-52, and HPV-33). In Gabon, the diversity of oncogenic HPV in FFPE cervical biopsies was similarly limited to six genotypes (HPV-16, HPV-18, HPV-33, HPV-35, HPV-45, and HPV-58) [35], whereas nine HR-HPV genotypes could be detected in Senegal (HPV-16, HPV-18, HPV-31, HPV-33, HPV-35, HPV-39, HPV-45, HPV-56, and HPV-58) [31] and Cameroon (HPV-16, HPV-18, HPV-33, HPV-35, HPV-39, HPV-45, HPV-51, HPV-56, and HPV-82) [40]. The preselection of cervical biopsy samples with CIN2/3 or ICC decreases the probability of finding HPV genotypes not associated with cancer or high-grade lesions. Another factor that could reduce the diversity of HPV infection that could be envisaged in these women is the fact that all male partners in Mauritania are ritually circumcised in childhood [41]. Our observations point out also that the diversity of oncogenic HPV varies among sub-Saharan African countries. Indeed, the two main genotypes detected in CIN or ICC worldwide are HPV-16 and HPV-18 [42]. For example, in Gabon, the prevalence of HPV-16 was 75.4% and that of HPV-18 was 18.0% [35]. In Senegal, the prevalence of HPV-16 was 56.8% and that of HPV-18 was 14.6% [31]. Thus, the distribution of oncogenic HR-HPV genotypes in Mauritania appears unique, with HPV-16 and HPV-18 which ranked only as the second and sixth most detected genotypes, respectively. The most prevalent genotype was HPV-45, and the oncogenic genotypes HPV-39, HPV-52, and HPV-33 were more prevalent than HPV-18. The prevalence of HPV-45 (40.4%) was the highest in our series, which is reminiscent to the relatively high prevalence (13.0%) of this genotype in cervical lesions in Senegal and more generally in Africa (7.2% to 15.5%) [21,22,23]. Like what was observed for HPV-45, the genotype HPV-16, which was the second (38.3%) most detected in Mauritania women, is also frequently detected in ICC in sub-Saharan Africa, ranging from 13.8% [23], 51.2% [21] to 58.2% [22]. In addition, HPV-52, the third (23.4%) most detected genotype in our study, is also commonly detected in HPV-associated cervical lesions in the eastern and southern African areas [23], with large variations ranging from 2.3% to 13.7% [22]. However, in Senegal, while genital carriage of HPV-52 was very common in the general population (3.5%) [29] and female sex workers (32.6%) [43], this genotype was rarely detected in ICC in Mali and Senegal (0.7%) [30]. In Caucasian women, some HPV-52 variants have been described as being associated with a higher risk of developing high-grade lesions or cervical cancer [44,45]. Further genomic polymorphism studies of HPV-52 strains might be helpful to better understand the mechanisms of persistence or elimination of HPV-52 and its association with CIN or ICC in Mauritanian women [45]. Among LR-HPV, HPV-81 was detected in ten percent of study women, whereas the HPV-6 and HPV-11 targeted by the Gardasil® HPV vaccines could not be found. HPV-81 was relatively frequently detected in one of ten women with CIN2/3 or SCC, a prevalence of a similar range to those previously reported in childbearing-aged women living in Kenya (7.4%) [46] and South Africa (7.6%) [47]. According to IARC, HPV-81 is classified as an LR-HPV [2]. HPV-81 is recognized as a new type mostly found in individuals with a weak immune system [48], which is also a risk factor associated with precancerous and cancerous lesions [46,49]. However, none of our study participants were infected with HIV. On the other hand, HPV-81 was always associated with one or two HR-HPV types in our study, and its involvement in carcinogenesis remains uncertain. Whether HPV-81 may play a role in cancer etiology as a syndemic partner likely warrants further investigations.
A high rate (54.0%) of multiple HPV infection (2 to 3 HPV types) was observed in our study population. This proportion is higher than that generally found in other series which varied from 4% to 39% depending on the clinical stages [21,31,50,51,52,53,54] and HIV-serostatus [21,22,55]. In Senegal, a very high rate of multiple HPV genital infections (70.1%) was reported in female sex workers [43]. Whether multiple genital HPV infections in Mauritanian women could be associated with high-risk sexual behavior remains unknown. Otherwise, the association between multiple HPV infections and HIV infection previously reported [56,57] cannot explain the high prevalence of multiple cervical HPV infections in our study women, as they were not infected with HIV. Regardless, these features may constitute a real concern for the health care of Mauritanian women as multiple cervical HR-HPV infections increase the risk of cervical abnormalities [58], and are associated with poor outcome and treatment response of invasive cancer [52,59].
