Exploring Augmented Reality Integration in Diagnostic Imaging: Myth or Reality?
Abstract
1. Introduction
1.1. Augmented Reality: Origins and Definitions
1.2. Formulating the Research Hypothesis: Defining the Study’s Direction
1.2.1. Augmented Reality for Health
1.2.2. Augmented Reality Integration into Diagnostic Imaging
1.2.3. Augmented Reality Integration into Healthcare: The Contribution of COVID-19
- Facilitating training and knowledge dissemination: The COVID-19 outbreak simplified the training of healthcare professionals and the dissemination of knowledge through AR technology. This allowed for efficient skills acquisition and knowledge transfer, particularly in scenarios where traditional in-person training was limited due to the pandemic;
- Addressing staffing challenges: AR technology helped address staffing challenges by providing innovative solutions for training and empowering healthcare professionals to effectively manage patient care, even in the face of workforce shortages;
- Enhancing patient education: AR technology aided doctors in educating patients about their health issues, providing interactive and immersive experiences to enhance understanding and engagement;
- Utilizing AR and VR for communication and education: Virtual and augmented reality played a crucial role in communicating and disseminating knowledge about the COVID-19 disease. These technologies facilitated effective communication between healthcare providers and patients, as well as the general public, contributing to disease management and prevention efforts;
