The Assessment of Retinal Image Quality Using a Non-Mydriatic Fundus Camera in a Teleophthalmologic Platform
Abstract
1. Introduction
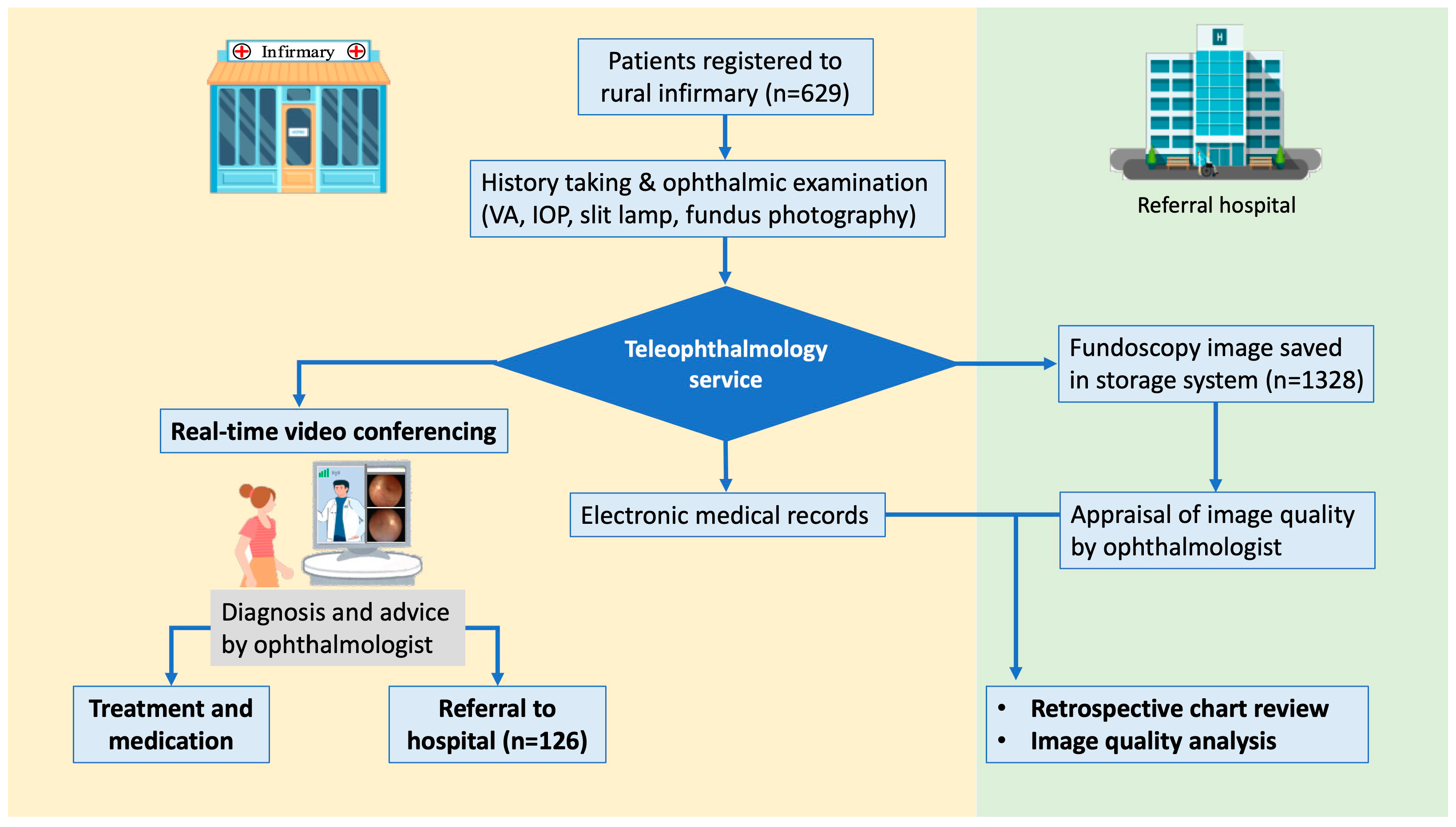
2. Materials and Methods
2.1. Participants and the Setting
2.2. Ophthalmic Examination, Image Acquisition, and Data Transmission
2.3. Clinical Diagnosis and Referral
2.4. Assessment of Diagnostic Agreement and Evaluation of Fundus Photographs
2.5. Statistical Analysis
3. Results
3.1. Participant Demographics and Characteristics
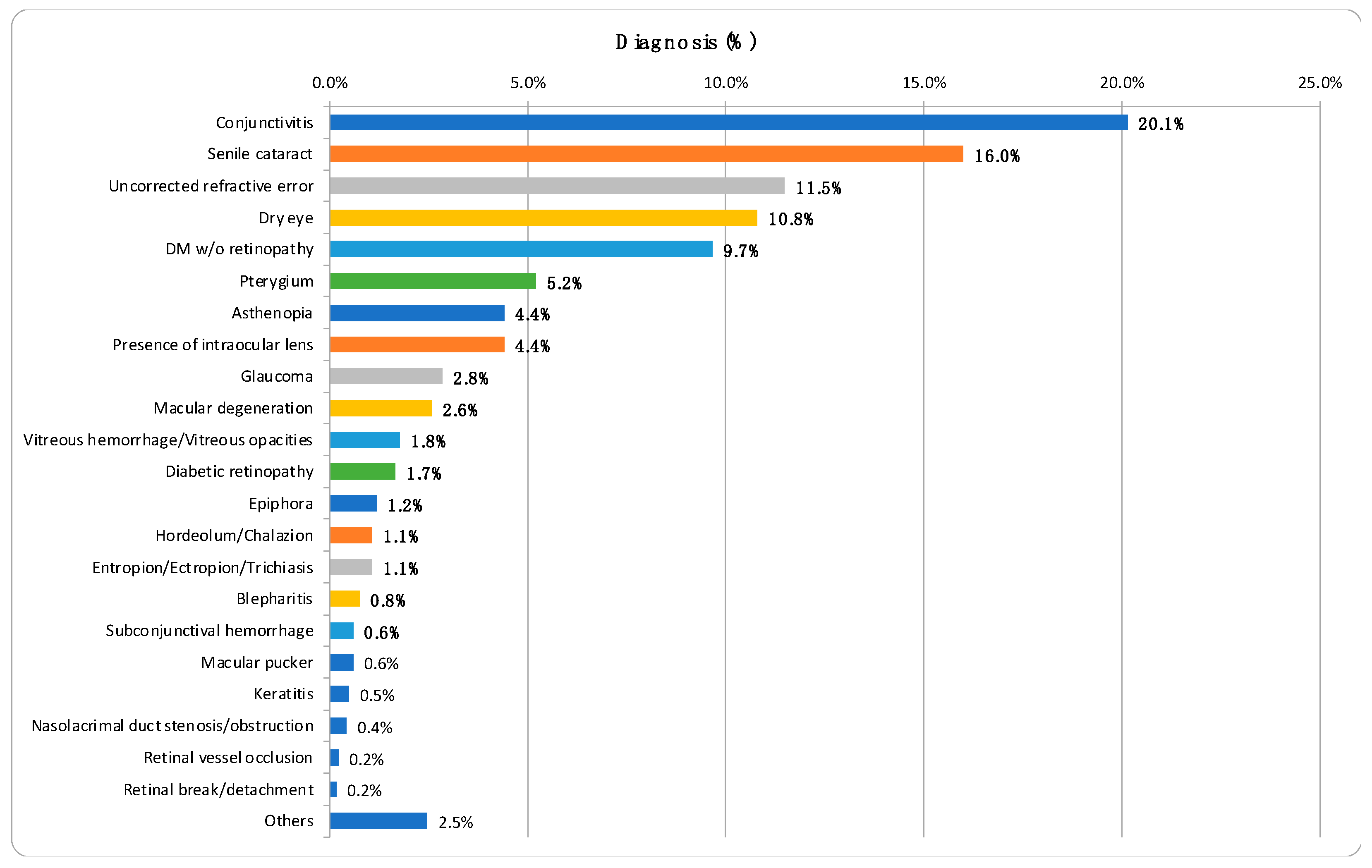
3.2. Distribution of Ocular Diseases
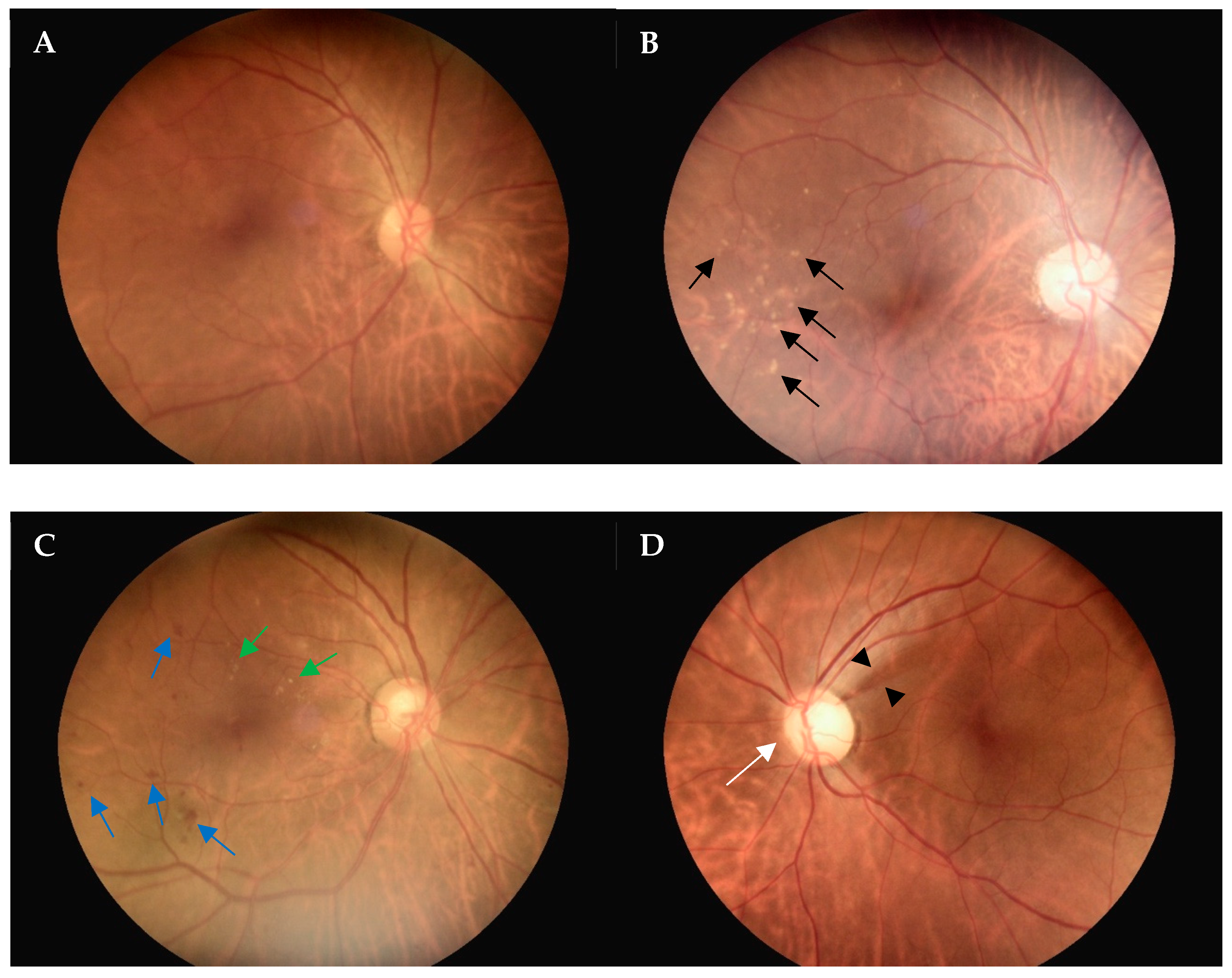
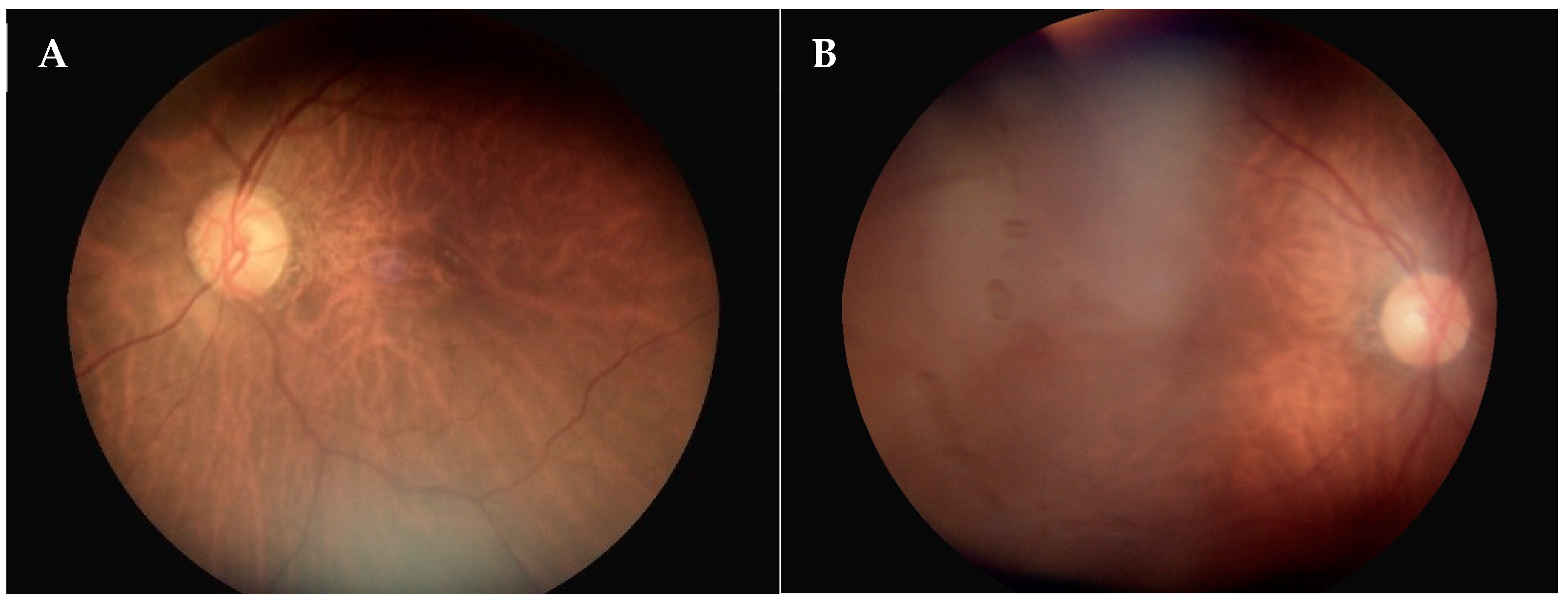
3.3. Evaluation of Fundoscopy Image Quality
3.4. Diagnostic Concordance of the Referrals
3.5. Risk Factors Associated with Poor-Quality Fundoscopy Images
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sood, S.; Mbarika, V.; Jugoo, S.; Dookhy, R.; Doarn, C.R.; Prakash, N.; Merrell, R.C. What Is Telemedicine? A Collection of 104 Peer-Reviewed Perspectives and Theoretical Underpinnings. Telemed. E-Health 2007, 13, 573–590. [Google Scholar]
- Sreelatha, O.K.; Ramesh, S.V. Teleophthalmology: Improving patient outcomes? Clin. Ophthalmol. 2016, 10, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.Y.; Blumenkranz, M.S.; Brothers, R.J.; Grosvenor, D.M. The sensitivity and specificity of single-field nonmydriatic monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: A comparison with ophthalmoscopy and standardized mydriatic color photography. Am. J. Ophthalmol. 