Cervical cancer is the leading cause of cancer-related deaths among women in sub-Saharan Africa, but it can be prevented by vaccination [9]. Although current vaccines only target up to nine different genotypes, cross-immunity and probably cross-protection occur between the genotypes targeted by the vaccine and nonvaccine genotypes [60]. However, the effectiveness of cervical HPV prevention by prophylactic vaccines remains largely dependent on the molecular epidemiology of HPV strains present in each region, most particularly in women with high-grade lesions or ICC. The majority (88.0%) of study women suffering from CIN2/3 or ICC were infected by 9-valent HPV Gardasil-9® vaccine genotypes. Furthermore, most (93.6%) women with HPV-positive cervical samples harbored at least one 9-valent HPV genotype. HPV-45 was the predominant genotype, followed by HPV-16, HPV-52, HPV-33, and HPV-18, and 38.3% of women were infected by multiple (two to three) 9-valent vaccine HPV genotypes. When considering all HPV-positive results, the majority (74.1%) corresponded to HPV genotypes covered by the Gardasil-9® vaccine, while 25.9% corresponded to nonvaccine HPV genotypes, mainly nonvaccine HR-HPV (HPV-39, HPV-35, and HPV-56). Detection of nonvaccine HR-HPV types circulating in the general adult female population, which may be non-rarely detected in precancerous and cancerous cervical tissues, is frequently reported in several sub-Saharan African countries [22,31,61,62,63]. Two-thirds of biopsies with nonvaccine HR-HPV were co-infected with vaccine-targeted HR-HPV, as previously observed in Ghana for HPV-35 and HPV-56 [61]. The co-infection of vaccine genotypes with nonvaccine HR-HPV may reduce the efficacy of HPV vaccines in preventing cervical cancer [22]. It has been suggested that the high prevalence of cervical HPV infections harboring simultaneously both nonvaccine HR-HPV and vaccine HR-HPV could be associated with the high age-standardized incidence rate (ASIR) of cervical cancer in sub-Saharan Africa [22]. Taken together, our observations in Mauritanian women indicate that around 90% of CIN2/3, ADC, or SCC are associated with HR-HPV covered by the 9-valent Gardasil® HPV vaccine. However, these findings also highlight the presence of other aggressive nonvaccine HR-HPV types representing one-third of oncogenic HR-HPV detected, indicating indirectly their circulation in the adult female population living in Mauritania. Our observations raise several practical issues in the prevention of HPV infection and cervical cancer in Mauritania. Firstly, the prophylactic HPV vaccination, which likely covers the majority of genital HPV detected in adult Mauritanian women suffering from severe cervical dysplasia, ADC, or SCC, remains essential for the primary prevention of cervical cancer. Thus, a public health program involved in HPV vaccination implementation should be clearly extended at the national level. However, according to our observations, prophylactic HPV vaccination would remain insufficient to cover all HPV genotypes associated with precancerous or malignant cervical lesions that might represent a risk for cervical cancer in Mauritania. Secondly, it now seems necessary to design for Mauritania and neighboring countries, as for many other countries in sub-Saharan Africa, a prophylactic HPV vaccine better adapted to the viral strains of HPV circulating in sub-Saharan regions in women after age 30 (or after age 25 if living with HIV). Finally, continuation and generalization of primary molecular screening of carcinogenic HPV according to the recently revised WHO recommendations [17] as well as the implementation of pathology laboratory facilities for cytology and histological confirmation and triage of HR-HPV-positive cases, which remains challenging in sub-Saharan Africa [64], are necessary to eradicate cervical cancer in Mauritania. New prevention strategies for cervical carcinoma, particularly those using self-sampling of female genital secretions for HPV molecular testing, are particularly suited to resource-constrained settings for hard-to-reach populations or when medical facilities are lacking [65,66,67,68,69].
In the present series, the number of SCC was about 10 times higher than ADC, as previously reported in the literature [39,70,71]. According to sociological aspects, our population of patients with CIN2/3 lesions or cervical cancer consisted of women ranging from 35 to 73 years old (mean: 56.7 years). Almost two-thirds of HPV-positive patients were over 50 years old, and the most affected age group was 60–69 years old. Stages II to IV were frequently represented (44.0%), testifying to a delay in screening, which may be linked to a lack of sensitization in women whose level of education was extremely low with half of the women never having been to school. Very similar socio-demographic profiles and stages of HPV-related lesions were previously observed in the neighboring country Senegal [31]. The multivariate analysis of the different variables of interest is difficult to interpret, due to the small size of the included population. However, it appears that advanced age and clinical stage were associated with multiple HR-HPV infections, likely because of immune-senescence or tumor aggressiveness [72,73]. Previous HPV screening was associated with precancerous CIN2/3 diagnosis and decreased occurrence of SCC, which confirms the critical need for effective primary molecular HPV screening in adult women living in Mauritania, with particular attention for elderly women.
No HPV DNA sequences were identified in 6.0% of our cases despite retesting. This rate of HPV-negative biopsy samples is lower than those generally reported for the FFPE sample, ranging from 10% [74], 10.8% [75], 12.5% [30] to 14.1% [31]. In our study, the quality of the DNA was assessed by evaluating the housekeeping TOP3 gene in all samples, which were all found to be adequate. However, negative HPV results could have been related to the sampling method. Indeed, FFPE preparation for molecular analysis or DNA extraction is composed of several critical steps that could impact the amount or the quality of genetic material to be amplified [76]. Indeed, it is well reported that DNA recovering in FFPE specimens may be partially degraded, influenced by several factors, such as formalin quality and concentration, length of fixation, paraffin quality, and temperature [76]. Consequently, DNA in FFPE biopsies is either completely or partially degraded into DNA fragments of 200 bp or less [77,78]. Interestingly, the Bioperfectus HPV assay relies on the amplification of only 100 bp-fragments, a feature that could be associated with better PCR efficiency when using DNA extracted from FFPE biopsies, and which could partly explain the low rate of HPV-negative samples in this study. It is also possible that mutations affecting the priming sites of the primers used in the Bioperfectus assay could have led to misdetection. Furthermore, the target region of the multiplex PCR used may have been deleted during the process of integration of the viral DNA into the host genome that occurs in more than 80% of cervical cancers [79,80]. Finally, the possibility that a small proportion of cervical carcinoma develops independently of HPV oncogenesis must be considered regarding the policy of vaccination and of detection of intraepithelial neoplasia based on virological testing [31].