- Virtual rehabilitation and pain management: AR technology proved useful for virtual rehabilitation and pain management of infected patients during treatment, offering personalized interventions and immersive experiences to improve patient outcomes;
- Reducing face-to-face interactions: AR and VR technologies created a platform that lowered the amount of face-to-face interactions by clinicians with infected patients, thereby minimizing the risk of disease transmission and optimizing infection control measures;
- Improving surveillance systems: AR technology contributed to the improvement of the surveillance system of the ongoing situation through live video broadcasting, enabling real-time monitoring and data analysis to inform public health interventions;
- Exploring new opportunities in healthcare that have never been faced or thought of before [23].
1.3. The Rationale and the Purpose of This Study
- What do scholars mean by augmented reality in imaging applications and how do they perceive it?
- How has the integration of augmented reality in diagnostic imaging evolved over time?
- What significant advancements and challenges have shaped this intersection and what are the emerging themes/patterns?
- How has augmented reality been integrated in the imaging domain with other innovative technologies (e.g., robotics, artificial intelligence, and augmented reality)?
- In what ways has augmented reality demonstrated its potential to enhance diagnostic capabilities, improve medical training, or transform patient care within the field of radiology, and what are the current obstacles to overcome?
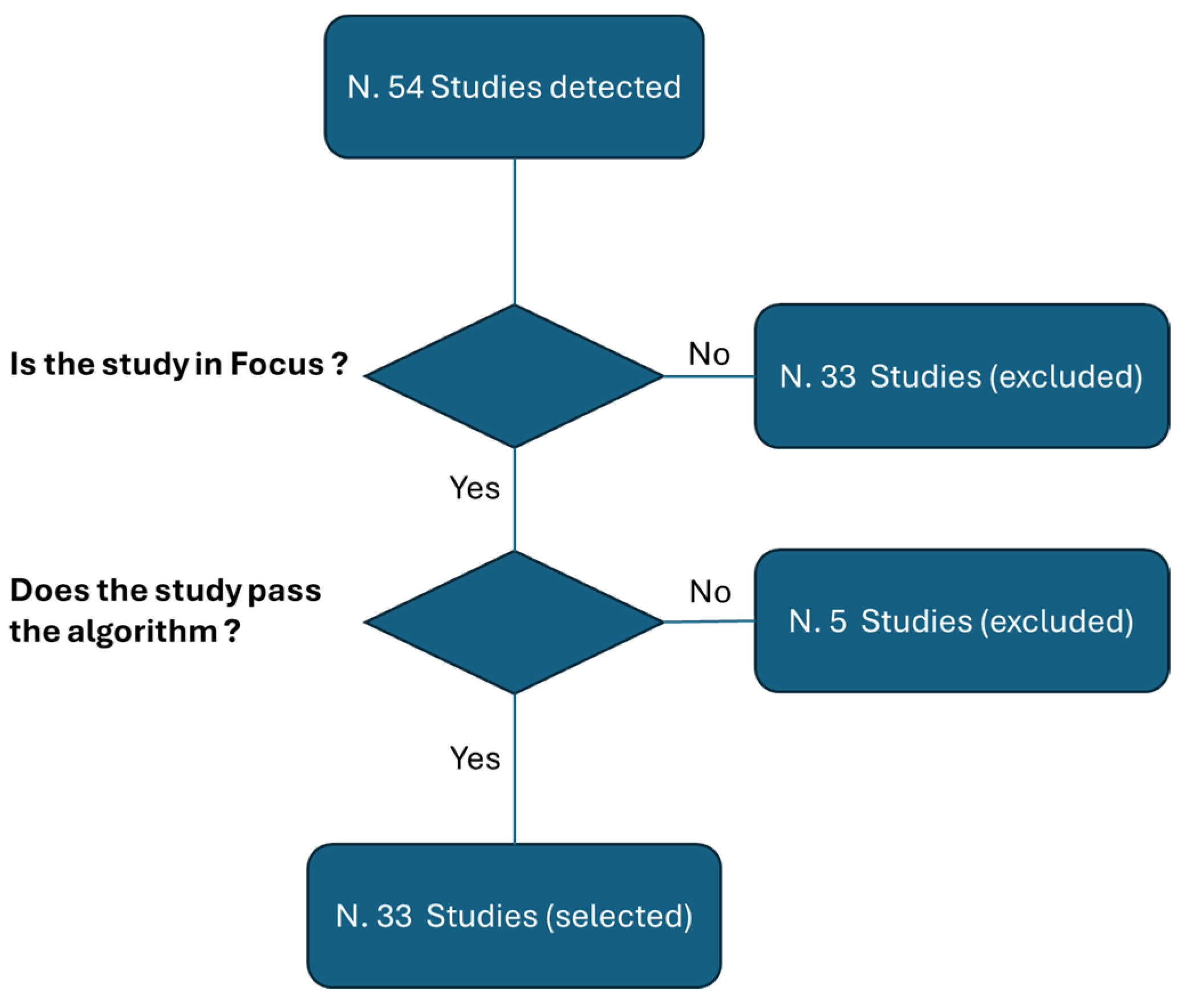
2. Methods
- The clarity of the study’s rationale as articulated in the introduction;