2002, 134, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.R.; Merin, L.M.; Salunga, A.M.; Hepworth, J.T.; Crutcher, T.D.; O’Day, D.M.; Pilon, B.A. Improving diabetic retinopathy screening ratios using telemedicine-based digital retinal imaging technology: The Vine Hill study. Diabetes Care 2007, 30, 574–578. [Google Scholar] [CrossRef]
- Vujosevic, S.; Benetti, E.; Massignan, F.; Pilotto, E.; Varano, M.; Cavarzeran, F.; Avogaro, A.; Midena, E. Screening for diabetic retinopathy: 1 and 3 nonmydriatic 45-degree digital fundus photographs vs 7 standard early treatment diabetic retinopathy study fields. Am. J. Ophthalmol. 2009, 148, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.A.; Scott, I.U.; Haller, J.A.; Maguire, A.M.; Marcus, D.; McDonald, H.R. Single-field fundus photography for diabetic retinopathy screening: A report by the American Academy of Ophthalmology. Ophthalmology 2004, 111, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Szabo, D.; Fiedler, O.; Somogyi, A.; Somfai, G.M.; Bíró, Z.; Ölvedy, V.; Hargitai, Z.; Németh, J. Telemedical diabetic retinopathy screening in Hungary: A pilot programme. J. Telemed. Telecare 2015, 21, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Huang, W.; Han, X.; Liao, C.; Jin, L.; He, M. The Impact of Pharmacological Dilation on Intraocular Pressure in Primary Angle Closure Suspects. Am. J. Ophthalmol. 2022, 235, 120–130. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Wang, J.-H.; Chiu, C.-J. Satisfaction with Teleophthalmology Services: Insights from Remote Areas of Taiwan. Healthcare 2024, 12, 818. [Google Scholar] [CrossRef]