Our study has several limitations that need to be considered. First, the representativeness of the included study population is not ensured. Indeed, such inclusion bias could be extended in other urban and rural remote areas in Mauritania, where no women were included. Second, the small sample size of our study population may have introduced a selection bias because included precancerous and cancer cases could represent a select group of women who were healthy enough to participate in study enrollment, and therefore likely had less severe cancer stages. Third, participants were included on a voluntary basis, which may constitute a source of recruitment bias, impacting the validity of the answers to the sociodemographic questionnaire, including items related to the intimacy of their lives. Finally, the preselection of pathologic cervical biopsy material decreases the probability of finding HPV genotypes not associated with high-grade lesions or cancer. Furthermore, FFPE biopsy samples are not the ideal material for HPV detection.
5. Conclusions
Our study shows that the HR-HPV genotypes in CIN2/3 and cervical cancer in Mauritanian women match generally with the HPV types targeted by the prophylactic 9-valent Gardasil-9® HPV vaccine, but unfrequently with the Gardasil-4® vaccine. This feature highlights the need for a shift from the quadrivalent to the 9-valent HPV vaccine for protection against chronic HPV infection and cervical neoplasia in Mauritania. The high prevalence of HPV types targeted by the Gardasil-9® HPV vaccine supports the continuation of the 9-valent HPV vaccine national program as this vaccine targets a large number of HR-HPV types that cause cancer. Our results also strongly support the intensification of a largescale roll-out of HPV vaccination to Mauritanian girls and the establishment of catch-up campaigns for young adolescents or adults. The reinforcement of primary molecular HPV testing and pathological triage are essential for the early detection of cervical precancerous lesions among women who are already infected with HPV, unvaccinated or partially vaccinated, and those infected with HPV types not targeted by current HPV vaccines. The circulation of nonvaccine HR-HPV types (16.5%), specifically HPV-39, HPV-35, and HPV-56, also raises concern in the Mauritanian population. In addition, our study showed that a minority of CIN2/3 or ICC might remain HPV-negative. Taken together, our observations could help inform health policy makers by providing useful HPV baseline data for assessing the impact of HPV vaccine effectiveness, and possibly assist in the development of a policy to improve HPV vaccination strategies. Finally, the primary prevention of precancerous and cancerous cervical diseases in Mauritania by the 9-valent prophylactic vaccination should be integrated into a large national program including sensitization and screening to sustainably decrease the mortality rate related to cervical cancer.
Author Contributions
Conceptualization, M.S.A., M.V.M.A., N.D.M.B. and M.L.C.B.A.; methodology, M.S.A. and L.B.; software, M.S.A. and R.-S.M.B.; validation, M.S.A., R.-S.M.B. and L.B; formal analysis, M.S.A., R.-S.M.B. and L.B.; investigation, M.S.A., M.V.M.A. and N.D.M.B.; resources, M.V.M.A., M.L.C.B.A. and N.D.M.B.; data curation, M.S.A., M.V.M.A., M.L.C.B.A. and N.D.M.B.; writing—original draft preparation, M.S.A., R.-S.M.B. and L.B.; writing—review and editing, M.S.A., M.V.M.A., M.L.C.B.A., N.D.M.B., R.-S.M.B. and L.B.; visualization, M.S.A., R.-S.M.B. and L.B; supervision, M.L.C.B.A. and L.B; project administration, M.L.C.B.A. and L.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board and Ethics Committee of the Nouakchott University, Nouakchott, Mauritania (approval no. 004/CE/UN on 27 January 2022). This study is research with a direct individual benefit, with the histological diagnosis of suspected cervical lesions and virological diagnosis of possible oncogenic HR-HPV. This work was conducted in accordance with the Ethical Guidelines of the World Medical Association Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the conclusions of this study are available from the corresponding author upon reasonable request.