- An examination of the study design;
- Transparency in describing the methods employed;
- The clarity of the results;
- The alignment of the conclusions with the results;
- Finally, an examination of any potential conflicts of interest.
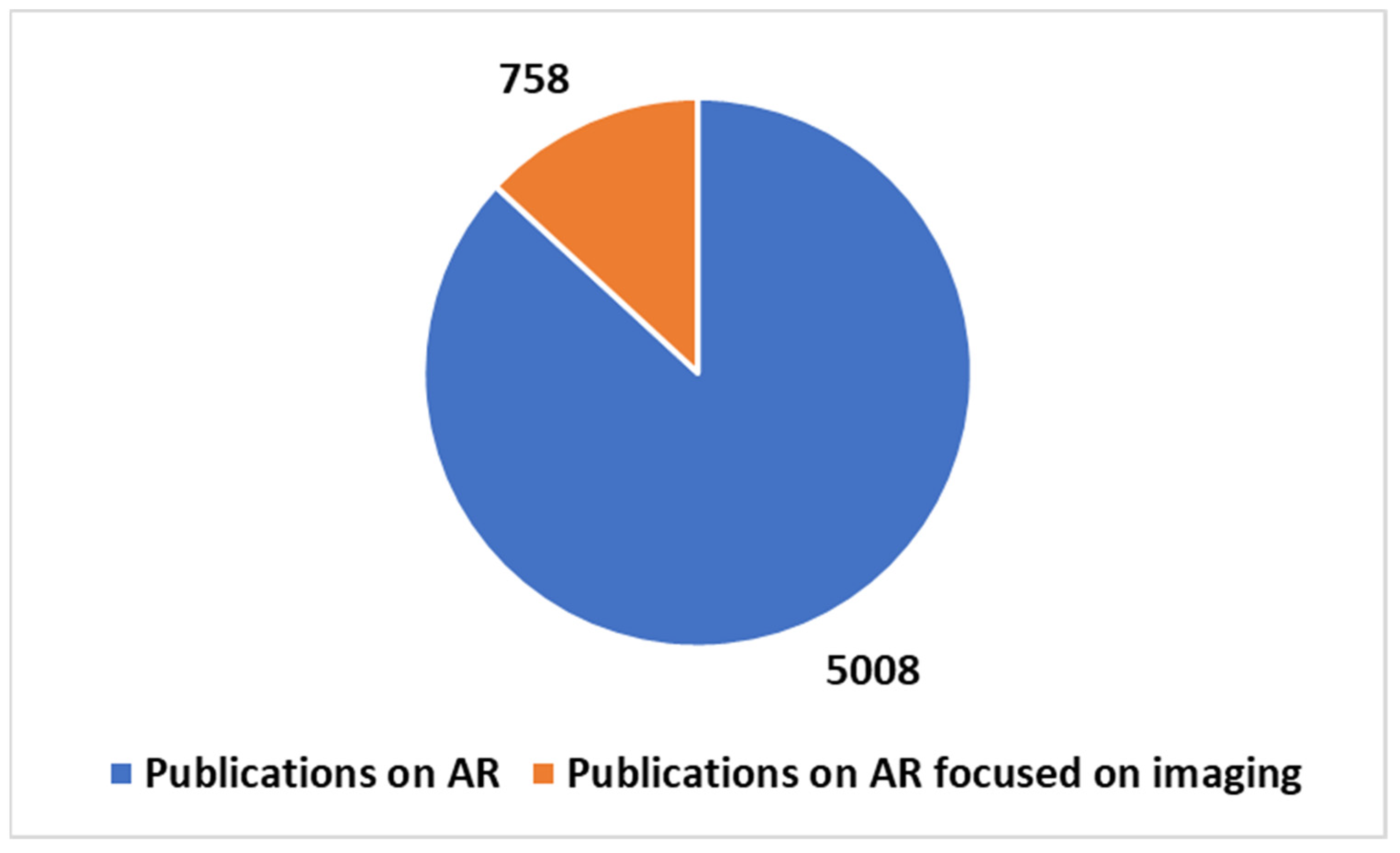
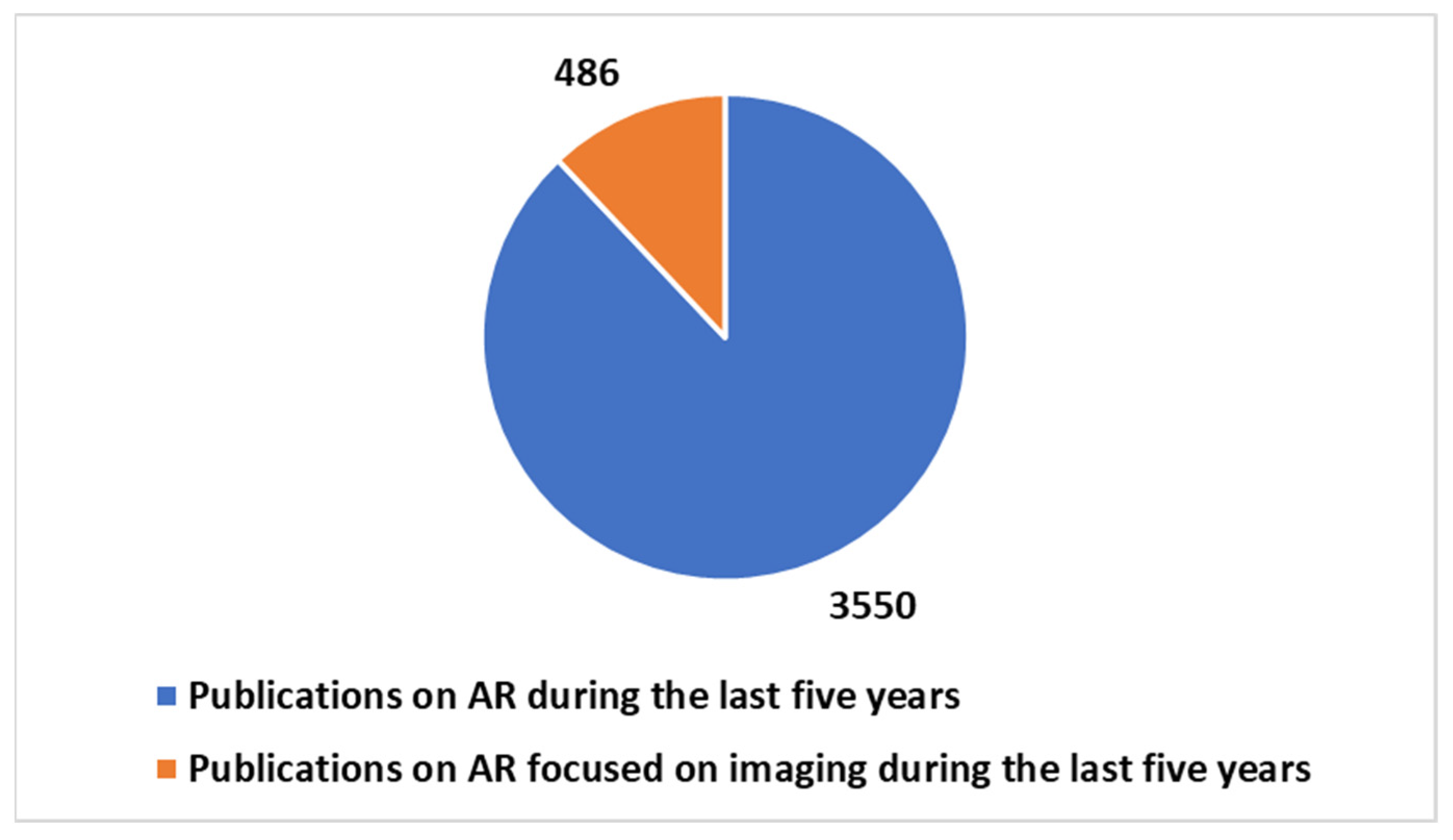
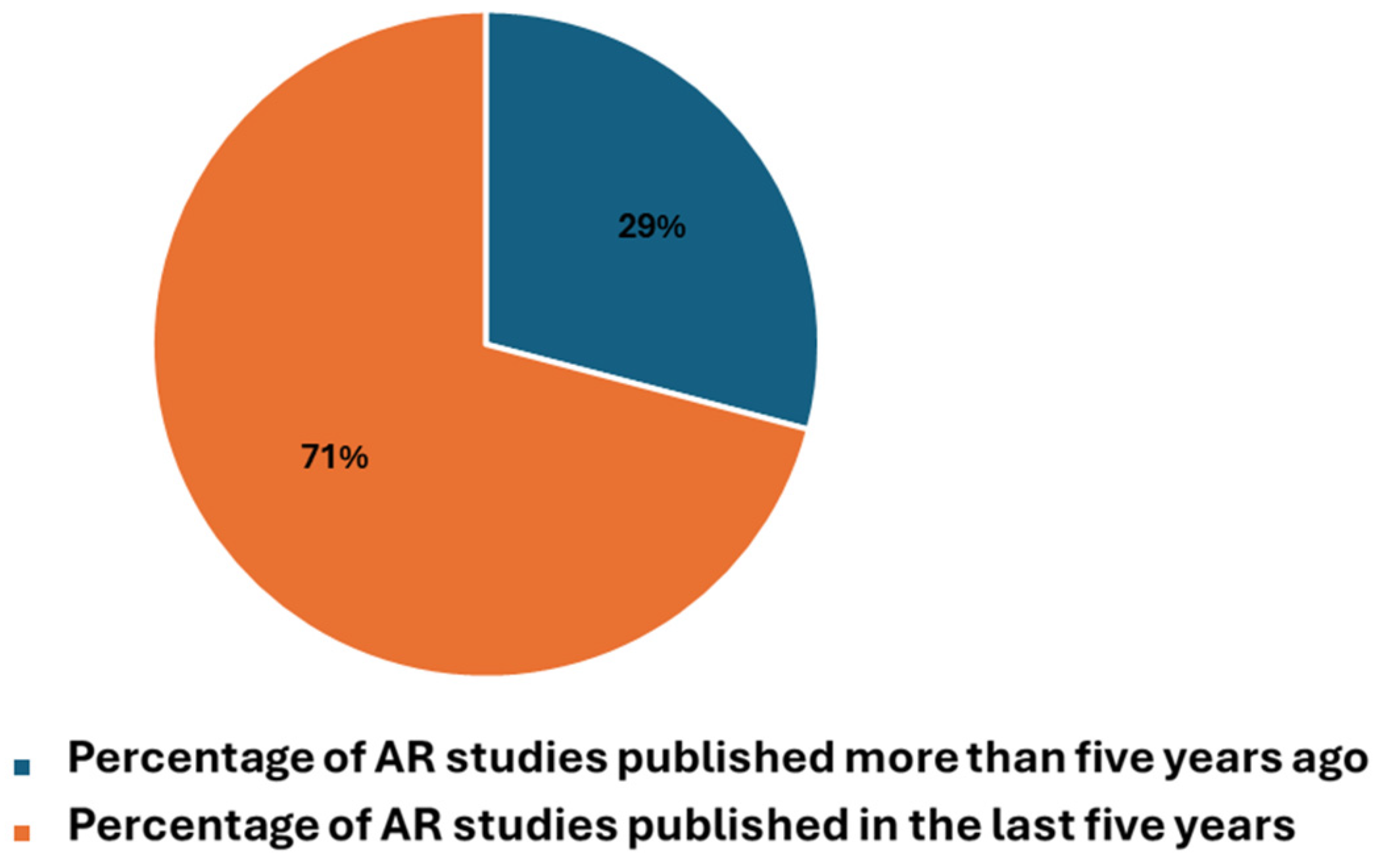
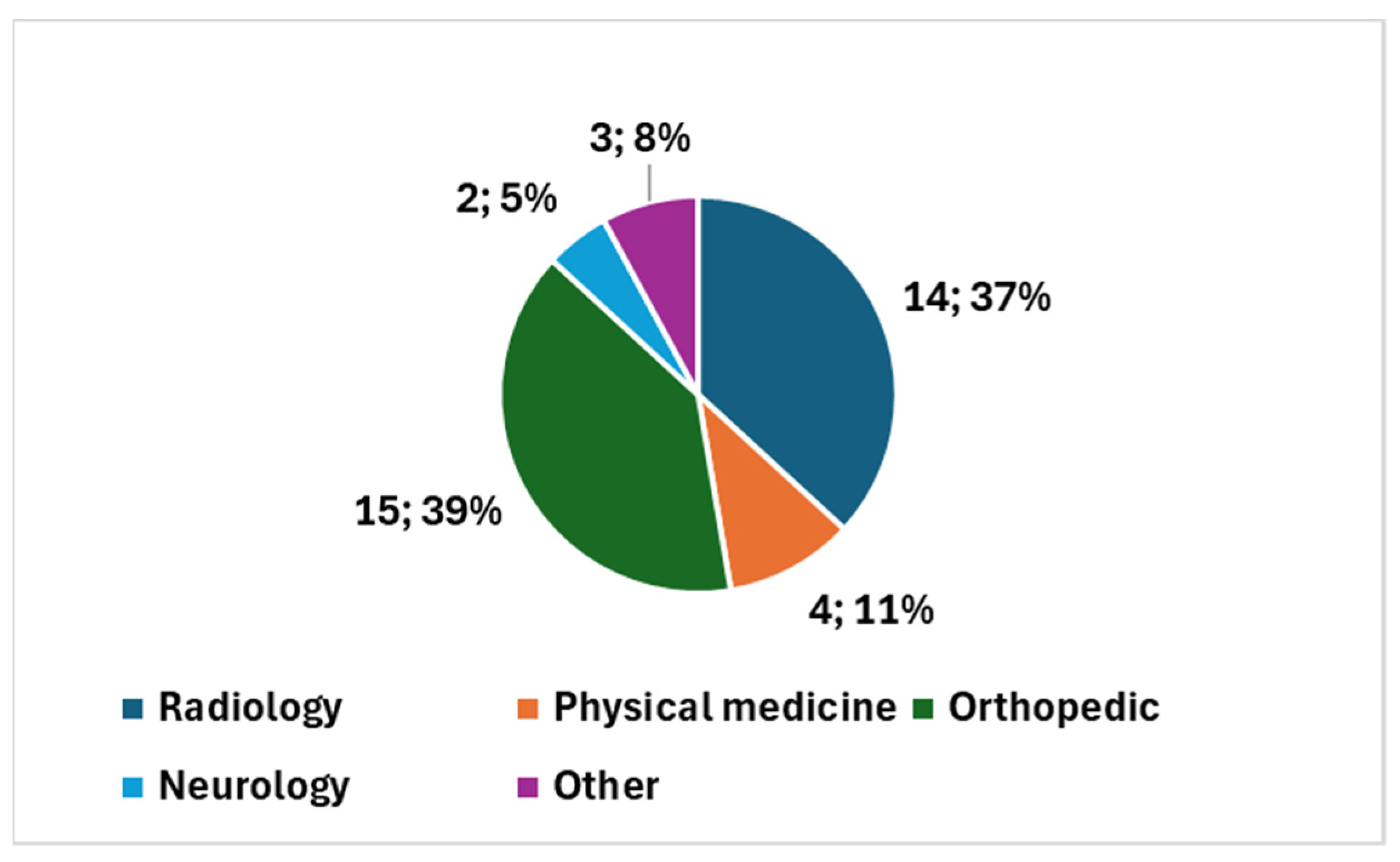
3. Results: Outcome from the Umbrella Review
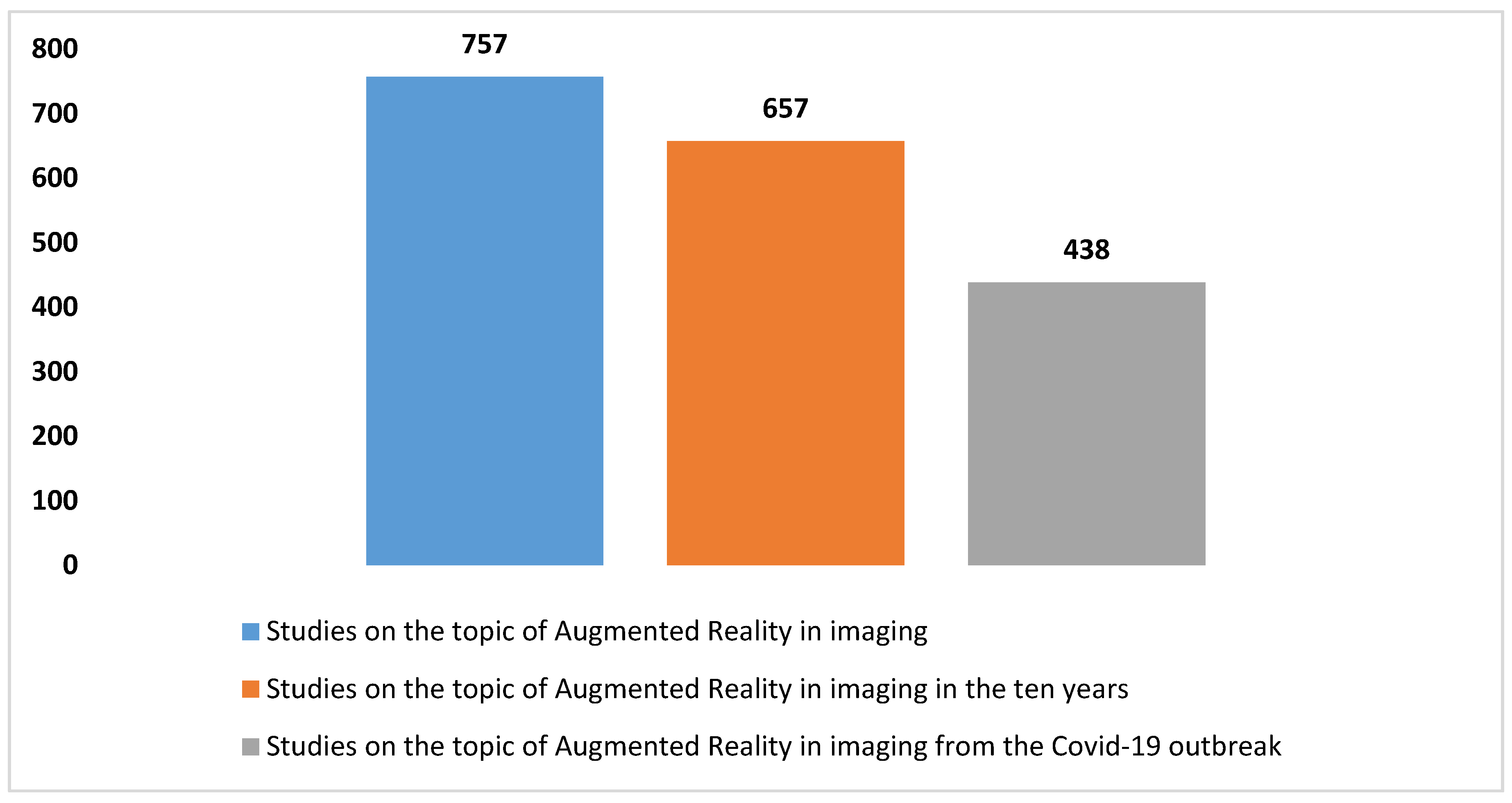
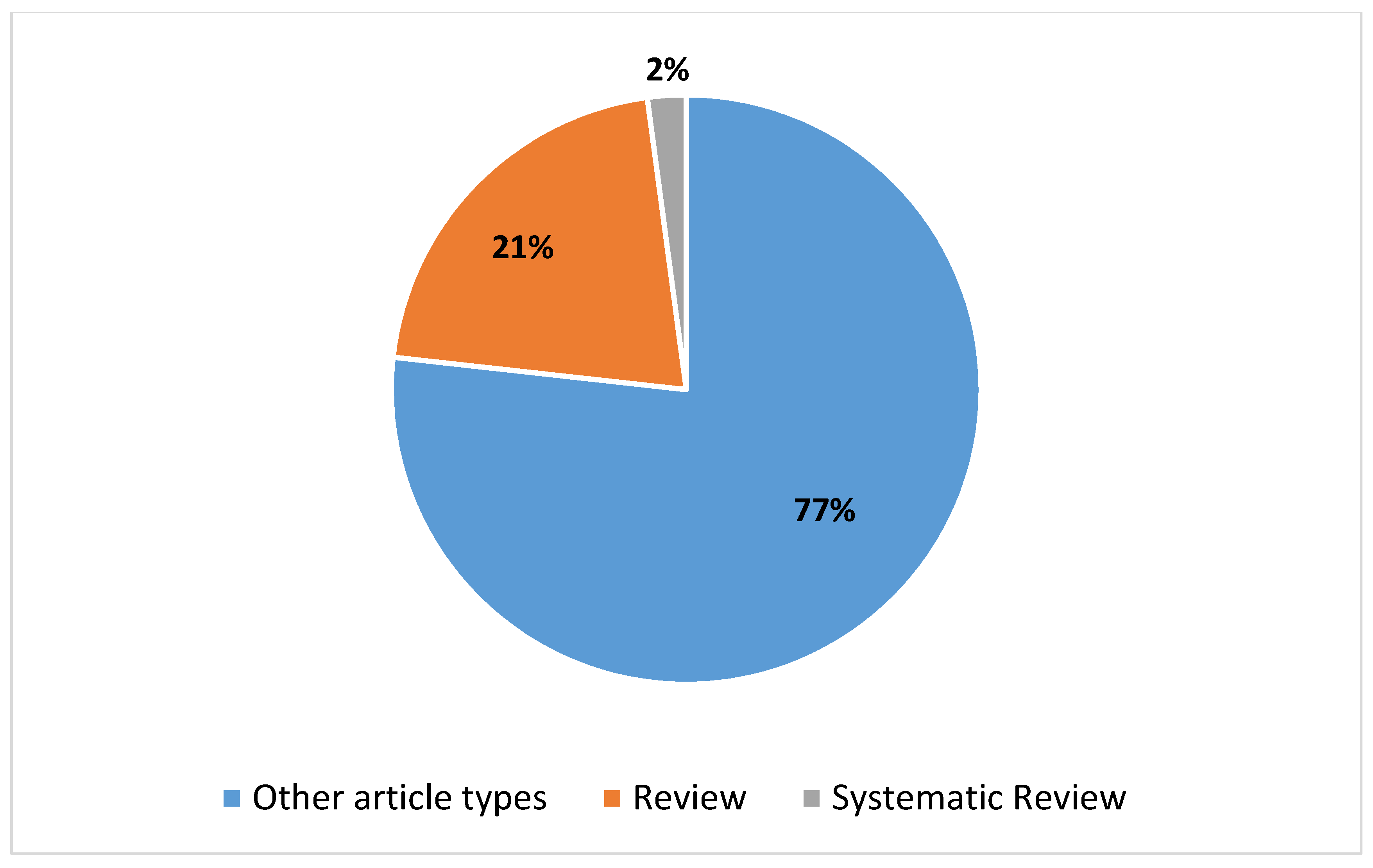
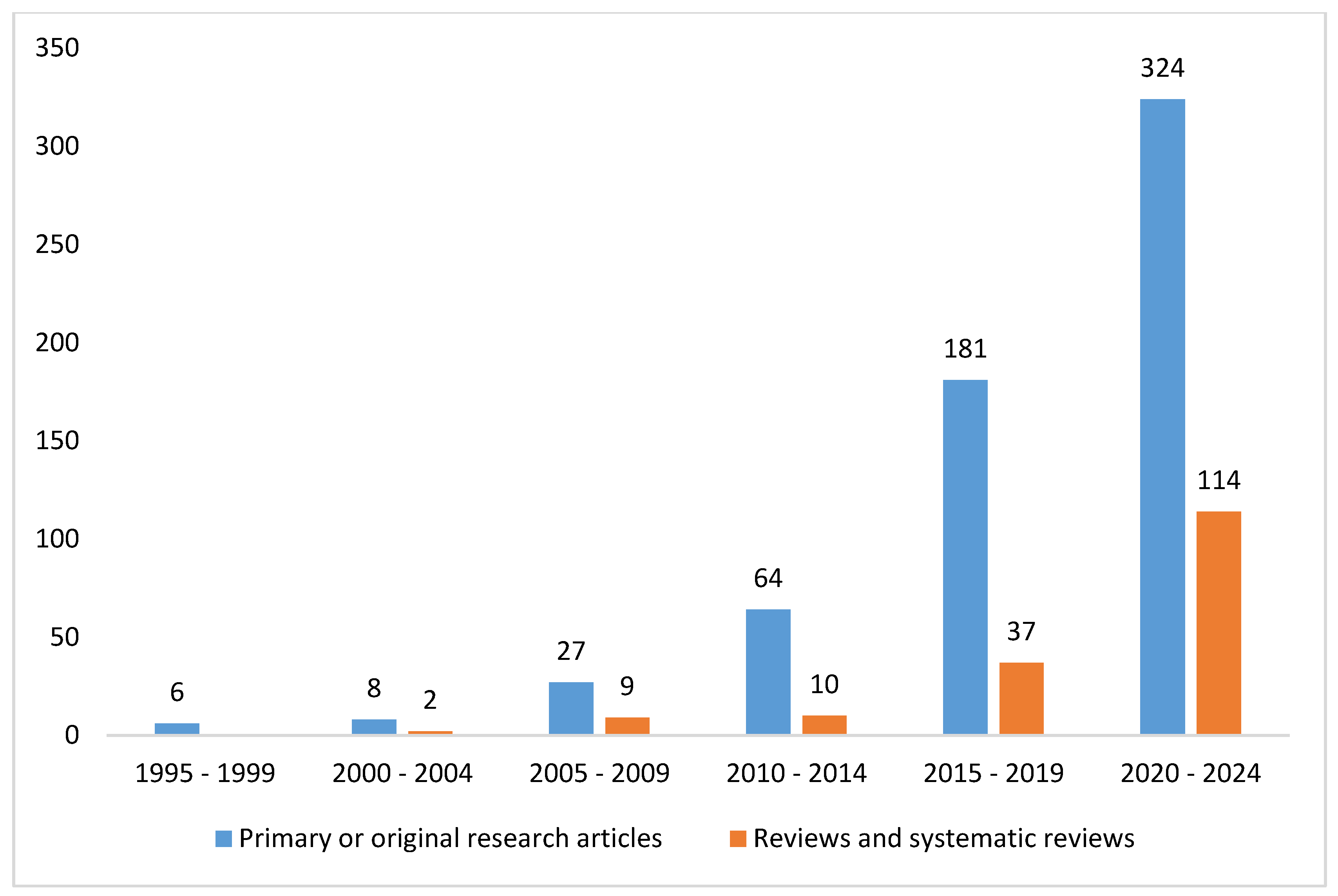
3.1. The Trends in the Studies on Augmented Reality Applications in Imaging
3.2. Outcome from the Umbrella Review of the Systematic Reviews
3.2.1. Qualitative Analysis of the Systematic Reviews
Common Message and Focus on AR and Diagnostic Imaging
Qualitative Analysis in Details
- Enhanced surgical preparation: VR and AR provide detailed preoperative simulations, leading to better preparedness and fewer intraoperative surprises;
- Real-time navigation: AR improves real-time guidance during surgery, enhancing accuracy and safety;
- Innovative rehabilitation: Postoperative use of VR and AR offers new methods for patient recovery, potentially speeding up rehabilitation and improving outcomes;
- Future prospects: The review suggests that AR can be integrated across different surgical stages to improve patient outcomes and overall surgical efficacy;
- The need for further research: The review emphasizes the necessity for additional comparative studies to evaluate the clinical outcomes and cost effectiveness comprehensively.