- Host, B.K.; Turner, A.W.; Muir, J. Real-time teleophthalmology video consultation: An analysis of patient satisfaction in rural Western Australia. Clin. Exp. Optom. 2018, 101, 129–134. [Google Scholar] [CrossRef]
- Le Tien, V.; Strého, M.; D’Athis, P.; Taillandier-Heriche, E.; Paillaud, E.; Mahiddine, H.; Coscas, G.; Lejonc, J.-L.; Soubrane, G.; Souied, E.H. Interobserver and intraobserver reliability of detecting age-related macular degeneration using a nonmydriatic digital camera. Am. J. Ophthalmol. 2008, 146, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Chew, E.Y. Screening options for diabetic retinopathy. Curr. Opin. Ophthalmol. 2006, 17, 519–522. [Google Scholar] [PubMed]
- Yeh, T.C.; Lo, K.-J.; Hwang, D.-K.; Lin, T.-C.; Chou, Y.-B. Evaluation of a remote telemedicine platform using a novel handheld fundus camera: Physician and patient perceptions from real-world experience. J. Chin. Med. Assoc. 2022, 85, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Lamirel, C.; Bruce, B.B.; Wright, D.W.; Delaney, K.P.; Newman, N.J.; Biousse, V. Quality of nonmydriatic digital fundus photography obtained by nurse practitioners in the emergency department: The FOTO-ED study. Ophthalmology 2012, 119, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Maberley, D.; Morris, A.; Hay, D.; Chang, A.; Hall, L.; Mandava, N. A comparison of digital retinal image quality among photographers with different levels of training using a non-mydriatic fundus camera. Ophthalmic Epidemiol. 2004, 11, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.C.; Chiang, Y.