Acknowledgments
Mariem Salma Abdoudaimis, PhD student from the Ecole Doctorale des Sciences et Technologies en Mauritanie, Nouakchott, Mauritania, is the holder of a merit scholarship awarded by the Cooperation and Cultural Action Service of the French Embassy in Mauritania. The authors are grateful to Saree Ho, International sales and marketing division, Bioperfectus (Jiangsu Bioperfectus Technologies Co., Ltd., Taizhou, China), for providing the HPV multi-plex PCR kits for the study. The authors are finally particularly thankful to Julien Puech, Full Life Sciences Engineer, for their expertise in molecular biology.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ghittoni, R.; Accardi, R.; Chiocca, S.; Tommasino, M. Role of human papillomaviruses in carcinogenesis. Ecancermedicalscience 2015, 9, 526. [Google Scholar] [CrossRef] [PubMed]
- Bouvard, V.; Baan, R.; Straif, K.; Grosse, Y.; Secretan, B.; El Ghissassi, F.; Benbrahim-Tallaa, L.; Guha, N.; Freeman, C.; Galichet, L.; et al. A review of human carcinogens–Part B: Biological agents. Lancet Oncol. 2009, 10, 321–322. [Google Scholar] [CrossRef] [PubMed]
- Subramanya, D.; Grivas, P.D. HPV and cervical cancer: Updates on an established relationship. Postgrad. Med. 2008, 120, 7–13. [Google Scholar] [CrossRef]
- Haedicke, J.; Iftner, T. Human papillomaviruses and cancer. Radiother. Oncol. 2013, 108, 397–402. [Google Scholar] [CrossRef]
- de Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef]
- Bruni, L.; Diaz, M.; Castellsagué, X.; Ferrer, E.; Bosch, F.X.; de Sanjosé, S. Cervical human papillomairus prevalence in 5 continents: Meta-analysis of 1 million women with normal cytological findings. J. Infect. Dis. 2010, 202, 1789–1799. [Google Scholar] [CrossRef]
- Lacey, C.J.; Lowndes, C.M.; Shah, K.V. Chapter 4: Burden and management of non-cancerous HPV-related conditions: HPV-6/11 disease. Vaccine 2006, 24 (Suppl. 3), S35–S41. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cervical Cancer. World Health Organization 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer (accessed on 23 March 2024).
- Mboumba Bouassa, R.S.; Prazuck, T.; Lethu, T.; Jenabian, M.A.; Meye, J.F.; Bélec, L. Cervical cancer in sub-Saharan Africa: A preventable noncommunicable disease. Expert Rev. Anti Infect. Ther. 2017, 15, 613–627. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Lekoane, K.M.B.; Kuupiel, D.; Mashamba-Thompson, T.P.; Ginindza, T.G. Evidence on the prevalence, incidence, mortality and trends of human papilloma virus-associated cancers in sub-Saharan Africa: Systematic scoping review. BMC Cancer 2019, 19, 563. [Google Scholar] [CrossRef]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; Sanjosé, S.; Saraiya, M.; Ferlay, J.; Freddie, B. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef] [PubMed]
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global Cancer Incidence and Mortality Rates and Trends--An Update. Cancer Epidemiol. Biomark. Prev. 2016, 25, 16–27. [Google Scholar] [CrossRef]
- Reza, S.; Anjum, R.; Khandoker, R.Z.; Khan, S.R.; Islam, M.R.; Dewan, S.M.R. Public health concern-driven insights and re-sponse of low- and middle-income nations to the World health Organization call for cervical cancer risk eradica-tion. Gynecol Oncol Rep 2024, 54, 101460. [Google Scholar] [CrossRef]
- World Health Organization. Global Cancer Observatory. Africa. Available online: https://gco.iarc.who.int/media/globocan/factsheets/populations/903-africa-fact-sheet.pdf (accessed on 23 March 2024).
- Parkin, D.M.; Bray, F.; Ferlay, J.; Pisani, P. Global cancer statistics, 2002. CA Cancer J Clin. 2005, 55, 74–108. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guideline for Screening and Treatment of Cervical Pre-Cancer Lesions for Cervical Cancer Prevention, Second Edition. World Health Organization 2021. Available online: https://www.who.int/publications/i/item/9789240030824 (accessed on 31 March 2024).
- Muresu, N.; Sotgiu, G.; Marras, S.; Gentili, D.; Sechi, I.; Cossu, A.; Dettori, A.; Pietri, R.E.; Paoni, L.; Ghi, M.E.; et al. Cervical Screening in North Sardinia (Italy): Genotype Distribu-tion and Prevalence of HPV among Women with ASC-US Cytology. Int. J. Environ. Res. Public Health 2022, 19, 693. [Google Scholar] [CrossRef]
- Hu, J.P.; Wang, J.L.; Li, Y.; Feng, Y.; Tian, C.Q.; Zhang, G.H.; Chen, X.Q.; Liu, H.X.; Yang, J.S.; Fang, Z.W.; et al. Prevalence and genotype dis-tribution of human papillomavirus infection among 66000 women from 2014 to 2023 in the plateau region of Southwest China. Virol. J. 2024, 21, 176. [Google Scholar] [CrossRef]
- Li, N.; Franceschi, S.; Howell-Jones, R.; Snijders, P.J.F.; Clifford, G.M. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: Variation by geographical region, histological type and year of publication. Int. J. Cancer 2011, 128, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Denny, L.; Adewole, I.; Anorlu, R.; Dreyer, G.; Moodley, M.; Smith, T.; Snyman, L.; Wiredu, E.; Molijn, A.; Quint, W.; et al. Human papillomavirus prevalence and type distribution in invasive cervical cancer in sub-Saharan Africa. Int. J. Cancer 2014, 134, 1389–1398. [Google Scholar] [CrossRef]
- Okoye, J.O.; Ofodile, C.A.; Adeleke, O.K.; Obioma, O. Prevalence of high-risk HPV genotypes in sub-Saharan Africa according to HIV status: A 20-year systematic review. Epidemiol. Health 2021, 43, e2021039. [Google Scholar] [CrossRef]
- Seyoum, A.; Assefa, N.; Gure, T.; Seyoum, B.; Mulu, A.; Mihret, A. Prevalence and Genotype Distribution of High-Risk Human Papillomavirus Infection Among Sub-Saharan African Women: A Systematic Review and Meta-Analysis. Front. Public Health 2022, 10, 890880. [Google Scholar] [CrossRef]
- World Health Organization. Cervical Cancer Mauritania 2021 Country Profile. Available online: https://www.who.int/publications/m/item/cervical-cancer-mrt-country-profile-2021 (accessed on 23 March 2024).