- Advanced training tools: VR and AR provide sophisticated training environments for ICU staff, allowing them to practice complex procedures without risks;
- Patient care: These technologies offer immersive experiences that reduce patient anxiety and pain, promoting better mental health and faster recovery;
- Rehabilitation: VR and AR present engaging and effective methods for patient rehabilitation;
- Growing adoption: The review anticipates an increase in the use of VR and AR in ICU settings due to their potential to improve both patient care and staff training.
- Precision in surgery: AR provides accurate overlays of anatomical information, enhancing the precision of neurosurgical procedures;
- Technological challenges: The current limitations include registration errors and synchronization issues between visual and tactile feedback;
- Future improvements: Advances in imaging, registration accuracy, and robotic integration could significantly enhance AR’s utility in neurosurgery.
- Preoperative planning: AR enhances the accuracy of surgical incisions and the identification of deep anatomical structures;
- Educational benefits: VR offers superior visualization of craniofacial trauma, benefiting surgeon training and education;
- Technological advancements: AR supports precise orientation and fixation of reconstruction plates and patient-specific implants;
- Accuracy margin: A technical accuracy margin of 2–3 mm must be considered for AR applications.
- Enhanced robotics: Combining AR with robotic systems improves precision, especially in challenging areas, such as tool placement and depth perception;
- Imaging integration: Advanced imaging and deep learning algorithms play crucial roles in overcoming surgical obstacles;
- Technological synergy: The review highlights the importance of integrating AR with advanced control features to enhance surgical outcomes.
- Imaging enhancements: Combining MRI, PSMA-PET CT, and other modalities with RARP improves precision and outcomes;
- Training advances: Advanced imaging technologies enhance surgeon training, improving preparation and skill development;
- Prospective studies: The review underscores the need for prospective studies to confirm the benefits of these combined approaches.
- Intraoperative visualization: AR offers advanced tools that improve the accuracy and guidance of neurosurgical procedures;
- Technological challenges: Issues like MRI brain segmentation, brain shifts, and coregistration errors need addressing for effective AR use;
- Future integration: Combining AR with artificial intelligence and multimodal imaging could further enhance neurosurgical outcomes.
- Surgical applications: AR applications include heads-up guided surgery, semi-transparent screens, direct image projection, and data transfer to monitors;
- High precision: AR provides high accuracy in maxillofacial surgery with minimal errors;
- Technological diversity: The review showcases different AR tools and methods, highlighting the diversity in technological approaches.
- Enhanced training: AR and VR offer immersive training tools, improving educational methods for surgeons;
- Clinical validation: Rigorous trials are needed to validate the benefits of AR and VR in surgical practice;
- Future developments: Potential advancements include AR-based imaging overlays and expanded remote guidance through telementoring.
- Educational tools: ER technologies improve training in ophthalmology, offering better visualization and a better understanding of procedures;
- Diagnostic advances: Enhanced imaging capabilities support more accurate diagnostics and assessments of ocular diseases;
- Therapeutic applications: ER technologies could improve therapeutic outcomes, though higher quality comparative studies are needed.
- Complex surgeries: AR enhances precision in complex spinal surgeries, offering improved outcomes;
- Case studies: Practical insights from case studies demonstrate AR’s potential in real-world applications;
- Technological challenges: Addressing issues like spinal deformities and instability are crucial for effective AR use in spinal surgeries.
- Head-mounted displays: OST-HMDs offer potential benefits in surgical navigation, improving precision and the user experience;
- System accuracy: Despite promising results, issues with accuracy and user perceptions need to be addressed;
- Technological advancements: Improvements in regard to interaction and perception are essential for the wider adoption of OST-HMDs in surgery.
- AI integration: AI enhances surgical training by improving preoperative preparation and intraoperative guidance;
- Ethical concerns: Addressing privacy, bias, and ethical issues are crucial for widespread AI adoption;
- Technological challenges: Improving real-time tracking and its integration with AR technologies is essential for optimizing AI’s role in surgery.
- Segmentation techniques: Machine learning advancements improve automatic segmentation of brain AVMs;
- Visualization tools: Innovative methods are required to enhance the visualization and management of AVMs;
- Technological potential: Continued development could significantly improve the characterization and treatment of AVMs.
- Three-dimensional Printing: 3D printing provides benefits in simulations, patient counseling, and precise preoperative planning;
- Material limitations: Issues like cost and the quality of materials need to be addressed for broader application;
- Virtual imaging: Virtual imaging enhances the accuracy of preoperative planning and supports better surgical outcomes.
- Navigation techniques: AR and VR improve navigation and visualization during minimally invasive surgeries, enhancing precision and safety;
- Machine learning: Machine learning offers promising solutions for overcoming registration challenges and improving surgical outcomes;
- Future research: Continued research and development are needed to address the current limitations and fully realize the potential of these technologies in surgery.
3.2.2. Comparative Analysis of the Systematic Reviews and Emerging Themes
4. Discussion: Illuminating the Highlights, Potential, Limitations, and Complementation of the Overview
4.1. Early Insights and Highlights
4.2. Emerging Potential
4.2.1. General Potential in Imaging Integration
4.2.2. Enhancing Integration Potential with Other Innovative Technologies in Imaging Applications
4.3. The Need for Broader Investigations
4.3.1. The Need for Broader Investigations in Specific Areas
4.3.2. Key Focus Areas for Broader Exploration in AR Applications in Imaging
4.4. Comprehensive Discussion on Harmonization and Alignment of Regulation
4.4.1. Standardization of Imaging in Digital Pathology and Radiology and the Impact on AR Integration
4.4.2. Trends in the Integration of Augmented Reality Medical Devices within the Health Domain
Trends
Approval as a Medical Device
4.4.3. Key Considerations on Harmonization and Alignments in Terms of Regulation
4.5. Takeaway Message
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Available online: https://www.merriam-webster.com/dictionary/augmented%20reality (accessed on 13 May 2024).
- Available online: https://dictionary.cambridge.org/dictionary/english/augmented-reality (accessed on 13 May 2024).
- Available online: https://www.oxfordlearnersdictionaries.com/definition/english/augmented-reality (accessed on 13 May 2024).
- Vaughan-Nichols, S.J. Augmented Reality: No Longer a Novelty? Computer 2009, 42, 19–22. [Google Scholar] [CrossRef]
- Leue, M.C.; Jung, T.; tom Dieck, D. Google Glass Augmented Reality: Generic Learning Outcomes for Art Galleries. In Information and Communication Technologies in Tourism 2015; Tussyadiah, I., Inversini, A., Eds.; Springer: Cham, Switzerland, 2015. [Google Scholar] [CrossRef]
- Fang, W.; Zhang, T.; Chen, L.; Hu, H. A survey on HoloLens AR in support of human-centric intelligent manufacturing. J. Intell. Manuf. 2023, 1–25. [Google Scholar] [CrossRef]
- Chwalek, P.; Zhong, S.; Ramsay, D.; Perry, N.; Paradiso, J. AirSpec: A Smart Glasses Platform, Tailored for Research in the Built Environment. In Adjunct Proceedings of the 2023 ACM International Joint Conference on Pervasive and Ubiquitous Computing & the 2023 ACM International Symposium on Wearable Computing, Cancun, Mexico, 8–12 October 2023; ACM: New York, NY, USA, 2023; 204p. [Google Scholar]
- Wu, T.; Xia, Z.; Zhou, M.; Kong, L.; Chen, Z. AMENet is a monocular depth estimation network designed for automatic stereoscopic display. Sci. Rep. 2024, 14, 5868. [Google Scholar] [CrossRef]
- Camba, J.; Contero, M.; Salvador-Herranz, G. Desktop vs. mobile: A comparative study of augmented reality systems for engineering visualizations in education. In Proceedings of the 2014 IEEE Frontiers in Education Conference (FIE), Madrid, Spain, 22–25 October 2014; pp. 1–8. [Google Scholar] [CrossRef]
- Dhar, P.; Rocks, T.; Samarasinghe, R.M.; Stephenson, G.; Smith, C. Augmented reality in medical education: Students’ experiences and learning outcomes. Med. Educ. Online 2021, 26, 1953953. [Google Scholar] [CrossRef]
- George, O.; Foster, J.; Xia, Z.; Jacobs, C. Augmented Reality in Medical Education: A Mixed Methods Feasibility Study. Cureus 2023, 15, e36927. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aliwi, I.; Schot, V.; Carrabba, M.; Duong, P.; Shievano, S.; Caputo, M.; Wray, J.; de Vecchi, A.; Biglino, G. The Role of Immersive Virtual Reality and Augmented Reality in Medical Communication: A Scoping Review. J. Patient Exp. 2023, 10, 23743735231171562. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dinh, A.; Yin, A.L.; Estrin, D.; Greenwald, P.; Fortenko, A. Augmented Reality in Real-time Telemedicine and Telementoring: Scoping Review. JMIR Mhealth Uhealth 2023, 11, e45464. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sadek, O.; Baldwin, F.; Gray, R.; Khayyat, N.; Fotis, T. Impact of Virtual and Augmented Reality on Quality of Medical Education During the COVID-19 Pandemic: A Systematic Review. J. Grad. Med. Educ. 2023, 15, 328–338. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eckert, M.; Volmerg, J.S.; Friedrich, C.M. Augmented Reality in Medicine: Systematic and Bibliographic Review. JMIR Mhealth Uhealth 2019, 7, e10967. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murali, S.; Paul, K.D.; McGwin, G.; Ponce, B.A. Updates to the Current Landscape of Augmented Reality in Medicine. Cureus 2021, 13, e15054. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://medicalfuturist.com/augmented-reality-in-healthcare-will-be-revolutionary/ (accessed on 13 May 2024).