-H.; Hsu, C.-L.; Liao, L.-S.; Chen, Y.-Y.; Chen, S.-J. Image quality and diagnostic accuracy of a handheld nonmydriatic fundus camera: Feasibility of a telemedical approach in screening retinal diseases. J. Chin. Med. Assoc. 2020, 83, 962–966. [Google Scholar] [CrossRef] [PubMed]
- Davila, J.R.; Sengupta, S.S.; Niziol, L.M.; Sindal, M.D.; Besirli, C.G.; Upadhyaya, S.; Woodward, M.A.; Venkatesh, R.; Robin, A.L.; Grubbs, J., Jr.; et al. Predictors of Photographic Quality with a Handheld Nonmydriatic Fundus Camera Used for Screening of Vision-Threatening Diabetic Retinopathy. Ophthalmologica 2017, 238, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Zhou, M.; Cao, Y.; Zheng, X.; Mao, H.; Lei, C.; Lin, W.; Jiang, J.; Chen, Y.; Song, D.; et al. Quality assessment of non-mydriatic fundus photographs for glaucoma screening in primary healthcare centres: A real-world study. BMJ Open Ophthalmol. 2023, 8, e001493. [Google Scholar] [CrossRef]
- Hark, L.A.; Myers, J.S.; Rahmatnejad, K.; Wang, Q.; Zhan, T.; Hegarty, S.E.; Leiby, B.E.; Udyaver, S.; Waisbourd, M.; Leite, S.; et al. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study: Analysis of Unreadable Fundus Images. J. Glaucoma 2018, 27, 999–1008. [Google Scholar] [CrossRef]
- Scanlon, P.H.; Foy, C.; Malhotra, R.; Aldington, S.J. The influence of age, duration of diabetes, cataract, and pupil size on image quality in digital photographic retinal screening. Diabetes Care 2005, 28, 2448–2453. [Google Scholar] [CrossRef]