- ICO/IARC Information Centre on HPV and Cancer. Mauritania. Human Papillomavirus and Related Cancers, Fact Sheet 2023 (2023-03-10). Available online: https://hpvcentre.net/statistics/reports/MRT_FS.pdf (accessed on 23 March 2024).
- ICO/IARC Information Centre on HPV and Cancer. Human Papillomavirus and Related Diseases Report. Mauritania. Available online: https://hpvcentre.net/statistics/reports/MRT.pdf (accessed on 23 March 2024).
- World Health Organization. Global Cancer Observatory. Mauritania. Available online: https://gco.iarc.who.int/media/globocan/factsheets/populations/478-mauritania-fact-sheet.pdf (accessed on 23 March 2024).
- Mauritania: Cervical Cancer. Available online: https://www.worldlifeexpectancy.com/mauritania-cervical-cancer (accessed on 23 March 2024).
- Mbaye el, H.S.; Gheit, T.; Dem, A.; McKay-Chopin, S.; Toure-Kane, N.C.; Mboup, S.; Tommasino, M.; Sylla, B.S.; Boye, C.S. Human papillomavirus infection in women in four regions of Senegal. J. Med. Virol. 2014, 86, 248–256. [Google Scholar] [CrossRef]
- Ndiaye, C.; Alemany, L.; Ndiaye, N.; Kamaté, B.; Diop, Y.; Odida, M.; Banjo, K.; Tous, S.; Klaustermeier, J.E.; Clavero, O.; et al. Human papillomavirus distribution in invasive cervical carcinoma in sub-Saharan Africa: Could HIV explain the differences? Trop. Med. Int. Health 2012, 17, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Diop-Ndiaye, H.; Sastre-Garau, X.; Drame, A.; Dembele, B.; Ba, N.N.; Diop-Diongue, O.; Mbow, M.; Diakhaby, M.E.B.; Woto-Gaye, G.; Toure Kane, C.; et al. Respective prevalence of high-risk HPV genotypes in cervical neoplasia in Senegal. J. Med. Virol. 2021, 93, 5110–5117. [Google Scholar] [CrossRef] [PubMed]
- Pecorelli, S.; Zigliani, L.; Odicino, F. Revised FIGO staging for carcinoma of the cervix. Int. J. Gynaecol. Obstet. Org. Int. Fed. Gynaecol. Obstet. 2009, 105, 107–108. [Google Scholar] [CrossRef]
- Sun, Z.; Zhang, R.; Liu, Z.; Liu, C.; Li, X.; Zhou, W.; Yang, L.; Ruan, Q.; Zhang, X. Development of a fluorescence-based multiplex genotyping method for simultaneous determination of human papillomavirus infections and viral loads. BMC Cancer 2015, 15, 860. [Google Scholar] [CrossRef] [PubMed]
- Hanai, R.; Caron, P.R.; Wang, J.C. Human TOP3: A single-copy gene encoding DNA topoisomerase III. Proc. Natl. Acad. Sci. USA 1996, 93, 3653–3657. [Google Scholar] [CrossRef] [PubMed]
- Moussavou-Boundzanga, P.; Koumakpayi, I.H.; Engohan Aloghe, C.; Chansi, J.K.; Revignet, R.; Leroy, E.M.; Berthet, N. HPV genotypes in high-grade cervical lesions and invasive cervical carcinoma detected in Gabonese women. Infect. Agent. Cancer 2023, 18, 16. [Google Scholar] [CrossRef]
- Zoa-Assoumou, S.; Ndjoyi-Mbiguino, A.; Mabika, B.M.; Belembaogo, E.; Khattabi, A.; Ennaji, M.M. Human papillomavirus genotypes distribution in cervical cancer cases in Gabon. Infect. Agent. Cancer 2016, 11, 42. [Google Scholar] [CrossRef][Green Version]
- Abate, E.; Aseffa, A.; El-Tayeb, M.; El-Hassan, I.; Yamuah, L.; Mihret, W.; Bekele, L.; Ashenafi, S.; El-Dawi, N.; Belayneh, M.; et al. Genotyping of human papillomavirus in paraffin embedded cervical tissue samples from women in Ethiopia and the Sudan. J. Med. Virol. 2013, 85, 282–287. [Google Scholar] [CrossRef]
- Sahasrabuddhe, V.V.; Mwanahamuntu, M.H.; Vermund, S.H.; Huh, W.K.; Lyon, M.D.; Stringer, J.S.; Parham, G.P. Prevalence and distribution of HPV genotypes among HIV-infected women in Zambia. Br. J. Cancer 2007, 96, 1480–1483. [Google Scholar] [CrossRef]
- Tsimba, P.C.L.; Boumba, L.M.A.; Mouamba, F.G.; Moudiongui-Mboungou Malanda, D.; Okoko Eckouda, B.A.; Peko, J.F. Molecular Characterization of Human Papillomaviruses Associated with Cervical Cancer in Brazzaville, Congo. Int. J. Res. Oncol. 2022, 1, 1–5. [Google Scholar] [CrossRef]
- Pirek, D.; Petignat, P.; Vassilakos, P.; Gourmaud, J.; Pache, J.C.; Rubbia-Brandt, L.; Sando, Z.; McKee, T.A.; Ho, L. Human papillomavirus genotype distribution among Cameroonian women with invasive cervical cancer: A retrospective study. Sex. Transm. Infect. 2015, 91, 440–444. [Google Scholar] [CrossRef]