- Kukla, P.; Maciejewska, K.; Strojna, I.; Zapał, M.; Zwierzchowski, G.; Bąk, B. Extended Reality in Diagnostic Imaging—A Literature Review. Tomography 2023, 9, 1071–1082. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://vestarad.com/the-future-of-medical-imaging-latest-augmented-reality-advancements/ (accessed on 13 May 2024).
- Douglas, D.B.; Wilke, C.A.; Gibson, J.D.; Boone, J.M.; Wintermark, M. Augmented Reality: Advances in Diagnostic Imaging. Multimodal Technol. Interact. 2017, 1, 29. [Google Scholar] [CrossRef]
- Baker, J.; Antypas, A.; Aggarwal, P.; Elliott, C.; Baxter, R.; Singh, S.; Jayasinghe, N.; Reed, D.; Boden, A.; Evans, I.; et al. Augmented Reality in Interventional Radiology: Transforming Training Paradigms. Cureus 2024, 16, e54907. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://www.towardshealthcare.com/insights/augmented-and-virtual-reality-in-healthcare-market (accessed on 13 May 2024).
- Jung, S.; Moon, Y.; Kim, J.; Kim, K. Deep Neural Network-Based Visual Feedback System for Nasopharyngeal Swab Sampling. Sensors 2023, 23, 8443. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giansanti, D. Advancing Dermatological Care: A Comprehensive Narrative Review of Tele-Dermatology and mHealth for Bridging Gaps and Expanding Opportunities beyond the COVID-19 Pandemic. Healthcare 2023, 11, 1911. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsai, T.Y.; Onuma, Y.; Złahoda-Huzior, A.; Kageyama, S.; Dudek, D.; Wang, Q.; Lim, R.P.; Garg, S.; Poon, E.K.W.; Puskas, J.; et al. Merging virtual and physical experiences: Extended realities in cardiovascular medicine. Eur. Heart J. 2023, 44, 3311–3322. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wisotzky, E.L.; Rosenthal, J.C.; Meij, S.; van den Dobblesteen, J.; Arens, P.; Hilsmann, A.; Eisert, P.; Uecker, F.C.; Schneider, A. Telepresence for surgical assistance and training using eXtended reality during and after pandemic periods. J. Telemed. Telecare, 2023; epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Saed, A. A Systematic Review of the Medical Student Feedback on Undergraduate Surgical Education During the Pandemic. Cureus 2022, 14, e30440. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shao, M.Y.; Vagg, T.; Seibold, M.; Doughty, M. Towards a Low-Cost Monitor-Based Augmented Reality Training Platform for At-Home Ultrasound Skill Development. J. Imaging 2022, 8, 305. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Di Martino, F.; Orciuoli, F. A computational framework to support the treatment of bedsores during COVID-19 diffusion. J. Ambient. Intell. Humaniz. Comput. 2022, 15, 219–229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morimoto, T.; Hirata, H.; Ueno, M.; Fukumori, N.; Sakai, T.; Sugimoto, M.; Kobayashi, T.; Tsukamoto, M.; Yoshihara, T.; Toda, Y.; et al. Digital Transformation Will Change Medical Education and Rehabilitation in Spine Surgery. Medicina 2022, 58, 508. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Benbelkacem, S.; Oulefki, A.; Agaian, S.; Zenati-Henda, N.; Trongtirakul, T.; Aouam, D.; Masmoudi, M.; Zemmouri, M. COVI3D: Automatic COVID-19 CT Image-Based Classification and Visualization Platform Utilizing Virtual and Augmented Reality Technologies. Diagnostics 2022, 12, 649. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Noël, J.; Moschovas, M.C.; Patel, E.; Rogers, T.; Marquinez, J.; Rocco, B.; Mottrie, A.; Patel, V. Step-by-step optimisation of robotic-assisted radical prostatectomy using augmented reality. Int. Braz. J. Urol. 2022, 48, 600–601. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kassutto, S.M.; Baston, C.; Clancy, C. Virtual, Augmented, and Alternate Reality in Medical Education: Socially Distanced but Fully Immersed. ATS Sch. 2021, 2, 651–664. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morimoto, T.; Kobayashi, T.; Hirata, H.; Otani, K.; Sugimoto, M.; Tsukamoto, M.; Yoshihara, T.; Ueno, M.; Mawatari, M. XR (Extended Reality: Virtual Reality, Augmented Reality, Mixed Reality) Technology in Spine Medicine: Status Quo and Quo Vadis. J. Clin. Med. 2022, 11, 470. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Okawa, A. Near future image of orthopedics after COVID-19 pandemic. J. Orthop. Sci. 2022, 27, 297–298. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bartal, G.; Vano, E.; Paulo, G. Get Protected! Recommendations for Staff in IR. Cardiovasc. Interv. Radiol. 2021, 44, 871–876. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tai, Y.; Gao, B.; Li, Q.; Yu, Z.; Zhu, C.; Chang, V. Trustworthy and Intelligent COVID-19 Diagnostic IoMT Through XR and Deep-Learning-Based Clinic Data Access. IEEE Internet Things J. 2021, 8, 15965–15976. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tai, Y.; Qian, K.; Huang, X.; Zhang, J.; Jan, M.A.; Yu, Z. Intelligent Intraoperative Haptic-AR Navigation for COVID-19 Lung Biopsy Using Deep Hybrid Model. IEEE Trans. Ind. Inform. 2021, 17, 6519–6527. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- ANDJ Checklist. Available online: https://www.elsevier.com/__data/promis_misc/ANDJ%20Narrative%20Review%20Checklist.pdf (accessed on 3 June 2023).
- Giansanti, D. An Overview of the Fusion of fMRI and AI in Autism. Diagnostics 2023, 13, 3552. [Google Scholar] [CrossRef]
- Sun, P.; Zhao, Y.; Men, J.; Ma, Z.R.; Jiang, H.Z.; Liu, C.Y.; Feng, W. Application of Virtual and Augmented Reality Technology in Hip Surgery: Systematic Review. J. Med. Internet Res. 2023, 25, e37599. [Google Scholar] [CrossRef] [PubMed]
- Kanschik, D.; Bruno, R.R.; Wolff, G.; Kelm, M.; Jung, C. Virtual and augmented reality in intensive care medicine: A systematic review. Ann. Intensive Care 2023, 13, 81. [Google Scholar] [CrossRef] [PubMed]
- Guha, D.; Alotaibi, N.M.; Nguyen, N.; Gupta, S.; McFaul, C.; Yang, V.X.D. Augmented Reality in Neurosurgery: A Review of Current Concepts and Emerging Applications. The Canadian journal of neurological sciences. J. Can. Sci. Neurol. 2017, 44, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Dubron, K.; Verbist, M.; Jacobs, R.; Olszewski, R.; Shaheen, E.; Willaert, R. Augmented and Virtual Reality for Preoperative Trauma Planning, Focusing on Orbital Reconstructions: A Systematic Review. J. Clin. Med. 2023, 12, 5203. [Google Scholar] [CrossRef] [PubMed]
- Seetohul, J.; Shafiee, M.; Sirlantzis, K. Augmented Reality (AR) for Surgical Robotic and Autonomous Systems: State of the Art, Challenges, and Solutions. Sensors 2023, 23, 6202. [Google Scholar] [CrossRef]
- Rodler, S.; Kidess, M.A.; Westhofen, T.; Kowalewski, K.F.; Belenchon, I.R.; Taratkin, M.; Puliatti, S.; Gómez Rivas, J.; Veccia, A.; Piazza, P.; et al. A Systematic Review of New Imaging Technologies for Robotic Prostatectomy: From Molecular Imaging to Augmented Reality. J. Clin. Med. 2023, 12, 5425. [Google Scholar] [CrossRef] [PubMed]
- Chidambaram, S.; Stifano, V.; Demetres, M.; Teyssandier, M.; Palumbo, M.C.; Redaelli, A.; Olivi, A.; Apuzzo, M.L.J.; Pannullo, S.C. Applications of augmented reality in the neurosurgical operating room: A systematic review of the literature. J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas. 2021, 91, 43–61. [Google Scholar] [CrossRef] [PubMed]
- Bosc, R.; Fitoussi, A.; Hersant, B.; Dao, T.H.; Meningaud, J.P. Intraoperative augmented reality with heads-up displays in maxillofacial surgery: A systematic review of the literature and a classification of relevant technologies. Int. J. Oral Maxillofac. Surg. 2019, 48, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Sparwasser, P.M.; Schoeb, D.; Miernik, A.; Borgmann, H. Augmented Reality und Virtual Reality im Operationssaal—Status Quo und Quo vadis [Augmented reality and virtual reality in the operating theatre status quo und quo vadis]. Aktuelle Urol. 2018, 49, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.W.; Tan, M.C.J.; Lam, M.; Koh, V.T.C. Applications of Extended Reality in Ophthalmology: Systematic Review. J. Med. Internet Res. 2021, 23, e24152. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Umana, G.E.; Scalia, G.; Spitaleri, A.; Passanisi, M.; Crea, A.; Tomasi, O.S.; Cicero, S.; Maugeri, R.; Iacopino, D.G.; Visocchi, M. Multilevel Corpectomy for Subaxial Cervical Spondylodiscitis: Literature Review and Role of Navigation, Intraoperative Imaging and Augmented Reality. Acta Neurochir. Suppl. 2023, 135, 331–338. [Google Scholar] [CrossRef]
- Doughty, M.; Ghugre, N.R.; Wright, G.A. Augmenting Performance: A Systematic Review of Optical See-Through Head-Mounted Displays in Surgery. J. Imaging 2022, 8, 203. [Google Scholar] [CrossRef]
- Rodriguez Peñaranda, N.; Eissa, A.; Ferretti, S.; Bianchi, G.; Di Bari, S.; Farinha, R.; Piazza, P.; Checcucci, E.; Belenchón, I.R.; Veccia, A.; et al. Artificial Intelligence in Surgical Training for Kidney Cancer: A Systematic Review of the Literature. Diagnostics 2023, 13, 3070. [Google Scholar] [CrossRef]
- Colombo, E.; Fick, T.; Esposito, G.; Germans, M.; Regli, L.; van Doormaal, T. Segmentation techniques of brain arteriovenous malformations for 3D visualization: A systematic review. Radiol. Med. 2022, 127, 1333–1341. [Google Scholar] [CrossRef]
- Checcucci, E.; De Cillis, S.; Porpiglia, F. 3D-printed models and virtual reality as new tools for image-guided robot-assisted nephron-sparing surgery: A systematic review of the newest evidences. Curr. Opin. Urol. 2020, 30, 55–64. [Google Scholar] [CrossRef]
- Unberath, M.; Gao, C.; Hu, Y.; Judish, M.; Taylor, R.H.; Armand, M.; Grupp, R. The Impact of Machine Learning on 2D/3D Registration for Image-Guided Interventions: A Systematic Review and Perspective. Front. Robot. AI 2021, 8, 716007. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Deodato, M.; Qualizza, C.; Martini, M.; Mazzari, L.; Furlanis, G.; Buoite Stella, A.; Manganotti, P. Efficacy of dual-task augmented reality rehabilitation in non-hospitalized adults with self-reported long COVID fatigue and cognitive impairment: A pilot study. Neurol. Sci. 2024, 45, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
- Housand, J.; Cornelius, A.; Shackleford, K.E. Greater usage and positive mood change for users of a dynamic VR app before and after the COVID-19 pandemic onset. Front. Psychol. 2024, 15, 1278207. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bumm, R.; Zaffino, P.; Lasso, A.; Estépar, R.S.J.; Pieper, S.; Wasserthal, J.; Spadea, M.F.; Latshang, T.; Kawel-Boehm, N.; Wäckerlin, A.; et al. Artificial intelligence (AI)-assisted chest computer tomography (CT) insights: A study on intensive care unit (ICU) admittance trends in 78 coronavirus disease 2019 (COVID-19) patients. J. Thorac. Dis. 2024, 16, 1009–1020. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tukur, M.; Saad, G.; AlShagathrh, F.M.; Househ, M.; Agus, M. Telehealth interventions during COVID-19 pandemic: A scoping review of applications, challenges, privacy and security issues. BMJ Health Care Inform. 2023, 30, e100676. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arntz, A.; Weber, F.; Handgraaf, M.; Lällä, K.; Korniloff, K.; Murtonen, K.P.; Chichaeva, J.; Kidritsch, A.; Heller, M.; Sakellari, E.; et al. Technologies in Home-Based Digital Rehabilitation: Scoping Review. JMIR Rehabil. Assist. Technol. 2023, 10, e43615. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, G.J.; Kang, H. The overview: A useful strategy in the rain of evidence. Korean J. Pain 2022, 35, 127–128. [Google Scholar] [CrossRef]
- Which Review Is That? A Guide to Review Types. Available online: https://unimelb.libguides.com/whichreview/umbrellareview (accessed on 13 May 2024).