- Cahill, M.; Eustace, P.; de Jesus, V. Pupillary autonomic denervation with increasing duration of diabetes mellitus. Br. J. Ophthalmol. 2001, 85, 1225–1230. [Google Scholar] [CrossRef] [PubMed]
- Mooren, R.R.M.S.M.V.d. Impact of intraocular lens design on anterior surface reflections. Investig. Ophthalmol. Vis. Sci. 2017, 58, 2724. [Google Scholar]
- Kymionis, G.D.; Kim, J.; Petrelli, M.; Grentzelos, M.A.; Hashemi, K.; Wagnières, G. Intraocular Lens Refractive Index and Its Impact on External Surface Reflections. J. Refract. Surg. 2021, 37, 398–402. [Google Scholar] [CrossRef] [PubMed]

| Variables | Male | Female | Total | p-Value |
|---|---|---|---|---|
| Number | 210 | 419 | 629 | |
| Age | 65.67 ± 16.01 | 63.77 ± 16.12 | 64.40 ± 16.10 | 0.163 |
| Age Group (n, %) | 0.183 | |||
| ≦20 years | 6 (2.9%) | 10 (2.4%) | 16 (2.5%) | |
| 21–30 years | 4 (1.9%) | 9 (2.1%) | 13 (2.1%) | |
| 31–40 years | 1 (0.5%) | 21 (5.0%) | 22 (3.5%) | |
| 41–50 years | 15 (7.1%) | 34 (8.1%) | 49 (7.8%) | |
| 51–60 years | 28 (13.3%) | 63 (15.0%) | 91 (14.5%) | |
| 61–70 years | 62 (29.5%) | 114 (27.2%) | 176 (28.0%) | |
| 71–80 years | 62 (29.5%) | 117 (27.9%) | 179 (28.5%) | |
| 81–90 years | 30 (14.3%) | 50 (11.9%) | 80 (12.7%) | |
| >90 years | 2 (1.0%) | 1 (0.2%) | 3 (0.5%) | |
| Referral (n, %) | 49 (23.3%) | 77 (18.4%) | 126 (20.0%) | 0.143 |
| Variables | Crude | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Age | 1.03 (1.02 to 1.04) | <0.001 * | 1.02 (1.01 to 1.03) | 0.004 * |
| Gender (M vs. F) | 1.31 (1.02 to 1.68) | 0.038 * | 1.19 (0.90 to 1.57) | 0.222 |
| Location | - | - | - | - |