- Smith, J.S.; Backes, D.M.; Hudgens, M.G.; Mei, W.; Chakraborty, H.; Rohner, E.; Moses, S.; Agot, K.; Meijer, C.J.L.M.; Bailey, R.C. Male Circumcision Reduces Penile HPV Incidence and Persistence: A Randomized Controlled Trial in Kenya. Cancer Epidemiol. Biomark. Prev. 2021, 30, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Kind, A.B.; Pavelyev, A.; Kothari, S.; El Mouaddin, N.; Schmidt, A.; Morais, E.; Guggisberg, P.; Lienert, F. Assessing the epidemiological impact on cervical cancer of switching from 4-valent to 9-valent HPV vaccine within a gender-neutral vaccination programme in Switzerland. BMC Public Health 2020, 20, 671. [Google Scholar] [CrossRef]
- Diop-Ndiaye, H.; Beiter, K.; Gheit, T.; Sow Ndoye, A.; Dramé, A.; McKay-Chopin, S.; Tommasino, M.; Bouh Boye, C.S.; Sylla, B.; Kane, C.T. Human Papillomavirus infection in senegalese female sex workers. Papillomavirus Res. 2019, 7, 97–101. [Google Scholar] [CrossRef]
- Aho, J.; Hankins, C.; Tremblay, C.; Forest, P.; Pourreaux, K.; Rouah, F.; Coutlée, F.; Canadian Women’s HIV Study Group. Genomic polymorphism of human papillomavirus type 52 predisposes toward persistent infection in sexually active women. J. Infect. Dis. 2004, 190, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Formentin, A.; Archambault, J.; Koushik, A.; Richardson, H.; Brassard, P.; Franco, E.L.; Coutlée, F. Human papillomavirus type 52 polymorphism and high-grade lesions of the uterine cervix. Int. J. Cancer 2013, 132, 1821–1830. [Google Scholar] [CrossRef]
- Omire, A.; Budambula, N.L.M.; Kirumbi, L.; Langat, H.; Kerosi, D.; Ochieng, W.; Lwembe, R. Cervical Dysplasia, Infection, and Phylogeny of Human Papillomavirus in HIV-Infected and HIV-Uninfected Women at a Reproductive Health Clinic in Nairobi, Kenya. Biomed. Res. Int. 2020, 2020, 4945608. [Google Scholar] [CrossRef]
- Mbulawa, Z.Z.A.; van Schalkwyk, C.; Hu, N.C.; Meiring, T.L.; Barnabas, S.; Dabee, S.; Jaspan, H.; Kriek, J.M.; Jaumdally, S.Z.; Muller, E.; et al. High human papillomavirus (HPV) prevalence in South African adolescents and young women encourages expanded HPV vaccination campaigns. PLoS ONE 2018, 13, e0190166. [Google Scholar] [CrossRef]
- Co, N.N.C.; Chu, L.-O.; Chow, K.F.; Tam, J.W.O.; Ng, E.K.O. HPV prevalence and detection of rare HPV genotypes in Hong Kong women from southern China with cytological abnormalities. ISRN Virol. 2013, 2013, 312706. [Google Scholar] [CrossRef]
- Choi, Y.D.; Han, C.W.; Chung, W.J.; eJung, W.W.; Lee, J.S.; Nam, J.H.; Lee, M.C.; Juhng, S.W.; Choi, H.S.; Park, C.S. Analysis of HPV-other samples by performing HPV DNA sequencing. J. Pathol. Transl. Med. 2009, 43, 250–253. [Google Scholar] [CrossRef]
- de Sanjose, S.; Quint, W.G.; Alemany, L.; Geraets, D.T.; Klaustermeier, J.E.; Lloveras, B.; Tous, S.; Felix, A.; Bravo, L.E.; Shin, H.R.; et al. Retrospective International Survey and HPV Time Trends Study Group. Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncol. 2010, 11, 1048–1056. [Google Scholar] [CrossRef]
- Li, J.; Wang, Y.Y.; Nan, X.; Tian, X.F.; Yan, T.; Wang, P.; Yin, Y.; Liu, Y.; Yuan, R.; Wang, G.Q.; et al. Prevalence of human papillomavirus genotypes among women with cervical lesions in the Shaanxi Province of China. Gent Mol. Res. 2016, 15, 1–9. [Google Scholar] [CrossRef]
- Nogueira Dias Genta, M.L.; Martins, T.R.; Mendoza Lopez, R.V.; Sadalla, J.C.; de Carvalho, J.P.M.; Baracat, E.C.; Levi, J.E.; Carvalho, J.P. Multiple HPV genotype infection impact on invasive cervical cancer presentation and survival. PLoS ONE 2017, 12, e0182854. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, J.; Kamiura, S.; Okayama, K.; Okodo, M.; Shibata, T.; Osaka, Y.; Fujita, S.; Takata, E.; Takagi, H.; Takakura, M.; et al. Single type infection of human papillomavirus as a cause for high-grade cervical intraepithelial neoplasia and invasive cancer in Japan. Papillomavirus Res. 2018, 6, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Kabir, A.; Bukar, M.; Nggada, H.A.; Rann, H.B.; Gidado, A.; Musa, A.B. Prevalence of human papillomavirus genotypes in cervical cancer in Maiduguri, Nigeria. Pan Afr. Med. J. 2019, 33, 284. [Google Scholar] [CrossRef] [PubMed]