- Molinaro, R.; Pirrera, A.; Renzoni, A. Special Applications of Medical Tattooing: Contouring and 3D Exemplified by Tattooing of the Nailbed and the Gingiva. Curr. Probl. Dermatol. 2022, 56, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Alexander, M.D. The future of digital dermatology. Clin. Exp. Dermatol. 2021, 46, 740–741. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.dicomstandard.org/ (accessed on 13 May 2024).
- Pirrera, A.; Giansanti, D. Human–Machine Collaboration in Diagnostics: Exploring the Synergy in Clinical Imaging with Artificial Intelligence. Diagnostics 2023, 13, 2162. [Google Scholar] [CrossRef]
- DICOM Whole Slide Imaging (WSI). NEMA. Available online: http://dicom.nema.org/Dicom/DICOMWSI/ (accessed on 13 May 2024).
- Giansanti, D.; Grigioni, M.; D’Avenio, G.; Morelli, S.; Maccioni, G.; Bondi, A.; Giovagnoli, M.R. Virtual microscopy and digital cytology: State of the art. Annali dell’Istituto Superiore di Sanità 2010, 46, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Kahn, C.E., Jr.; Carrino, J.A.; Flynn, M.J.; Peck, D.J.; Horii, S.C. DICOM and radiology: Past, present, and future. J. Am. Coll. Radiol. 2007, 4, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Hu, G.; Yan, J.; Li, D. Analysis of DICOM and its application in teleradiology. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 2003, 20, 171–174. (In Chinese) [Google Scholar] [PubMed]
- Lastrucci, A.; Giansanti, D. Radiological Crossroads: Navigating the Intersection of Virtual Reality and Digital Radiology through a Comprehensive Narrative Review of Reviews. Robotics 2024, 13, 69. [Google Scholar] [CrossRef]
- Available online: https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices?utm_medium=email&utm_source=govdelivery&utm_source=STAT+Newsletters&utm_campaign=1f31ee8897-health_tech_COPY_01&utm_medium=email&utm_term=0_8cab1d7961-1f31ee8897-15180843 (accessed on 13 May 2024).
- Available online: https://www.fda.gov/media/176814/download (accessed on 13 May 2024).
- Available online: https://www.fda.gov/media/176815/download (accessed on 13 May 2024).
- Available online: https://www.statista.com/statistics/1410751/vr-and-ar-medical-devices-approved-in-the-us-by-area/ (accessed on 13 May 2024).
- Available online: https://www.dicomdirector.com/recent-fda-device-reclassifications/ (accessed on 13 May 2024).
- Available online: https://www.dicomdirector.com/category/intravision-xr/ (accessed on 13 May 2024).
- Available online: https://www.fda.gov/media/160086/download (accessed on 13 May 2024).
- Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32017R0745 (accessed on 13 May 2024).
- Available online: https://health.ec.europa.eu/system/files/2023-10/md_mdcg_2023-4_software_en.pdf (accessed on 13 May 2024).
- Bini, F.; Franzò, M.; Maccaro, A.; Piaggio, D.; Pecchia, L.; Marinozzi, F. Is medical device regulatory compliance growing as fast as extended reality to avoid misunderstandings in the future? Health Technol. 2023, 13, 831–842. [Google Scholar] [CrossRef]
- The European Parliament and the Council of the Euroepan Union. Council Directive 93/42/EEC of 14 June 1993 concerning Medical Devices 1993.4. Available online: http://data.europa.eu/eli/dir/1993/42/oj (accessed on 13 May 2024).
- Baxter, C.; Carroll, J.A.; Keogh, B.; Vandelanotte, C. Seeking inspiration: Examining the validity and reliability of a new smartphone respiratory therapy exergame app. Sensors 2021, 21, 6472. [Google Scholar] [CrossRef]
- Franzò, M.; Pica, A.; Pascucci, S.; Serrao, M.; Marinozzi, F.; Bini, F. A proof of Concept Combined using mixed reality for personalized neurorehabilitation of cerebellar ataxic patients. Sensors 2023, 23, 1680. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.; Kennedy-malone, L.; Thompson, J.; Monge, E.C. The effect of an exergame on physical activity among olderadults residing in a long-term care facility: A pilot study. Geriatr. Nurs. 2022, 44, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Pensieri, C.; Pennacchini, M. Overview: Virtual reality in Medicine. J. Virtual Worlds Res. 2014, 7. [Google Scholar] [CrossRef]
- Available online: https://www.canhealth.com/2021/07/28/vr-radiology-platform-approved-by-health-canada/ (accessed on 13 May 2024).
| Review Study | Focus on Diagnostic Imaging | Focus on AR Integration |
|---|---|---|
| Sun et al. (2023) [41] | The study delves into the transformative role of virtual reality (VR) and augmented reality (AR) imaging technologies in hip-related surgery. It reviews 40 studies, showcasing their applications in preoperative simulation, intraoperative navigation, and postoperative rehabilitation. While highlighting their potential to enhance surgical precision and safety, it emphasizes the necessity for more comparative research to accurately gauge their clinical efficacy and cost effectiveness. | The study centers on augmented reality (AR) integration in hip-related surgery. Examining 40 studies, it assesses AR’s utility in preoperative simulation, intraoperative navigation, and postoperative rehabilitation. Despite showing promise for enhancing surgical precision and safety, further comparative research is crucial to fully understand AR’s clinical efficacy and cost effectiveness. |
| Kanschik et al. (2023) [42] | The study delves into the application of virtual reality (VR) and augmented reality (AR) in intensive care medicine, through a systematic review of 59 studies. It highlights how these technologies assist healthcare providers in training, planning procedures, and aiding patients’ well-being within the ICU setting. Despite variations in study design, VR and AR show promise in improving care practices, with the potential for further development and increased utilization in healthcare. | The study examines the integration of augmented reality (AR) in intensive care medicine, reviewing 59 studies to explore possible applications. AR assists healthcare providers in training, planning procedures, and supporting patients within the ICU setting. Despite variations in study design, AR demonstrates potential for enhancing care practices, indicating opportunities for further development and expanded integration in healthcare settings. |
| Guha et al. (2017) [43] | The systematic review investigates the evolution and current application of augmented reality (AR) in neurosurgery, a field known for its advancements in image-guided surgery. Despite challenges, such as registration errors and impaired depth perception, AR shows promise in accurately overlaying three-dimensional datasets in the surgical field. Future advancements in imaging, registration, display technology, and robotics are expected to further enhance AR’s role in improving surgical outcomes in neurosurgery. | The systematic review focuses on the application of augmented reality in neurosurgery, a field renowned for pioneering image-guided surgery. It assesses current neurosurgical AR applications, highlighting challenges like registration errors and impaired depth perception. Despite obstacles, AR’s ability to overlay three-dimensional datasets accurately signifies its potential in enhancing surgical precision. The review anticipates future advancements in imaging, registration, and display technology, underscoring AR’s promising role in neurosurgical operating rooms. |
| Dubron et al. (2023) [44] | The systematic review examines the utilization of extended reality, encompassing augmented reality (AR), mixed reality (MR), and virtual reality (VR), in preoperative planning for orbital fractures. It contrasts extended reality with conventional planning techniques, focusing on computer-aided surgical simulation, patient-specific implants (PSIs), and fracture reconstruction using computed tomography data. The review underscores AR’s role in enhancing accuracy and precision during orbital fracture management, particularly in guiding incisions, identifying anatomical tissues, and facilitating intraoperative imaging enhancement. Furthermore, it highlights VR-based educational tools for offering enhanced visualization and comprehension of craniofacial trauma compared to traditional imaging approaches. | The systematic review specifically examines the role of augmented reality (AR) in preoperative planning for orbital fractures, alongside mixed reality (MR) and virtual reality (VR). It compares AR with conventional planning techniques, emphasizing its contributions to computer-aided surgical simulation, patient-specific implants (PSIs), and fracture reconstruction based on computed tomography data. Notably, AR is highlighted for its ability to enhance accuracy and precision in orbital fracture management, guiding incisions, identifying anatomical tissues, and improving intraoperative imaging. Additionally, the review acknowledges AR’s potential in offering real-time visualization and precise positioning of implants during surgery, demonstrating its value in optimizing surgical outcomes. |
| Seetohul et al. (2023) [45] | The paper provides a systematic review of surgical robotic platforms, focusing on integrating augmented reality (AR) to enhance interventions. It addresses challenges like tool placement accuracy and depth perception in medical imaging. Analyzing robots such as Novarad and SpineAssist, it identifies shortcomings in optimization algorithms and proposes solutions for tool-to-organ collision detection. Despite challenges, the study suggests promising results in reducing occlusion and end-effector collisions, supporting AR’s potential in future surgical applications. | The paper systematically reviews the integration of augmented reality (AR) in surgical robotic platforms, aiming to enhance surgical interventions. It identifies challenges like tool placement accuracy and depth perception in medical imaging, proposing solutions to optimize AR technology. Analyzing robots such as Novarad and SpineAssist, it highlights AR’s role in improving the user’s perception of the augmented world. Despite challenges, the study indicates promising results, supporting AR’s potential to revolutionize surgical procedures in the future. |
| Rodler et al. (2023) [46] | The study provides a comprehensive analysis of new imaging technologies in robotic-assisted radical prostatectomy (RARP) for prostate cancer management. Through a systematic review of 46 studies, it highlights the use of imaging for primary tumor detection, intraoperative lymph node detection, and surgeon training. The feasibility of combining imaging technologies, such as MRI, PSMA-PET CT, and intraoperative dyes, has been demonstrated, but prospective confirmation of improved surgical outcomes is ongoing. | The study focuses on the integration of new imaging technologies, including augmented reality (AR), in robotic-assisted radical prostatectomy (RARP) for prostate cancer management. Through a systematic review of 46 studies, it examines the role of AR in primary tumor detection, intraoperative lymph node detection, and surgeon training. While the feasibility of combining AR with imaging modalities like MRI and PSMA-PET CT has been demonstrated, ongoing research aims to confirm their prospective impact on surgical outcomes. |