| Chishang | 1.17 (0.83 to 1.65) | 0.375 | 0.91 (0.62 to 1.33) | 0.614 |
| Haiduan | 1.07 (0.76 to 1.50) | 0.707 | 1.47 (0.99 to 2.18) | 0.055 |
| Luye | 0.73 (0.52 to 1.02) | 0.066 | 0.82 (0.56 to 1.19) | 0.294 |
| Yanping | 0.87 (0.30 to 2.51) | 0.795 | 3.03 (0.99 to 9.18) | 0.051 |
| Guanshan | Reference | Reference | ||
| Pseudophakia | 4.19 (2.98 to 5.90) | <0.001 * | 4.06 (2.74 to 6.00) | <0.001 * |
| Cataract | 2.19 (1.71 to 2.81) | <0.001 * | 2.29 (1.69 to 3.11) | <0.001 * |
| Diabetes mellitus | 3.86 (2.95 to 5.07) | <0.001 * | 3.01 (2.25 to 4.01) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, T.-Y.; Wang, J.-H.; Chen, N.; Chiu, C.-J. The Assessment of Retinal Image Quality Using a Non-Mydriatic Fundus Camera in a Teleophthalmologic Platform. Diagnostics 2024, 14, 1543. https://doi.org/10.3390/diagnostics14141543
Chan T-Y, Wang J-H, Chen N, Chiu C-J. The Assessment of Retinal Image Quality Using a Non-Mydriatic Fundus Camera in a Teleophthalmologic Platform. Diagnostics. 2024; 14(14):1543. https://doi.org/10.3390/diagnostics14141543
Chicago/Turabian StyleChan, Tsung-Yueh, Jen-Hung Wang, Nancy Chen, and Cheng-Jen Chiu. 2024. "The Assessment of Retinal Image Quality Using a Non-Mydriatic Fundus Camera in a Teleophthalmologic Platform" Diagnostics 14, no. 14: 1543. https://doi.org/10.3390/diagnostics14141543
APA StyleChan, T.-Y., Wang, J.-H., Chen, N., & Chiu, C.-J. (2024). The Assessment of Retinal Image Quality Using a Non-Mydriatic Fundus Camera in a Teleophthalmologic Platform. Diagnostics, 14(14), 1543. https://doi.org/10.3390/diagnostics14141543