- Jaquet, A.; Horo, A.; Charbonneau, V.; Ekouevi, D.K.; Roncin, L.; Toure, B.; Coffie, P.; Minga, A.; Sasco, A.J.; Garrigue, I.; et al. Cervical human papillomavirus and HIV infection in women of child-bearing age in Abidjan, Côte d’Ivoire, 2010. Br. J. Cancer 2012, 107, 556–563. [Google Scholar] [CrossRef]
- Obiri-Yeboah, D.; Akakpo, P.K.; Mutocheluh, M.; Adjei-Danso, E.; Allornuvor, G.; Amoako-Sakyi, D.; Adu-Sarkodie, Y.; Mayaud, P. Epidemiology of cervical human papillomavirus (HPV) infection and squamous intraepithelial lesions (SIL) among a cohort of HIV-infected and uninfected Ghanaian women. BMC Cancer 2017, 17, 688. [Google Scholar] [CrossRef]
- Camargo, M.; Del Río-Ospina, L.; Soto-De León, S.C.; Sánchez, R.; Pineda-Peña, A.C.; Sussmann, O.; Patarroyo, M.E.; Patarroyo, M.A. Association of HIV status with infection by multiple HPV types. Trop. Med. Int. Health 2018, 23, 1259–1268. [Google Scholar] [CrossRef]
- Adler, D.H.; Wallace, M.; Bennie, T.; Abar, B.; Meiring, T.L.; Williamson, A.I.; Bekker, L.G. Cumulative impact of HIV and multiple concurrent human Papillomavirus infections on the risk of cervical dysplasia. Adv. Virol. 2016, 2016, 7310894. [Google Scholar] [CrossRef]
- Bello, B.D.; Spinillo, A.; Alberizzi, P.; Cesari, S.; Gardella, B.; D’Ambrosio, G.; Roccio, M.; Silini, E.M. Cervical infections by multiple human papillomavirus (HPV) genotypes: Prevalence and impact on the risk of precancerous epithelial lesions. J. Med. Virol. 2009, 81, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Malagón, T.; Drolet, M.; Boily, M.C.; Franco, E.L.; Jit, M.; Brisson, J.; Brisson, M. Cross-protective efficacy of two human papillomavirus vaccines: A systematic review and meta-analysis. Lancet Infect. Dis. 2012, 12, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Yar, D.D.; Salifu, S.P.; Darko, S.N.; Annan, A.A.; Gyimah, A.A.; Buabeng, K.O.; Owusu-Dabo, E. Genotypic characterisation of human papillomavirus infections among persons living with HIV infection; a case-control study in Kumasi, Ghana. Trop. Med. Int. Health 2016, 21, 275–282. [Google Scholar] [CrossRef]
- Mboumba Bouassa, R.S.; Nodjikouambaye, Z.A.; Sadjoli, D.; Adawaye, C.; Péré, H.; Veyer, D.; Matta, M.; Robin, L.; Tonen-Wolyec, S.; Moussa, A.M.; et al. High prevalence of cervical high-risk human papillomavirus infection mostly covered by Gardasil-9 prophylactic vaccine in adult women living in N’Djamena, Chad. PLoS ONE 2019, 14, e0217486. [Google Scholar] [CrossRef]
- Tsimba Lemba, P.C.; Boumba, L.M.A.; Péré, H.; Nganga, P.C.; Veyer, D.; Puech, J.; Mboumba Bouassa, R.S.; Malanda-Kiminou, P.; Moukassa, D.; Bélec, L. Human papillomavirus genotype distribution by cytological status and associated risk factors in the general population of Congolese women living in urban and rural areas: Implications for cervical cancer prevention. Infect. Dis. Now. 2023, 53, 104762. [Google Scholar] [CrossRef]
- Finocchario-Kessler, S.; Wexler, C.; Maloba, M.; Mabachi, N.; Ndikum-Mofor, F.; Bukusi, E. Cervical cancer prevention and treatment research in Africa: A systematic review from a public health perspective. BMC Womens Health 2016, 16, 29. [Google Scholar] [CrossRef]
- Mandigo, M.; Frett, B.; Laurent, J.R.; Bishop, I.; Raymondville, M.; Marsh, S.; Kobetz, E. Pairing community health workers with HPV self-sampling for cervical cancer prevention in rural Haiti. Int. J. Gynaecol. Obstet. 2015, 128, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Nodjikouambaye, Z.A.; Compain, F.; Sadjoli, D.; Mboumba Bouassa, R.S.; Péré, H.; Veyer, D.; Robin, L.; Adawaye, C.; To-nen-Wolyec, S.; Moussa, A.M.; et al. Accuracy of Curable Sexually Transmitted Infections and Genital Mycoplasmas Screening by Multiplex Real-Time PCR Using a Self-Collected Veil among Adult Women in Sub-Saharan Africa. Infect. Dis. Obstet. Gynecol. 2019, 2019, 8639510. [Google Scholar] [CrossRef]