| Chidambaram et al. (2021) [47] | The systematic review delves into the role of augmented reality (AR) technology in neurosurgery, aiming to enhance intraoperative visualization and guidance beyond traditional neuronavigation. Through the analysis of 54 articles, it explores how AR has been integrated into clinical practice in both brain and spine subspecialties. Despite its potential benefits, challenges such as accurate brain segmentation, accounting for brain shift, and reducing coregistration errors need to be addressed for widespread adoption. Additionally, the study suggests future avenues for combining AR with multimodal imaging techniques and artificial intelligence to further improve its impact in neurosurgery. | The systematic review focuses on augmented reality (AR) technology in neurosurgery, aiming to enhance intraoperative visualization and guidance beyond traditional neuronavigation. Analyzing 54 articles, it explores AR’s integration into clinical practice in brain and spine subspecialties. While acknowledging potential benefits, the study highlights challenges like accurate brain segmentation and coregistration errors. It also proposes future research directions, suggesting the combination of AR with multimodal imaging techniques and artificial intelligence to enhance its impact in neurosurgery. |
| Bosc et al. (2019) [48] | The systematic review classifies augmented reality (AR) applications in maxillofacial surgery, distinguishing them from other virtual imaging procedures. Thirteen publications were analyzed, with five describing hands-free and heads-up AR approaches using smart glasses or headsets combined with tracking. Most reported minimal error (<1 mm) between virtual models and patients. AR during surgery is categorized into heads-up guided surgery with or without tracking, guided surgery using semi-transparent screens, digital projection onto patients, and digital data transfer to monitor displays. | The systematic review specifically focuses on augmented reality (AR) applications in maxillofacial surgery, aiming to differentiate them from other virtual imaging procedures. Thirteen publications were analyzed to classify AR methods, with five describing hands-free and heads-up AR approaches using smart glasses or headsets combined with tracking. The study categorizes AR during surgery into four types based on guidance techniques and visualization methods. Most publications reported minimal error between virtual models and patients, highlighting the potential of AR in enhancing surgical precision. |
| Sparwasser et al. (2018) [49] | The article discusses the current and future applications of virtual reality (VR) and augmented reality (AR) in surgery, emphasizing the potential clinical improvements. Through systematic literature research and analysis of investment trends, it highlights the increasing integration of AR and VR technologies into surgical practice. Key applications include intraoperative overlap with radiological imaging, telementoring, and surgical education. While promising, the benefits of AR and VR for clinical endpoints are yet to be fully understood and require rigorous examination through clinical trials. Physicians are expected to play a crucial role in leveraging these technologies for patient benefit in surgery. | The article assesses the current and future applications of augmented reality (AR) in surgery, alongside virtual reality (VR). Through systematic literature research and analysis, it highlights the increasing integration of AR into surgical practice. Key areas of focus include intraoperative overlap with radiological imaging, telementoring, and surgical education. However, the article also acknowledges the need for rigorous clinical trials to fully understand the benefits of AR for clinical endpoints. Physicians are expected to play a pivotal role in leveraging AR technology for patient benefit in surgery. |
| Ong et al. (2021) [50] | The systematic review explores the utility of extended reality (XR) in ophthalmology, covering education, diagnostics, and therapeutics. Out of 12,490 records, 87 met the eligibility criteria, with most studies focusing on education. While XR shows promise, the majority of studies were of poor quality, and only a few addressed validity evidence. Surgical simulators were found to improve performance and reduce complications, while ophthalmoscopy simulators enhanced clinical skills. In diagnostics, XR platforms demonstrated a proof-of-concept in presenting ocular imaging data and assessing patients with ophthalmic diseases. In therapeutics, heads-up surgical systems showed comparable outcomes compared to conventional surgery. However, more high-quality comparative studies are needed to fully evaluate XR’s role in ophthalmic practice. | The systematic review investigates the utility of extended reality (XR), which includes augmented reality (AR), in ophthalmology, particularly in education, diagnostics, and therapeutics. Out of 12,490 records, 87 studies met the eligibility criteria, with the majority focusing on education. While promising, most studies were of poor quality, and only a few addressed validity evidence. Surgical simulators were found to improve performance and reduce complications, while ophthalmoscopy simulators enhanced clinical skills. In diagnostics, XR platforms demonstrated a proof-of-concept in presenting ocular imaging data and assessing patients with ophthalmic diseases. However, more high-quality comparative studies are needed to fully assess the role of XR, including AR, in ophthalmic practice. |
| Umana et al. (2023) [51] | The study investigates the management of subaxial cervical spine spondylodiscitis, focusing on ≥three-level cervical corpectomies. A literature review and an emblematic case presentation are conducted. Thirteen papers were selected, with 28 patients treated with ≥three-level corpectomy. A combined anterior and posterior approach was common, with minimal intraoperative complications. Postoperative complications included wound hematoma, pneumonia, and dysphagia. The study concludes that multilevel corpectomies for cervical spinal osteomyelitis are safe and effective, especially with multimodal navigation utilizing intraoperative imaging and augmented reality. | The study primarily focuses on the management of subaxial cervical spine spondylodiscitis, particularly regarding ≥three-level cervical corpectomies. While the study does not specifically emphasize augmented reality (AR), it does mention the use of multimodal navigation, which includes AR, during the surgical procedure. The authors highlight the potential benefits of merging intraoperative imaging acquisition, navigation, and augmented reality for guiding implant positioning in complex anatomies and assessing optimal surgical outcomes. |
| Doughty et al. (2022) [52] | The systematic review evaluates challenges in using optical see-through head-mounted displays (OST-HMDs) for AR-assisted surgery. Fifty-seven articles from January 2021 to March 2022 were categorized based on AR navigation components. CT scans and surface-rendered models were commonly used preoperatively. Microsoft HoloLens was the primary OST-HMD, with emphasis on orthopedic and maxillofacial surgeries. Despite promising accuracy, human and technical challenges persist that need to be addressed before widespread adoption. | The systematic review investigates challenges in utilizing optical see-through head-mounted displays (OST-HMDs) for augmented reality (AR)-assisted surgery. It highlights the prevalence of Microsoft HoloLens devices and common preoperative input data sources like computed tomography (CT) scans. Virtual content is often directly superimposed onto target sites, but challenges related to perception and interaction need addressing before widespread AR adoption in surgical navigation. |
| Rodriguez Peñaranda et al. (2023) [53] | The review investigates the role of artificial intelligence (AI) in kidney cancer surgical training, utilizing advanced imaging techniques. Following PRISMA 2020 criteria, PubMed and SCOPUS databases were searched, yielding 14 eligible studies. AI applications include analyzing surgical workflows, annotating instruments, and 3D reconstruction. AI enhances surgical skill appraisal and offers benefits in intraoperative guidance and preoperative preparation. Challenges remain in regard to real-time tracking and registration. While AI shows promise in advancing surgical training with unbiased evaluations and personalized feedback, concerns regarding metric measurement, ethics, and data privacy must be addressed for full integration. | The review discusses the potential role of artificial intelligence (AI) in kidney cancer surgical training, with a focus on advanced imaging techniques. While the review primarily emphasizes AI applications, it briefly mentions augmented reality (AR) as part of the technology landscape that can enhance training. Specifically, AR could potentially contribute to surgical skill appraisal and provide benefits in terms of intraoperative guidance and preoperative preparation. However, the review does not extensively explore AR’s role compared to AI. |
| Colombo et al. (2022) [54] | The systematic review focuses on 3D segmentation and visualization techniques for brain arteriovenous malformations (bAVMs). Thirty-three studies were included, with MRI, DSA, and CT as primary imaging modalities. Automatic segmentation was predominant (61%), with a median time of 10 min. Semiautomatic and manual segmentation methods were also used. Most studies utilized screens for visualization, while only one utilized a heads-up display (HUD). Integration with mixed reality was found in four studies. The review underscores the absence of a gold standard and highlights the growing trend toward machine learning-based segmentation algorithms, particularly unsupervised fuzzy-based algorithms, suggesting ongoing efforts for improvement and innovation of visualization tools. | The systematic review primarily focuses on 3D segmentation and visualization techniques for brain arteriovenous malformations (bAVMs), without specific emphasis on augmented reality (AR). While the review discusses various visualization methods, including integration with mixed reality in four studies, it does not extensively explore AR’s role compared to other techniques. Therefore, AR’s specific application in the context of bAVM visualization is not a central focus of the review. |
| Checcucci et al. (2020) [55] | The systematic review assesses the impact of 3D printed and virtual imaging on preoperative and intraoperative aspects of robotic nephron-sparing surgery (NSS) for kidney cancer. Ten articles meeting the inclusion criteria were reviewed, with an overall ‘intermediate’ quality score and a moderate/high risk of bias across the studies. Specifically, 3D-printed models were deemed more useful for preoperative simulations and patient counseling, enhancing the understanding of anatomical structures and procedures. However, cost and material quality remain limitations. Virtual imaging in a mixed reality environment improved preoperative planning, while intraoperatively, augmented reality techniques allowed for overlaying 3D models onto real anatomy. Despite being a developing technology, virtual imaging shows promise, with potential applications expanding over time. | The systematic review primarily focuses on the impact of 3D printed and virtual imaging technologies on robotic nephron-sparing surgery (NSS) for kidney cancer, without specific emphasis on augmented reality (AR). While the review discusses the use of 3D virtual models in a mixed reality environment for preoperative planning and mentions augmented reality procedures intraoperatively, it does not extensively explore AR’s role compared to other techniques. Therefore, AR’s specific application in the context of NSS for kidney cancer is not a central focus of the review. |
| Unberath et al. (2021) [56] | The manuscript discusses the potential of image-based navigation, particularly in minimally invasive surgery, emphasizing its role in enhancing reproducibility, safety, and precision. It highlights the importance of 2D/3D registration in spatial relationship estimation between preoperative 3D structures and intraoperative 2D images, such as X-ray fluoroscopy or endoscopy. While traditional analytical solutions face challenges, the emergence of machine learning-based approaches offers promise in addressing these issues by approximating functional mapping. The review provides insights into recent advancements in machine learning’s impact on 2D/3D registration and outlines pressing needs, open problems, and potential future directions in the field. | The text primarily focuses on image-based navigation and the impact of machine learning on 2D/3D registration in the context of minimally invasive surgery. Augmented reality is cited in relation to its role at the intersection with image-based navigation, as AR technologies can enhance surgical visualization by overlaying digital information onto the surgeon’s view of the real-world surgical environment. While not directly focused on AR, in this study it is remarked that AR could potentially play a role in the broader discussion on advancing surgical workflows and mixed reality environments mentioned in the text. |
| Review Study | Theme |
|---|---|
| Sun et al. (2023) [41] | Revolutionary potential of VR and AR in hip surgery, emphasizing preoperative simulation, intraoperative navigation, and postoperative rehabilitation. |
| Kanschik et al. (2023) [42] | Potential of VR and AR in ICU for training, stress reduction, pain management, rehabilitation, and communication enhancement. |
| Guha et al. (2017) [43] | Pioneering role of AR in neurosurgery, focusing on image-guided surgery and the challenges and prospects associated with its precise application. |
| Dubron et al. (2023) [44] | Use of ER, AR, MR, and VR in preoperative planning of orbital fractures, highlighting AR’s role in improving surgical accuracy and precision. |
| Seetohul et al. (2023) [45] | Integration of AR into surgical robotic and autonomous systems, emphasizing the need for improved accuracy and advanced imaging techniques. |
| Rodler et al. (2023) [46] | Integration of new imaging technologies in robotic-assisted radical prostatectomy for prostate cancer, focusing on imaging modalities and their potential benefits. |
| Chidambaram et al. (2021) [47] | Application of AR technology in neurosurgery, particularly its potential to improve intraoperative visualization and surgical precision. |
| Bosc et al. (2019) [48] | Evaluation of AR applications in maxillofacial surgery, categorizing surgical approaches and emphasizing accuracy with minimal errors. |
| Sparwasser et al. (2018) [49] | Integration and future prospects of AR and VR in surgery, highlighting their potential to improve clinical outcomes, surgical training, and intraoperative procedures. |
| Ong et al. (2021) [50] | Use of ER (VR, AR, MR) in ophthalmology for education, diagnostics, and therapeutics, focusing on its potential benefits and the need for further research. |
| Umana et al. (2023) [51] | Application of augmented reality and neuronavigation in complex spinal treatments, emphasizing successful outcomes and challenges. |
| Doughty et al. (2022) [52] | Investigation of challenges with optical see-through head-mounted displays (OST-HMDs) for AR in surgery, focusing on system accuracy and technical difficulties. |
| Rodriguez Peñaranda et al. (2023) [53] | Role of artificial intelligence (AI) in renal cancer surgery training, particularly its application in advanced imaging for improved training and planning. |
| Colombo et al. (2022) [54] | Evaluation of 3D segmentation and visualization techniques for brain arteriovenous malformations (bAVMs), emphasizing the potential of automatic segmentation algorithms and the need for improvements. |
| Checcucci et al. (2020) [55] | Impact of 3D printing and virtual imaging on preoperative planning and intraoperative navigation in robotic nephron-sparing surgery in kidney cancer, highlighting their advantages and limitations. |
| Unberath et al. (2021) [56] | Role of image-based navigation in minimally invasive surgery, focusing on its potential to improve precision, safety, and cost effectiveness, and the role of machine learning in addressing registration challenges. |
| Area | Potential | References |
|---|---|---|
| Enhanced Visualization and Spatial Awareness | AR overlays digital information onto the surgical field in real-time, enhancing spatial awareness and allowing for precise navigation of anatomical structures. Surgeons can visualize critical structures in a 3D space, improving surgical interventions. | [41,43,45,47,49,53] |
| Preoperative Planning and Simulation | AR integrates patient-specific imaging data into a 3D virtual environment for comprehensive preoperative planning and simulation. Surgeons can rehearse procedures, reducing risks and improving outcomes. | [41,44,49,54,55,56] |
| Intraoperative Navigation and Guidance | AR-based navigation systems provide real-time guidance to surgeons, enhancing precision and efficiency during procedures. Surgeons can accurately locate target structures and optimize instrument positioning. | [41,43,45,47,49,53] |
| Education and Training | AR offers innovative solutions for surgical education and training, enabling trainees to practice complex procedures in realistic scenarios. Immediate feedback enhances skill development and proficiency. | [41,42,44,49,50,55] |
| Patient Engagement and Communication | AR enhances patient engagement by providing interactive visualizations of medical conditions and treatment plans. Surgeons can educate patients and foster shared decision-making, improving satisfaction and adherence to treatment. | [42,49,55] |
| Personalized Medicine and Surgical Precision | AR enables personalized surgical interventions based on patient-specific data and anatomical models. Surgeons can tailor treatments for optimal outcomes and enhance precision with real-time feedback. | [41,44,49,54,55,56] |
| Research and Innovation | AR facilitates research on surgical techniques and outcomes assessments. It accelerates advancements in medical device development and the exploration of innovative solutions. | [41,45,53,56] |
| Area | Description | Integrated Technologies | Studies |
|---|---|---|---|
| Hip-related Surgery | VAR technologies enhance precision and safety. Integration with robotics optimizes workflows, positioning, and implants. | Robotics, AI, VAR | “Virtual Reality and Augmented Reality in Hip-Related Surgery” (Reference [41]) |
| Intensive Care Medicine | VAR with AI revolutionizes training and patient care. AI analyzes data, while VAR provides guidance. | Robotics, AI, VAR | “Virtual Reality and Augmented Reality in Intensive Care Medicine” (Reference [42]) |
| Neurosurgery | Robotics and AI with VAR improve navigation and visualization, enhancing surgical outcomes. | Robotics, AI, VAR | “Augmented Reality in Neurosurgery” (Reference [43]) |
| Orbital Fractures | Integration facilitates preoperative planning and guidance. AI analyzes data, VAR aids visualization. | Robotics, AI, VAR | “Extended Reality in Preoperative Planning for Orbital Fractures” (Reference [44]) |
| Renal Cell Carcinoma | VAR with robotics and AI offer personalized treatment and training. AI customizes approaches, VAR aids visualization. | Robotics, AI, VAR | “Artificial Intelligence in Kidney Cancer Surgery” (Reference [53]) |
| Area of Improvement | Specific Key Suggestions for Broader Investigation | References |
|---|---|---|
| Preoperative Planning and Simulation | 1. Validate accuracy and clinical benefits of AR-assisted preoperative planning through rigorous clinical studies. | [44,51] |
| 2. Investigate AR applications in complex procedures, like orbital fractures and spinal surgeries, to assess effectiveness. | [44,51] | |
| Intraoperative Navigation and Guidance | 1. Address challenges, such as those related to accurate brain segmentation and hardware limitations, to scale AR use in neurosurgery. | [43,47,52] |
| 2. Conduct further research to enhance AR-based navigation systems for improved surgical precision and efficiency. | [41,43,45,47,49,53] | |
| Education and Training | 1. Evaluate and validate the efficacy of AR-driven educational tools through rigorous clinical studies. | [42,50] |
| 2. Integrate AR-based training into existing curricula and assess its impact on skill development and patient outcomes. | [41,42,44,49,50,55] | |
| Personalized Medicine and Surgical Precision | 1. Continue research and development efforts to improve technical accuracy of AR systems. | [41,44,49,54,55,56] |
| 2. Validate the clinical benefits of AR in personalized medicine through longitudinal studies and real-world applications. | [41,44,49,54,55,56] | |
| Overall Integration of AR in Surgery | 1. Foster collaborative efforts among clinicians, engineers, and researchers to address the technical challenges and validate the clinical benefits. | [41,45,53,56] |
| 2. Ensure seamless integration of AR technology into surgical practice by prioritizing interoperability and user-friendly interfaces. | [41,45,53,56] |
| Areas Requiring Broader Investigation | References |
|---|---|
| Integration of VR, AR, and robotics in terms of synergy | [41,42,43,44,53] |
| Clinical outcomes and comparative studies | [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56] |
| Optimization of surgical workflows | [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56] |
| Technological challenges and solutions | [41,42,43,49,50,51,52,56] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lastrucci, A.; Wandael, Y.; Barra, A.; Ricci, R.; Maccioni, G.; Pirrera, A.; Giansanti, D. Exploring Augmented Reality Integration in Diagnostic Imaging: Myth or Reality? Diagnostics 2024, 14, 1333. https://doi.org/10.3390/diagnostics14131333
Lastrucci A, Wandael Y, Barra A, Ricci R, Maccioni G, Pirrera A, Giansanti D. Exploring Augmented Reality Integration in Diagnostic Imaging: Myth or Reality? Diagnostics. 2024; 14(13):1333. https://doi.org/10.3390/diagnostics14131333
Chicago/Turabian StyleLastrucci, Andrea, Yannick Wandael, Angelo Barra, Renzo Ricci, Giovanni Maccioni, Antonia Pirrera, and Daniele Giansanti. 2024. "Exploring Augmented Reality Integration in Diagnostic Imaging: Myth or Reality?" Diagnostics 14, no. 13: 1333. https://doi.org/10.3390/diagnostics14131333
APA StyleLastrucci, A., Wandael, Y., Barra, A., Ricci, R., Maccioni, G., Pirrera, A., & Giansanti, D. (2024). Exploring Augmented Reality Integration in Diagnostic Imaging: Myth or Reality? Diagnostics, 14(13), 1333. https://doi.org/10.3390/diagnostics14131333