- Martinelli, M.; Giubbi, C.; Sechi, I.; Bottari, F.; Iacobone, A.D.; Musumeci, R.; Perdoni, F.; Muresu, N.; Piana, A.; Fruscio, R.; et al. Evaluation of BD Onclarity™ HPV Assay on Self-Collected Vaginal and First-Void Urine Samples as Compared to Clinician-Collected Cervical Samples: A Pilot Study. Diagnostics 2022, 12, 3075. [Google Scholar] [CrossRef]
- Garcia, P.J.; Santos, C.; Chiappe, M.; Valderrama, M.; Carcamo, C.P. Academic account-ability to local communities and society through Programme Science: A case study from the HPV self-sampling programme HOPE in Peru. J. Int. AIDS Soc. 2024, 27 (Suppl. 2), e26297. [Google Scholar] [CrossRef]
- Yang, C.Y.; Chang, T.C.; Chou, H.H.; Chao, A.; Hsu, S.T.; Shih, Y.H.; Huang, H.J.; Lin, C.T.; Chen, M.Y.; Sun, L.; et al. Evaluation of a novel vaginal cells self-sampling de-vice for human papillomavirus testing in cervical cancer screening: A clinical trial assessing reliability and ac-ceptability. Bioeng. Transl. Med. 2024, 9, e10653. [Google Scholar] [CrossRef]
- Mubiayi, N.; Bogaert, E.; Boman, F.; Leblanc, E.; Vinatier, D.; Leroy, J.L.M.; Querleu, D. Cytological history of 148 women with invasive cervical cancer. Gynecol. Obstet. Fertil. 2002, 30, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Lavoué, V.; Gautier, C.; Piette, C.; Porée, P.; Mesbah, H.; Foucher, F.; Vialard, J.; Levêque, J. Cytological study of 191 women with invasive cervical cancer in Brittany, France. J. Gynecol. Obstet. Biol. Reprod. 2009, 38, 396–403. [Google Scholar] [CrossRef]
- Herrero, R.; Castle, P.E.; Schiffman, M.; Bratti, M.C.; Hildesheim, A.; Morales, J.; Alfaro, M.; Sherman, M.E.; Wacholder, S.; Chen, S.; et al. Epidemiologic profile of type-specific human papillomavirus infection and cervical neoplasia in Guanacaste, Costa Rica. J. Infect. Dis. 2005, 191, 1796–1807. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.R.; Weaver, B. Human papillomavirus in older women: New infection or reactivation? J. Infect. Dis. 2013, 207, 211–212. [Google Scholar] [CrossRef] [PubMed]
- Nicolás, I.; Marimon, L.; Barnadas, E.; Saco, A.; Rodríguez-Carunchio, L.; Fusté, P.; Martí, C.; Rodriguez-Trujillo, A.; Torne, A.; Del Pino, M.; et al. HPV-negative tumors of the uterine cervix. Mod. Pathol. 2019, 32, 1189–1196. [Google Scholar] [CrossRef]
- Veyer, D.; Wack, M.; Grard, O.; Bonfils, P.; Hans, S.; Bélec, L.; Badoual, C.; Péré, H. HPV detection and genotyping of head and neck cancer biopsies by molecular testing with regard to the new oropharyngeal squamous cell carcinoma classification based on HPV status. Pathology 2019, 51, 421–425. [Google Scholar] [CrossRef]
- Klopfleisch, R.; Weiss, A.T.; Gruber, A.D. Excavation of a buried treasure--DNA, mRNA, miRNA and protein analysis in formalin fixed, paraffin embedded tissues. Histol. Histopathol. 2011, 26, 797–810. [Google Scholar]
- Gilbert, M.T.; Haselkorn, T.; Bunce, M.; Sanchez, J.J.; Lucas, S.B.; Jewell, L.D.; Van Marck, E.; Worobey, M. The Isolation of Nucleic Acids from Fixed, Paraffin-Embedded Tissues–Which Methods Are Useful When? PLoS ONE 2007, 2, e537. [Google Scholar] [CrossRef]
- Steinau, M.; Patel, S.S.; Unger, E.R. Efficient DNA extraction for HPV genotyping in formalin-fixed, paraffin-embedded tissues. J. Mol. Diagn. 2011, 13, 377–381. [Google Scholar] [CrossRef]
- The Cancer Genome Atlas Research Network. Integrated genomic and molecular characterization of cervical cancer. Nature 2017, 543, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Nkili-Meyong, A.A.; Moussavou-Boundzanga, P.; Labouba, I.; Koumakpayi, I.H.; Jeannot, E.; Descorps-Declere, S.; Sastre-Garau, X.; Leroy, E.M.; Belembaogo, E.; Berthet, N. Genome-wide profling of human papillomavirus DNA integration in liquid-based cytology specimens from a Gabonese female population using HPV capture technology. Sci. Rep. 2019, 9, 1504. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).